Evaluation of Ultrasound Accuracy in Acute Appendicitis Diagnosis
Abstract
1. Introduction
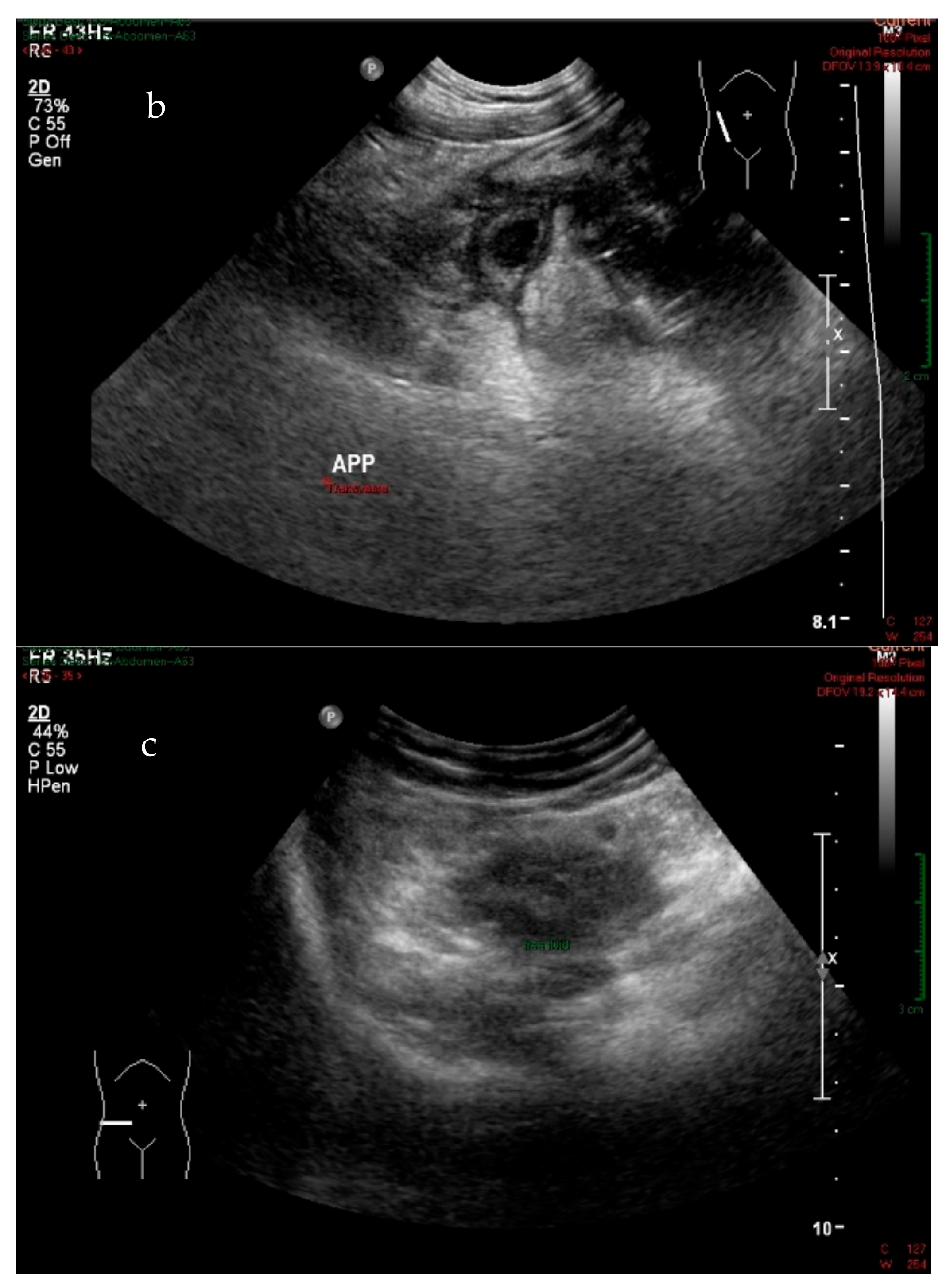
2. Materials and Methods
2.1. Patients
2.2. Medical Staff
2.3. US Procedure
2.4. Histopathological Results
2.5. Data Analysis
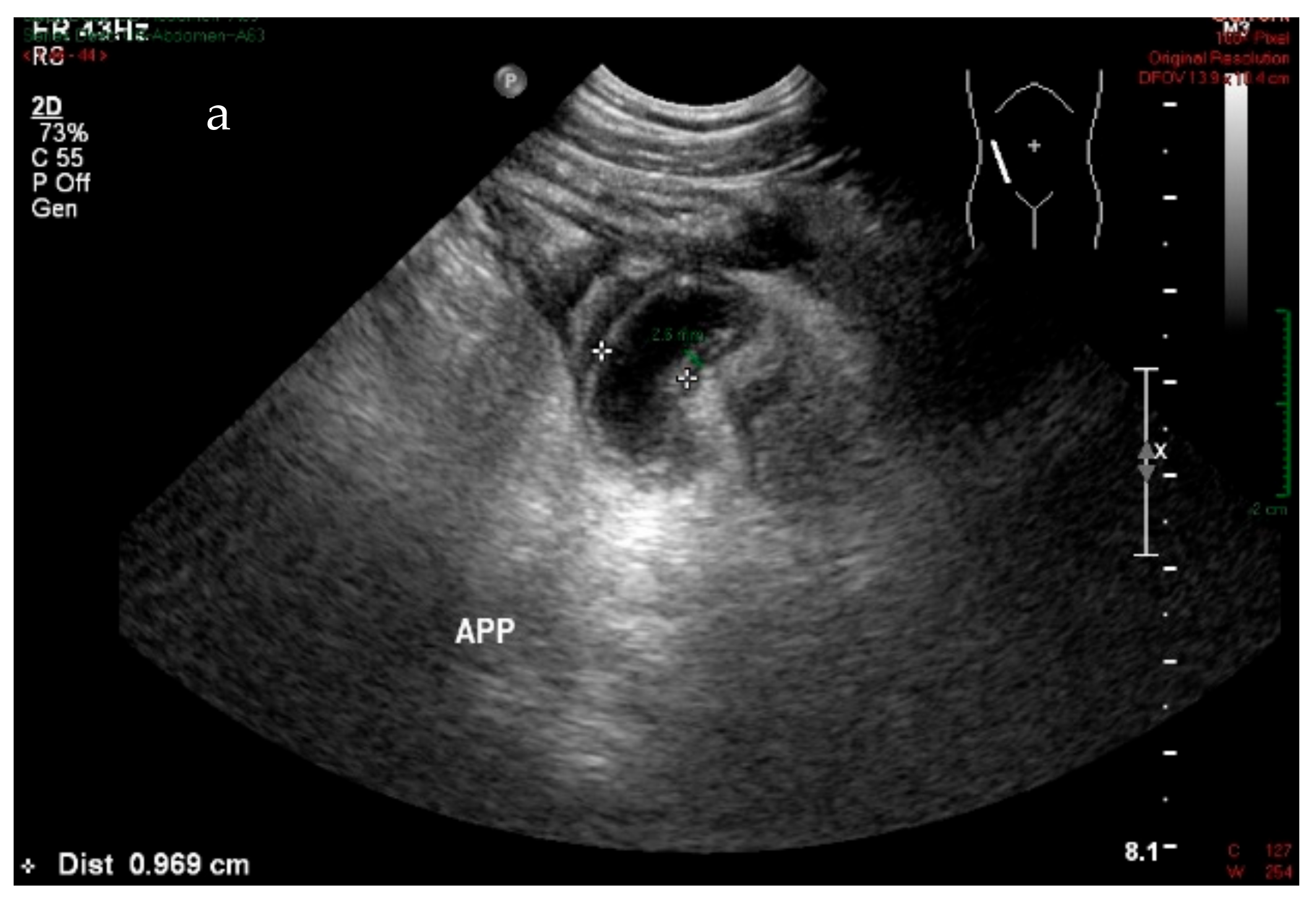
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Omari, A.H.; Khammash, M.R.; Qasaimeh, G.R.; Shammari, A.K.; Yaseen, M.K.B.; Hammori, S.K. Acute appendicitis in the elderly: risk factors for perforation. World J. Emerg. Surg. 2014, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Storm-Dickerson, T.L.; Horattas, M.C. What have we learned over the past 20 years about appendicitis in the elderly? Am. J. Surg. 2003, 185, 198–201. [Google Scholar] [CrossRef]
- Vriesman, A.C.V.B.; Puylaert, J.B.C.M. Mimics of Appendicitis: Alternative Nonsurgical Diagnoses with Sonography and CT. Am. J. Roentgenol. 2006, 186, 1103–1112. [Google Scholar] [CrossRef]
- Cobben, L.P.; Groot, I.; Haans, L.; Blickman, J.G.; Puylaert, J. MRI for Clinically Suspected Appendicitis During Pregnancy. Am. J. Roentgenol. 2004, 183, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Wagner, P.L.; Eachempati, S.R.; Soe, K.; Pieracci, F.M.; Shou, J.; Barie, P.S. Defining the current negative appendectomy rate: For whom is preoperative computed tomography making an impact? Surgery 2008, 144, 276–282. [Google Scholar] [CrossRef]
- Von Titte, S.N.; McCabe, C.J.; Ottinger, L.W. Delayed appendectomy for appendicitis: Causes and consequences. Am. J. Emerg. Med. 1996, 14, 620–622. [Google Scholar] [CrossRef]
- Birnbaum, B.A.; Wilson, S.R. Appendicitis at the Millennium. Radiology 2000, 215, 337–348. [Google Scholar] [CrossRef]
- Keyzer, C.; Zalcman, M.; De Maertelaer, V.; Coppens, E.; Bali, M.-A.; Gevenois, P.A.; Van Gansbeke, D. Comparison of US and Unenhanced Multi–Detector Row CT in Patients Suspected of having Acute Appendicitis 1. Radiology 2005, 236, 527–534. [Google Scholar] [CrossRef]
- Townsend, C.M., Jr.; Beauchamp, R.D.; Evers, B.M.; Mattox, K.L. (Eds.) Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 20th ed.; Elsevier: Philadelphia, PA, USA, 2016. [Google Scholar]
- Neumayer, L. Imaging in appendicitis: a review with special emphasis on the treatment of women. Obstet. Gynecol. 2003, 102, 1404–1409. [Google Scholar] [CrossRef]
- Larson, D.B.; Rader, S.B.; Forman, H.P.; Fenton, L.Z. Informing Parents About CT Radiation Exposure in Children: It’s OK to Tell Them. Am. J. Roentgenol. 2007, 189, 271–275. [Google Scholar] [CrossRef]
- Memon, A.A.; Vohra, L.M.; Khaliq, T.; Lehri, A.A. Diagnostic Accuracy of Alvarado Score in the Diagnosis of acute Appendicitis. Pak. J. Med. Sci. 2009, 25, 118–121. [Google Scholar]
- Khan, U.; Kitar, M.; Krichen, I.; Maazoun, K.; Althobaiti, R.A.; Khalif, M.; Adwani, M. To determine validity of ultrasound in predicting acute appendicitis among children keeping histopathology as gold standard. Ann. Med. Surg. 2019, 38, 22–27. [Google Scholar] [CrossRef]
- Marin, J.R.; Lewiss, R.E.; Ultrasound, W.I.N.F.O.C. Point-of-Care Ultrasonography by Pediatric Emergency Medicine Physicians. Pediatr. 2015, 135, e1113–e1122. [Google Scholar] [CrossRef] [PubMed]
- Russell, W.S.; Schuh, A.M.; Hill, J.G.; Hebra, A.; Cina, R.A.; Smith, C.D.; Streck, C.J. Clinical Practice Guidelines for Pediatric Appendicitis Evaluation Can Decrease Computed Tomography Utilization While Maintaining Diagnostic Accuracy. Pediatric Emerg. Care 2013, 29, 568–573. [Google Scholar] [CrossRef] [PubMed]
- Izbicki, J.R.; Wilker, D.K.; Mandelkow, H.K.; Müller, K.; Siebeck, M.; Geissler, K.; Schweiberer, L. Retro- and prospective studies on the value of clinical and laboratory chemical data in acute appendicitis. Chir. Z. Alle Geb. Oper. Medizen 1990, 61, 887–893. [Google Scholar]
- Pinto, F.; Pinto, A.; Russo, A.; Coppolino, F.; Bracale, R.; Fonio, P.; Macarini, L.; Giganti, M. Accuracy of ultrasonography in the diagnosis of acute appendicitis in adult patients: review of the literature. Crit. Ultrasound J. 2013, 5, S2. [Google Scholar] [CrossRef]
- Giljaca, V.; Nadarevic, T.; Poropat, G.; Nadarevic, V.S.; Stimac, D. Diagnostic Accuracy of Abdominal Ultrasound for Diagnosis of Acute Appendicitis: Systematic Review and Meta-analysis. World J. Surg. 2016, 41, 693–700. [Google Scholar] [CrossRef]
- Puylaert, J.B.; Rutgers, P.H.; Lalisang, R.I.; De Vries, B.C.; Van Der Werf, S.D.; Dörr, J.P.; Blok, R.A. A Prospective Study of Ultrasonography in the Diagnosis of Appendicitis. N. Engl. J. Med. 1987, 317, 666–669. [Google Scholar] [CrossRef]
- D’Souza, N.; Grant, D.; Royston, E.; Farouk, M. The value of ultrasonography in the diagnosis of appendicitis. Int. J. Surg. 2015, 13, 165–169. [Google Scholar] [CrossRef]
- Lee, S.L.; Walsh, A.J.; Ho, H.S. Computed Tomography and Ultrasonography Do Not Improve and May Delay the Diagnosis and Treatment of Acute Appendicitis. Arch. Surg. 2001, 136, 556–562. [Google Scholar] [CrossRef]
- Lorusso, F.; Fonio, P.; Scardapane, A.; Giganti, M.; Rubini, G.; Ferrante, A.; Ianora, A.A.S. Gatrointestinal imaging with multidetector CT and MRI. Recenti Prog. Med. 2012, 103, 493–499. [Google Scholar] [PubMed]
- Summa, M.; Perrone, F.; Priora, F.; Testa, S.; Quarati, R.; Spinoglio, G. Integrated clinical-ultrasonographic diagnosis in acute appendicitis. J. Ultrasound 2007, 10, 175–178. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Al-Ajerami, Y. Sensitivity and specificity of ultrasound in the diagnosis of acute appendicitis. East. Mediterr. Health J. 2012, 18, 66–69. [Google Scholar] [CrossRef]
- Hussain, S.; Rahman, A.; Abbasi, T.; Aziz, T. Diagnostic accuracy of ultrasonography in acute appendicitis. J. Ayub Med Coll. Abbottabad JAMC 2014, 26, 12–17. [Google Scholar]
- Brown, M.A. Imaging Acute Appendicitis. Semin. Ultrasound CT MRI 2008, 29, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H. Sonography of acute appendicitis. Semin. Ultrasound CT MRI 2003, 24, 83–90. [Google Scholar] [CrossRef]
- Schuh, S.; Man, C.; Cheng, A.; Murphy, A.; Mohanta, A.; Moineddin, R.; Tomlinson, G.; Langer, J.C.; Doria, A.S. Predictors of Non-Diagnostic Ultrasound Scanning in Children with Suspected Appendicitis. J. Pediatrics 2011, 158, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Paulson, E.K.; Kalady, M.F.; Pappas, T.N. Suspected Appendicitis. N. Engl. J. Med. 2003, 348, 236–242. [Google Scholar] [CrossRef]
- Gilmore, O.; Browett, J.; Griffin, P.; Ross, I.; Brodribb, A.; Cooke, T.; Higgs, M.; Williamson, R. APPENDICITIS AND MIMICKING CONDITIONS. Lancet 1975, 306, 421–424. [Google Scholar] [CrossRef]
- Douglas, C.D.; E Macpherson, N.; Davidson, P.M.; Gani, J.S. Randomised controlled trial of ultrasonography in diagnosis of acute appendicitis, incorporating the Alvarado score. BMJ 2000, 321, 919. [Google Scholar] [CrossRef]
- Hanafi, M.G.; Shiri, A. Retracted Article: Diagnostic Accuracy of Acute Appendicitis by Ultrasound in Hospital Emergency. Jentashapir J. Heal. Res. 2018, 9, 8787–8793. [Google Scholar] [CrossRef]
- Van Randen, A.; Laméris, W.; Van Es, H.W.; Van Heesewijk, H.P.M.; Van Ramshorst, B.; Hove, W.T.; Bouma, W.H.; Van Leeuwen, M.S.; Van Keulen, E.M.; Bossuyt, B.M.; et al. A comparison of the Accuracy of Ultrasound and Computed Tomography in common diagnoses causing acute abdominal pain. Eur. Radiol. 2011, 21, 1535–1545. [Google Scholar] [CrossRef] [PubMed]
| Number of Patients (%) | Number of Accurate Diagnosis (%) | |
|---|---|---|
| Sex | ||
| Male | 48 (36.4%) | 20 (32.8%) |
| Female | 84 (63.6%) | 41 (67.2%) |
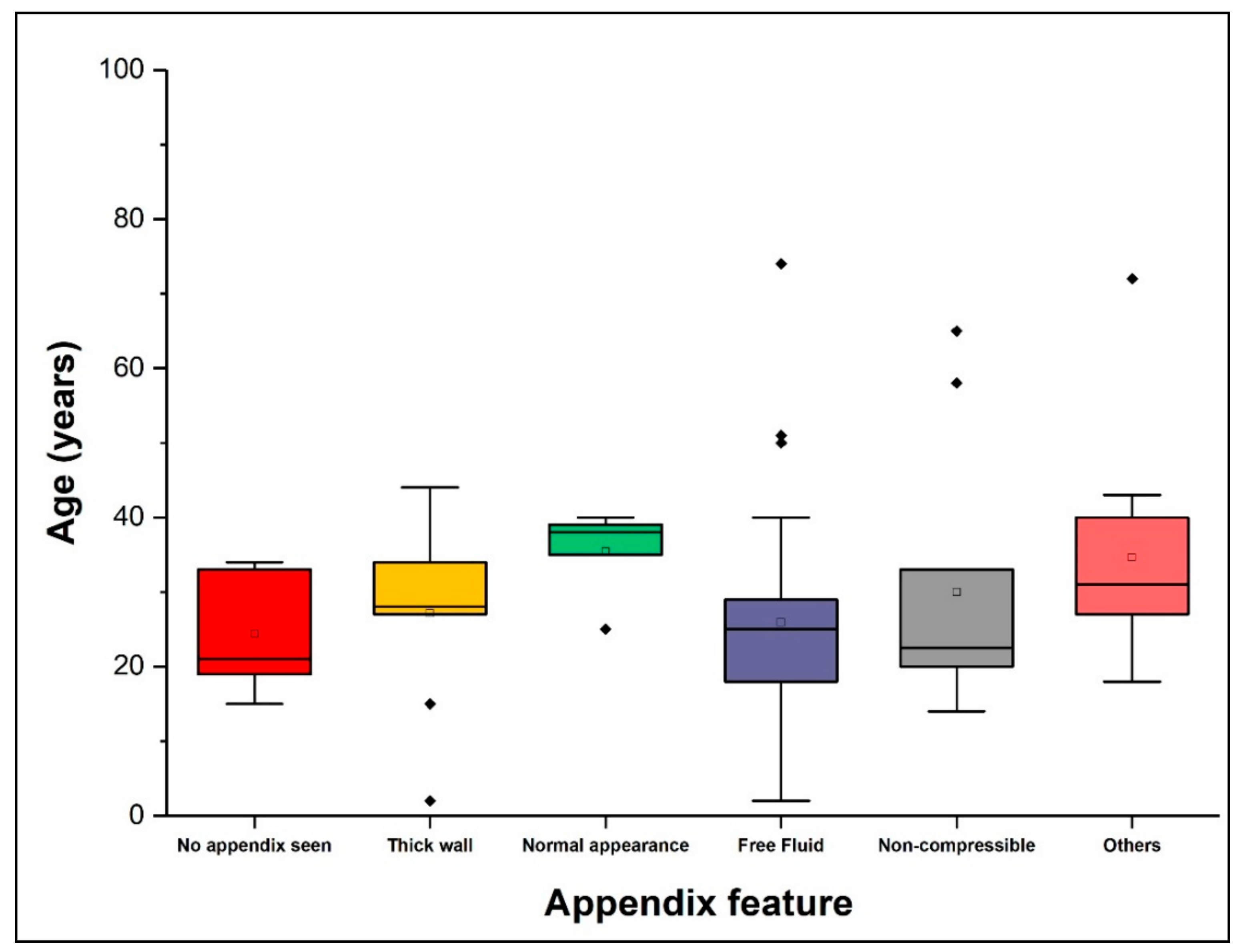
| Age range | ||
| 1–20 | 37 (28%) | 18 (48.6%) |
| 21–40 | 79 (59.8%) | 36 (47.4%) |
| 41–60 | 7 (5.3%) | 4 (50%) |
| 61–80 | 7 (5.3%) | 1 (14.3%) |
| 81–100 | 1 (0.76%) | 0 (0.0%) |
| Experience | Sensitivity (%) | Specificity (%) |
|---|---|---|
| <10 years | 36% | 83.3% |
| 10–19 years | 31% | 89% |
| >20 years | 52% | 100% |
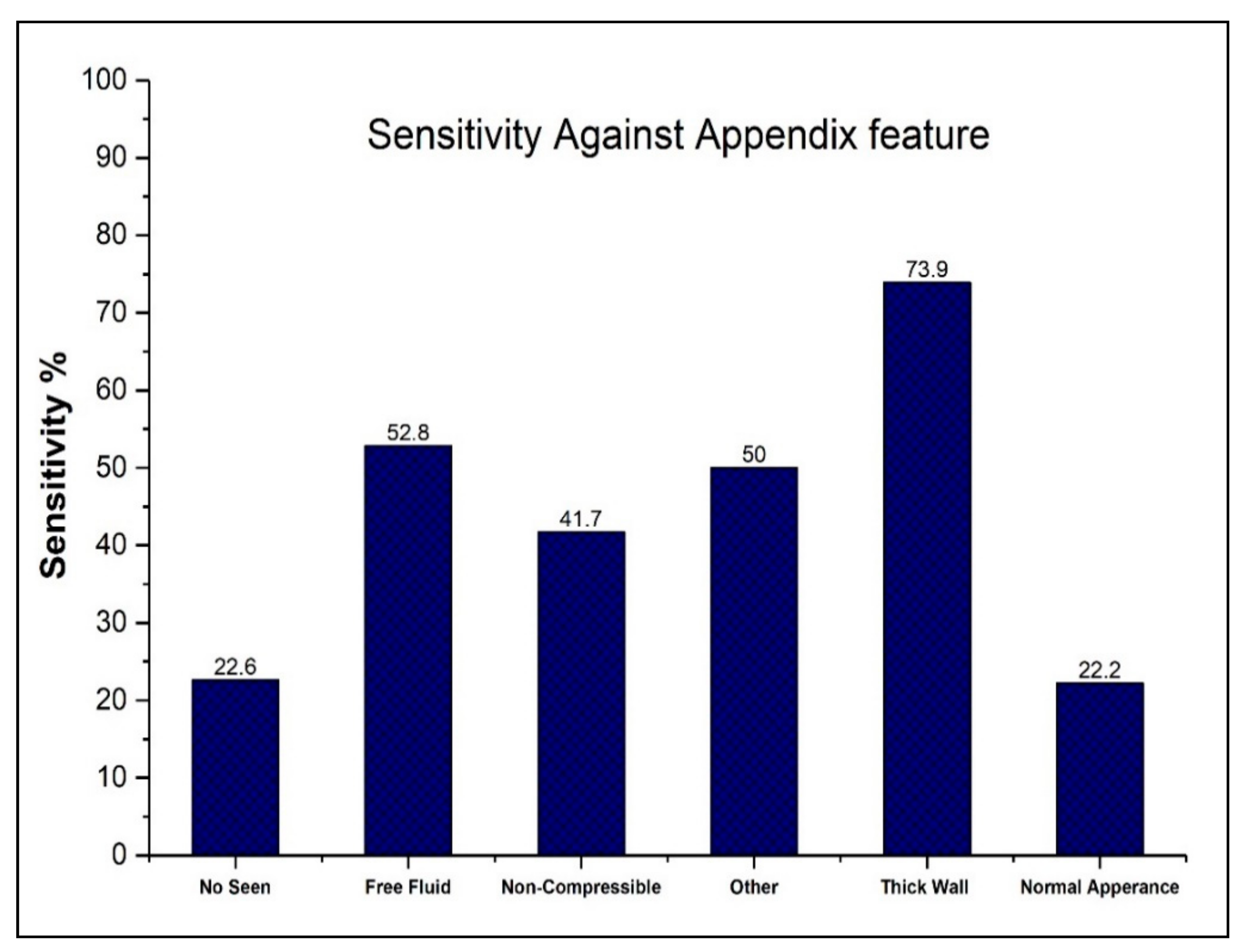
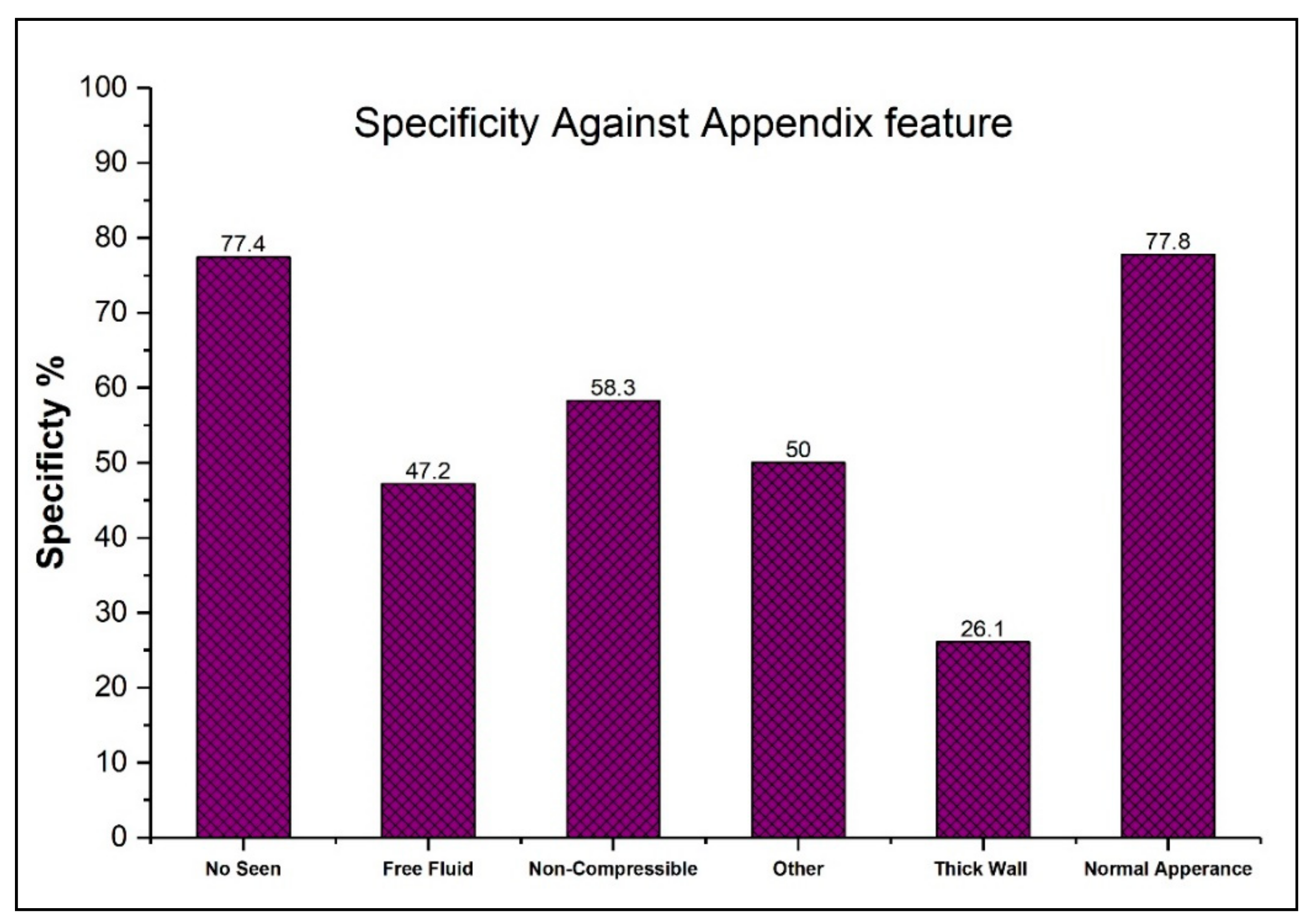
| Imaging Feature | Accurate (N = 61) | Missed (N = 71) |
|---|---|---|
| Diameter ≥ 7 mm | 17 | 6 |
| Free fluid | 28 | 25 |
| Lack of compressibility | 5 | 7 |
| No appendix seen | 7 | 24 |
| Normal appearance | 2 | 7 |
| Other | 2 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alelyani, M.; Hadadi, I.; Shubayr, N.; Alashban, Y.; Alqahtani, M.; Adam, M.; Almater, H.; Alamri, S. Evaluation of Ultrasound Accuracy in Acute Appendicitis Diagnosis. Appl. Sci. 2021, 11, 2682. https://doi.org/10.3390/app11062682
Alelyani M, Hadadi I, Shubayr N, Alashban Y, Alqahtani M, Adam M, Almater H, Alamri S. Evaluation of Ultrasound Accuracy in Acute Appendicitis Diagnosis. Applied Sciences. 2021; 11(6):2682. https://doi.org/10.3390/app11062682
Chicago/Turabian StyleAlelyani, Magbool, Ibrahim Hadadi, Nasser Shubayr, Yazeed Alashban, Mohammed Alqahtani, Mohamed Adam, Hajar Almater, and Sultan Alamri. 2021. "Evaluation of Ultrasound Accuracy in Acute Appendicitis Diagnosis" Applied Sciences 11, no. 6: 2682. https://doi.org/10.3390/app11062682
APA StyleAlelyani, M., Hadadi, I., Shubayr, N., Alashban, Y., Alqahtani, M., Adam, M., Almater, H., & Alamri, S. (2021). Evaluation of Ultrasound Accuracy in Acute Appendicitis Diagnosis. Applied Sciences, 11(6), 2682. https://doi.org/10.3390/app11062682






