1. Introduction
Three-dimensional printing is also called additive manufacturing or rapid prototyping, and it has contributed to the popularization of digital dentistry while overcoming the limitations of subtractive machining methods based on milling or grinding [
1,
2]. The current methods of prosthesis production using 3D printing can overcome the limitations of subtractive manufacturing, such as reducing cutting forces due to the wear of milling tools, limitations associated with tool sizes, difficulty in manufacturing complex shapes, and material wastage. There are now wide ranges of equipment and raw materials with various prices and performances available in the market [
3].
3D printers based on stereolithography (SLA) or digital light processing (DLP) are currently the most widely used in digital dentistry. These two methods are classified based on the light source and curing method, and they have the advantages of high-precision printing and excellent surface texture [
2,
4,
5]. The use of various photopolymeric resins makes it possible to manufacture diverse types of objects, from individual trays and dental models to final prostheses such as radiographic stents, provisional crowns, record bases, and dentures [
1,
6,
7,
8,
9]. The development and use of 3D printers facilitate the fabrication of custom prostheses with complex configurations. However, the processing principles of 3D printers mean that certain specific factors that are not present in conventional manufacturing methods need to be considered. The accuracy and mechanical properties of 3D printing can be affected by variables such as machine settings, output position or build angle, number of layers, and configuration of the support structure. However, the high diversity of 3D printers and materials and the heterogeneity of their combinations mean that the 3D printing process and the associated postcuring process still need to be optimized and standardized [
10,
11,
12,
13,
14].
Postcuring is an essential step when using a photopolymer resin with an SLA or DLP printer, as it can cause improvements in mechanical or biological properties through crosslinking of unreacted monomers after processing of 3D printing materials [
15,
16]. Objects that have been printed by these printers are cleaned of unpolymerized residual monomers, and additional polymerization is performed using ultraviolet light (UV) produced by light-emitting diodes (LEDs) in postcuring equipment. The degree of polymerization greatly affects not only the biocompatibility and color stability of the fabricated object but also its mechanical properties and dimensional stability [
14,
17,
18,
19]. It is known that the lower the polymerization rate in the 3D printing process, the greater the dimensional change occurs in the postcuring step, and the shrinkage of the area directly exposed to UV light occurs a lot, which can lead to bending due to non-uniform shrinkage [
20]. Minimizing errors in the production process, and especially in the 3D printing process and postcuring, can result in a more predictable prosthesis manufacturing workflow. Several studies have investigated the precision, dimensional stability, and mechanical properties using several 3D printers [
11,
12,
21,
22,
23,
24,
25,
26,
27]. Many companies provide guidelines for the use of materials and equipment required for the 3D printing process. However, in the process of manufacturing a series of prostheses using various products as an open system, it is often difficult to follow the guidelines of the company as it is. In addition, there are no unified guidelines among companies. Users are making the process based on empirical evidence.
During the postcuring process, a dimensional change is expected because additional curing of the residual uncured resin occurs, but studies on this are lacking. In addition, the support structure that connects the bottom surface where printing starts on the 3D printer’s platform and the prosthesis is essential for the 3D printing process and is thought to play a role in stabilizing the dimension of the workpiece in the subsequent postcuring process. However, to the best of our knowledge, there was no study on the effect of the removal time of the support structure in the 3D printing process. Rather, in many experiments involving 3D printers, the timing of removal of the support structure was not controlled. Studies relating to the accuracy and mechanical properties of produced samples can be divided into those where the support structure was removed after postcuring [
21,
27] or before postcuring [
24,
25] or not accurately recorded [
10,
12,
13,
25].
This study produced maxillary and mandibular edentulous denture bases using a 3D printing system based on SLA and DLP technologies, with the aim of determining the dimensional stability according to the postcuring time and the presence or absence of a support structure during postcuring. The null hypothesis was that the dimensional stability of the denture base produced by 3D printing does not differ significantly with the postcuring time, the presence or absence of a support structure during postcuring, or the arch position.
2. Materials and Methods
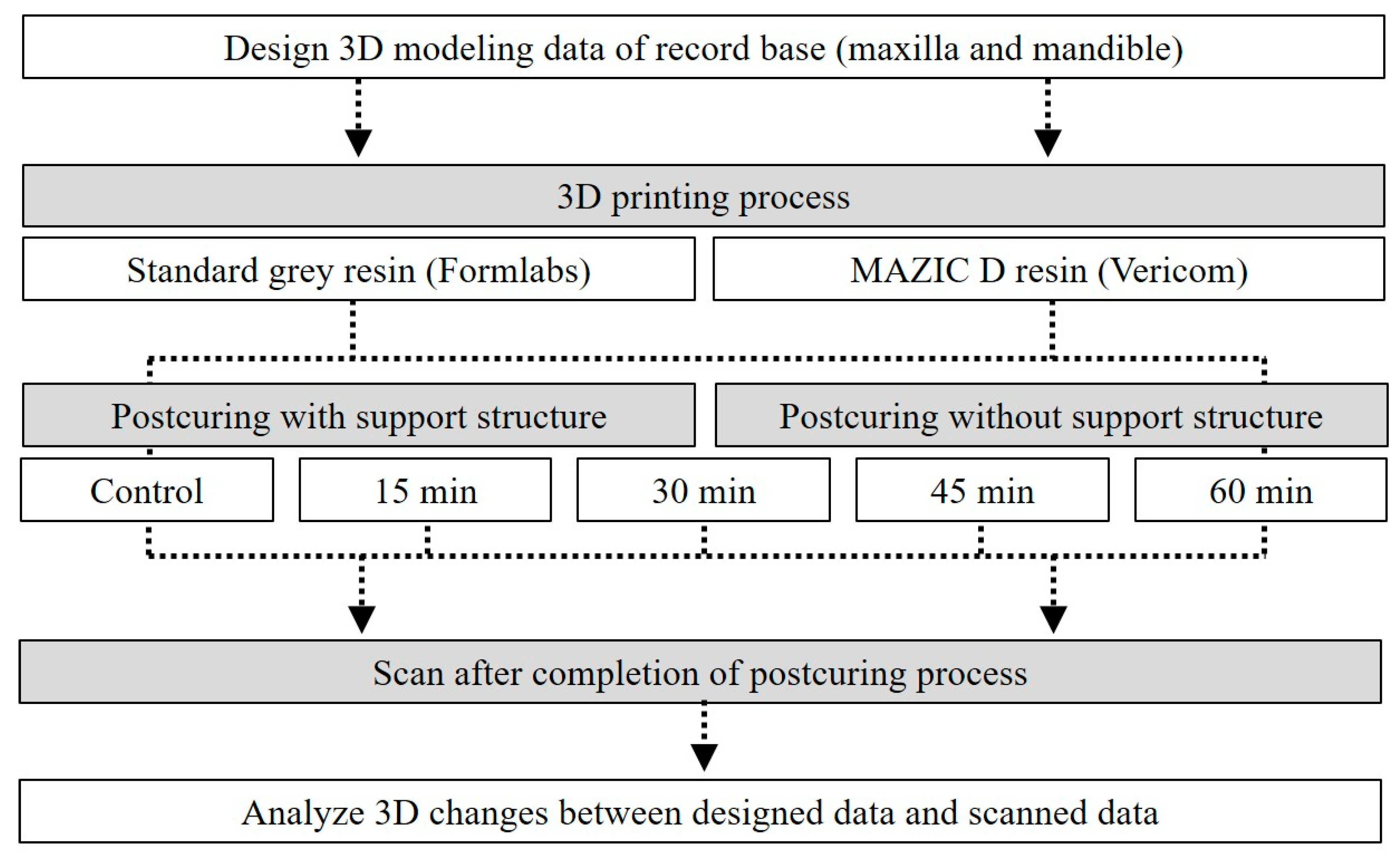
For designing the standard denture base, a fully edentulous maxilla and mandible reference model was selected and then scanned using a tabletop scanner (Identica T500, Medit, Seoul, Korea). After importing the scanned model data into CAD software for dental use (Exocad DentalCAD, Exocad, Darmstadt, Germany), the denture base was designed, and the designed data were exported as an STL (standard tessellation language) file (
Figure 1).
Two types of 3D printing photocurable resin were used for the 3D printing of the design file: standard gray resin (Formlabs, Somerville, MA, USA) and MAZIC D resin (Vericom, Anyang, Korea) (
Table 1). Each photocurable resin was mixed in accordance with the manufacturer’s recommended mixing time using a material mixing unit (LC-3DMixer, NextDent, Soesterberg, The Netherlands) to ensure that the contents were adequately mixed prior to printing. In order to optimally three-dimensionally print the material used, slicing software and a 3D printer with settings compatible with each photocurable resin were used. For printing MAZIC D resin, support generation and mesh slicing were performed using slicing software (Chitu DLP Slicer, CBD-Tech, Guangdong, China) for 3D printing.
A support structure was placed on the outer surface of the denture base, and the thickness of each building layer was set to 100 µm. Three-dimensional printing of the mesh file was performed using a DLP 3D printer with 24,405-nm UV LEDs in a 50-W matrix (ParaLED, Phrozen Shuffle, Phrozen, Hsinchu, Taiwan). For the standard gray resin, the support arrangement design specified by the Chitu DLP Slicer software was imported into the Preform slicer software (Formlabs, Somervill, MA, USA) to make the same arrangement, and three-dimensionally printed using a compatible SLA 3D printer with a 250-mW 405-nm UV LED (Form3, Formlabs). Each manufactured denture base was washed with 100% isopropyl alcohol for 10 min using washing equipment (TwinTornado, Medifive, Seoul, Korea) and then postcured using a postcuring device (MP100, Hebsiba, Incheon, Korea).
For the purpose of this study, the postcuring time and the removal of the support structure before the postcuring process were set differently for each group. In the no-support group, after 3D printing the denture base, the support structure was removed prior to carrying out postcuring. For the support group, postcuring was performed without removal of the support structure after printing the denture base. In addition to a control group (with no postcuring), postcuring times of 15, 30, 45, and 60 min were employed (
n = 10 for each denture base). Data relating to the denture base in all groups were obtained using 3D scanning with a tabletop scanner after postcuring. The overall experimental workflow employed in this study is outlined in
Figure 2.
All acquired data were exported to 3D analysis software (Geomagic Control X, 3D Systems, Rock Hill, SC, USA). To analyze the dimensional changes during postcuring of the denture base, the 3D modeling data and the scanned data after postcuring were compared and analyzed. The data to be compared were initially aligned using a three-point registration process and then further aligned using a best-fit algorithm. Differences between the groups were analyzed using the root-mean-square error (RMSE) values calculated as follows (1):
where
is the measurement point of reference
i,
is the measurement point of scan data
i, and
n is the total number of points measured in each data set. The overall deviations were displayed in color maps to facilitate intuitive comparisons, assigning a deviation range of ±500 µm and a tolerance of ±50 µm.
Standard statistical software (SPSS Statistics, version 25.0, IBM Corporation, Armonk, NY, USA) was used for the statistical analyses. The Shapiro–Wilk test was performed to confirm that the data in each group conformed to a normal distribution. Three-way ANOVA was used to evaluate the effect of the presence or absence of a support structure during postcuring, arch position (maxilla or mandible), and postcuring time on the RMSE values between the modeling and scanned data. One-way ANOVA was used to test dimensional changes within the same arch and materials based on the postcuring time, and a post-hoc test was performed using the Bonferroni method (α = 0.05). Differences between the support and no-support groups according to time in the same arch and the same material were analyzed using Student’s t-test (α = 0.05).
3. Results
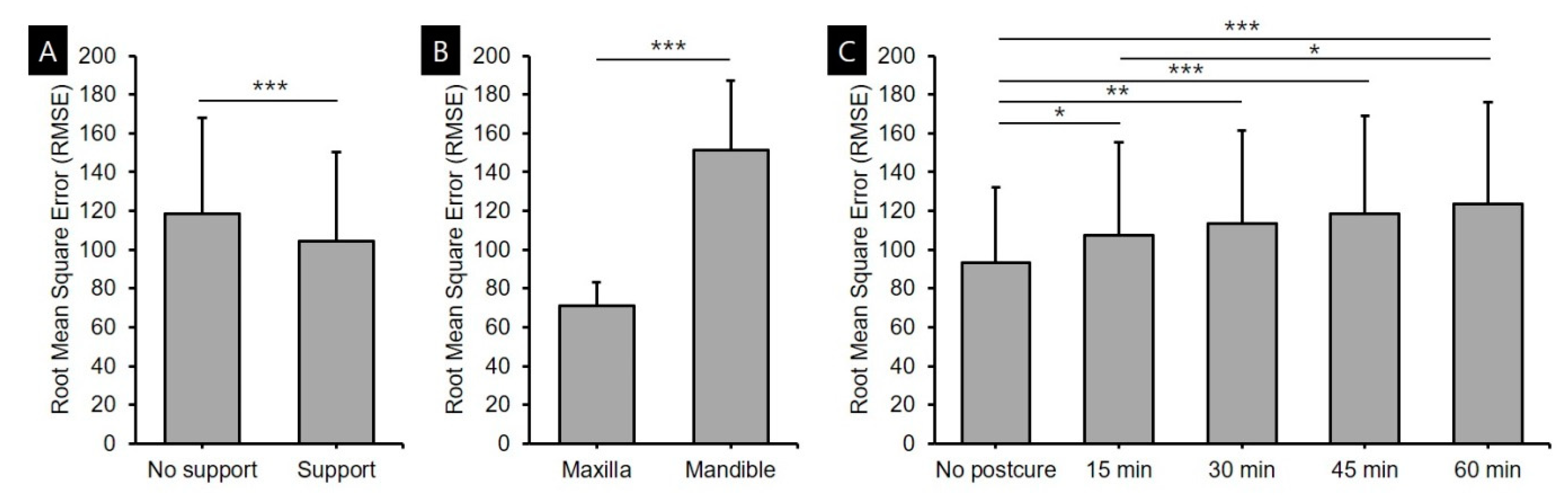
The results of the three-way ANOVAs of standard gray resin and MAZIC D resin are presented in
Figure 3 and
Figure 4. The three-way ANOVA of standard gray resin for the RMSE values between the modeling and scan data after the postcuring process confirmed that the dimensional changes were significantly affected by whether the support structure was removed (
F = 17.317,
p < 0.001), the arch position (
F = 567.555,
p < 0.001), and the postcuring time (
F = 9.755,
p < 0.001) (
Figure 3). The accuracy was higher for the group in which the support structure was present during the postcuring process than for the group without support and higher for the maxilla than for the mandible. The error increased gradually with the postcuring time during the process of polymerization of the unpolymerized residual resin. However, there were no significant interactions between support removal and arch position (
F = 2.151,
p = 0.144), support removal and postcuring time (
F = 1.295,
p = 0.274), or arch position and postcuring time (
F = 0.805,
p = 0.523), nor between all three factors (
F = 0.268,
p = 0.898).
The three-way ANOVA of MAZIC D resin confirmed that the dimensional changes were significantly affected by support removal (
F = 98.774,
p < 0.001), arch position (
F = 191.145,
p < 0.001), and postcuring time (
F = 32.032,
p < 0.001) (
Figure 4). The accuracy was highest in the group in which the support structure was present and the maxillary group, and the error increased with the postcuring time. Significant interactions were observed between support removal and arch position (
F = 66.668,
p < 0.001), support removal and postcuring time (
F = 8.174,
p < 0.001), and among all three factors (
F = 3.786,
p = 0.006). However, there was no significant interaction between the arch position and postcuring time (
F = 0.590,
p = 0.670).
Dimensional accuracy was evaluated when the same 3D printing resin was used in the same arch, and the overall results are presented in
Figure 5 and
Figure 6 and in
Table 2. For the maxilla base printed three-dimensionally using standard gray resin, the dimensional changes were smaller in the group in which postcuring was performed with the support structure present. The error increased with the postcuring time even in the specimen with the support structure, but the magnitude of the increase was relatively small. The error ranges in the no-support, and support groups were 58.3–83.6 µm and 58.9–72.9 µm, respectively. The accuracy differed significantly between the presence and absence of the support structure for all postcuring times, but not in the control group that did not undergo postcuring (
Figure 5A). The pattern was the same in the mandible-base group printed using standard gray resin, but the accuracy was lower than in the maxillary group, with error ranges of 130.4–185.6 µm in the no-support group and 124.8–148.0 µm in the support group (
Figure 5B).
When printing denture bases using MAZIC D resin, the dimensional changes in the no-support group were largest after the first 15 min of postcuring for both the maxillary and mandibular bases, after which there were no significant variations in the dimensional changes (
Figure 6). In the maxilla group with MAZIC D resin, the dimensions changed during the postcuring process even when the support structure was present, and the errors were in the range of 72.6–104.6 µm. There was a significant difference between the no-support and support groups only after 15 min of postcuring, with a large initial dimensional change in the no-support group, but no change thereafter. It seems that the polymerization of MAZIC D resin proceeded faster than the standard gray resin (
Figure 6A). In the mandible group with MAZIC D, there was no significant dimensional change when the support structure was present during the postcuring process, and the error range was 99.7–105.1 µm. There were significant differences between the no-support and support groups at all postcuring time periods other than for the control group (
Figure 6B).
The qualitative overall deviation results are presented as color maps in
Figure 7 and
Figure 8. The error was smallest in the control group without postcuring. In the case of the maxilla, there were positive errors in the anterior alveolar ridge area and the maxillary tuberosity area and negative errors in the center of the palate. As the postcuring time increased, the flange area of the denture base around the posterior teeth showed a pattern of increasing positive errors, and the palate area showed a pattern of increasing negative errors. In the case of the mandible, the errors were largest in the retromolar pad area, where there were positive errors. The alveolar ridge area around the lingual border and the premolar area showed negative errors. In these areas, the errors increased with the postcuring time. The groups using standard gray resin and MAZIC D resin showed similar trends (
Figure 7 and
Figure 8).
4. Discussion
The purpose of this study was to determine the dimensional stability of maxillary and mandibular edentulous denture bases according to the postcuring time and whether the support structure is present or removed during the postcuring process after 3D printing. Denture-based samples were constructed using 3D printers with two resins, and postcuring times of 0, 15, 30, 45, and 60 min were investigated. Three-way ANOVAs showed that when using the SLA-type Form3 printer and standard gray resin or the DLP-type Phrozen Shuffle printer and MAZIC D resin, the accuracy was significantly higher when postcuring was performed with the support structure present and higher for the maxilla than the mandible. The dimensional changes gradually accumulated, and the deviations increased with the postcuring time. Therefore, the null hypothesis of this study, that there are no dimensional changes according to the removal of the support structure, arch position, and postcuring time, was rejected.
Most previous studies have found that digital dentures and record bases produced by 3D printing are highly accurate. In the present experiments, when using standard gray resin with the SLA-type Form3 printer, the error in the no-support group increased significantly with the postcuring time for both maxillary and mandibular denture bases. In the support group, there were significant changes as the postcuring time increased in the maxilla, but there were few changes in the dimension for the mandible and no significant differences according to the postcuring time (
Figure 5,
Table 2). Kalberer et al. [
24], which was designed to remove the support structure before postcuring, is noteworthy that the accuracy was inferior in their 3D printing group, which contrasts with other studies. Those authors observed a significantly larger dimensional difference for the maxillary edentulous denture base constructed using an SLA 3D printer than for the milled type of base. They attributed this observation to the deformation of partially polymerized prostheses during demounting or to polymerization shrinkage. Their analysis results are consistent with those of the present experiments, which showed that differences in dimensional changes appeared with or without a support structure.
In both the SLA and DLP methods, the postcuring step is as important as the design and printing processes, and an insufficient postcuring time can result in dimensional changes or reduced strength due to the presence of unpolymerized resin [
28]. If the output is an individual tray, insufficient postcuring may result in distortion of the tray and the impression body after obtaining the impression. In the case of a denture base, insufficient postcuring may cause issues relating to its fit, which affects the accuracy of the artificial tooth attachment due to warping of the joint, and may, in turn, lead to an overall occlusal error. In addition, even for a three-dimensionally printed model, insufficient postcuring can lead to errors in the fabrication of the prosthesis that cause serious problems [
29].
In the present experiments using the MAZIC D resin and the DLP-type Phrozen Shuffle 3D printer, dimensional changes during postcuring were hardly observed in the group with the support structure present. However, in the group where the support structure was not present, a rapid change in dimensions was observed during the first 15 min of postcuring. As mentioned above, this is considered to be due to a problem with the initial polymerization rate. Additional changes may have occurred due to the presence of bulk resin in the palate area and the direction of polymerization shrinkage in this direction. The difference in the characteristics of change between standard gray resin and Mazic D resin seems to be due not only to the difference in initial polymerization due to the difference between SLA and DLP but also to the faster polymerization rate of MAZIC D resin during the postcuring period. Preventing such a dimensional change due to the presence of residual monomers requires the manufacturer’s instructions to be followed exactly. However, since many CAD/CAM systems are open-source systems and due to various types of 3D printers, software, and materials being used by clinicians and laboratories, the manufacturer’s instructions related to the use of standardized company equipment and resins might diverge. In addition, it should be considered that the postcuring time may vary with the values set for 3D printing devices [
25].
When using MAZIC D resin and a DLP 3D printer, continuous errors were observed in the maxilla regardless of the postcuring time or presence of a support structure. The larger error for the maxilla than for the mandible was attributed to the large error in the palate area. The palate of the maxilla can play a role in maintaining the dimensional stability of the fabricated object, such as a support structure used in the 3D printing process does, but unlike the support structure, it is an area that is used without being removed. Hwang et al. [
12] recently found both positive and negative errors in the maxillary palate for maxillary denture bases produced using the DLP 3D printer, which is similar results to this present experiments. Those authors attributed the geometry deviations to the 100-degree construction angle and sagging of the liquid material under its own weight. This analysis can be supported through the result that palate error is small even in the milled type manufacturing method [
12,
30]. In addition, in the postcuring process, since there may be a difference in the shrinkage between the part that is directly irradiated with UV light and the part that is not directly irradiated with UV light, this may cause bending and lead to an error in the denture base [
20]. In this study, the average RMSE values of standard gray resin and MAZIC D resin were similar, but in the color map shown in
Figure 7, it was confirmed that the overall deviation of MAZIC D resin was large. This trend was especially observed in the maxilla, and it can be confirmed through the fact that the standard deviation value of MAZIC D resin is higher than that of standard gray resin in all postcuring time periods.
Recent comparative studies found that the accuracy of 3D printing methods was equivalent to or better than those of existing milling methods [
21,
26,
27], although inaccurate and irreproducible results have also been reported [
24,
25]. It is noteworthy that these studies involved various postcuring times and support-structure removal times. Those experiments applied postcuring times such as 10, 15, and 30 min, or the exact time was not recorded [
10,
24,
25,
27]. More accurate comparative experiments require the postcuring time to be properly controlled and recorded, given that this is a very important parameter.
The present study was subject to some limitations. Since the required postcuring time varies with the 3D printer, material type, and light source (e.g., its wavelength and intensity) of the postcuring device, standard guidelines cannot be determined solely from the results of this study. In addition, while two types of materials, 3D printers and denture bases with a uniform thickness, were used in the present experiments, the diversity of materials and equipment will be greater in in vivo applications, and the thickness will vary according to the type of residual ridge. Future studies involving various types of equipment, materials, layer thicknesses, and irregular shapes may provide more meaningful guidelines for the optimal conditions to use when producing prostheses using 3D printing technology.