Estimating Specific Patient Organ Dose for Chest CT Examinations with Monte Carlo Method
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Patient Size Calculation
2.2. Development of Voxelized Phantom Model for Individual Patients
2.3. Organ Dose Simulations for Individual Patients
3. Results
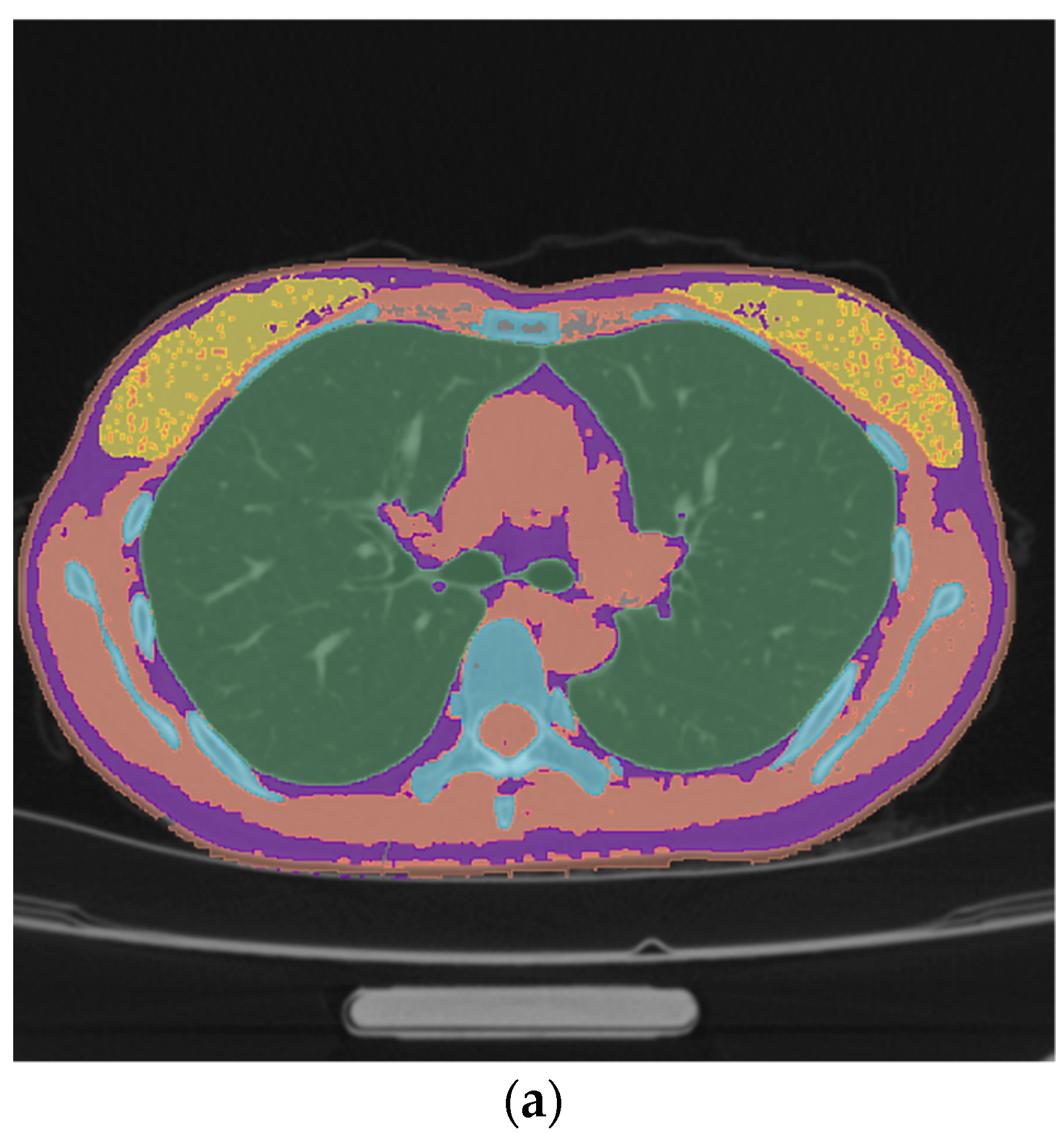
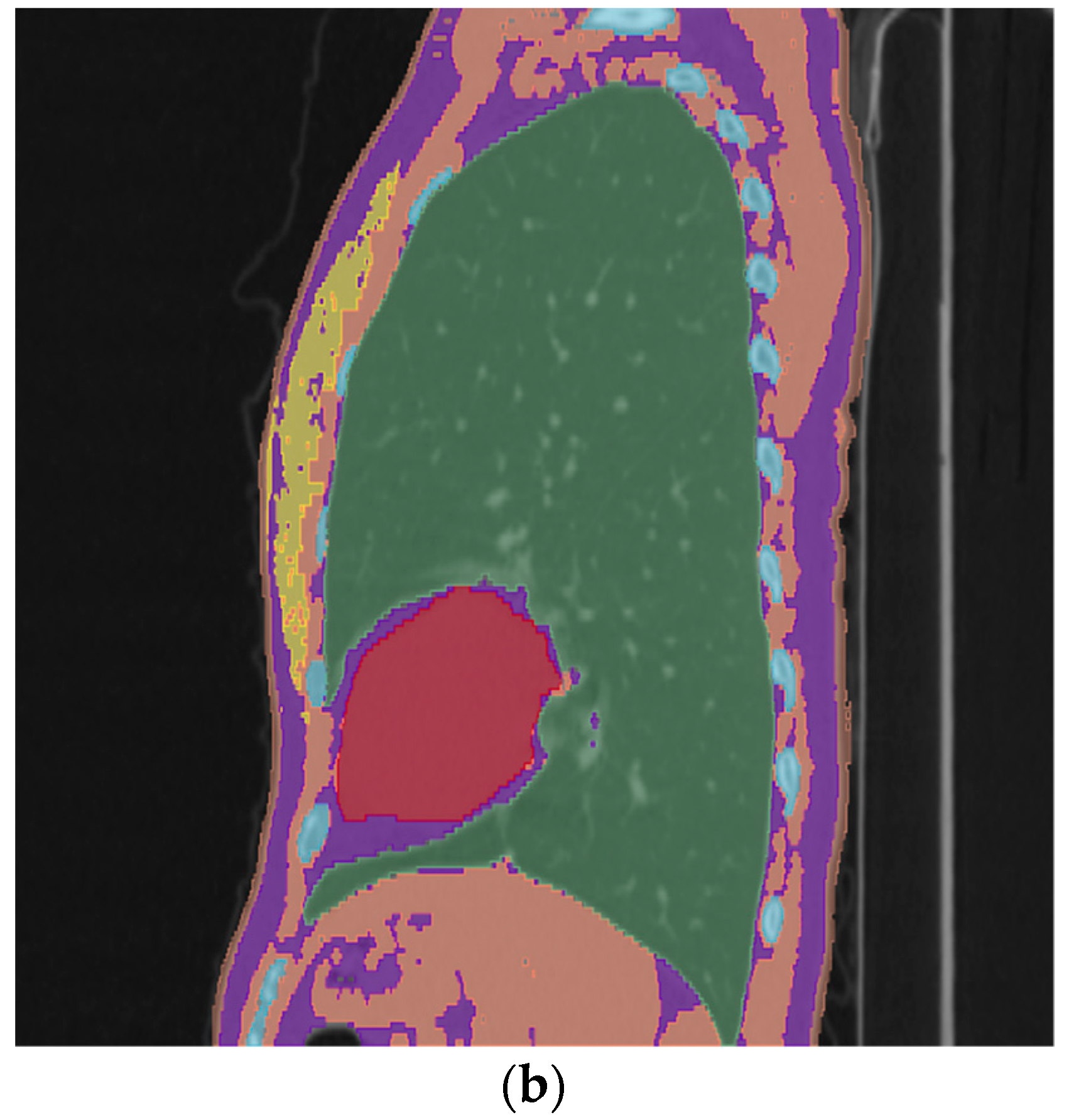
3.1. Voxelized Chest Models of Patients
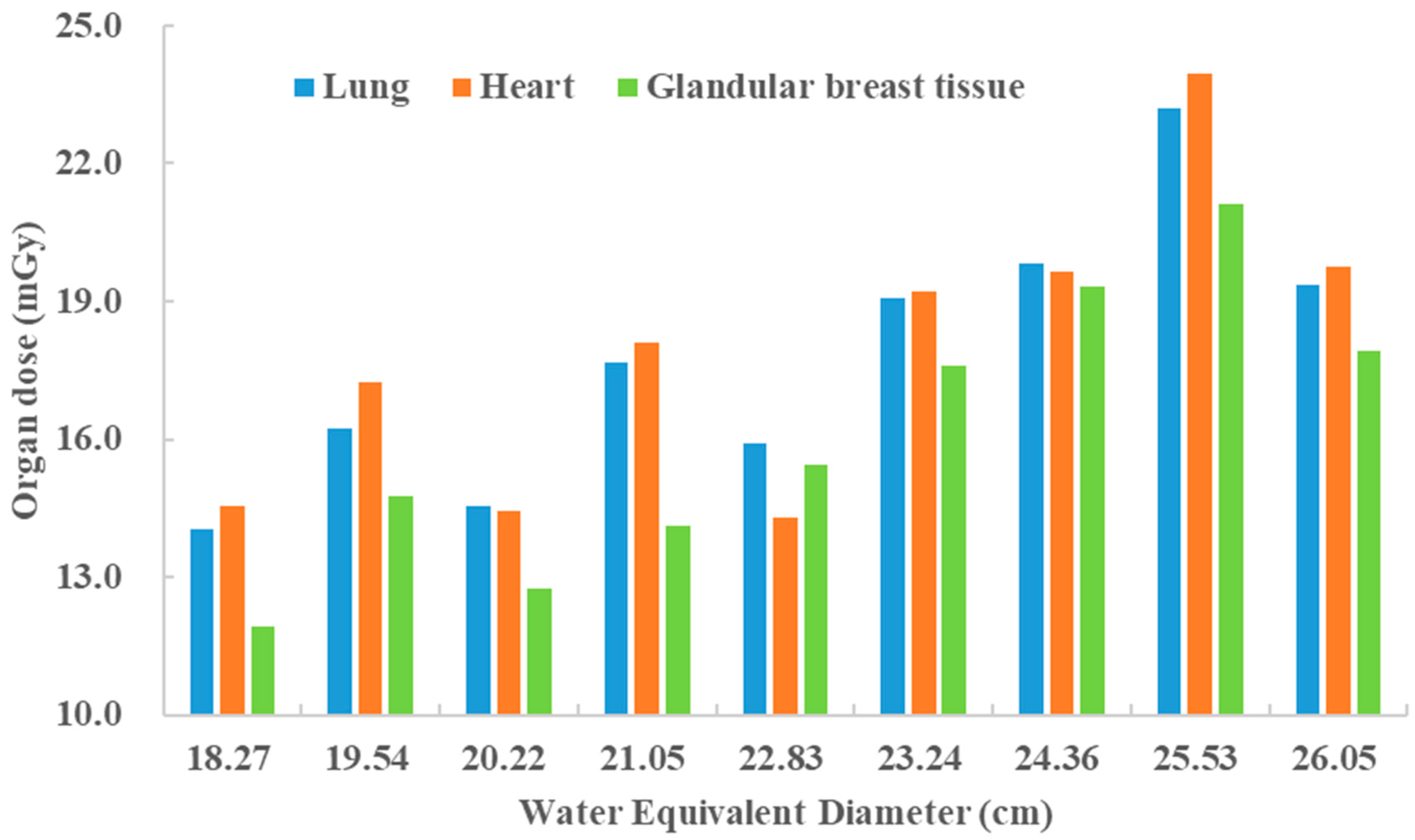
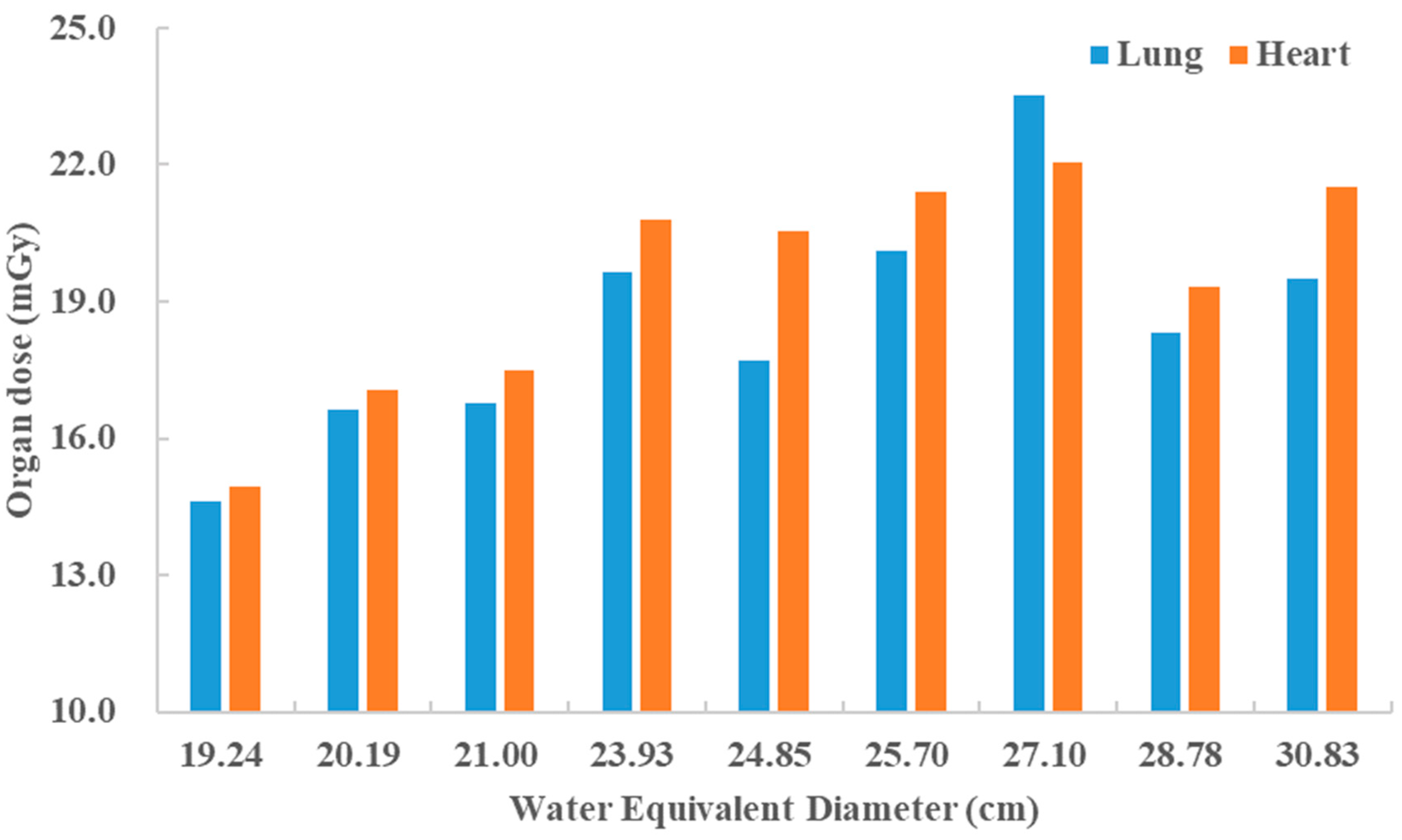
3.2. Simulated Organ Doses
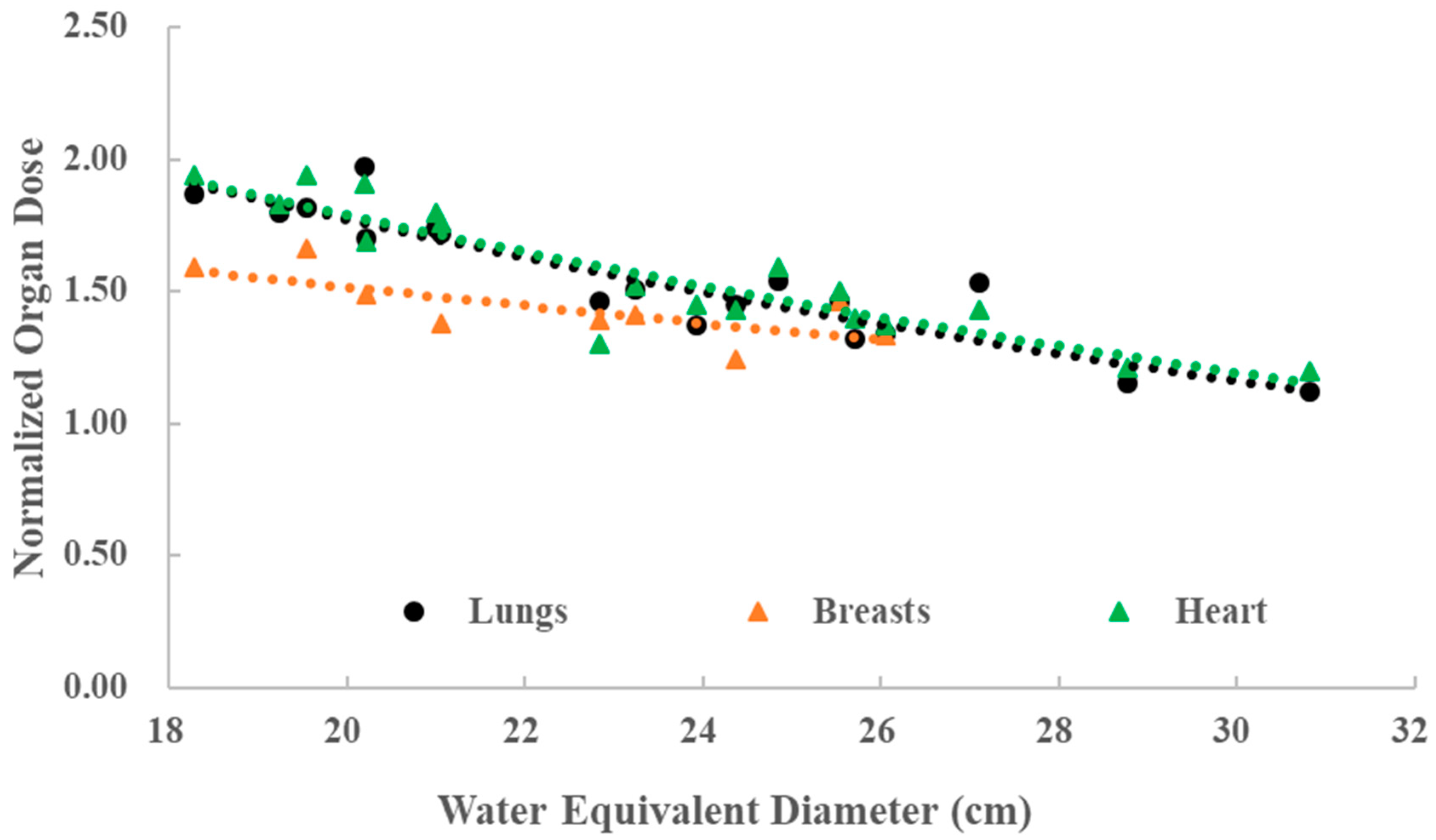
3.3. Estimation of Organ Doses with CTDIvol and WED
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Commission on Radiological Protection. Annals of the ICRP-Publication 102-Managing Patient Dose in Multi-Detector Computed Tomography (MDCT); ELSEVIER: Ottawa, ON, Canada, 2007; Volume 37. [Google Scholar]
- Shuryak, I.; Lubin, J.H.; Brenner, D.J. Potential for adult-based epidemiological studies to characterize overall cancer risks associated with a lifetime of CT scans. Radiat. Res. 2014, 181, 584–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brenner, D.J. What we know and what we don’t know about cancer risks associated with radiation doses from radiological imaging. Br. J. Radiol. 2014, 87, 20130629. [Google Scholar] [CrossRef] [PubMed]
- United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2019 Report: Sources and Effects of Ionizing Radiation. Report to the General Assembly with Scientific Annexes; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Brenner, D.J.; Hall, E.J. Computed tomography—An increasing source of radiation exposure. N. Engl. J. Med. 2007, 357, 2277–2284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCollough, C.H.; Leng, S.; Yu, L.; Cody, D.D.; Boone, J.M.; McNitt-Gray, M.F. CT dose index and patient dose: They are not the same thing. Radiology 2011, 259, 311–316. [Google Scholar] [CrossRef] [Green Version]
- American Association of Physicists in Medicine. Size-Specific Dose Estimates (SSDE) in Pediatric and Adult Body CT; Report of AAPM task group 204; American Association of Physicists in Medicine: College Park, MD, USA, 2011. [Google Scholar]
- International Electrotechnical Commission. Methods for Calculating Size Specific Dose Estimates (SSDE) on Computed Tomography; IEC 62985; International Electrotechnical Commission: Geneva, Switzerland, 2019. [Google Scholar]
- International Commission on Radiological Protection. Annals of the ICRP-Publication 110-Adult Reference Computational Phantoms; ELSEVIER: Ottawa, ON, Canada, 2009. [Google Scholar]
- Ding, A.; Gao, Y.; Liu, H.; Caracappa, P.F.; Long, D.J.; Bolch, W.E.; Liu, B.; Xu, X.G. VirtualDose: A software for reporting organ doses from CT for adult and pediatric patients. Phys. Med. Biol. 2015, 60, 5601–5625. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.; Kim, K.P.; Bolch, W.E.; Moroz, B.E.; Folio, L. NCICT: A computational solution to estimate organ doses for pediatric and adult patients undergoing CT scans. J. Radiol. Prot. 2015, 35, 891–909. [Google Scholar] [CrossRef]
- Abadi, E.; Harrawood, B.; Sharma, S.; Kapadia, A.; Segars, W.P.; Samei, E. DukeSim: A realistic, rapid, and scanner-specific simulation framework in computed tomography. IEEE Trans. Med. Imaging 2019, 38, 1457–1465. [Google Scholar] [CrossRef]
- Angel, E.; Yaghmai, N.; Jude, C.M.; DeMarco, J.J.; Cagnon, C.H.; Goldin, J.G.; McCollough, C.H.; Primak, A.N.; Cody, D.D.; Stevens, D.M.; et al. Dose to radiosensitive organs during routine chest CT: Effects of tube current modulation. AJR Am. J. Roentgenol. 2009, 193, 1340–1345. [Google Scholar] [CrossRef] [Green Version]
- Khatonabadi, M.; Kim, H.J.; Lu, P.; McMillan, K.L.; Cagnon, C.H.; DeMarco, J.J.; McNitt-Gray, M.F. The feasibility of a regional CTDIvol to estimate organ dose from tube current modulated CT exams. Med. Phys. 2013, 40, 051903. [Google Scholar] [CrossRef] [Green Version]
- Tian, X.; Li, X.; Segars, W.P.; Paulson, E.K.; Frush, D.P.; Samei, E. Pediatric chest and abdominopelvic CT: Organ dose estimation based on 42 patient models. Radiology 2014, 270, 535–547. [Google Scholar] [CrossRef]
- Bostani, M.; McMillan, K.; Lu, P.; Kim, H.J.; Cagnon, C.H.; DeMarco, J.J.; McNitt-Gray, M.F. Attenuation-based size metric for estimating organ dose to patients undergoing tube current modulated CT exams. Med. Phys. 2015, 42, 958–968. [Google Scholar] [CrossRef] [PubMed]
- Bostani, M.; McMillan, K.; Lu, P.; Kim, G.H.; Cody, D.; Arbique, G.; Greenberg, S.B.; DeMarco, J.J.; Cagnon, C.H.; McNitt-Gray, M.F. Estimating organ doses from tube current modulated CT examinations using a generalized linear model. Med. Phys. 2017, 44, 1500–1513. [Google Scholar] [CrossRef] [PubMed]
- Abuhaimed, A.; Martin, C.J. Assessment of organ doses for CT patients based on x-ray attenuation using water equivalent diameter. Radiat. Phys. Chem. 2021, 181, e109332. [Google Scholar] [CrossRef]
- McMillan, K.; Bostani, M.; Cagnon, C.H.; Yu, L.; Leng, S.; McCollough, C.H.; McNitt-Gray, M.F. Estimating patient dose from CT exams that use automatic exposure control: Development and validation of methods to accurately estimate tube current values. Med. Phys. 2017, 44, 4262–4275. [Google Scholar] [CrossRef]
- American Association of Physicists in Medicine. Use of Water Equivalent Diameter for Calculating Patient Size and Size-Specific Dose Estimates (SSDE) in CT; Report of AAPM task group 220; American Association of Physicists in Medicine: College Park, MD, USA, 2014. [Google Scholar]
- International Commission on Radiological Protection. Annals of the ICRP-Publication 89-Basic Anatomical and Physiological Data for Use in Radiological Protection; International Commission on Radiological Protection: Ottawa, ON, Canada, 2003. [Google Scholar]
- National Standard of the People’s Republic of China (NSPRC). Reference Individuals for Use in Radiation Protection: Part 1 Physique Parameters; Chinese Standard GBZ/T200.1; People’s Medical Publishing House Co., Ltd.: Beijing, China, 2007.
- National Standard of the People’s Republic of China (NSPRC). Reference Individuals for Use in Radiation Protection: Part 2 Masses of Main Organs and Tissues; Chinese Standard GBZ/T200.2; People’s Medical Publishing House Co., Ltd.: Beijing, China, 2007.
- Kalra, M.; Maher, M.; Toth, T.; Schmidt, B.; Westerman, B.; Morgan, H.; Saini, S. Techniques and applications of automatic tube current modulation for CT. Radiology 2004, 233, 549–657. [Google Scholar] [CrossRef]
- Zheng, S.; Zhang, Y.; Huang, L.; Zheng, Q.; Liu, P.; Guo, H.; Zou, T.; Yan, J. Investigation and analysis of the application frequency of medical X-CT and the dose in Fujian Province in 2016. Chin. J. Radiol. Health 2018, 6, 543–546. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; Wang, Y.; Chu, P.; Chung, R.; Einstein, A.J.; Balcombe, J.; Cocker, M.; Das, M.; Delman, B.N.; Flynn, M.; et al. International variation in radiation dose for computed tomography examinations: Prospective cohort study. BMJ 2019, 364, k4931. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y. Study on the Method for Estimating Organ Dose from X-CT Scans with Automatic Tube Current Modulation. Master’s Thesis, Radiation Medicine, Fudan University, Shanghai, China, 2018. [Google Scholar]
- Yang, Y.; Zhuo, W.; Chen, B.; Lu, S.; Zhou, P.; Ren, W.; Liu, H. A new phantom developed to test the ATCM performance of chest CT scanners. J. Radiol. Prot. 2021, 41, 349. [Google Scholar] [CrossRef]
- Punnoose, J.; Xu, J.; Sisniega, A.; Zbijewski, W.; Siewerdsen, J. Technical Note:Spektr 3.0 A computational tool for X-Ray spectrum modeling and analysis. Med. Phys. 2016, 43, 4711–4717. [Google Scholar] [CrossRef]
- Turner, A.C.; Zankl, M.; Demarco, J.J.; Cagnon, C.H.; Zhang, D.; Angel, E.; Cody, D.D.; Stevens, D.M.; McCollough, C.H.; McNitt-Gray, M.F. The feasibility of a scanner-independent technique to estimate organ dose from MDCT scans: Using CTDIvol to account for differences between scanners. Med. Phys. 2010, 37, 1816–1825. [Google Scholar] [CrossRef] [Green Version]
- Su, Y.; Lu, G.; Xiao, G.; Du, X.; Sun, Q. The study and prediction of the total number of radio-diagnosis and radiotherapy examination in hospitals. Chin. J. Radiol. Health 2017, 26, 302–305. [Google Scholar]
- Yao, J.; Gao, L.; Qian, A.; Wang, B.; Jiang, Z. Survey on frequency of medical X-ray diagnosis in Shanghai. Chin. J. Radiol. Med. Prot. 2019, 39, 370–375. [Google Scholar] [CrossRef]
| Patient ID | Age | Gender | WED (cm) | CTDIvol (mGy) | Lung Volume (cm3) | Heart Volume (cm3) | Glandular Tissue Volume of both Breasts (cm3) |
|---|---|---|---|---|---|---|---|
| 1 | 32 | F | 18.27 | 7.63 | 3461 | 609 | 233 |
| 2 | 26 | F | 19.54 | 8.89 | 3588 | 546 | 28 |
| 3 | 69 | F | 20.22 | 10.21 | 4411 | 590 | 73 |
| 4 | 44 | F | 21.05 | 8.92 | 3029 | 632 | 68 |
| 5 | 64 | F | 22.83 | 12.63 | 4200 | 659 | 72 |
| 6 | 61 | F | 23.24 | 11.34 | 3381 | 651 | 42 |
| 7 | 35 | F | 24.36 | 13.84 | 4134 | 656 | 188 |
| 8 | 70 | F | 25.53 | 16.28 | 4449 | 744 | 77 |
| 9 | 40 | F | 26.05 | 14.46 | 4023 | 636 | 303 |
| 10 | 26 | M | 19.24 | 8.76 | 4857 | 488 | ND (a) |
| 11 | 25 | M | 20.19 | 10.50 | 7746 | 760 | ND (a) |
| 12 | 44 | M | 21.00 | 10.30 | 5996 | 753 | ND (a) |
| 13 | 44 | M | 23.93 | 15.46 | 4560 | 866 | ND (a) |
| 14 | 78 | M | 24.85 | 14.50 | 5283 | 810 | ND (a) |
| 15 | 34 | M | 25.70 | 15.38 | 4334 | 754 | ND (a) |
| 16 | 49 | M | 27.10 | 14.18 | 2590 | 868 | ND (a) |
| 17 | 39 | M | 28.78 | 16.05 | 4319 | 829 | ND (a) |
| 18 | 33 | M | 30.83 | 18.31 | 3934 | 842 | ND (a) |
| Average | 45 ± 17 | 23.48 ± 3.50 (b) | 12.65 ± 3.15 | 4350 ± 1161 | 705 ± 113 | 120 ± 96 | |
| ICRP 89 | -- | M | -- | -- | 4615.38 | 807.69 | -- |
| -- | F | -- | -- | 3653.85 | 596.15 | 196.08 |
| Organ | Bostani et al. | Abuhaimed et al. | This Study | |||
|---|---|---|---|---|---|---|
| Range | Average | Range | Average | Range | Average | |
| Lung | (−13.50–17.40) % | 6.54% | (−13.70–17.92) % | 7.48% | (−13.54–16.56) % | 5.34% |
| Heart | -- | -- | (−7.18–33.20) % | 9.74% | (−7.65–25.09) % | 2.13% |
| Breast | (−18.15–25.36) % | −10.08% | -- | -- | (−8.54–5.90) % | 0.93% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Zhuo, W.; Zhao, Y.; Xie, T.; Wang, C.; Liu, H. Estimating Specific Patient Organ Dose for Chest CT Examinations with Monte Carlo Method. Appl. Sci. 2021, 11, 8961. https://doi.org/10.3390/app11198961
Yang Y, Zhuo W, Zhao Y, Xie T, Wang C, Liu H. Estimating Specific Patient Organ Dose for Chest CT Examinations with Monte Carlo Method. Applied Sciences. 2021; 11(19):8961. https://doi.org/10.3390/app11198961
Chicago/Turabian StyleYang, Yang, Weihai Zhuo, Yiyang Zhao, Tianwu Xie, Chuyan Wang, and Haikuan Liu. 2021. "Estimating Specific Patient Organ Dose for Chest CT Examinations with Monte Carlo Method" Applied Sciences 11, no. 19: 8961. https://doi.org/10.3390/app11198961
APA StyleYang, Y., Zhuo, W., Zhao, Y., Xie, T., Wang, C., & Liu, H. (2021). Estimating Specific Patient Organ Dose for Chest CT Examinations with Monte Carlo Method. Applied Sciences, 11(19), 8961. https://doi.org/10.3390/app11198961






