Outpatient Total Knee Arthroplasty: A Meta-Analysis
Abstract
:1. Introduction
2. Material and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
- P (Population): end stage knee osteoarthritis;
- I (Intervention): outpatient TKA;
- C (Comparison): inpatient TKA;
- O (Outcomes): PROMs, complications.
2.3. Selection and Data Collection
2.4. Data Items
2.5. Methodology Quality Assessment
2.6. Synthesis Methods
3. Results
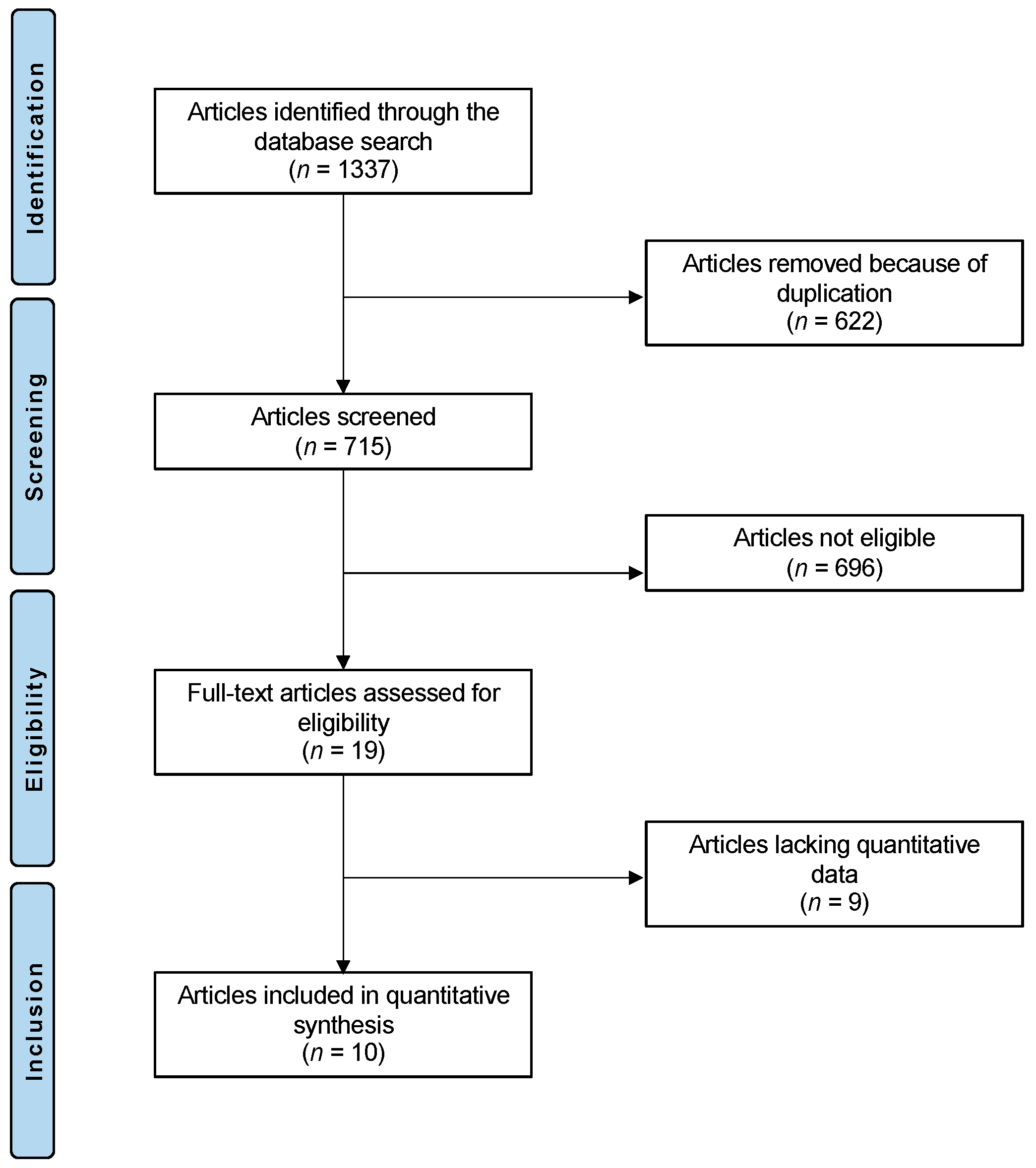
3.1. Study Selection
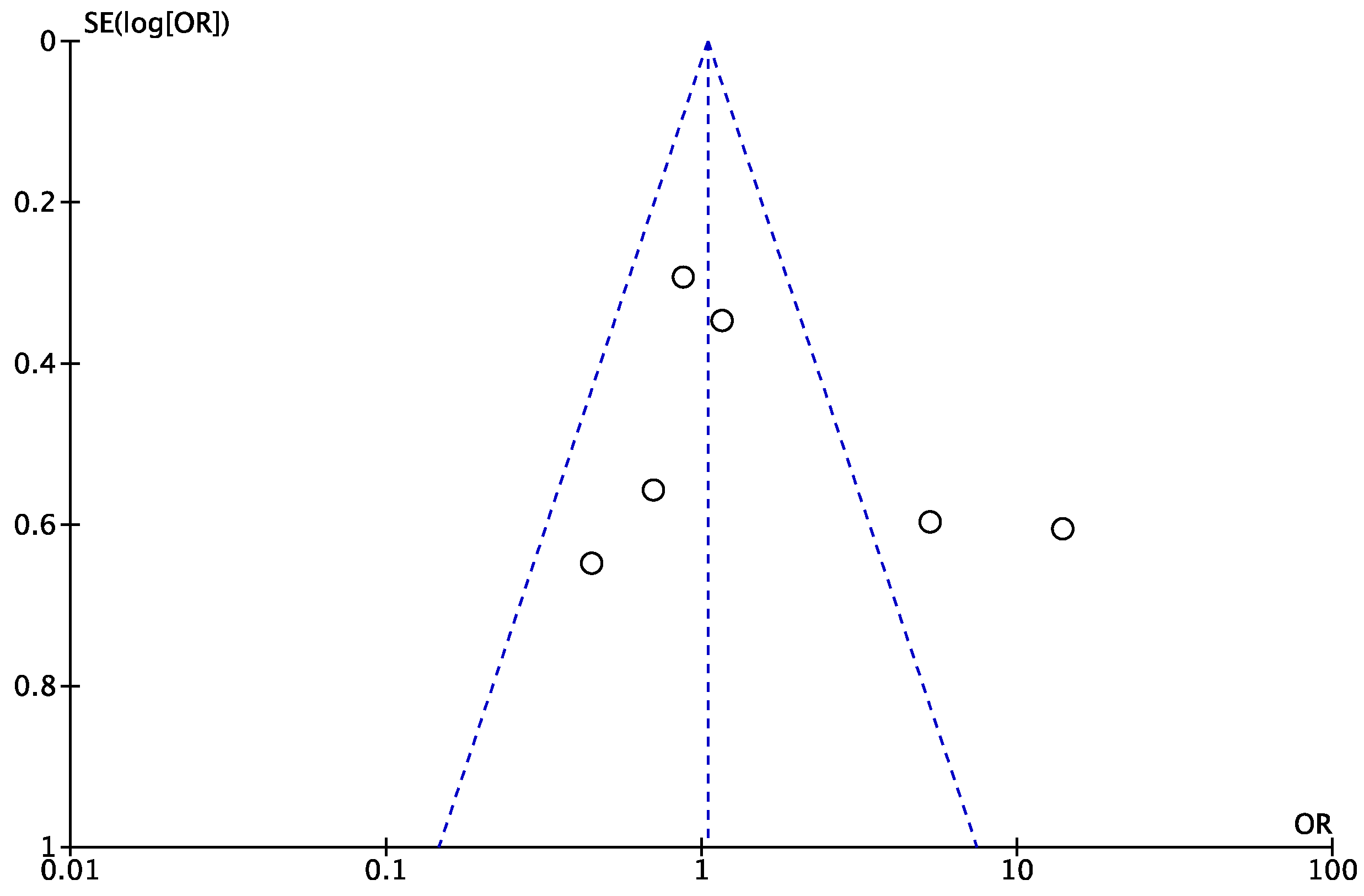
3.2. Risk of Publication Bias Assessment
3.3. Methodological Quality Assessment
3.4. Study Characteristics and Results of Individual Studies
3.5. Results of Syntheses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kolisek, F.R.; McGrath, M.S.; Jessup, N.M.; Monesmith, E.A.; Mont, M.A. Comparison of Outpatient versus Inpatient Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 2009, 467, 1438–1442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodríguez-Merchán, E.C. Outpatient total knee arthroplasty: Is it worth considering? EFORT Open Rev. 2020, 5, 172–179. [Google Scholar] [CrossRef]
- Yang, J.; Olsen, A.S.; Serino, J.; Terhune, E.B.; DeBenedetti, A.; Della Valle, C.J. Similar 90-day outcomes among inpatient and outpatient arthroplasties: A single-surgeon matched cohort analysis. Bone Jt. J. 2021, 103-B (Suppl. 7B), 84–90. [Google Scholar] [CrossRef]
- Fassihi, S.C.; Malahias, M.-A.; Gu, A.; Richardson, S.S.; Buller, L.T.; Stake, S.; De Martino, I.; Pathak, N.; Chen, A.Z.; Ast, M.P.; et al. Hospital Discharge within a Day After Total Knee Arthroplasty Does Not Affect 1-Year Complications Compared With Rapid Discharge. J. Am. Acad. Orthop. Surg. 2021, 29, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.K.; Milles, J.L.; Stambough, J.B.; Barnes, C.L.; Mears, S.C. Inpatient versus Outpatient Total Knee Arthroplasty. J. Knee Surg. 2019, 32, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Lan, R.H.; Samuel, L.T.; Grits, D.; Kamath, A.F. Contemporary Outpatient Arthroplasty Is Safe Compared with Inpatient Surgery: A Propensity Score-Matched Analysis of 574,375 Procedures. J. Bone Jt. Surg.-Am. Vol. 2021, 103, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Adelani, M.A.; Barrack, R.L. Patient Perceptions of the Safety of Outpatient Total Knee Arthroplasty. J. Arthroplast. 2018, 34, 462–464. [Google Scholar] [CrossRef]
- Scully, R.D.; Kappa, J.E.; Melvin, J.S. “Outpatient”—Same-calendar-day Discharge Hip and Knee Arthroplasty. J. Am. Acad. Orthop. Surg. 2020, 28, e900–e909. [Google Scholar] [CrossRef]
- Huang, A.; Ryu, J.-J.; Dervin, G. Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can. J. Surg. 2017, 60, 57–62. [Google Scholar] [CrossRef]
- Meneghini, R.; Ziemba-Davis, M. Patient Perceptions Regarding Outpatient Hip and Knee Arthroplasties. J. Arthroplast. 2017, 32, 2701–2705.e1. [Google Scholar] [CrossRef] [Green Version]
- Bordoni, V.; Poggi, A.; Zaffagnini, S.; Previtali, D.; Filardo, G.; Candrian, C. Outpatient total knee arthroplasty leads to a higher number of complications: A meta-analysis. J. Orthop. Surg. Res. 2020, 15, 408. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, R.W.; Jennings, J.M.; Dennis, D.A. Enhancing Recovery After Total Knee Arthroplasty. Orthop. Clin. North Am. 2017, 48, 391–400. [Google Scholar] [CrossRef]
- Pollock, M.; Somerville, L.; Firth, A.; Lanting, B. Outpatient Total Hip Arthroplasty, Total Knee Arthroplasty, and Unicompartmental Knee Arthroplasty: A Systematic Review of the Literature. JBJS Rev. 2016, 4, e4. [Google Scholar] [CrossRef]
- Stephan, A. An Update on Total Joint Arthroplasty: Current Models of Care, Strategies, and Innovations Providing the Best Patient Outcomes and the Big Changes in the Patient Experience. Nurs. Clin. N. Am. 2020, 55, 203–208. [Google Scholar] [CrossRef]
- Bovonratwet, P.; Shen, T.; Ast, M.P.; Mayman, D.J.; Haas, S.B.; Su, E.P. Reasons and Risk Factors for 30-Day Readmission After Outpatient Total Knee Arthroplasty: A Review of 3015 Cases. J. Arthroplast. 2020, 35, 2451–2457. [Google Scholar] [CrossRef]
- Castrodad, I.M.D.; Recai, T.M.; Abraham, M.M.; Etcheson, J.I.; Mohamed, N.S.; Edalatpour, A.; Delanois, R.E. Rehabilitation protocols following total knee arthroplasty: A review of study designs and outcome measures. Ann. Transl. Med. 2019, 7 (Suppl. 7), S255. [Google Scholar] [CrossRef]
- Carey, K.; Morgan, J.; Lin, M.-Y.; Kain, M.S.; Creevy, W.R. Patient Outcomes Following Total Joint Replacement Surgery: A Comparison of Hospitals and Ambulatory Surgery Centers. J. Arthroplast. 2019, 35, 7–11. [Google Scholar] [CrossRef] [Green Version]
- Courtney, P.M.; Froimson, M.I.; Meneghini, R.M.; Lee, G.-C.; Della Valle, C.J. Can Total Knee Arthroplasty Be Performed Safely as an Outpatient in the Medicare Population? J. Arthroplast. 2018, 33, S28–S31. [Google Scholar] [CrossRef] [PubMed]
- Gromov, K.; Jørgensen, C.C.; Petersen, P.B.; Kjaersgaard-Andersen, P.; Revald, P.; Troelsen, A.; Kehlet, H.; Husted, H. Complications and readmissions following outpatient total hip and knee arthroplasty: A prospective 2-center study with matched controls. Acta Orthop. 2019, 90, 281–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Husted, C.; Gromov, K.; Hansen, H.K.; Troelsen, A.; Kristensen, B.B.; Husted, H. Outpatient total hip or knee arthroplasty in ambulatory surgery center versus arthroplasty ward: A randomized controlled trial. Acta Orthop. 2019, 91, 42–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, M.P.; Calkins, T.E.; Culvern, C.; Kogan, M.; Della Valle, C.J. Inpatient Versus Outpatient Hip and Knee Arthroplasty: Which Has Higher Patient Satisfaction? J. Arthroplast. 2018, 33, 3402–3406. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. Explanation of the 2011 Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence (Background Document). Oxford Centre for Evidence-Based Medicine. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/explanation-of-the-2011-ocebm-levels-of-evidence/ (accessed on 18 October 2020).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.; Misra, D.; Felson, D.; Crossley, K.; Roos, E.M. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Rheum. 2011, 63 (Suppl. 11), S208–S228. [Google Scholar] [CrossRef] [Green Version]
- Coleman, B.D.; Khan, K.M.; Maffulli, N.; Cook, J.L.; Wark, J.D. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Scand. J. Med. Sci. Sports 2000, 10, 2–11. [Google Scholar] [CrossRef]
- Lovald, S.T.; Ong, K.L.; Malkani, A.L.; Lau, E.C.; Schmier, J.; Kurtz, S.M.; Manley, M.T. Complications, Mortality, and Costs for Outpatient and Short-Stay Total Knee Arthroplasty Patients in Comparison to Standard-Stay Patients. J. Arthroplast. 2014, 29, 510–515. [Google Scholar] [CrossRef]
- Lovecchio, F.; Alvi, H.; Sahota, S.; Beal, M.; Manning, D. Is Outpatient Arthroplasty as Safe as Fast-Track Inpatient Arthroplasty? A Propensity Score Matched Analysis. J. Arthroplast. 2016, 31, 197–201. [Google Scholar] [CrossRef]
- Otero, J.E.; Gholson, J.J.; Pugely, A.; Gao, Y.; Bedard, N.A.; Callaghan, J.J. Length of Hospitalization After Joint Arthroplasty: Does Early Discharge Affect Complications and Readmission Rates? J. Arthroplast. 2016, 31, 2714–2725. [Google Scholar] [CrossRef]
- Schotanus, M.G.M.; Bemelmans, Y.F.L.; Grimm, B.; Heyligers, I.C.; Kort, N.P. Physical activity after outpatient surgery and enhanced recovery for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 25, 3366–3371. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.A.; Sanders, S.; Gerlinger, T.; Della Valle, C.; Jacobs, J.J.; Rosenberg, A.G. Outpatient Total Knee Arthroplasty with a Minimally Invasive Technique. J. Arthroplast. 2005, 20, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.A.; Kusuma, S.K.; Sanders, S.A.; Thill, E.S.; Sporer, S.M. The Feasibility and Perioperative Complications of Outpatient Knee Arthroplasty. Clin. Orthop. Relat. Res. 2009, 467, 1443–1449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arshi, A.; Leong, N.L.; D’Oro, A.; Wang, C.; Buser, Z.; Wang, J.C.; Jones, K.J.; Petrigliano, F.A.; SooHoo, N.F. Outpatient Total Knee Arthroplasty Is Associated with Higher Risk of Perioperative Complications. J. Bone Jt. Surgery-Am. Vol. 2017, 99, 1978–1986. [Google Scholar] [CrossRef] [PubMed]
- Bovonratwet, P.; Ondeck, N.T.; Nelson, S.J.; Cui, J.J.; Webb, M.L.; Grauer, J.N. Comparison of Outpatient vs Inpatient Total Knee Arthroplasty: An ACS-NSQIP Analysis. J. Arthroplast. 2017, 32, 1773–1778. [Google Scholar] [CrossRef]
- Harris, K.K.; Dawson, J.; Jones, L.D.; Beard, D.J.; Price, A.J. Extending the use of PROMs in the NHS—Using the Oxford Knee Score in patients undergoing non-operative management for knee osteoarthritis: A validation study. BMJ Open 2013, 3, e003365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beard, D.J.; Harris, K.; Dawson, J.; Doll, H.; Murray, D.W.; Carr, A.J.; Price, A.J. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J. Clin. Epidemiol. 2014, 68, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Ng, N.; MacDonald, D.; Scott, C.E.H.; Howie, C.R. One-year Oxford knee scores should be used in preference to 6-month scores when assessing the outcome of total knee arthroplasty. Knee Surg. Relat. Res. 2020, 32, 43. [Google Scholar] [CrossRef] [PubMed]
- Khow, Y.Z.; Liow, M.H.L.; Goh, G.S.; Chen, J.Y.; Lo, N.N.; Yeo, S.J. The oxford knee score minimal clinically important difference for revision total knee arthroplasty. Knee 2021, 32, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Myers, S.P.; Kutcher, M.E.; Rosengart, M.R.; Sperry, J.L.; Peitzman, A.B.; Brown, J.B.; Neal, M.D. Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism. J. Trauma Acute Care Surg. 2019, 86, 20–27. [Google Scholar] [CrossRef]
- Henry, D.A.; Carless, P.A.; Moxey, A.J.; O′Connell, D.; Stokes, B.J.; Fergusson, D.A.; Ker, K. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst. Rev. 2011, 2011, CD001886. [Google Scholar] [CrossRef]
- Ng, W.; Jerath, A.; Wasowicz, M. Tranexamic acid: A clinical review. Anestezjol. Intensywna Ter. 2015, 47, 339–350. [Google Scholar] [CrossRef]
- Jørgensen, C.C.; Kehlet, H.; The Lundbeck Foundation Centre for Fast-track Hip and Knee Replacement Collaborative group. Time course and reasons for 90-day mortality in fast-track hip and knee arthroplasty. Acta Anaesthesiol. Scand. 2017, 61, 436–444. [Google Scholar] [CrossRef]
- Hertog, A.D.; Gliesche, K.; Timm, J.; Mühlbauer, B.; Zebrowski, S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: A randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch. Orthop. Trauma Surg. 2012, 132, 1153–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, M.-H.; Kim, B.-H.; Ahn, S.-J.; Yoo, S.-H.; Kang, S.-W.; Kim, Y.-J.; Kim, D.-H. Peri-articular injections of local anaesthesia can replace patient-controlled analgesia after total knee arthroplasty: A randomised controlled study. Int. Orthop. 2015, 40, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Yang, Z.; Xie, X.; Zhao, J.; Kang, P. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: A systematic review and meta-analysis. Int. Orthop. 2015, 40, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Gillis, M.E.; Dobransky, J.; Dervin, G.F. Defining growth potential and barriers to same day discharge total knee arthroplasty. Int. Orthop. 2018, 43, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Cheng, W.; Sun, L.; Yao, Y.; Cao, Q.; Ye, S.; Qi, L.; Xu, S.; Wu, X.; Jing, J. Mini-subvastus versus medial parapatellar approach for total knee arthroplasty: A prospective randomized controlled study. Int. Orthop. 2017, 42, 543–549. [Google Scholar] [CrossRef]
- Argenson, J.-N.A.; Husted, H.; Lombardi, A.; Booth, R.E.; Thienpont, E. Global Forum: An International Perspective on Outpatient Surgical Procedures for Adult Hip and Knee Reconstruction. J. Bone Jt. Surg.-Am. Vol. 2016, 98, e55. [Google Scholar] [CrossRef] [PubMed]
- Courtney, P.M.; Boniello, A.J.; Berger, R.A. Complications Following Outpatient Total Joint Arthroplasty: An Analysis of a National Database. J. Arthroplast. 2017, 32, 1426–1430. [Google Scholar] [CrossRef]
- Kort, N.P.; Bemelmans, Y.F.L.; van der Kuy, H.; Jansen, J.; Schotanus, M.G.M. Patient selection criteria for outpatient joint arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 25, 2668–2675. [Google Scholar] [CrossRef]
- Keulen, M.H.; Asselberghs, S.; Boonen, B.; Hendrickx, R.P.; van Haaren, E.H.; Schotanus, M.G. Predictors of (Un)successful Same-Day Discharge in Selected Patients Following Outpatient Hip and Knee Arthroplasty. J. Arthroplast. 2020, 35, 1986–1992. [Google Scholar] [CrossRef]

| Part A: Only One Score to be Given for Each of the 7 Sections | |
|---|---|
| 1. Study size: number of patients | 9.1 ± 2.0 (4 to 10) |
| 2. Mean follow-up | 2.2 ± 3.0 (4 to 0) |
| 3. Surgical approach | 7.8 ± 3.1 (0 to 10) |
| 4. Type of study | 7.5 ± 5.4 (0 to 10) |
| 5. Description of diagnosis | 4.5 ± 1.6 (0 to 5) |
| 6. Descriptions of surgical technique | 6.0 ± 3.9 (0 to 10) |
| 7. Description of postoperative rehabilitation | 3.5 ± 3.4 (0 to 5) |
| Part B: Scores may be Given for Each Option in each of the 3 Sections if Applicable | |
| 1. Outcome criteria | |
| Outcome measures clearly defined | 1.4 ± 1.0 (0 to 2) |
| Timing of outcome assessment clearly stated | 1.6 ± 0.8 (0 to 2) |
| Use of outcome criteria that has reported reliability | 2.1 ± 1.4 (0 to 3) |
| General health measure included | 2.4 ± 1.3 (0 to 3) |
| 2. Procedure of assessing outcomes | |
| Participants recruited | 3.5 ± 2.4 (0 to 5) |
| Investigator independent of surgeon | 3.2 ± 1.7 (0 to 4) |
| Written assessment | 2.4 ± 1.3 (0 to 3) |
| Completion of assessment by patients themselves with minimal investigator assistance | 2.4 ± 1.3 (0 to 3) |
| 3. Description of subject selection process | |
| Selection criteria reported and unbiased | 3.5 ± 2.4 (0 to 5) |
| Recruitment rate reported > 80% | 3.9 ± 2.2 (0 to 5) |
| Author, Year | Journal | Design | Follow-up (Months) | Treatment | Patients (n) | Mean Age | Women (%) | Mean BMI |
|---|---|---|---|---|---|---|---|---|
| Carey et al., 2019 [17] | J. Arthroplasty | Retrospective | 3 | Outpatient | 858 | 61.0 | ||
| Inpatient | 2574 | 61.0 | ||||||
| Courtney et al., 2018 [18] | J. Arthroplasty | Retrospective | 1 | Outpatient | 365 | 72.3 | 62 | 31.8 |
| Inpatient | 45,738 | 72.8 | 63 | 31.8 | ||||
| Gromov et al., 2019 [19] | Acta Orthop. | Prospective | 3 | Outpatient | 46 | 61.0 | 41 | 28.0 |
| Inpatient | 134 | 62.0 | 43 | 28.0 | ||||
| Husted et al., 2019 [20] | Acta Orthop. | RCT | 3 | Outpatient | 16 | 58.0 | 8 | 28.0 |
| Inpatient | 14 | 63.0 | 64 | 29.0 | ||||
| Kelly et al., 2018 [21] | J. Arthroplasty | Prospective | Outpatient | 21 | 59.2 | 58 | 30.4 | |
| Inpatient | 61 | 64.1 | 28 | 32.7 | ||||
| Kolisek et al., 2009 [1] | Clin. Orthop. Relat. Res. | Prospective | 12 | Outpatient | 64 | 55.0 | 38 | 30.8 |
| Inpatient | 64 | 55.0 | 38 | 30.8 | ||||
| Lovald et al., 2014 [26] | J. Arthroplasty | Retrospective | 24 | Outpatient | 454 | 68.0 | ||
| Inpatient | 71,341 | 71.0 | ||||||
| Lovecchio et al., 2016 [27] | J. Arthroplasty | Prospective | 3 | Outpatient | 309 | 64.0 | 56 | 30.0 |
| Inpatient | 891 | 64.0 | 55 | 31.0 | ||||
| Otero et al., 2016 [28] | J. Arthroplasty | Prospective | 1 | Outpatient | 379 | 65.2 | 58 | 32.5 |
| Inpatient | 35,870 | 67.3 | 66 | 32.9 | ||||
| Schotanus et al., 2016 [29] | Knee Surg. Sport Traumatol. Arthrosc. | Prospective | 2 | Outpatient | 10 | 64.1 | 20 | 27.7 |
| Inpatient | 10 | 66.9 | 50 | 29.2 | ||||
| Overall | 159,219 | 63.7 | 46.8% | 30.3 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Migliorini, F.; Pintore, A.; Cipollaro, L.; Oliva, F.; Maffulli, N. Outpatient Total Knee Arthroplasty: A Meta-Analysis. Appl. Sci. 2021, 11, 9376. https://doi.org/10.3390/app11209376
Migliorini F, Pintore A, Cipollaro L, Oliva F, Maffulli N. Outpatient Total Knee Arthroplasty: A Meta-Analysis. Applied Sciences. 2021; 11(20):9376. https://doi.org/10.3390/app11209376
Chicago/Turabian StyleMigliorini, Filippo, Andrea Pintore, Lucio Cipollaro, Francesco Oliva, and Nicola Maffulli. 2021. "Outpatient Total Knee Arthroplasty: A Meta-Analysis" Applied Sciences 11, no. 20: 9376. https://doi.org/10.3390/app11209376
APA StyleMigliorini, F., Pintore, A., Cipollaro, L., Oliva, F., & Maffulli, N. (2021). Outpatient Total Knee Arthroplasty: A Meta-Analysis. Applied Sciences, 11(20), 9376. https://doi.org/10.3390/app11209376









