Effect of Digital Technologies on the Marginal Accuracy of Conventional and Cantilever Co–Cr Posterior-Fixed Partial Dentures Frameworks
Abstract
1. Introduction
2. Materials and Methods
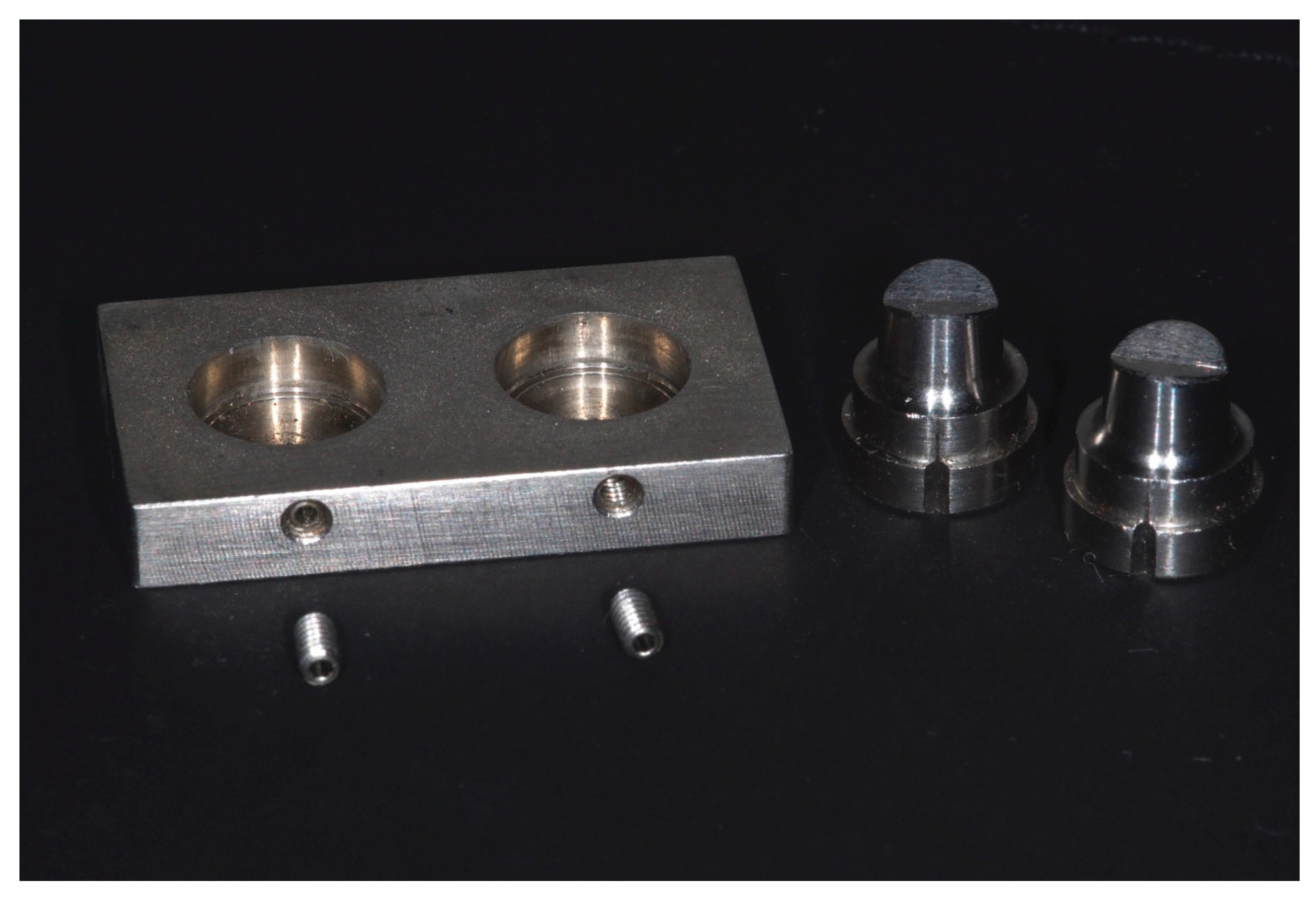
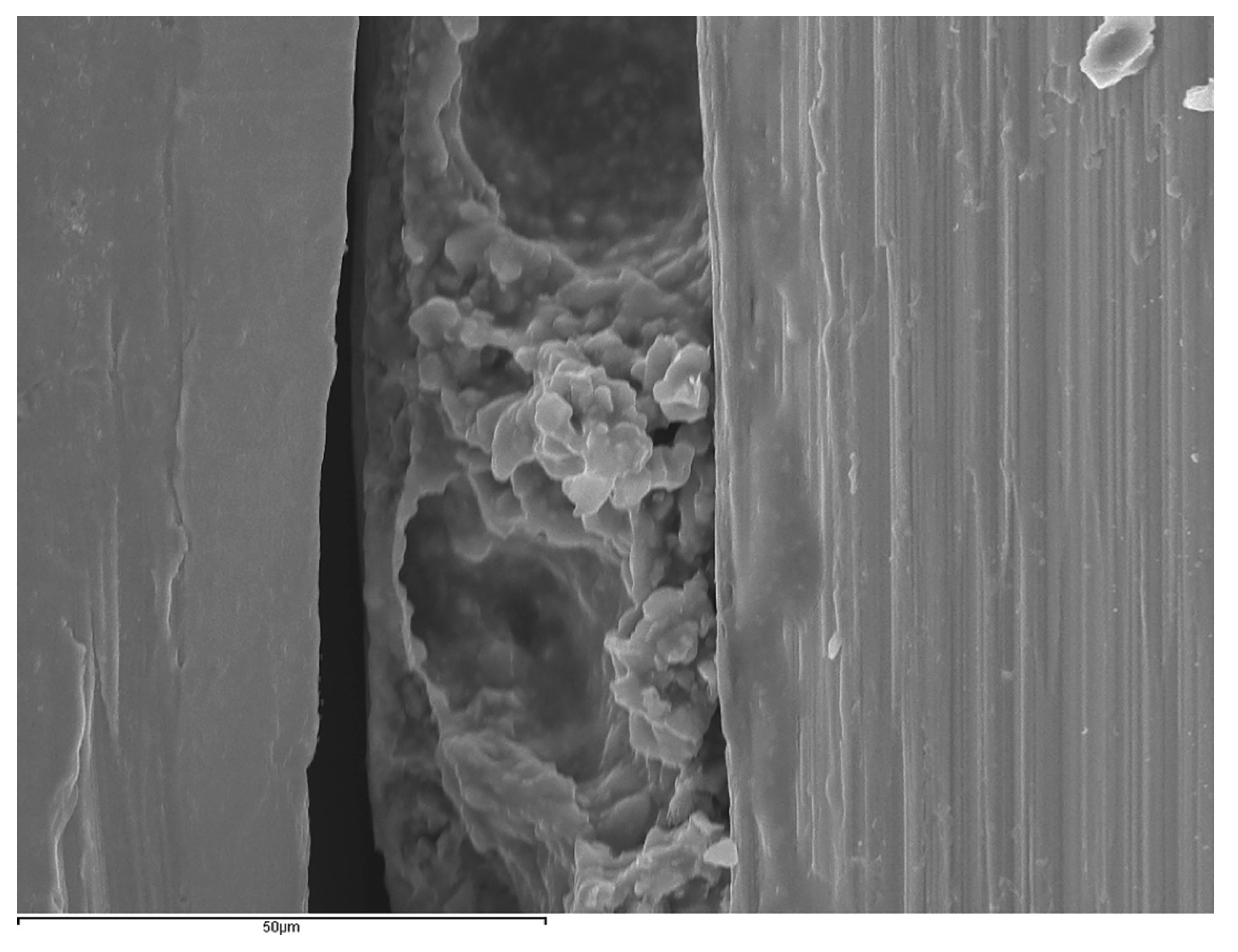
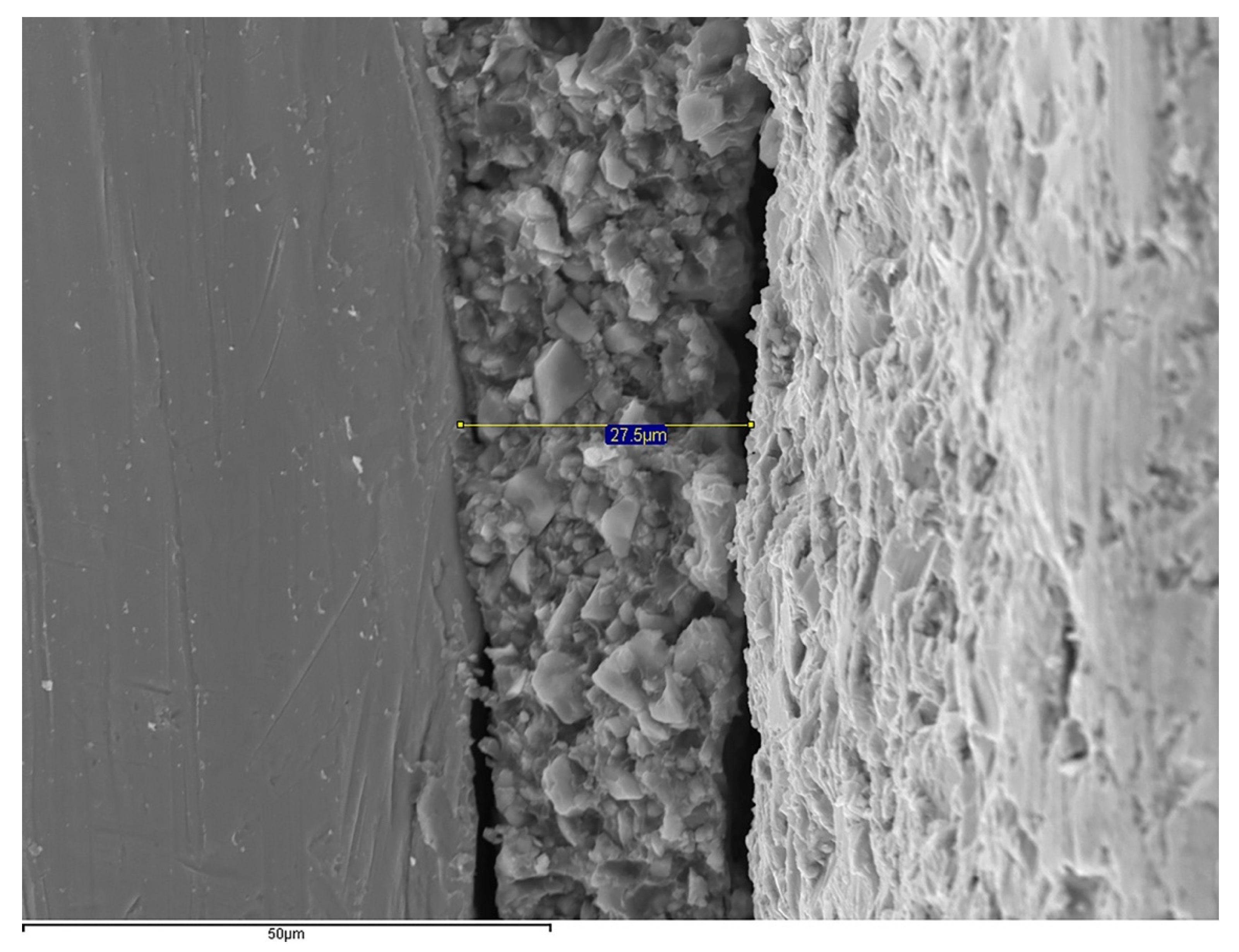
2.1. Experimental Model
2.2. Fabrication of the Restorations
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roberts, H.W.; Berzins, D.W.; Moore, B.K.; Charlton, D.G. Metal-ceramic alloys in dentistry: A review. J. Prosthodont. 2009, 18, 188–194. [Google Scholar] [CrossRef]
- Sailer, I.; Strasding, M.; Valente, N.A.; Zwahlen, M.; Liu, S.; Pjetursson, B.E. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic multiple-unit fixed dental prostheses. Clin. Oral. Implants. Res. 2018, 29, 184–198. [Google Scholar] [CrossRef]
- Ozcan, M. Fracture reasons in ceramic-fused-to-metal restorations. J. Oral Rehabil. 2003, 30, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Limones, A.; Molinero-Mourelle, P.; Azevedo, L.; Romeo-Rubio, M.; Correia, A.; Gomez-Polo, M. Zirconia-ceramic versus metal-ceramic posterior multiunit tooth-supported fixed dental prostheses: A systematic review and meta-analysis of randomized controlled trials. J. Am. Dent. Assoc. 2020, 151, 230–238e237. [Google Scholar] [CrossRef]
- Kelly, J.R.; Rose, T.C. Nonprecious alloys for use in fixed prosthodontics: A literature review. J. Prosthet. Dent. 1983, 49, 363–370. [Google Scholar] [CrossRef]
- Kane, L.M.; Chronaios, D.; Sierraalta, M.; George, F.M. Marginal and internal adaptation of milled cobalt-chromium copings. J. Prosthet. Dent. 2015, 114, 680–685. [Google Scholar] [CrossRef]
- Wataha, J.C. Alloys for prosthodontic restorations. J. Prosthet. Dent. 2002, 87, 351–363. [Google Scholar] [CrossRef]
- Li, K.C.; Prior, D.J.; Waddell, J.N.; Swain, M.V. Comparison of the microstructure and phase stability of as-cast, CAD/CAM and powder metallurgy manufactured Co–Cr dental alloys. Dent. Mater. 2015, 31, e306–e315. [Google Scholar] [CrossRef]
- Lucchetti, M.C.; Fratto, G.; Valeriani, F.; de Vittori, E.; Giampaoli, S.; Papetti, P.; Spica, V.R.; Manzon, L. Cobalt-chromium alloys in dentistry: An evaluation of metal ion release. J. Prosthet. Dent. 2015, 114, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Xin, X.Z.; Chen, J.; Xiang, N.; Gong, Y.; Wei, B. Surface characteristics and corrosion properties of selective laser melted Co–Cr dental alloy after porcelain firing. Dent. Mater. 2014, 30, 263–270. [Google Scholar] [CrossRef] [PubMed]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.B.; Kim, J.H.; Kim, W.C. Three-dimensional evaluation of gaps associated with fixed dental prostheses fabricated with new technologies. J. Prosthet. Dent. 2014, 112, 1432–1436. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 2011, 56, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Koutsoukis, T.; Zinelis, S.; Eliades, G.; Al-Wazzan, K.; Rifaiy, M.A.; Al Jabbari, Y.S. Selective Laser Melting Technique of Co–Cr Dental Alloys: A Review of Structure and Properties and Comparative Analysis with Other Available Techniques. J. Prosthodont. 2015, 24, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Nesse, H.; Ulstein, D.M.; Vaage, M.M.; Øilo, M. Internal and marginal fit of cobalt-chromium fixed dental prostheses fabricated with 3 different techniques. J. Prosthet. Dent. 2015, 114, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Oyague, R.; Lynch, C.D.; Turrion, A.S.; Lopez-Lozano, J.F.; Torres-Lagares, D.; Suarez-García, M.J. Misfit and microleakage of implant-supported crown copings obtained by laser sintering and casting techniques, luted with glass-ionomer, resin cements and acrylic/urethane-based agents. J. Dent. 2013, 41, 90–96. [Google Scholar] [CrossRef]
- Sundar, M.K.; Chikmagalur, S.B.; Pasha, F. Marginal fit and microleakage of cast and metal laser sintered copings—An in vitro study. J. Prosthodont. Res. 2014, 58, 252–258. [Google Scholar] [CrossRef]
- Traini, T.; Mangano, C.; Sammons, R.L.; Mangano, F.; Macchi, A.; Piattelli, A. Direct laser metal sintering as a new approach to fabrication of an isoelastic functionally graded material for manufacture of porous titanium dental implants. Dent. Mater. 2008, 24, 1525–1533. [Google Scholar] [CrossRef]
- Kim, K.B.; Kim, W.C.; Kim, H.Y.; Kim, J.H. An evaluation of marginal fit of three-unit fixed dental prostheses fabricated by direct metal laser sintering system. Dent. Mater. 2013, 29, e91–e96. [Google Scholar] [CrossRef]
- Ramfjord, S.P. Periodontal aspects of restorative dentistry. J. Oral Rehabil. 1974, 1, 107–126. [Google Scholar] [CrossRef] [PubMed]
- Goldman, M.; Laosonthorn, P.; White, R.R. Microleakage—Full crowns and the dental pulp. J. Endod. 1992, 18, 43–45. [Google Scholar] [CrossRef]
- Felton, D.A.; Kanoy, B.E.; Bayne, S.C.; Wirthman, G.P. Effect of in vivo crown margin discrepancies on periodontal health. J. Prosthet. Dent. 1991, 65, 357–364. [Google Scholar] [CrossRef]
- Piemjai, M. Effect of seating force, margin design, and cement on marginal seal and retention of complete metal crowns. Int. J. Prosthodont. 2001, 14, 412–416. [Google Scholar]
- Beuer, F.; Edelhoff, D.; Gernet, W.; Naumann, M. Effect of preparation angles on the precision of zirconia crown copings fabricated by CAD/CAM system. Dent. Mater. J. 2008, 27, 814–820. [Google Scholar] [CrossRef]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454.e10. [Google Scholar] [CrossRef] [PubMed]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.; Gonzalo, E.; Gomez-Polo, M.; Lopez-Suarez, C.; Suarez, M.J. SEM evaluation of the precision of fit of CAD/CAM zirconia and metal-ceramic posterior crowns. Dent. Mater. J. 2017, 36, 387–393. [Google Scholar] [CrossRef]
- Gonzalo, E.; Suárez, M.J.; Serrano, B.; Lozano, J.F. A comparison of the marginal vertical discrepancies of zirconium and metal ceramic posterior fixed dental prostheses before and after cementation. J. Prosthet. Dent. 2009, 102, 378–384. [Google Scholar] [CrossRef]
- Wolfart, S.; Wegner, S.M.; Al-Halabi, A.; Kern, M. Clinical evaluation of marginal fit of a new experimental all-ceramic system before and after cementation. Int. J. Prosthodont. 2003, 16, 587–592. [Google Scholar]
- Beschnidt, S.M.; Strub, J.R. Evaluation of the marginal accuracy of different all-ceramic crown systems after simulation in the artificial mouth. J. Oral Rehabil. 1999, 26, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Freire, Y.; Gonzalo, E.; Lopez-Suarez, C.; Suarez, M.J. The Marginal Fit of CAD/CAM Monolithic Ceramic and Metal-Ceramic Crowns. J. Prosthodont. 2019, 28, 299–304. [Google Scholar] [CrossRef] [PubMed]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Ortega, R.; Gonzalo, E.; Gomez-Polo, M.; Suárez, M.J. Marginal and Internal Discrepancies of Posterior Zirconia-Based Crowns Fabricated with Three Different CAD/CAM Systems Versus Metal-Ceramic. Int. J. Prosthodont. 2015, 28, 509–511. [Google Scholar] [CrossRef] [PubMed]
- Att, W.; Komine, F.; Gerds, T.; Strub, J.R. Marginal adaptation of three different zirconium dioxide three-unit fixed dental prostheses. J. Prosthet. Dent. 2009, 101, 239–247. [Google Scholar] [CrossRef]
- Suárez, M.J.; Lozano, J.F.; Salido, M.P.; Martínez, F. Marginal fit of titanium metal-ceramic crowns. Int. J. Prosthodont. 2005, 18, 390–391. [Google Scholar]
- Witkowski, S.; Komine, F.; Gerds, T. Marginal accuracy of titanium copings fabricated by casting and CAD/CAM techniques. J. Prosthet. Dent. 2006, 96, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Boitelle, P.; Mawussi, B.; Tapie, L.; Fromentin, O. A systematic review of CAD/CAM fit restoration evaluations. J. Oral Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef] [PubMed]
- Gonzalo, E.; Suárez, M.J.; Serrano, B.; Lozano, J.F. Comparative analysis of two measurement methods for marginal fit in metal-ceramic and zirconia posterior FPDs. Int. J. Prosthodont. 2009, 22, 374–377. [Google Scholar]
- Groten, M.; Axmann, D.; Pröbster, L.; Weber, H. Determination of the minimum number of marginal gap measurements required for practical in vitro testing. J. Prosthet. Dent. 2000, 83, 40–49. [Google Scholar] [CrossRef]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef]
- Marchionni, S.; Baldissara, P.; Monaco, C.; Scotti, R. A systematic method for predetermined scanning electron microscope analysis in dental science. Scanning 2010, 32, 97–103. [Google Scholar] [CrossRef]
- Quintas, A.F.; Oliveira, F.; Bottino, M.A. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: An in vitro evaluation. J. Prosthet. Dent. 2004, 92, 250–257. [Google Scholar] [CrossRef]
- Fransson, B.; Oilo, G.; Gjeitanger, R. The fit of metal-ceramic crowns, a clinical study. Dent. Mater. 1985, 1, 197–199. [Google Scholar] [CrossRef]
- Oyague, R.C.; Sanchez-Turrion, A.; Lopez-Lozano, J.F.; Suarez-Garcia, M.J. Vertical discrepancy and microleakage of laser-sintered and vacuum-cast implant-supported structures luted with different cement types. J. Dent. 2012, 40, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Castillo-de-Oyague, R.; Sanchez-Turrion, A.; Lopez-Lozano, J.F.; Albaladejo, A.; Torres-Lagares, D.; Montero, J.; Suarez-Garcia, M. Vertical misfit of laser-sintered and vacuum-cast implant-supported crown copings luted with definitive and temporary luting agents. Med. Oral Patol. Oral Cir. Bucal 2012, e610–e617. [Google Scholar] [CrossRef]
- Fathi, H.M.; Al-Masoody, A.H.; El-Ghezawi, N.; Johnson, A. The accuracy of fit of crowns made from wax patterns produced conventionally (hand formed) and via CAD/CAM technology. Eur. J. Prosthodont. Restor. Dent. 2016, 24, 10–17. [Google Scholar] [PubMed]
- Kim, K.B.; Kim, J.H.; Kim, W.C.; Kim, H.Y. Evaluation of the marginal and internal gap of metal-ceramic crown fabricated with a selective laser sintering technology: Two- and three-dimensional replica techniques. J. Adv. Prosthodont. 2013, 5, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Farjood, E.; Vojdani, M.; Torabi, K.; Khaledi, A.A. Marginal and internal fit of metal copings fabricated with rapid prototyping and conventional waxing. J. Prosthet. Dent. 2017, 117, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Karaman, T.; Ulku, S.Z.; Zengingul, A.I.; Guven, S.; Eratilla, V.; Sumer, E. Evaluation and comparison of the marginal adaptation of two different substructure materials. J. Adv. Prosthodont. 2015, 7, 257–263. [Google Scholar] [CrossRef]
- Hong, M.H.; Min, B.K.; Lee, D.H.; Kwon, T.Y. Marginal fit of metal-ceramic crowns fabricated by using a casting and two selective laser melting processes before and after ceramic firing. J. Prosthet. Dent. 2019, 122, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Zhang, L.; Zhu, J.; Zhang, X. Clinical marginal and internal fit of metal ceramic crowns fabricated with a selective laser melting technology. J. Prosthet. Dent. 2015, 113, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Xiang, N.; Wei, B. The marginal fit of selective laser melting-fabricated metal crowns: An in vitro study. J. Prosthet. Dent. 2014, 112, 1437–1440. [Google Scholar] [CrossRef]
- Afify, A.; Haney, S.; Verrett, R.; Mansueto, M.; Cray, J.; Johnson, R. Marginal discrepancy of noble metal-ceramic fixed dental prosthesis frameworks fabricated by conventional and digital technologies. J. Prosthet. Dent. 2018, 119, 307.e1–307.e7. [Google Scholar] [CrossRef]
- Tamac, E.; Toksavul, S.; Toman, M. Clinical marginal and internal adaptation of CAD/CAM milling, laser sintering, and cast metal ceramic crowns. J. Prosthet. Dent. 2014, 112, 909–913. [Google Scholar] [CrossRef] [PubMed]
- Lövgren, N.; Roxner, R.; Klemendz, S.; Larsson, C. Effect of production method on surface roughness, marginal and internal fit, and retention of cobalt-chromium single crowns. J. Prosthet. Dent. 2017, 118, 95–101. [Google Scholar] [CrossRef]
- Ortorp, A.; Jonsson, D.; Mouhsen, A.; von Steyern, P.V. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: A comparative in vitro study. Dent. Mater. 2011, 27, 356–363. [Google Scholar] [CrossRef]
- Kocaağaoğlu, H.; Kılınç, H.; Albayrak, H.; Kara, M. In vitro evaluation of marginal, axial, and occlusal discrepancies in metal ceramic restorations produced with new technologies. J. Prosthet. Dent. 2016, 116, 368–374. [Google Scholar] [CrossRef]
- Park, J.K.; Kim, H.Y.; Kim, W.C.; Kim, J.H. Evaluation of the fit of metal ceramic restorations fabricated with a pre-sintered soft alloy. J. Prosthet. Dent. 2016, 116, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Lee, D.H.; Kwon, S.M.; Kwon, T.Y. A microcomputed tomography evaluation of the marginal fit of cobalt-chromium alloy copings fabricated by new manufacturing techniques and alloy systems. J. Prosthet. Dent. 2017, 117, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Real-Voltas, F.; Romano-Cardozo, E.; Figueras-Alvarez, O.; Brufau-de Barbera, M.; Cabratosa-Termes, J. Comparison of the Marginal Fit of Cobalt-Chromium Metal-Ceramic Crowns Fabricated by CAD/CAM Techniques and Conventional Methods at Three Production Stages. Int. J. Prosthodont. 2017, 30, 304–305. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Lang, N.P. Prosthetic treatment planning on the basis of scientific evidence. J. Oral Rehabil. 2008, 35 (Suppl. S1), 72–79. [Google Scholar] [CrossRef]
- Henderson, D.; Blevins, W.R.; Wesley, R.C.; Seward, T. The cantilever type of posterior fixed partial dentures: A laboratory study. J. Prosthet. Dent. 1970, 24, 47–67. [Google Scholar] [CrossRef]
- Yang, H.S.; Chung, H.J.; Park, Y.J. Stress analysis of a cantilevered fixed partial denture with normal and reduced bone support. J. Prosthet. Dent. 1996, 76, 424–430. [Google Scholar] [CrossRef]
- Wolfart, S.; Harder, S.; Eschbach, S.; Lehmann, F.; Kern, M. Four-year clinical results of fixed dental prostheses with zirconia substructures (Cercon): End abutments vs. cantilever design. Eur. J. Oral. Sci. 2009, 117, 741–749. [Google Scholar] [CrossRef]
- Rehmann, P.; Podhorsky, A.; Wöstmann, B. Treatment Outcomes of Cantilever Fixed Partial Dentures on Vital Abutment Teeth: A Retrospective Analysis. Int. J. Prosthodont. 2015, 28, 577–582. [Google Scholar] [CrossRef]
- Palmqvist, S.; Swartz, B. Artificial crowns and fixed partial dentures 18 to 23 years after placement. Int. J. Prosthodont. 1993, 6, 279–285. [Google Scholar] [PubMed]
- Zenthöfer, A.; Ohlmann, B.; Rammelsberg, P.; Bömicke, W. Performance of zirconia ceramic cantilever fixed dental prostheses: 3-year results from a prospective, randomized, controlled pilot study. J. Prosthet. Dent. 2015, 114, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Quante, K.; Ludwig, K.; Kern, M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent. Mater. 2008, 24, 1311–1315. [Google Scholar] [CrossRef] [PubMed]
- Laurent, M.; Scheer, P.; Dejou, J.; Laborde, G. Clinical evaluation of the marginal fit of cast crowns—Validation of the silicone replica method. J. Oral Rehabil. 2008, 35, 116–122. [Google Scholar] [CrossRef]
- Mitchell, C.A.; Pintado, M.R.; Douglas, W.H. Nondestructive, in vitro quantification of crown margins. J. Prosthet. Dent. 2001, 85, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Coli, P.; Karlsson, S. Precision of a CAD/CAM technique for the production of zirconium dioxide copings. Int. J. Prosthodont. 2004, 17, 577–580. [Google Scholar] [CrossRef] [PubMed]
- Pimenta, M.A.; Frasca, L.C.; Lopes, R.; Rivaldo, E. Evaluation of marginal and internal fit of ceramic and metallic crown copings using X-ray microtomography (micro-CT) technology. J. Prosthet. Dent. 2015, 114, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Groten, M.; Girthofer, S.; Pröbster, L. Marginal fit consistency of copy-milled all-ceramic crowns during fabrication by light and scanning electron microscopic analysis in vitro. J. Oral Rehabil. 1997, 24, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Persson, A.; Andersson, M.; Oden, A.; Sandborgh-Englund, G. A three-dimensional evaluation of a laser scanner and a touch-probe scanner. J. Prosthet. Dent. 2006, 95, 194–200. [Google Scholar] [CrossRef] [PubMed]


| Manufacturing Technique | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group Code | Coping Alloys Brands and Manufacturers | Dental Alloy Composition (Weight %) | ||||||||||
| (1) Intermediate Pontic | (2) Cantilever Pontic | Co | Cr | Mo | W | Si | Fe | C | Mn | Ni | N | |
| CM | CMc | Super 8 (Dental Alloys Products, San Diego, CA, USA) | 59.5 | 31.5 | 5 | - | 2 | ≤1 | ≤1 | ≤1 | - | - |
| LS | LSc | ST2724G (Sint-Tech, Clermont-Ferrand, France) | 65 | 28–30 | 5–6 | - | ≤1 | ≤0.5 | ≤0.02 | ≤1 | ≤1 | - |
| SM | SMc | Ceramill® Sintron R 71 L (Amann Girrbach, Koblach, Austria) | 66 | 28 | 5 | - | ≤1 | ≤1 | ≤0.1 | ≤1 | - | - |
| HM | HMc | Starbond CoS DISC basic (Scheftner, Mainz, Germany) | 59 | 25 | 3.5 | 9.5 | 1 | ≤1.5 | ≤1.5 | ≤1.5 | - | ≤1.5 |
| Group 1 | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| CM | 40.11 | 10.43 | 26.90 | 53.90 |
| LS | 41.84 | 10.36 | 27.16 | 57.20 |
| SM | 39.78 | 8.77 | 24.24 | 53.10 |
| HM | 38.67 | 18.27 | 22.83 | 80.01 |
| Group 2 | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| CMc | 34.55 | 6.93 | 26.94 | 50.71 |
| LSc | 35.22 | 10.60 | 26.17 | 62.42 |
| SMc | 40.81 | 5.55 | 32.18 | 49.21 |
| HMc | 34.17 | 15.85 | 19.63 | 71.69 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobar, C.; Rodríguez, V.; Lopez-Suarez, C.; Peláez, J.; Brinckmann, J.C.-B.; Suárez, M.J. Effect of Digital Technologies on the Marginal Accuracy of Conventional and Cantilever Co–Cr Posterior-Fixed Partial Dentures Frameworks. Appl. Sci. 2021, 11, 2988. https://doi.org/10.3390/app11072988
Tobar C, Rodríguez V, Lopez-Suarez C, Peláez J, Brinckmann JC-B, Suárez MJ. Effect of Digital Technologies on the Marginal Accuracy of Conventional and Cantilever Co–Cr Posterior-Fixed Partial Dentures Frameworks. Applied Sciences. 2021; 11(7):2988. https://doi.org/10.3390/app11072988
Chicago/Turabian StyleTobar, Celia, Verónica Rodríguez, Carlos Lopez-Suarez, Jesús Peláez, Jorge Cortés-Bretón Brinckmann, and María J. Suárez. 2021. "Effect of Digital Technologies on the Marginal Accuracy of Conventional and Cantilever Co–Cr Posterior-Fixed Partial Dentures Frameworks" Applied Sciences 11, no. 7: 2988. https://doi.org/10.3390/app11072988
APA StyleTobar, C., Rodríguez, V., Lopez-Suarez, C., Peláez, J., Brinckmann, J. C.-B., & Suárez, M. J. (2021). Effect of Digital Technologies on the Marginal Accuracy of Conventional and Cantilever Co–Cr Posterior-Fixed Partial Dentures Frameworks. Applied Sciences, 11(7), 2988. https://doi.org/10.3390/app11072988







