A Concise Review of Silver Diamine Fluoride on Oral Biofilm
Abstract
1. Introduction
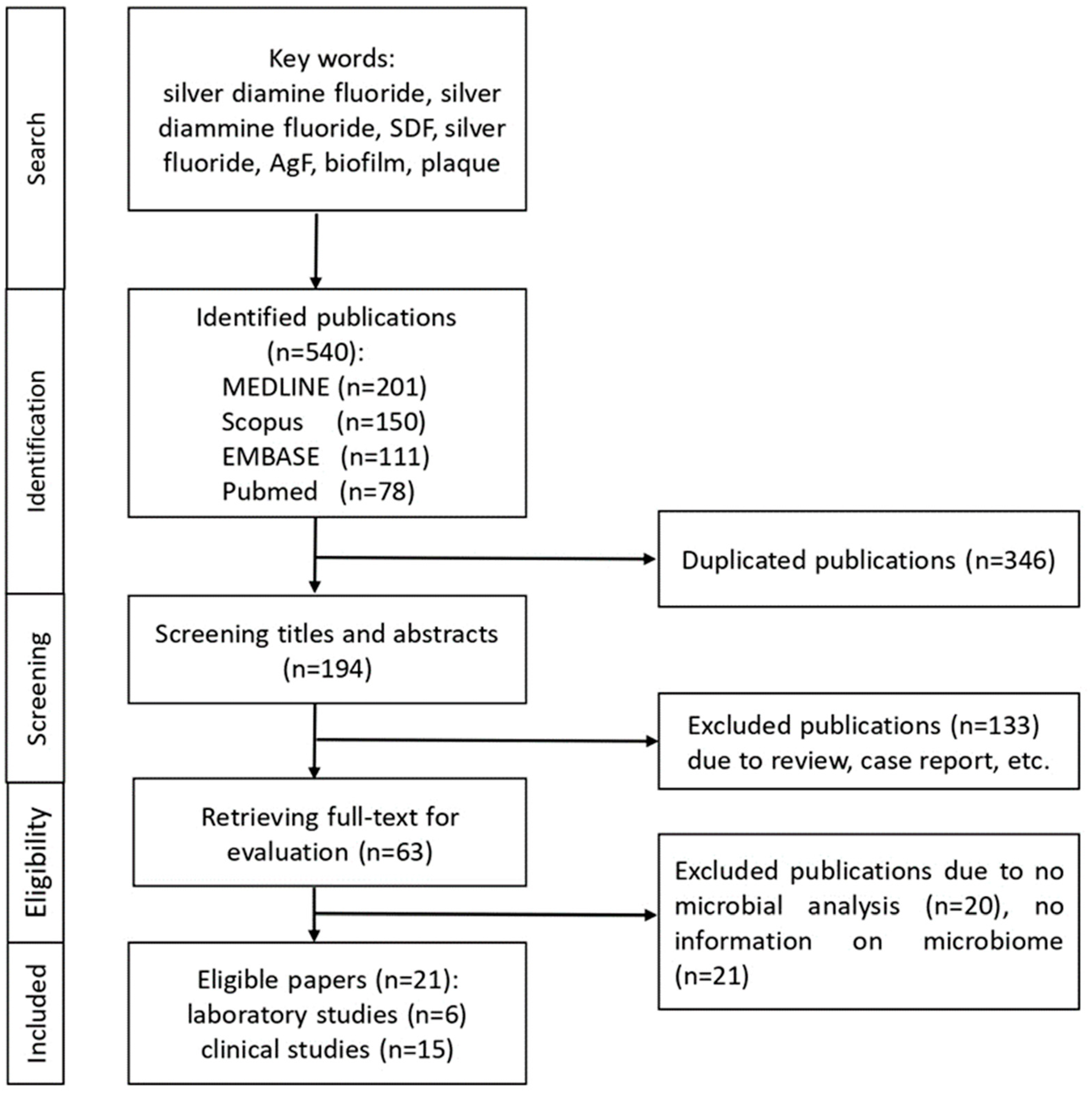
2. Materials and Methods
3. Results
3.1. Application of Silver Diamine Fluoride on Bacteria
3.1.1. Antibacterial Effect
3.1.2. Microbiota Change in Community Diversity and/or Composition within Biofilm
3.2. Application of Silver Diamine Fluoride on Fungus
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Washio, J.; Mayanagi, G.; Takahashi, N. Challenge to metabolomics of oral biofilm. J. Biosci. 2010, 52, 225. [Google Scholar] [CrossRef]
- Takahashi, N.; Nyvad, B. The role of bacteria in the caries process: Ecological perspectives. J. Dent. Res. 2011, 90, 294–303. [Google Scholar] [CrossRef]
- Margolis, H.; Moreno, E. Composition and cariogenic potential of dental plaque fluid. Crit. Rev. Oral Biol. Med. 1994, 5, 1–25. [Google Scholar] [CrossRef]
- Kleinberg, I. A mixed-bacteria ecological approach to understanding the role of the oral bacteria in dental caries causation: An alternative to Streptococcus mutans and the specific-plaque hypothesis. Crit. Rev. Oral Biol. Med. 2002, 13, 108–125. [Google Scholar] [CrossRef]
- Tanzer, J.M.; Livingston, J.; Thompson, A.M. The microbiology of primary dental caries in humans. J. Dent. Educ. 2001, 65, 1028–1037. [Google Scholar] [CrossRef]
- Hamada, S.; Slade, H.D. Biology, immunology, and cariogenicity of Streptococcus mutans. Microbiol. Rev. 1980, 44, 331–384. [Google Scholar] [CrossRef]
- Loesche, W.J. Role of Streptococcus mutans in human dental decay. Microbiol. Rev. 1986, 50, 353–380. [Google Scholar] [CrossRef]
- Yamaga, R.; Yokomizo, I. Arrestment of caries of deciduous teeth with diamine silver fluoride. Dent. Outlook 1969, 33, 1007–1013. [Google Scholar]
- Chu, C.H.; Lo, E.C.M. Promoting caries arrest in children with silver diamine fluoride: A review. Oral Health Prev. Dent. 2008, 6, 315–321. [Google Scholar]
- Horst, J.A. Silver fluoride as a treatment for dental caries. Adv. Dent. Res. 2018, 29, 135–140. [Google Scholar] [CrossRef]
- Mei, M.L.; Lo, E.C.M.; Chu, C.H. Clinical use of silver diamine fluoride in dental treatment. Compend. Contin. Educ. Dent. 2016, 37, 93–98. [Google Scholar] [PubMed]
- Peng, J.Y.; Botelho, M.; Matinlinna, J. Silver compounds used in dentistry for caries management: A review. J. Dent. 2012, 40, 531–541. [Google Scholar] [CrossRef]
- Nassar, H.M.; Gregory, R.L. Biofilm sensitivity of seven Streptococcus mutans strains to different fluoride levels. J. Oral Microbiol. 2017, 9, 1328265. [Google Scholar] [CrossRef] [PubMed]
- Pandit, S.; Kim, J.E.; Jung, K.H.; Chang, K.W.; Jeon, J.G. Effect of sodium fluoride on the virulence factors and composition of Streptococcus mutans biofilms. Arch. Oral Biol. 2011, 56, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Mei, L.; Seneviratne, C.J.; Lo, E.C.M. Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int. J. Paediatr. Dent. 2012, 22, 2–10. [Google Scholar] [CrossRef]
- Fakhruddin, K.S.; Egusa, H.; Ngo, H.C.; Panduwawala, C.; Pesee, S.; Venkatachalam, T.; Samaranayake, L.P. Silver diamine fluoride (SDF) used in childhood caries management has potent antifungal activity against oral Candida species. BMC Microbiol. 2020, 20, 95. [Google Scholar] [CrossRef]
- Yu, O.Y.; Zhao, I.S.; Mei, M.L.; Lo, E.C.M.; Chu, C.H. Caries-arresting effects of silver diamine fluoride and sodium fluoride on dentine caries lesions. J. Dent. 2018, 78, 65–71. [Google Scholar] [CrossRef]
- Lu, M.; Xiang, Z.; Gong, T.; Zhou, X.; Zhang, Z.; Tang, B.; Zeng, J.; Wang, L.; Cui, T.; Li, Y. Intrinsic fluoride tolerance regulated by a transcription factor. J. Dent. Res. 2020, 99, 1270–1278. [Google Scholar] [CrossRef]
- Mei, M.L.; Lo, E.C.M.; Chu, C.H. Arresting dentine caries with silver diamine fluoride: What's behind it? J. Dent. Res. 2018, 97, 751–758. [Google Scholar] [CrossRef]
- Gao, S.S.; Zhao, I.S.; Hiraishi, N.; Duangthip, D.; Mei, M.L.; Lo, E.C.M.; Chu, C.H. Clinical trials of silver diamine fluoride in arresting caries among children: A systematic review. JDR Clin. Trans. Res. 2016, 1, 201–210. [Google Scholar] [CrossRef]
- Hendre, A.D.; Taylor, G.W.; Chávez, E.M.; Hyde, S. A systematic review of silver diamine fluoride: Effectiveness and application in older adults. Gerodontology 2017, 34, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Rams, T.E.; Sautter, J.D.; Ramírez-Martínez, G.J.; Whitaker, E.J. Antimicrobial activity of silver diamine fluoride on human periodontitis microbiota. Gen Dent. 2020, 68, 24–28. [Google Scholar]
- Shah, S.; Bhaskar, V.; Venkataraghavan, K.; Choudhary, P.; Ganesh, M.; Trivedi, K. Efficacy of silver diamine fluoride as an antibacterial as well as antiplaque agent compared to fluoride varnish and acidulated phosphate fluoride gel: An in vivo study. Indian J. Dent. Res. 2013, 24, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Göstemeyer, G.; Kohls, A.; Paris, S.; Schwendicke, F. Root caries prevention via sodium fluoride, chlorhexidine and silver diamine fluoride in vitro. Odontology 2018, 106, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Hiraishi, N.; You, C.K.; King, N.M.; Tagami, J.; Tay, F.R. Antimicrobial efficacy of 3.8% silver diamine fluoride and its effect on root dentin. J. Endod. 2010, 36, 1026–1029. [Google Scholar] [CrossRef] [PubMed]
- Göstemeyer, G.; Schulze, F.; Paris, S.; Schwendicke, F. Arrest of root carious lesions via sodium fluoride, chlorhexidine and silver diamine fluoride in vitro. Materials 2017, 11, 9. [Google Scholar] [CrossRef] [PubMed]
- Al-Madi, E.M.; Al-Jamie, M.A.; Al-Owaid, N.M.; Almohaimede, A.A.; Al-Owid, A.M. Antibacterial efficacy of silver diamine fluoride as a root canal irrigant. Clin. Exp. Dent. Res. 2019, 5, 551–556. [Google Scholar] [CrossRef]
- Soekanto, S.A.; Marpaung, L.J.; Himmatushohwah Djais, A.A.; Rina, R. Efficacy of propolis fluoride and nano silver fluoride for inhibition of streptococcus mutans and enterococcus faecalis biofilm formation. Int. J. App. Pharm. 2017, 9, 51–54. [Google Scholar] [CrossRef]
- Liu, B.Y.; Mei, L.; Chu, C.H.; Lo, E.C.M. Effect of silver fluoride in preventing the formation of artificial dentinal caries lesions in vitro. Chin. J. Dent. Res. 2019, 22, 273–280. [Google Scholar]
- Mei, M.L.; Yan, Z.; Duangthip, D.; Niu, J.Y.; Yu, O.Y.; You, M.; Lo, E.C.M.; Chu, C.H. Effect of silver diamine fluoride on plaque microbiome in children. J. Dent. 2020, 102, 103479. [Google Scholar] [CrossRef]
- Milgrom, P.; Horst, J.A.; Ludwig, S.; Rothen, M.; Chaffee, B.W.; Lyalina, S.; Pollard, K.S.; DeRisi, J.L.; Mancl, L. Topical silver diamine fluoride for dental caries arrest in preschool children: A randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J. Dent. 2018, 68, 72–78. [Google Scholar] [CrossRef]
- Mitwalli, H.; Mourao, M.D.A.; Dennison, J.; Yaman, P.; Paster, B.J.; Fontana, M. Effect of silver diamine fluoride treatment on microbial profiles of plaque biofilms from root/cervical caries lesions. Caries Res. 2019, 53, 555–566. [Google Scholar] [CrossRef] [PubMed]
- Alshahni, R.Z.; Alshahni, M.M.; Hiraishi, N.; Makimura, K.; Tagami, J. Effect of silver diamine fluoride on reducing candida albicans adhesion on dentine. Mycopathologia 2020, 185, 691–698. [Google Scholar] [PubMed]
- Wu, L.; Gareiss, S.K.; Morrow, B.R.; Babu, J.P.; Hottel, T.; Garcia-Godoy, F.; Li, F.; Hong, L. Antibacterial properties of silver-loaded gelatin sponges prepared with silver diamine fluoride. Am. J. Dent. 2019, 32, 276–280. [Google Scholar]
- Vinson, L.A.; Gilbert, P.R.; Sanders, B.J.; Moser, E.; Gregory, R.L. Silver diamine fluoride and potassium iodide disruption of in vitro streptococcus mutans biofilm. J. Dent. Child. 2018, 85, 120–124. [Google Scholar]
- Sorkhdini, P.; Gregory, R.L.; Crystal, Y.O.; Tang, Q.; Lippert, F. Effectiveness of in vitro primary coronal caries prevention with silver diamine fluoride—Chemical vs biofilm models. J Dent. 2020, 99, 103418. [Google Scholar] [CrossRef]
- Mei, M.L.; Li, Q.L.; Chu, C.H.; Lo, E.C.M.; Samaranayake, L.P. Antibacterial effects of silver diamine fluoride on multi-species cariogenic biofilm on caries. Ann. Clin. Microbiol. Antimicrob. 2013, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Lou, Y.; Botelho, M.G.; Darvel, B.W. Reaction of silver diamine fluoride with hydroxyapatite and protein. J. Dent. 2011, 39, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Knight, G.M.; McIntyre, J.M.; Craig, G.G.; Mulyani Zilm, P.S.; Gully, N.J. Inability to form a biofilm of Streptococcus mutans on silver fluoride-and potassium iodide-treated demineralized dentin. Quintessence Int. 2009, 40, 155–161. [Google Scholar]
- Lou, Y.; Darvell, B.W.; Botelho, M.G. Antibacterial effect of silver diamine fluoride on cariogenic organism. J. Contemp. Dent. Pract. 2018, 19, 591–598. [Google Scholar]
- Pandit, S.; Kim, G.; Lee, M.; Jeon, J. Evaluation of streptococcus mutans biofilms formed on fluoride releasing and non fluoride releasing resin composites. J. Dent. 2011, 39, 780–787. [Google Scholar] [CrossRef] [PubMed]
- Esberg, A.; Sheng, N.; Mårell, L.; Claesson, R.; Persson, K.; Borén, T.; Strömberg, N. Streptococcus mutans adhesin biotypes that match and predict individual caries development. EBioMedicine 2017, 24, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Dachang, W.; Lei, Z.; Jianjun, L.; Juanjuan, Q.; Yi, X. Effect of Lactobacillus species on Streptococcus mutans biofilm formation. Pak. J. Pharm. Sci. 2014, 27, 1523–1528. [Google Scholar] [PubMed]
- Zhu, B.; Li, J.Y.; Hao, Y.Q.; Zhou, X.D. Establishment and evaluation of the in vitro dynamic biofilm model. Shanghai Kou Qiang Yi Xue. 2010, 19, 60–65. [Google Scholar]
- Takahashi, N.; Nyvad, B. Caries ecology revisited: Microbial dynamics and the caries process. Caries Res. 2008, 42, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.A.; Costa, A.C.; Silva, M.P.; Back-Brito, G.N.; Jorge, A.O. Candida albicans and virulence factors that increases it pathogenicity. The battle against microbial pathogens: Basic science, technological advances and educational programs; microbiology series, vol. 2. Badajoz FORMATEX Res. Cent. 2015, 61, 1. [Google Scholar]
- Modrzewska, B.; Kurnatowski, P. Adherence of Candida sp. to host tissues and cells as one of its pathogenicity features. Ann. Parasitol. 2015, 61, 1. [Google Scholar]
- Carradori, S.; Chimenti, P.; Fazaari, M.; Granese, A.; Angiolella, L. Antimicrobial activity, synergism and inhibition of germ tube formation by crocus sativus-derived compounds against Candida spp. J. Enzyme Inhib. Med. Chem. 2016, 31, 189–193. [Google Scholar] [CrossRef]
- Xiao, J.; Huang, X.; Alkhers, N.; Alzamil, H.; Alzoubi, S.; Wu, T.T.; Castillo, D.A.; Campbell, F.; Davis, J.; Hrzog, K. Candida albicans and early childhood caries: A systematic review and meta-analysis. Caries Res. 2018, 52, 102–112. [Google Scholar] [CrossRef]
| Author, Year | Setting; Substrate | Microbiota | Period; Assessment | Intervention | Antibacterial Effect |
|---|---|---|---|---|---|
| Hiraishi et al., 2010 | In vitro; human dentin | E. faecalis | 15 min, 60 min; CFU | Gp1: Ca(OH)2 Gp2: SDF Gp3: NaOCl Gp4: NaCl | CFU 15 min Gp2, Gp3 < Gp1, Gp4 CFU 60 min: G2, Gp3 had no E. faecalis |
| Chu et al., 2012 | In vitro; human dentin | S. mutans, A. naeslundii | 7 days; CFU, CLSM | Gp1: SDF Gp2: Water | CFU: Gp1 < Gp2 CLSM: Gp2 < Gp1 |
| Mei et al., 2013a | In vitro; human dentin | S. mutans L. acidophilus | 7 days; CFU, CLSM | Gp1: SDF Gp2: Water | CFU: Gp1 < Gp2 CLSM: Gp2 < Gp1 |
| Mei et al., 2013b | In vitro; human dentin | Consortium of S. mutans, S. sobrinus, L. acidophilus, L. rhamnosus, A. naeslund | 7 days, 14 days, 21 days; CFU, CLSM | Gp1: SDF Gp2: Water | CFU: Gp1 < Gp2 CLSM: Gp2 < Gp1 |
| Shah et al., 2013 | In vivo | S. mutans | BL, 3 days, 6 months, 12 months, 18 months; CFU | Gp1: SDF Gp2: NaF + CaF Gp3: APF gel | CFU: Gp1 < Gp2 Gp1 = Gp3 |
| Savas et al., 2015 | In vitro; bovine enamel | S. mutans | 7 days; TBC, pH | Gp1: Water Gp2: SDF | Antibacterial activity: Gp2 > Gp1 |
| Göstemeyer et al., 2017 | In vitro; bovine dentine | L. rhamnosus | 6 days; CFU | Gp1: Water Gp2: SDF | CFU: Gp2 < Gp1 |
| Soekanto et al., 2017 | In vitro | S. mutans, E. faecalis | 1 day; MIC, MBC | Gp1: SDF Gp2: NSF Gp3: PPF | MIC: Gp2: 3%-S.mutans, 3%-E.faecalis; Gp3: 3%-S.mutans, 6%-E.faecalis; MBC: Gp2: 4%-S.mutans, 4%-E.faecalis; Gp3: 10%-S.mutans |
| Göstemeyer et al., 2018 | In vitro; bovine dentin | L. rhamnosus | 12 days; CFU | Gp1: SDF Gp2: CHX Gp3: N/T | CFU: No significant difference |
| Vinson et al., 2018 | In vitro | S. mutans | 1 day; CFU | Gp1: SDF Gp2: SDF + KI Gp3: KI | CFU: Gp3 > Gp2 > Gp1 |
| Yu et al., 2018 | In vitro; human dentin | S. mutans | 7 days; CFU, CLSM | Gp1: SDF + NaF Gp2: SDF Gp3: NaF Gp4: Water | CFU: Gp2 < Gp1 < Gp4 < Gp3 CLSM: Gp2 > Gp1 > Gp3,Gp4 |
| Al-Madi et al., 2019 | In vitro; human dentin | E. faecalis | 21 days; CLSM | Gp1: SDF Gp2: CHX Gp3: NaOCl | CLSM: Gp3 >Gp1 > Gp2 |
| Wu et al., 2019 | In vitro | S. mutans | 4 days: inhibition zone; 7 days: biofilm assay | Gp1: SDF Gp2: No silver Gp3: AgNO3 | Inhibition zone: Gp1,Gp3 > Gp2, Antibacterial activity: Gp1 > Gp2 |
| Sorkhdini et al., 2020 | In vitro; human enamel | S. mutans | 3 days; CFU | Gp1: SDF Gp2: SDF + KI Gp3: AgNO3 Gp4: Water | CFU:Gp1 < Gp2 < Gp3 < Gp4 |
| Rams et al., 2020 | In vitro | Plaque from adults with SP | 7 days; CFU, MALDI-TOF | Gp1: SDF Gp2: N/T | TVC: Gp1 < Gp 2 PLPP: Gp1 < Gp 2 |
| Authors, Year | Setting; Plaque Sample | Microbiome Detecting Method; Time Points | Diversity Assessing Method or Index | Main Findings |
|---|---|---|---|---|
| Milgrom et al., 2018 | In vivo; plaque from children | RNA sequencing; BL, follow-up after 14 to 21 days | LME4 (R core team) | S. mutans and lactobacilli: in all samples except one; Cariogenic bacteria: no significant changes; Diversity analyses: no significant differences |
| Mitwalli et al., 2019 | In vivo; plaque from adults | 16S rDNA PCR; BL, 1 month | Shannon–Weaver index, Fisher’s alpha | Reduced: Actinomyce sp., P. acidifaciens, S. inopinata, Propionibacterium sp., T. denticola, B. dentium, P. denticolens, A. israelii; Diversity analyses: no significant difference pre- and post-intervention |
| Mei et al., 2020 | In vivo; plaque from children | 16S rRNA gene sequencing; BL, 2 weeks, 12 weeks | Shannon index | Active caries: reduced diversity 12 weeks after SDF; S. mutans, Lactobacillus sp. increased; Arrested caries: S. mutans, Lactobacillus sp. reduced; Diversity analyses: no significant change before and after 2 or 12 weeks in active caries |
| Liu et al., 2020 | In vitro; plaque from children | 16S rRNA gene sequencing; BL, 1 day, 7 days | Shannon index | Diversity analyses: no significant change in plaque; Reduction in carbohydrate transportation and metabolic functions in plaque at 1 day and 7 days post-intervention |
| Authors, Year | Setting; Substrate | Candida Species | Period; Assessment | Intervention Group | Main Findings |
|---|---|---|---|---|---|
| Alshahni et al., 2020 | In vitro; human dentin | C. albicans | 3 days; CFU, CQ, Rt-PCR, SEM | Gp1: 3.8% SDF Gp2: 38% SDF Gp3: No treatment | CFU: Gp1,Gp2 < Gp3 CQ: Gp1,Gp2 < Gp3 Rt-PCR: Gp1,Gp2 < Gp3 SEM: Cell wall damage in Gp1, Gp2 |
| Fakhruddin et al., 2020 | In vitro; paper disc | C. albicans, C. glabrata, C. parapsilosis, C. tropicalis, C. krusei, C. dubliniensis | 2 days; ZGI, Multi-PCR, MIC | Gp1: Amphotericin B Gp2: Fluoconazole Gp3: SDF complex | Gp3: anti-candidal potency; UI: Cell wall damage in Gp3; ZGI: C. tropicalis: Gp3 < Gp1,Gp2; C. krusei, C. glabrata, C. albicans: Gp3 > Gp1,Gp2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Got, S.-R.; Yin, I.X.; Lo, E.C.-M.; Chu, C.-H. A Concise Review of Silver Diamine Fluoride on Oral Biofilm. Appl. Sci. 2021, 11, 3232. https://doi.org/10.3390/app11073232
Zhang J, Got S-R, Yin IX, Lo EC-M, Chu C-H. A Concise Review of Silver Diamine Fluoride on Oral Biofilm. Applied Sciences. 2021; 11(7):3232. https://doi.org/10.3390/app11073232
Chicago/Turabian StyleZhang, Jingyang, Sofiya-Roksolana Got, Iris Xiaoxue Yin, Edward Chin-Man Lo, and Chun-Hung Chu. 2021. "A Concise Review of Silver Diamine Fluoride on Oral Biofilm" Applied Sciences 11, no. 7: 3232. https://doi.org/10.3390/app11073232
APA StyleZhang, J., Got, S.-R., Yin, I. X., Lo, E. C.-M., & Chu, C.-H. (2021). A Concise Review of Silver Diamine Fluoride on Oral Biofilm. Applied Sciences, 11(7), 3232. https://doi.org/10.3390/app11073232







