Effects of Hip Abductor Strengthening on Musculoskeletal Loading in Hip Dysplasia Patients after Total Hip Replacement
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Experimental Data
2.2. Gait Analysis
2.3. Musculoskeletal Modeling and Gait Simulations
2.4. Statistical Analyses
3. Results
3.1. Function and Gait Analysis Results
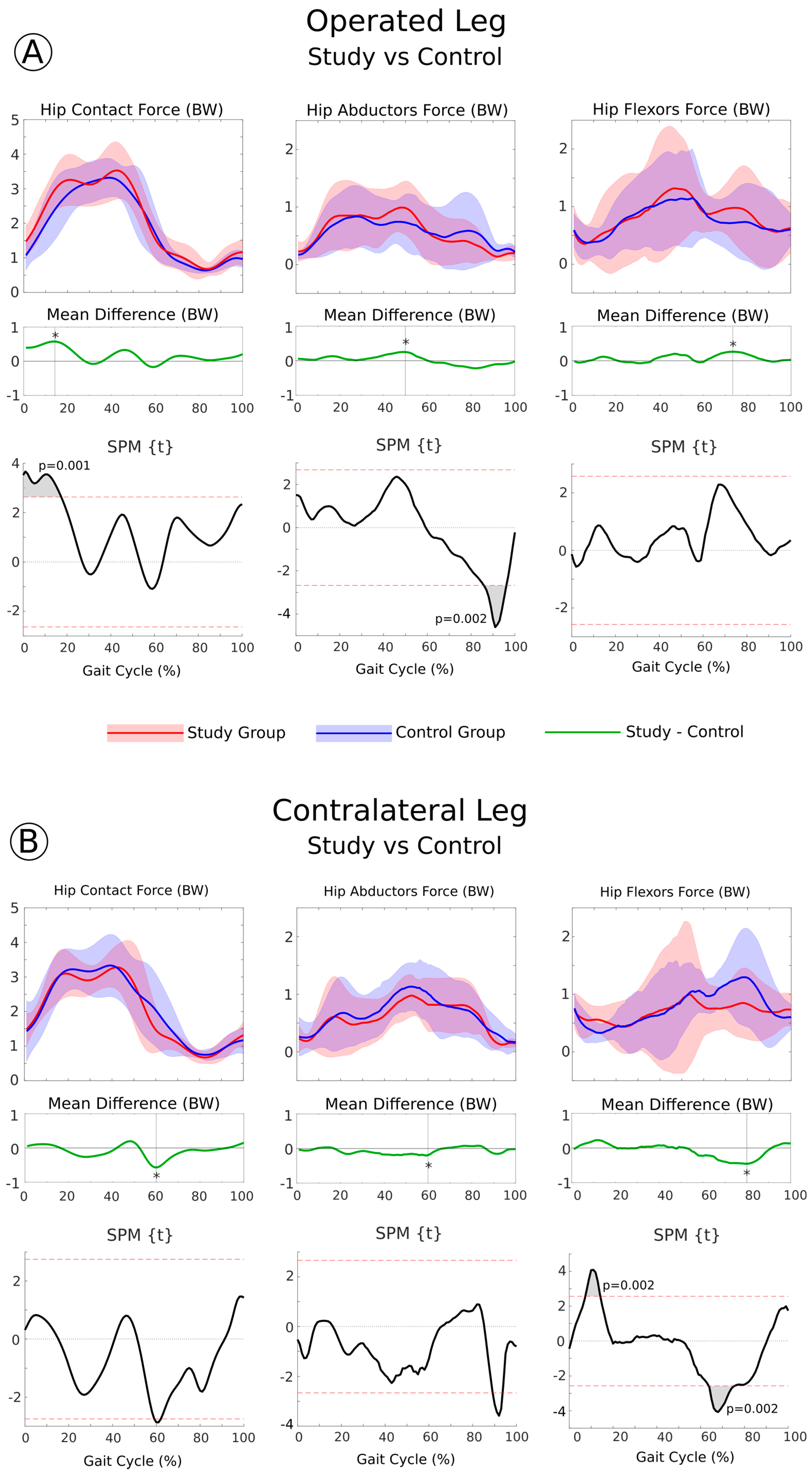
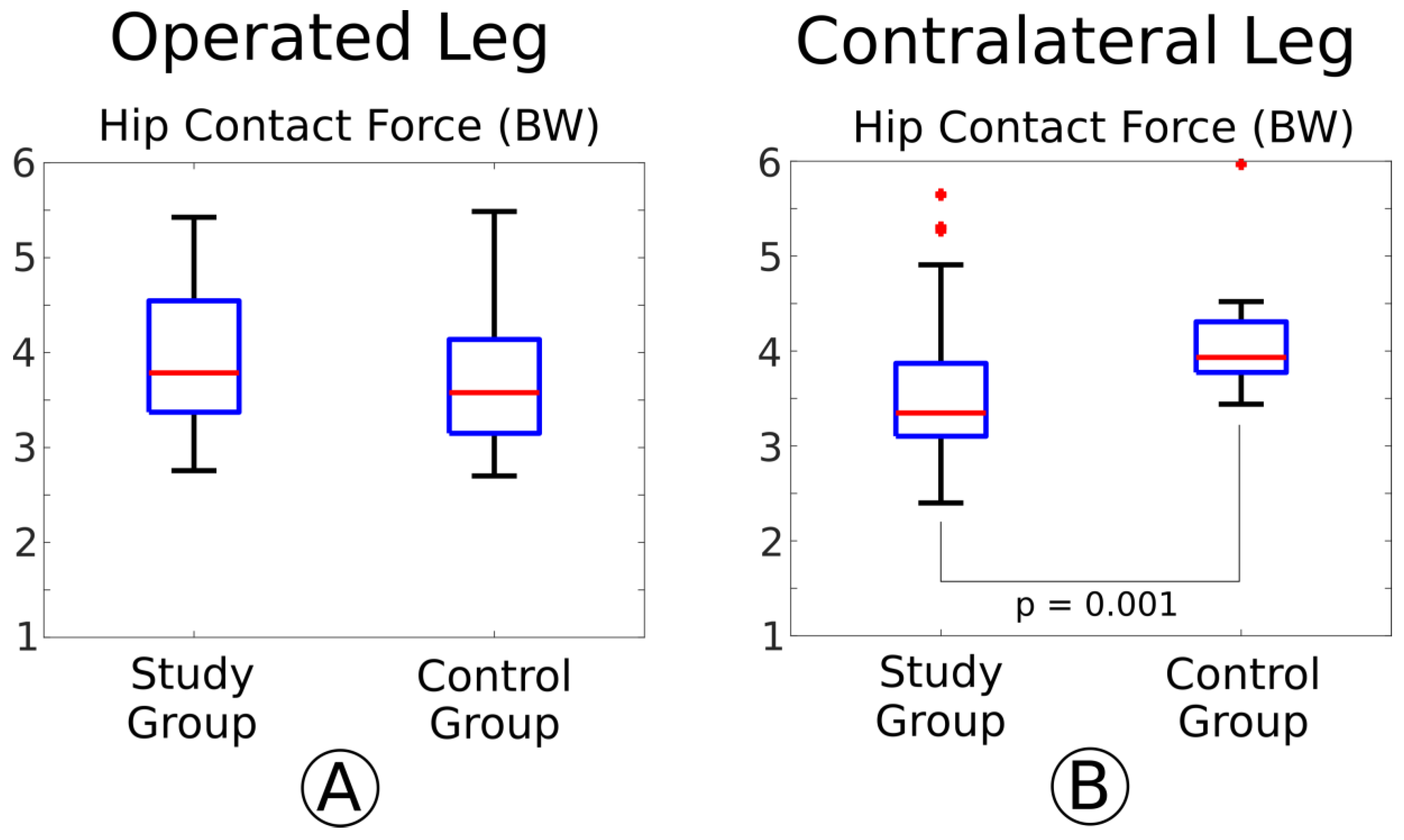
3.2. Analysis of the Musculoskeletal Forces
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Reikerås, O.; Haaland, J.E.; Lereim, P. Femoral Shortening in Total Hip Arthroplasty for High Developmental Dysplasia of the Hip. Clin. Orthop. Relat. Res. 2010, 468, 1949–1955. [Google Scholar] [CrossRef] [PubMed]
- Lecerf, G.; Fessy, M.-H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, P.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef]
- McGrory, B.; Morrey, B.; Cahalan, T.; An, K.; Cabanela, M. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J. Bone Jt. Surg. Br. Vol. 1995, 77, 865–869. [Google Scholar] [CrossRef]
- Liu, R.; Wen, X.; Tong, Z.; Wang, K.; Wang, C. Changes of gluteus medius muscle in the adult patients with unilateral developmental dysplasia of the hip. BMC Musculoskelet. Disord. 2012, 13, 101. [Google Scholar] [CrossRef]
- Rasch, A.; Byström, A.H.; Dalén, N.; Martinez-Carranza, N.; Berg, H.E. Persisting muscle atrophy two years after replacement of the hip. J. Bone Jt. Surg. Br. Vol. 2009, 91, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Di Monaco, M.; Castiglioni, C. Which type of exercise therapy is effective after hip arthroplasty? A systematic review of randomized controlled trials. Eur. J. Phys. Rehabil. Med. 2013, 49, 893–907. [Google Scholar]
- Di Monaco, M.; Vallero, F.; Tappero, R.; Cavanna, A. Rehabilitation after total hip arthroplasty: A systematic review of controlled trials on physical exercise programs. Eur. J. Phys. Rehabil. Med. 2009, 45, 303–317. [Google Scholar]
- Madara, K.C.; Marmon, A.; Aljehani, M.; Hunter-Giordano, A.; Zeni, J., Jr.; Raisis, L. Progressive Rehabilitation after Total Hip Arthroplasty: A Pilot and Feasibility Study. Int. J. Sports Phys. Ther. 2019, 14, 564–581. [Google Scholar] [CrossRef] [PubMed]
- Matheis, C.; Stöggl, T. Strength and mobilization training within the first week following total hip arthroplasty. J. Bodyw. Mov. Ther. 2018, 22, 519–527. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Cavazzuti, L.; Amabile, M.; Tassinari, E.; Valente, G.; Zanotti, G.; Vaienti, E.; Orsini, S.; Mariani, E.; Taddei, F. Abductor muscle strengthening in THA patients operated with minimally-invasive anterolateral approach for developmental hip dysplasia. HIP Int. 2021, 31, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Ning, N.; Pei, F.; Shen, B.; Zhou, Z.; Li, Z. Gait Kinematic Deviations in Patients With Developmental Dysplasia of the Hip Treated With Total Hip Arthroplasty. Orthopedics 2017, 40, e425–e431. [Google Scholar] [CrossRef]
- Catani, F.; Benedetti, M.G.; Binazzi, R.; De Zerbi, M.; Leardini, A.; Giannini, S. Functional evaluation in total hip replacement patients. Chir. Degli Organi Mov. 1999, 83, 349–357. [Google Scholar]
- Wesseling, M.; De Groote, F.; Meyer, C.; Corten, K.; Simon, J.-P.; Desloovere, K.; Jonkers, I. Subject-specific musculoskeletal modelling in patients before and after total hip arthroplasty. Comput. Methods Biomech. Biomed. Eng. 2016, 19, 1683–1691. [Google Scholar] [CrossRef] [PubMed]
- Myers, C.A.; Laz, P.J.; Shelburne, K.B.; Judd, D.L.; Winters, J.D.; Stevens-Lapsley, J.E.; Davidson, B.S. Simulated hip abductor strengthening reduces peak joint contact forces in patients with total hip arthroplasty. J. Biomech. 2019, 93, 18–27. [Google Scholar] [CrossRef]
- Elkins, J.M.; Pedersen, D.R.; Callaghan, J.J.; Brown, T.D. Fracture Propagation Propensity of Ceramic Liners During Impingement-Subluxation. J. Arthroplast. 2012, 27, 520–526. [Google Scholar] [CrossRef]
- Brandt, J.-M.; Gascoyne, T.C.; E Guenther, L.; Allen, A.; Hedden, D.R.; Turgeon, T.R.; Bohm, E.R. Clinical failure analysis of contemporary ceramic-on-ceramic total hip replacements. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2013, 227, 833–846. [Google Scholar] [CrossRef] [PubMed]
- Hicks, J.L.; Uchida, T.K.; Seth, A.; Rajagopal, A.; Delp, S.L. Is My Model Good Enough? Best Practices for Verification and Validation of Musculoskeletal Models and Simulations of Movement. J. Biomech. Eng. 2015, 137, 020905. [Google Scholar] [CrossRef] [PubMed]
- Pandy, M.G.; Andriacchi, T.P. Muscle and Joint Function in Human Locomotion. Annu. Rev. Biomed. Eng. 2010, 12, 401–433. [Google Scholar] [CrossRef]
- Marangoz, S.; Atilla, B.; Gök, H.; Yavuzer, G.; Ergin, S.; Tokgözoğlu, A.M.; Alpaslan, M. Gait analysis in adults with severe hip dysplasia before and after total hip arthroplasty. HIP Int. 2010, 20, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Ewen, A.M.; Stewart, S.; Gibson, A.S.C.; Kashyap, S.N.; Caplan, N. Post-operative gait analysis in total hip replacement patients—A review of current literature and meta-analysis. Gait Posture 2012, 36, 1–6. [Google Scholar] [CrossRef]
- Bahl, J.S.; Nelson, M.J.; Taylor, M.; Solomon, L.B.; Arnold, J.B.; Thewlis, D. Biomechanical changes and recovery of gait function after total hip arthroplasty for osteoarthritis: A systematic review and meta-analysis. Osteoarthr. Cartil. 2018, 26, 847–863. [Google Scholar] [CrossRef]
- Leardini, A.; Sawacha, Z.; Paolini, G.; Ingrosso, S.; Nativo, R.; Benedetti, M.G. A new anatomically based protocol for gait analysis in children. Gait Posture 2007, 26, 560–571. [Google Scholar] [CrossRef]
- Rajagopal, A.; Dembia, C.L.; Demers, M.S.; Delp, D.D.; Hicks, J.L.; Delp, S.L. Full-Body Musculoskeletal Model for Muscle-Driven Simulation of Human Gait. IEEE Trans. Biomed. Eng. 2016, 63, 2068–2079. [Google Scholar] [CrossRef] [PubMed]
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-Source Software to Create and Analyze Dynamic Simulations of Movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef] [PubMed]
- Anderson, F.C.; Pandy, M.G. Static and dynamic optimization solutions for gait are practically equivalent. J. Biomech. 2001, 34, 153–161. [Google Scholar] [CrossRef]
- Nichols, T.E.; Holmes, A.P. Nonparametric permutation tests for functional neuroimaging: A primer with examples. Hum. Brain Mapp. 2002, 15, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Pataky, T.C.; Robinson, M.A.; Vanrenterghem, J. Vector field statistical analysis of kinematic and force trajectories. J. Biomech. 2013, 46, 2394–2401. [Google Scholar] [CrossRef]
- Wesseling, M.; Meyer, C.; Corten, K.; Desloovere, K.; Jonkers, I. Longitudinal joint loading in patients before and up to one year after unilateral total hip arthroplasty. Gait Posture 2018, 61, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Lai, K.-A.; Lin, C.-J.; Jou, I.-M.; Su, F.-C. Gait analysis after total hip arthroplasty with leg-length equalization in women with unilateral congenital complete dislocation of the hip—Comparison with untreated patients. J. Orthop. Res. 2001, 19, 1147–1152. [Google Scholar] [CrossRef]
- Valente, G.; Taddei, F.; Jonkers, I. Influence of weak hip abductor muscles on joint contact forces during normal walking: Probabilistic modeling analysis. J. Biomech. 2013, 46, 2186–2193. [Google Scholar] [CrossRef]
- Giarmatzis, G.; Jonkers, I.; Wesseling, M.; Van Rossom, S.; Verschueren, S. Loading of Hip Measured by Hip Contact Forces at Different Speeds of Walking and Running. J. Bone Miner. Res. 2015, 30, 1431–1440. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Gaffney, B.M.; Shelburne, K.B.; Pascual-Garrido, C.; Clohisy, J.C.; Harris, M.D. Dysplastic hip anatomy alters muscle moment arm lengths, lines of action, and contributions to joint reaction forces during gait. J. Biomech. 2020, 110, 109968. [Google Scholar] [CrossRef]
- Skalshøi, O.; Iversen, C.H.; Nielsen, D.B.; Jacobsen, J.; Mechlenburg, I.; Søballe, K.; Sørensen, H. Walking patterns and hip contact forces in patients with hip dysplasia. Gait Posture 2015, 42, 529–533. [Google Scholar] [CrossRef]
- Thomas-Aitken, H.D.; Willey, M.C.; Goetz, J.E. Joint contact stresses calculated for acetabular dysplasia patients using discrete element analysis are significantly influenced by the applied gait pattern. J. Biomech. 2018, 79, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, H.; Skalshøi, O.; Nielsen, D.B.; Jacobsen, J.S.; Søballe, K.; Mechlenburg, I. Hip muscle and joint contact forces before, 6 and 12 months after minimally invasive periacetabular osteotomy. HIP Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Damm, P.; Zonneveld, J.; Brackertz, S.; Streitparth, F.; Winkler, T. Gluteal muscle damage leads to higher in vivo hip joint loads 3 months after total hip arthroplasty. PLoS ONE 2018, 13, e0190626. [Google Scholar] [CrossRef] [PubMed]
- Kovalak, E.; Özdemir, H.; Ermutlu, C.; Obut, A. Assessment of hip abductors by MRI after total hip arthroplasty and effect of fatty atrophy on functional outcome. Acta Orthop. Traumatol. Turc. 2018, 52, 196–200. [Google Scholar] [CrossRef]
- Eng, J.J.; Chu, K.S. Reliability and comparison of weight-bearing ability during standing tasks for individuals with chronic stroke. Arch. Phys. Med. Rehabil. 2002, 83, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Shakoor, N.; Hurwitz, D.E.; Block, J.A.; Shott, S.; Case, J.P. Asymmetric knee loading in advanced unilateral hip osteoarthritis. Arthritis Rheum. 2003, 48, 1556–1561. [Google Scholar] [CrossRef] [PubMed]

| Study Group | Control Group | |
| Sample Size | 12 | 6 |
| Gender | 11 female/1 male | 5 female/1 male |
| Follow-up (months) | 7 (1) | 7 (1.5) |
| Age (years) | 58.2 (9.4) | 53 (6.8) |
| Body Mass (kg) | 63 (8.8) | 66 (15) |
| Height (m) | 1.6 (0.04) | 1.59 (0.13) |
| BMI (kg/m2) | 24 (3.1) | 23.3 (3.9) |
| Study Group | Control Group | Mann–Whitney U-Test | |||
| Median | IQR | Median | IQR | p-values | |
| Stance time operated side (% stride) | 61.1 | 2.4 | 62.5 | 5.5 | 0.037 |
| Stance time contralateral side (% stride) | 62.2 | 3.3 | 62.9 | 4.5 | 0.786 |
| Stride length operated side (% height) | 72.9 | 9.2 | 67.9 | 9.2 | 0.062 |
| Stride length contralateral side (% height) | 72.5 | 11.3 | 70.2 | 7.3 | 0.270 |
| Cycle times (s) | 1.13 | 0.17 | 1.17 | 0.26 | 0.007 |
| Cadence (stride/m) | 52.6 | 7.8 | 52.2 | 10.4 | 0.009 |
| Speed (cm/s) | 105.5 | 21.6 | 96.3 | 30.9 | 0.017 |
| Study Group | Control Group | Mann–Whitney U-Test | |||
| Median | IQR | Median | IQR | p-values | |
| Pelvic obliquity max peak | 2.7 | 4.1 | 2.3 | 1.2 | 0.658 |
| Pelvic obliquity min peak | −2.5 | 5.8 | −3.3 | 3.4 | 0.999 |
| Hip flex/ext ROM | 32.4 | 5.2 | 34.6 | 16.1 | 0.999 |
| Hip abd/add ROM | 10.9 | 4.9 | 10.1 | 3 | 0.999 |
| Hip int/ext rotation ROM | 9 | 4.2 | 8.4 | 2.3 | 0.999 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valente, G.; Taddei, F.; Leardini, A.; Benedetti, M.G. Effects of Hip Abductor Strengthening on Musculoskeletal Loading in Hip Dysplasia Patients after Total Hip Replacement. Appl. Sci. 2021, 11, 2123. https://doi.org/10.3390/app11052123
Valente G, Taddei F, Leardini A, Benedetti MG. Effects of Hip Abductor Strengthening on Musculoskeletal Loading in Hip Dysplasia Patients after Total Hip Replacement. Applied Sciences. 2021; 11(5):2123. https://doi.org/10.3390/app11052123
Chicago/Turabian StyleValente, Giordano, Fulvia Taddei, Alberto Leardini, and Maria Grazia Benedetti. 2021. "Effects of Hip Abductor Strengthening on Musculoskeletal Loading in Hip Dysplasia Patients after Total Hip Replacement" Applied Sciences 11, no. 5: 2123. https://doi.org/10.3390/app11052123
APA StyleValente, G., Taddei, F., Leardini, A., & Benedetti, M. G. (2021). Effects of Hip Abductor Strengthening on Musculoskeletal Loading in Hip Dysplasia Patients after Total Hip Replacement. Applied Sciences, 11(5), 2123. https://doi.org/10.3390/app11052123







