Decision Support for Removing Fractured Endodontic Instruments: A Patient-Specific Approach
Abstract
Featured Application
Abstract
1. Introduction
2. Case Report
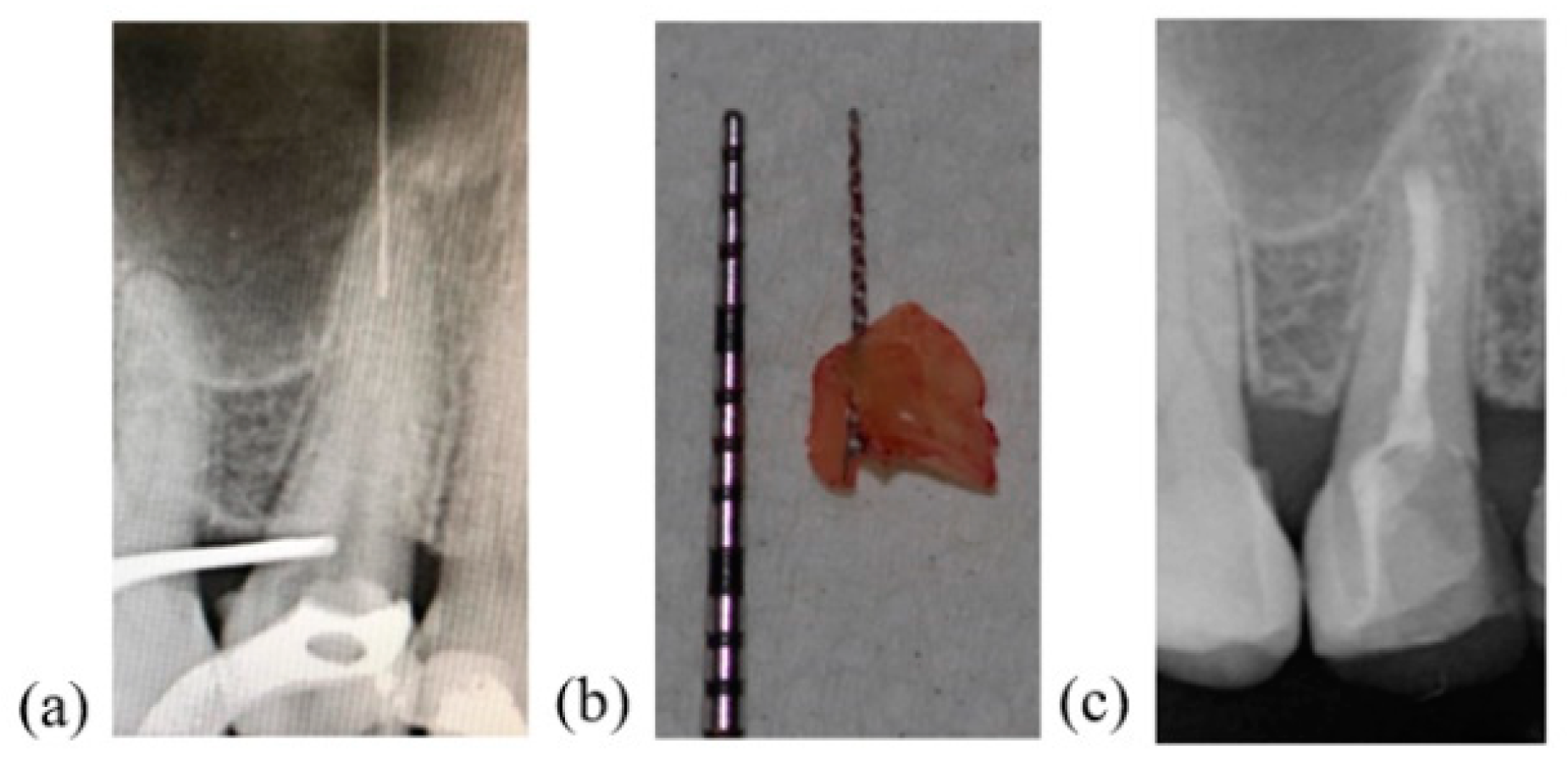
2.1. Case Presentation
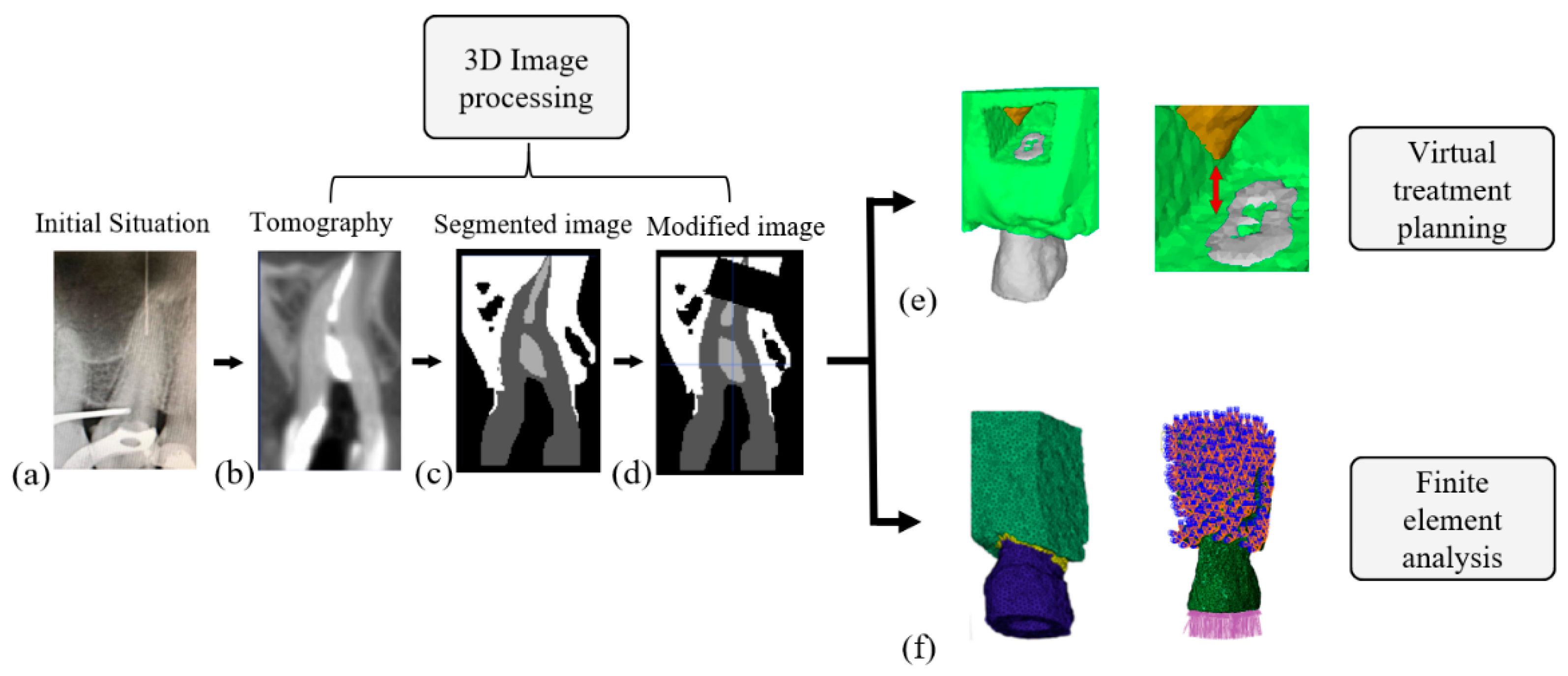
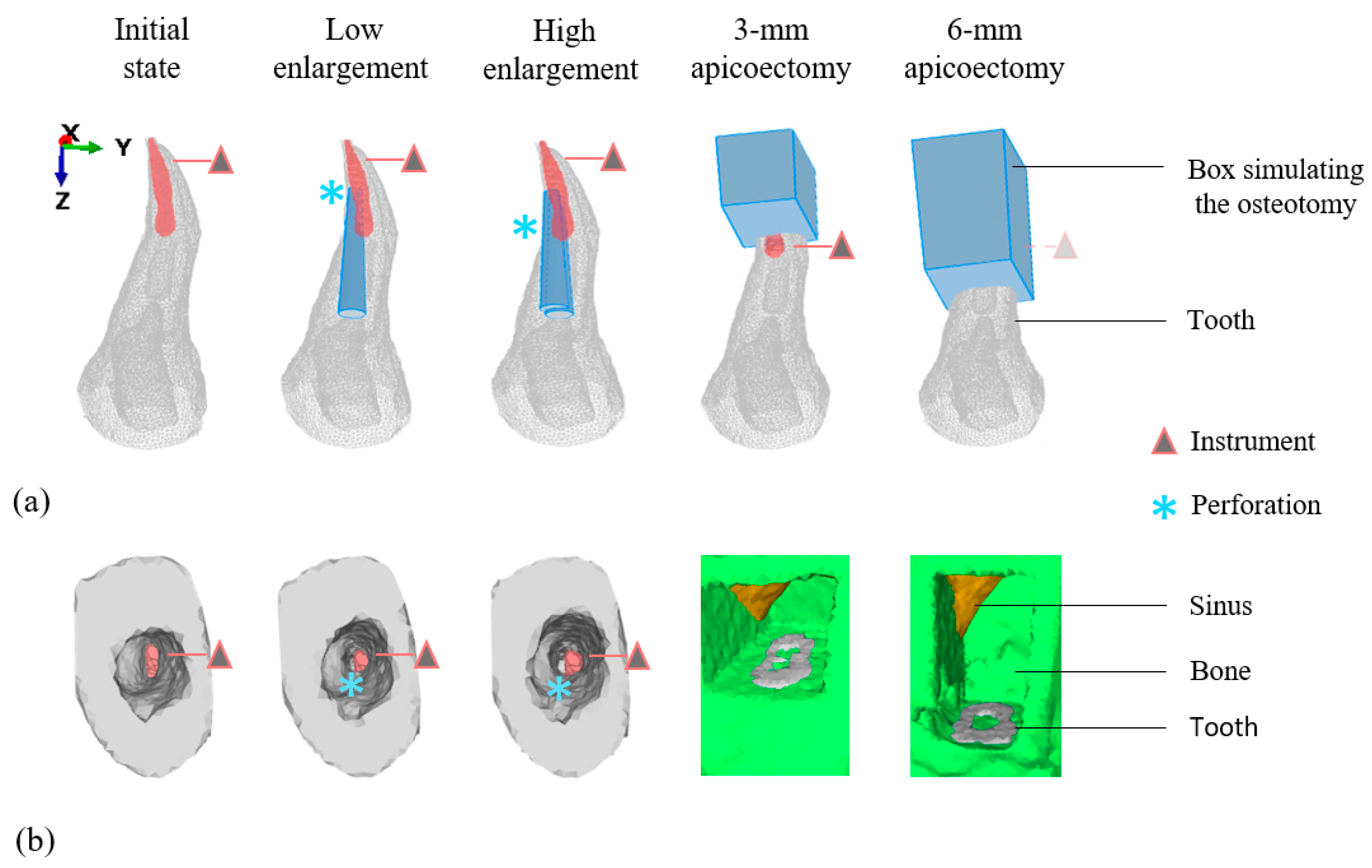
2.2. Virtual Treatment Planning
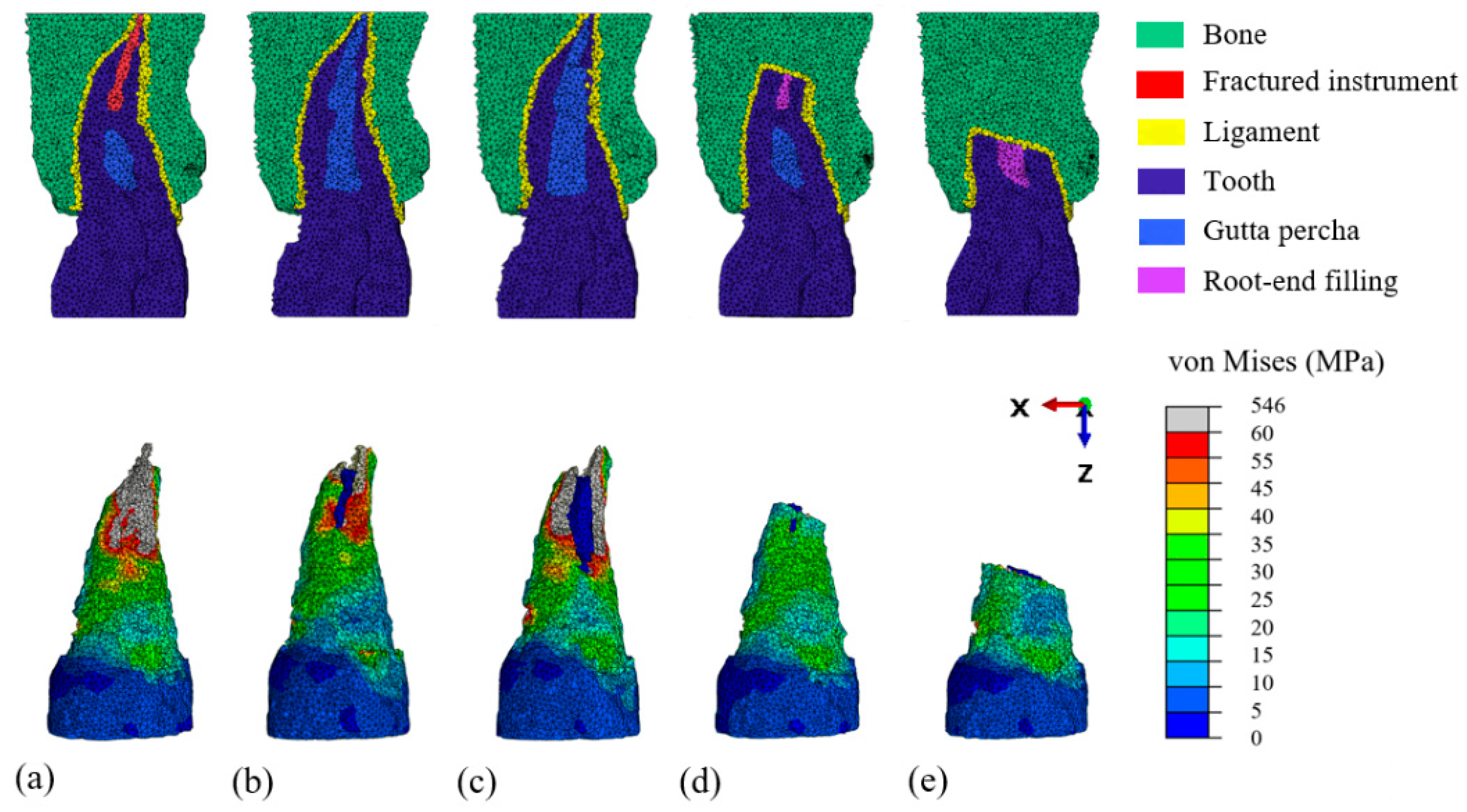
2.3. Finite Element Modeling and Mechanical Analysis
2.4. Management of the Fractured Instrument
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Madarati, A.A.; Hunter, M.J.; Dummer, P.M.H. Management of intracanal separated instruments. J. Endod. 2013, 39, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.K.; Kohli, M.R.; Kim, J.S. A retrospective clinical study of incidence of root canal instrument separation in an endodontics graduate program: A PennEndo database study. J. Endod. 2006, 32, 1048–1052. [Google Scholar] [CrossRef]
- Tzanetakis, G.N.; Kontakiotis, E.G.; Maurikou, D.V.; Marzelou, M.P. Prevalence and management of instrument fracture in the postgraduate endodontic program at the Dental School of Athens: A five-year retrospective clinical study. J. Endod. 2008, 34, 675–678. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, M.B.; Louca, C.; Duncan, H.F. Clinical decision-making after endodontic instrument fracture. Br. Dent. J 2013, 214, 395–400. [Google Scholar] [CrossRef]
- Panitvisai, P.; Parunnit, P.; Sathorn, C.; Messer, H.H. Impact of a retained instrument on treatment outcome: A systematic review and meta-analysis. J. Endod. 2010, 36, 775–780. [Google Scholar] [CrossRef]
- Suter, B.; Lussi, A.; Sequeira, P. Probability of removing fractured instruments from root canals. Int. Endod. J. 2005, 38, 112–123. [Google Scholar] [CrossRef]
- Setzer, F.C.; Shah, S.B.; Kohli, M.R.; Karabucak, B.; Kim, S. Outcome of endodontic surgery: A meta-analysis of the literature-part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J. Endod. 2010, 36, 1757–1765. [Google Scholar] [CrossRef]
- Von Arx, T.; Jensen, S.; Bornstein, M. Changes of root length and root-to-crown ratio after apical surgery: An analysis by using cone-beam computed tomography. J. Endod. 2015, 41, 1424–1429. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.; Hong, H.T.; Roh, B.D.; Chun, H.J. Influence of apical root resection on the biomechanical response of a single-rooted tooth: A 3-dimensional finite element analysis. J. Endod. 2014, 40, 1489–1493. [Google Scholar] [CrossRef] [PubMed]
- Schestatsky, R.; Dartora, G.; Felberg, R.; Spazzin, A.O.; Sarkis-Onofre, R.; Bacchi, A.; Pereira, G.K.R. Do endodontic retreatment techniques influence the fracture strength of endodontically treated teeth? A systematic review and meta-analysis. J. Mech. Behav. Biomed. Mater. 2019, 90, 306–312. [Google Scholar] [CrossRef]
- Soares, C.J.; Rodrigues, M.P.; Faria-E-Silva, A.L.; Santos-Filho, P.C.F.; Veríssimo, C.; Kim, H.C.; Versluis, A. How biomechanics can affect the endodontic treated teeth and their restorative procedures? Braz. Oral Res. 2018, 32, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Rodby, K.A.; Turin, S.; Jacobs, R.J.; Cruz, J.F.; Hassid, V.J.; Kolokythas, A.; Antony, A.K. Advances in oncologic head and neck reconstruction: Systematic review and future considerations of virtual surgical planning and computer aided design/computer aided modeling. J. Plast. Reconstr. Aesthetic Surg. 2014, 67, 1171–1185. [Google Scholar] [CrossRef]
- Tang, N.S.J.; Ahmadi, I.; Ramakrishnan, A. Virtual surgical planning in fibula free flap head and neck reconstruction: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1465–1477. [Google Scholar] [CrossRef]
- Eggermont, F.; van der Wal, G.; Westhoff, P.; Laar, A.; de Jong, M.; Rozema, T.; Kroon, H.M.; Ayu, O.; Derikx, L.; Dijkstra, S.; et al. Patient-specific finite element computer models improve fracture risk assessments in cancer patients with femoral bone metastases compared to clinical guidelines. Bone 2020, 130, 115101. [Google Scholar] [CrossRef]
- Ni, N.; Ye, J.; Wang, L.; Shen, S.; Han, L.; Wang, Y. Stress distribution in a mandibular premolar after separated nickel-titanium instrument removal and root canal preparation: A three-dimensional finite element analysis. J. Int. Med. Res. 2019, 47, 1555–1564. [Google Scholar] [CrossRef]
- Kim, S.; Park, S.Y.; Lee, Y.; Lee, C.J.; Karabucak, B.; Kim, H.C.; Kim, E. Stress analyses of retrograde cavity preparation designs for surgical endodontics in the mesial root of the mandibular molar: A finite element analysis; Part I. J. Endod. 2019, 45, 442–446. [Google Scholar] [CrossRef]
- Gümrükçü, Z.; Kurt, S.; Köse, S. Effect of root resection length and graft type used after apical resection: A finite element study. J. Oral Maxillofac. Surg. 2019, 77, 1770.e1–1770.e8. [Google Scholar] [CrossRef] [PubMed]
- Nevares, G.; Cunha, R.S.; Zuolo, M.; da Silveira Bueno, C.E. Success rates for removing or bypassing fractured instruments: A prospective clinical study. J. Endod. 2012, 38, 442–444. [Google Scholar] [CrossRef] [PubMed]
- Beldie, L.; Walker, B.; Lu, Y.; Richmond, S.; Middleton, J. Finite element modelling of maxillofacial surgery and facial expressions—A preliminary study. Int. J. Med. Robot. Comput. Assist. Surg. 2010, 6, 422–430. [Google Scholar] [CrossRef]
- Jacinto, H.; Kéchichian, R.; Desvignes, M.; Prost, R.; Valette, S. A web interface for 3D visualization and interactive segmentation of medical images. In Proceedings of the 17th International Conference on 3D Web Technology, Los Angeles, CA, USA, 4–5 August 2012; Volume 17, pp. 51–58. [Google Scholar]
- Chang, Y.H.; Lee, H.; Lin, C.L. Early resin luting material damage around a circular fiber post in a root canal treated premolar by using micro-computerized tomographic and finite element sub-modeling analyses. J. Mech. Behav. Biomed. Mater. 2015, 51, 184–193. [Google Scholar] [CrossRef]
- Thompson, S.A. An overview of nickel—Titanium alloys used in dentistry. Int. Endod. J. 2000, 33, 297–310. [Google Scholar] [CrossRef]
- Hondrum, S.O. Temporary dental restorative materials for military field use. Mil. Med. 1998, 163, 381–385. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Juloski, J.; Apicella, D.; Ferrari, M. The effect of ferrule height on stress distribution within a tooth restored with fibre posts and ceramic crown: A finite element analysis. Dent. Mater. 2014, 30, 1304–1315. [Google Scholar] [CrossRef] [PubMed]
- Erdemir, A.; Guess, T.M.; Halloran, J.; Tadepalli, S.C.; Morrison, T.M. Considerations for reporting finite element analysis studies in biomechanics. J. Biomech. 2012, 45, 625–633. [Google Scholar] [CrossRef]
- Zhu, J.Z.; Zienkiewicz, O.C. A posteriori error estimation and three-dimensional automatic mesh generation. Finite Elem. Anal. Des. 1997, 25, 167–184. [Google Scholar] [CrossRef]
- Fischer, A.; Eidel, B. Convergence and Error Analysis of FE-HMM/FE for energetically consistent micro-coupling conditions in linear elastic solids. Eur. J. Mech. A/Solids 2019, 77, 103735. [Google Scholar] [CrossRef]
- Fischer, A.; Eidel, B. Error analysis for quadtree-type mesh coarsening algorithms adapted to pixelized heterogeneous microstructures. Comput. Mech. 2020, 65, 1467–1491. [Google Scholar] [CrossRef]
- Hauman, C.H.J.; Chandler, N.P.; Tong, D.C. Endodontic implications of the maxillary sinus: A review. Int. Endod. J. 2002, 35, 127–141. [Google Scholar] [CrossRef]
- Scarfe, W.C.; Levin, M.D.; Gane, D.; Farman, A.G. Use of cone beam computed tomography in endodontics. Int. J. Dent. 2009, 2009, 634567. [Google Scholar] [CrossRef]
- Parashos, P.; Messer, H.H. Rotary NiTi instrument fracture and its consequences. J. Endod. 2006, 32, 1031–1043. [Google Scholar] [CrossRef]
- Gambarini, G.; Galli, M.; Stefanelli, L.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, F.; Testarelli, L. Endodontic microsurgery using dynamic navigation system: A case report. J. Endod. 2019, 45, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Zubizarreta-macho, Á.; De Pedro, M.A.; Deglow, E.; Agustín-Panadero, R.; Mena Álvarez, J. Accuracy of computer-aided dynamic navigation compared to computer-aided static procedure for endodontic access cavities: An in vitro study 2020. J. Clin. Med. 2020, 1, 2–9. [Google Scholar]
- Herford, A.S.; Miller, M.; Lauritano, F.; Cervino, G.; Signorino, F.; Maiorana, C. The use of virtual surgical planning and navigation in the treatment of orbital trauma. Chin. J. Traumatol. 2017, 20, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Giacomino, C.M.; Ray, J.J.; Wealleans, J.A. Targeted Endodontic Microsurgery: A Novel Approach to Anatomically Challenging Scenarios Using 3-dimensional—Printed Guides and Trephine Burs—A Report of 3 Cases. J. Endod. 2018, 44, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Palma, P.J.; Marques, J.A.; Casau, M.; Santos, A.; Caramelo, F.; Falacho, R.I.; Santos, J.M. Evaluation of Root-End Preparation with Two Different Endodontic Microsurgery Ultrasonic Tips. Biomedicines 2020, 8, 383. [Google Scholar] [CrossRef]
- Ran, S.J.; Yang, X.; Sun, Z.; Zhang, Y.; Chen, J.X.; Wang, D.M.; Liu, B. Effect of length of apical root resection on the biomechanical response of a maxillary central incisor in various occlusal relationships. Int. Endod. J. 2020, 53, 111–121. [Google Scholar] [CrossRef]
- Richert, R.; Farges, J.C.; Tamimi, F.; Naouar, N.; Boisse, P.; Ducret, M. Validated finite element models of premolars: A scoping review. Materials 2020, 13, 3280. [Google Scholar] [CrossRef]
- Benazzi, S.; Grosse, I.R.; Gruppioni, G.; Weber, G.W.; Kullmer, O. Comparison of occlusal loading conditions in a lower second premolar using three-dimensional finite element analysis. Clin. Oral Investig. 2014, 18, 369–375. [Google Scholar] [CrossRef]
- Murakami, N.; Wakabayash, N. Finite element contact analysis as a critical technique in dental biomechanics: A review. J. Prosthodont. Res. 2014, 58, 92–101. [Google Scholar] [CrossRef]
- Acar, B.; Kamburoğlu, K.; Tatar, I.; Arıkan, V.; Çelik, H.H.; Yüksel, S.; Özen, T. Comparison of micro-computerized tomography and cone-beam computerized tomography in the detection of accessory canals in primary molars. Imaging Sci. Dent. 2015, 45, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Rangel, F.A.; Maal, T.J.J.; Bronkhorst, E.M.; Breuning, K.H.; Schols, J.G.J.H.; Bergé, S.J.; Kuijpers-Jagtman, A. M Accuracy and reliability of a novel method for fusion of digital dental casts and cone beam computed tomography scans. PLoS ONE 2013, 8, e59130. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, K.; Hasan, I.; Keilig, L.; Reimann, S.; Eliades, T.; Jäger, A.; Deschner, J.; Bourauel, C. Biomechanical time dependency of the periodontal ligament: A combined experimental and numerical approach. Eur. J. Orthod. 2013, 35, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Arzukanyan, A.V.; Spagnuolo, G.; Campagna, P.; Cicciù, M. Application of bioengineering devices for stress evaluation in dentistry: The last 10 years FEM parametric analysis of outcomes and current trends. Minerva Stomatol. 2020, 69, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Lahoud, P.; EzEldeen, M.; Beznik, T.; Willems, H.; Leite, A.; Van Gerven, A.; Jacobs, R. Artificial intelligence for fast and accurate 3D tooth segmentation on CBCT. J. Endod. 2021. [Google Scholar] [CrossRef] [PubMed]
- Wrzosek, M.K.; Peacock, Z.S.; Laviv, A.; Goldwaser, B.R.; Ortiz, R.; Resnick, C.M.; Troulis, M.J.; Kaban, L.B. Comparison of time required for traditional versus virtual orthognathic surgery treatment planning. Int. J. Oral Maxillofac. Surg. 2016, 45, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
| Material | Young’s Modulus (GPa) | Poisson’s Ratio |
|---|---|---|
| Dentine | 18.6 | 0.31 |
| Ligament | 0.069 | 0.45 |
| Trabecular bone | 1.3 | 0.3 |
| Gutta | 0.069 | 0.45 |
| Root-end filling (modified zinc-oxide eugenol) | 0.1 | 0.31 |
| Nickel Titanium (ProTaper Gold) | 50 | 0.26 |
| Structure | Number of Elements | Number of Nodes | Error Indicator Zhu Zienkiewicz |
|---|---|---|---|
| Initial model | 202,636 | 29,742 | 9.1% |
| Low enlargement | 202,462 | 29,637 | 9.2% |
| High enlargement | 202,027 | 29,614 | 9.3% |
| 3-mm apicoectomy | 201,714 | 29,855 | 8.9% |
| 6-mm apicoectomy | 207,250 | 31,126 | 9.2% |
| Clinical Situation | Change on the 3D Initial Image | High Stress Location |
|---|---|---|
| Initial state | No | Around the instrument |
| Low enlargement | Apical perforation | Around the perforation |
| High enlargement | Lateral perforation | Around the perforation |
| 3 mm apicoectomy | Decrease of the crown root ratio | Resected apex |
| 6 mm apicoectomy | Decrease of the crown root ratio | Resected apex |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Richert, R.; Farges, J.-C.; Villat, C.; Valette, S.; Boisse, P.; Ducret, M. Decision Support for Removing Fractured Endodontic Instruments: A Patient-Specific Approach. Appl. Sci. 2021, 11, 2602. https://doi.org/10.3390/app11062602
Richert R, Farges J-C, Villat C, Valette S, Boisse P, Ducret M. Decision Support for Removing Fractured Endodontic Instruments: A Patient-Specific Approach. Applied Sciences. 2021; 11(6):2602. https://doi.org/10.3390/app11062602
Chicago/Turabian StyleRichert, Raphaël, Jean-Christophe Farges, Cyril Villat, Sébastien Valette, Philippe Boisse, and Maxime Ducret. 2021. "Decision Support for Removing Fractured Endodontic Instruments: A Patient-Specific Approach" Applied Sciences 11, no. 6: 2602. https://doi.org/10.3390/app11062602
APA StyleRichert, R., Farges, J.-C., Villat, C., Valette, S., Boisse, P., & Ducret, M. (2021). Decision Support for Removing Fractured Endodontic Instruments: A Patient-Specific Approach. Applied Sciences, 11(6), 2602. https://doi.org/10.3390/app11062602









