Risk Factors of Avulsion Fracture after Iliac Crestal Flap for Jaw Reconstruction
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
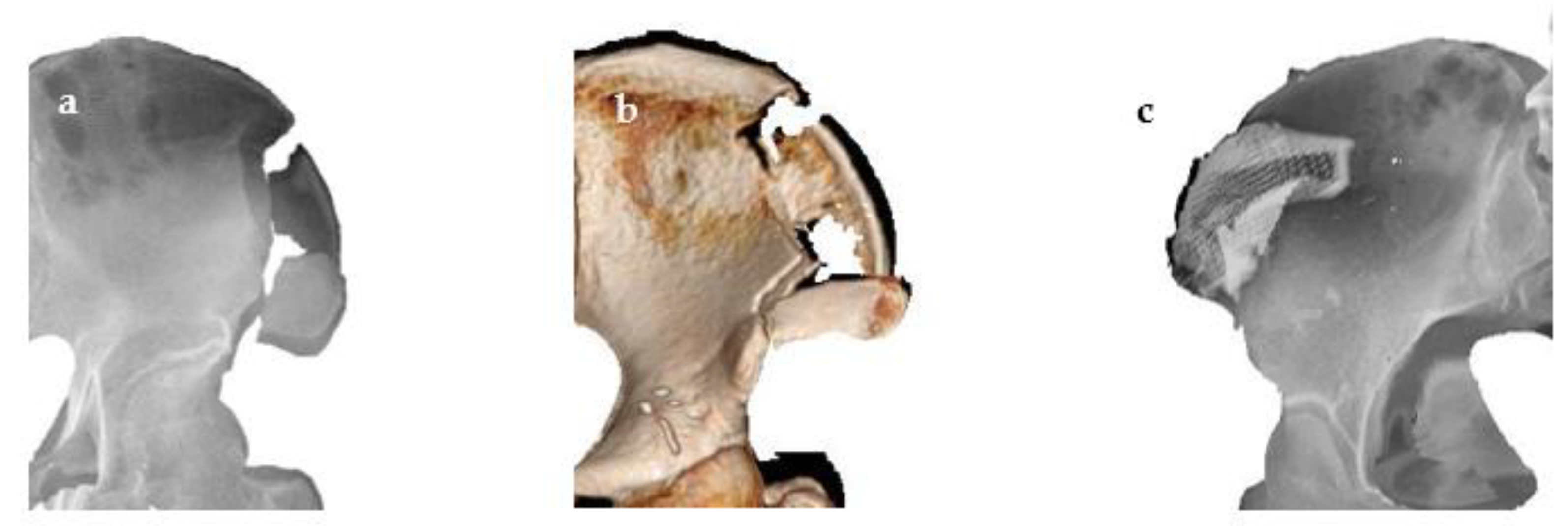
2.2. Operation and Postoperative Care
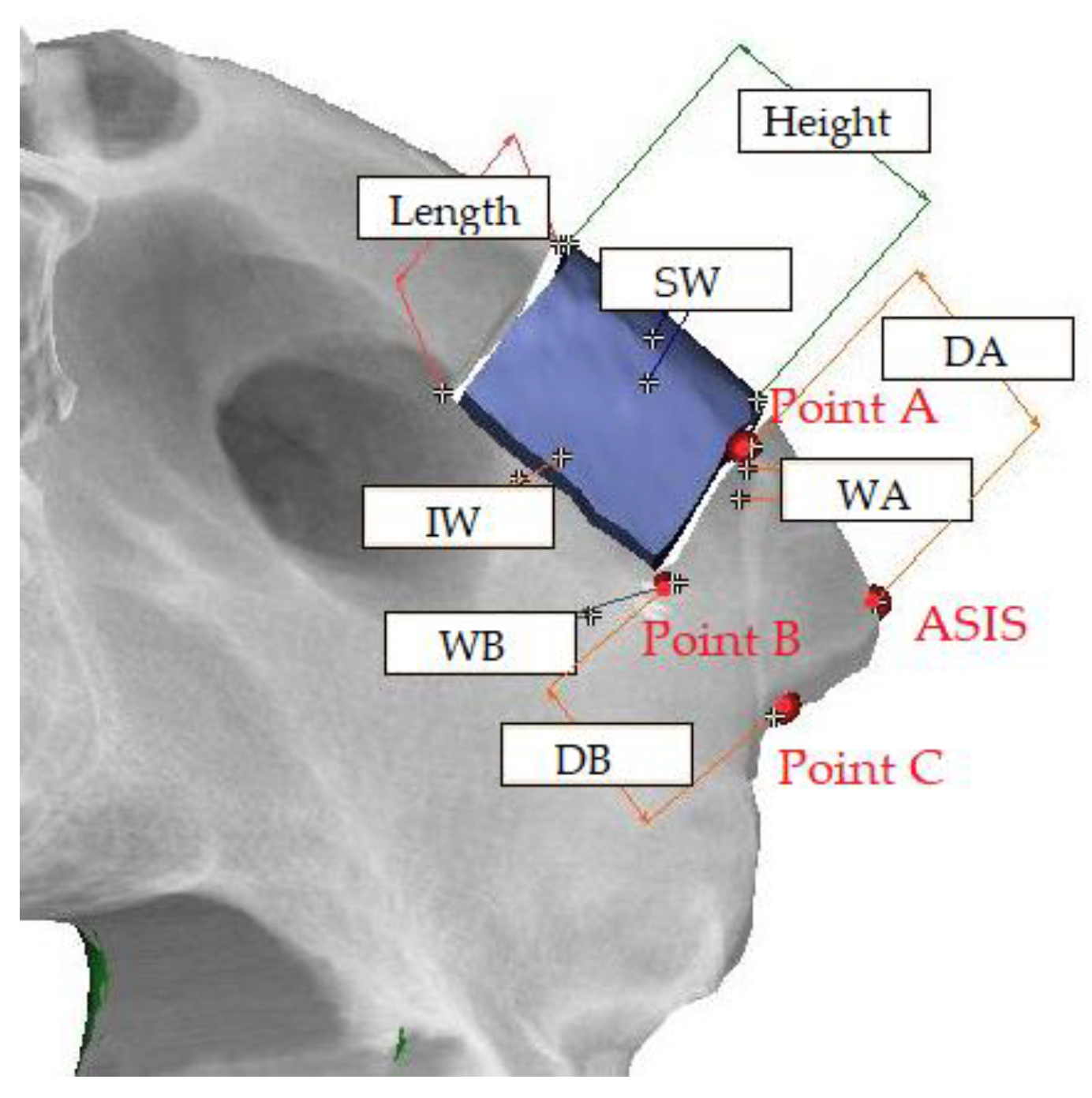
2.3. Measurement
2.4. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. Anatomical Characteristics
3.3. Postoperative Care
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arrington, E.D.; Smith, W.J.; Chambers, H.G.; Bucknell, A.L.; Davino, N.A. Complications of iliac crest bone graft harvesting. Clin. Orthop. Relat. Res. 1996, 329, 300–309. [Google Scholar] [CrossRef]
- Möhlhenrich, S.C.; Kniha, K.; Elvers, D.; Ayoub, N.; Goloborodko, E.; Hölzle, F.; Modabber, A. Intraosseous stability of dental implants in free revascularized fibula and iliac crest bone flaps. J. Cranio Maxillofac. Surg. 2016, 44, 1935–1939. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.-Y. Monocortical deep circumflex iliac artery flap in jaw reconstruction. J. Craniofac. Surg. 2015, 26, 1294–1298. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Moon, S.Y. The Deep Circumflex Iliac Artery Flap for Mandibular Reconstruction and Donor Site Reconstruction with a Patient-Specific Implant: A Case Report. Appl. Sci. 2020, 10, 1587. [Google Scholar] [CrossRef]
- İliak, K.G.A.T.A.; Kırığı, K.K. Avulsion fracture of the anterior iliac crest after bone graft harvest: Case report and review of techniques, risk factors and treatment. Turk. Neurosurg. 2011, 21, 423–426. [Google Scholar]
- Joshi, A.; Kostakis, G. An investigation of post-operative morbidity following iliac crest graft harvesting. Br. Dent. J. 2004, 196, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Westrich, G.H.; Geller, D.S.; O’Malley, M.J.; Deland, J.T.; Helfet, D.L. Anterior iliac crest bone graft harvesting using the corticocancellous reamer system. J. Orthop. Trauma 2001, 15, 500–506. [Google Scholar] [CrossRef]
- Ahlmann, E.; Patzakis, M.; Roidis, N.; Shepherd, L.; Holtom, P. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. JBJS 2002, 84, 716–720. [Google Scholar] [CrossRef]
- Hill, N.M.; Geoffrey Horne, J.; Devane, P.A. Donor site morbidity in the iliac crest bone graft. Aust. N. Z. J. Surg. 1999, 69, 726–728. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, A.; Ghassemi, M.; Modabber, A.; Knobe, M.; Fritz, U.; Riediger, D.; Gerressen, M. Functional long-term results after the harvest of vascularised iliac bone grafts bicortically with the anterior superior iliac spine included. Br. J. Oral Maxillofac. Surg. 2013, 51, e47–e50. [Google Scholar] [CrossRef]
- Nodarian, T.; Sariali, E.; Khiami, F.; Pascal-Mousselard, H.; Catonné, Y. Iliac crest bone graft harvesting complications: A case of liver herniation. Orthop. Traumatol. Surg. Res. 2010, 96, 593–596. [Google Scholar] [CrossRef][Green Version]
- Kalk, W.W.; Raghoebar, G.M.; Jansma, J.; Boering, G. Morbidity from iliac crest bone harvesting. J. Oral Maxillofac. Surg. 1996, 54, 1424–1429. [Google Scholar] [CrossRef]
- Skaggs, D.L.; Samuelson, M.A.; Hale, J.M.; Kay, R.M.; Tolo, V.T. Complications of posterior iliac crest bone grafting in spine surgery in children. Spine 2000, 25, 2400–2402. [Google Scholar] [CrossRef]
- Goulet, J.A.; Senunas, L.E.; DeSilva, G.L.; Greenfield, M.L.V. Autogenous iliac crest bone graft: Complications and functional assessment. Clin. Orthop. Relat. Res. 1997, 339, 76–81. [Google Scholar] [CrossRef]
- Schaaf, H.; Lendeckel, S.; Howaldt, H.-P.; Streckbein, P. Donor site morbidity after bone harvesting from the anterior iliac crest. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 109, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, A.; Ghassemi, M.; Riediger, D.; Hilgers, R.-D.; Gerressen, M. Comparison of donor-site engraftment after harvesting vascularized and nonvascularized iliac bone grafts. J. Oral Maxillofac. Surg. 2009, 67, 1589–1594. [Google Scholar] [CrossRef]
- Urken, M.L.; Vickery, C.; Weinberg, H.; Buchbinder, D.; Lawson, W.; Biller, H.F. The internal oblique-iliac crest osseomyocutaneous free flap in oromandibular reconstruction: Report of 20 cases. Arch. Otolaryngol. Head Neck Surg. 1989, 115, 339–349. [Google Scholar] [CrossRef]
- Ebraheim, N.A.; Yang, H.; Lu, J.; Biyani, A.; Yeasting, R.A. Anterior iliac crest bone graft: Anatomic considerations. Spine 1997, 22, 847–849. [Google Scholar] [CrossRef] [PubMed]
- Kessler, P.; Thorwarth, M.; Bloch-Birkholz, A.; Nkenke, E.; Neukam, F. Harvesting of bone from the iliac crest—Comparison of the anterior and posterior sites. Br. J. Oral Maxillofac. Surg. 2005, 43, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Babbi, L.; Barbanti-Brodano, G.; Gasbarrini, A.; Boriani, S. Iliac crest bone graft: A 23-years hystory of infection at donor site in vertebral arthrodesis and a review of current bone substitutes. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4670–4676. [Google Scholar] [PubMed]
- Al-Sayyad, M. Fracture of the anterior iliac crest following autogenous bone grafting. Saudi Med. J. 2006, 27. [Google Scholar]
- Zermatten, P.; Wettstein, M. Iliac wing fracture following graft harvesting from the anterior iliac crest: Literature review based on a case report. Orthop.Traumatol. Surg. Res. 2012, 98, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.W.; Bohlman, H. Fracture at the iliac bone graft harvest site after fusion of the spine. Clin. Orthop. Relat. Res. 1994, 208–213. [Google Scholar]
- Samartzis, D.; Shen, F.H. Postoperative iliac-crest avulsion fracture. Cmaj 2006, 175, 475. [Google Scholar] [CrossRef][Green Version]
- Nocini, P.F.; Bedogni, A.; Valsecchi, S.; Trevisiol, L.; Ferrari, F.; Fior, A.; Saia, G. Fractures of the iliac crest following anterior and posterior bone graft harvesting. Review of the literature and case presentation. Minerva Stomatol. 2003, 52, 441–448. [Google Scholar]
- Porchet, F.; Jaques, B. Unusual complications at iliac crest bone graft donor site: Experience with two cases. Neurosurgery 1996, 39, 856–858. [Google Scholar] [CrossRef] [PubMed]
- Guha, S.; Poole, M. Stress fracture of the iliac bone with subfascial femoral neuropathy: Unusual complications at a bone graft donor site: Case report. Br. J. Plast. Surg. 1983, 36, 305–306. [Google Scholar] [CrossRef]
- Fernando, T.L.; Kim, S.S.; Mohler, D.G. Complete pelvic ring failure after posterior iliac bone graft harvesting. Spine 1999, 24, 2101. [Google Scholar] [CrossRef]
- Jones, A.; Dougherty, P.; Sharkey, N.; Benson, D. Iliac crest bone graft. Osteotome versus saw. Spine 1993, 18, 2048–2052. [Google Scholar] [CrossRef]
- Hu, R.; Hearn, T.; Yang, J. Bone Graft Harvest Site As a Determinant of Iliac Crest Strength. Clin. Orthop. Relat. Res. 1995, 252–256. [Google Scholar] [CrossRef]
- Behairy, Y.M.; Al-Sebai, W. A modified technique for harvesting full-thickness iliac crest bone graft. Spine 2001, 26, 695–697. [Google Scholar] [CrossRef] [PubMed]
- Steffen, T.; Downer, P.; Steiner, B.; Hehli, M.; Aebi, M. Minimally invasive bone harvesting tools. Eur. Spine J. 2000, 9, S114–S118. [Google Scholar] [CrossRef][Green Version]
- Sàndor, G.K.; Rittenberg, B.N.; Clokie, C.M.; Caminiti, M.F. Clinical success in harvesting autogenous bone using a minimally invasive trephine. J. Oral Maxillofac. Surg. 2003, 61, 164–168. [Google Scholar] [CrossRef]
- Nkenke, E.; Weisbach, V.; Winckler, E.; Kessler, P.; Schultze-Mosgau, S.; Wiltfang, J.; Neukam, F. Morbidity of harvesting of bone grafts from the iliac crest for preprosthetic augmentation procedures: A prospective study. Int. J. Oral Maxillofac. Surg. 2004, 33, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Barone, A.; Ricci, M.; Mangano, F.; Covani, U. Morbidity associated with iliac crest harvesting in the treatment of maxillary and mandibular atrophies: A 10-year analysis. J. Oral Maxillofac. Surg. 2011, 69, 2298–2304. [Google Scholar] [CrossRef] [PubMed]
- Sasso, R.C.; LeHuec, J.C.; Shaffrey, C.; Group, S.I.R. Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: A prospective patient satisfaction outcome assessment. Clin. Spine Surg. 2005, 18, S77–S81. [Google Scholar] [CrossRef] [PubMed]
- Swan, M.; Goodacre, T. Morbidity at the iliac crest donor site following bone grafting of the cleft alveolus. Br. J. Oral Maxillofac. Surg. 2006, 44, 129–133. [Google Scholar] [CrossRef]
- Robertson, P.A.; Wray, A.C. Natural history of posterior iliac crest bone graft donation for spinal surgery: A prospective analysis of morbidity. Spine 2001, 26, 1473–1476. [Google Scholar] [CrossRef]
- Huemer, G.M.; Puelacher, W.; Schoeller, T. Improving the iliac crest donor site by plate insertion after harvesting vascularized bone. J. Cranio Maxillofac. Surg. 2004, 32, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Ito, M.; Abumi, K.; Moridaira, H.; Shono, Y.; Kotani, Y.; Minami, A.; Kaneda, K. Iliac crest reconstruction with a bioactive ceramic spacer. Eur. Spine J. 2005, 14, 99–102. [Google Scholar] [CrossRef]
- Halsnad, S.; Dhariwal, D.; Bocca, A.; Evans, P.; Hodder, S. Titanium plate reconstruction of the osseous defect after harvest of a composite free flap using the deep circumflex iliac artery. Br. J. Oral Maxillofac. Surg. 2004, 42, 254–256. [Google Scholar] [CrossRef]
- Chan, K.; Resnick, D.; Pathria, M.; Jacobson, J. Pelvic instability after bone graft harvesting from posterior iliac crest: Report of nine patients. Skelet. Radiol. 2001, 30, 278–281. [Google Scholar] [CrossRef]
- Reale, F.; Gambacorta, D.; Mencattini, G. Iliac crest fracture after removal of two bone plugs for anterior cervical fusion: Case report. J. Neurosurg. 1979, 51, 560–561. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, A.F.; Turner, P.T.; Loeser, J.D. Fracture of the anterior superior iliac spine following anterior cervical fusion using iliac crest: Case report. J. Neurosurg. 1978, 48, 809–810. [Google Scholar] [CrossRef] [PubMed]
- Burstein, F.D.; Simms, C.; Cohen, S.R.; Work, F.; Paschal, M. Iliac crest bone graft harvesting techniques: A comparison. Plast. Reconstr. Surg. 2000, 105, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Eufinger, H.; Leppänen, H. Iliac crest donor site morbidity following open and closed methods of bone harvest for alveolar cleft osteoplasty. J. Cranio Maxillofac. Surg. 2000, 28, 31–38. [Google Scholar] [CrossRef]
- Brawley, S.C.; Simpson, R.B. Results of an alternative autogenous iliac crest bone graft harvest method. Orthopedics 2006, 29, 342. [Google Scholar] [CrossRef]
- Neo, M.; Matsushita, M.; Morita, T.; Nakamura, T. Pseudoaneurysm of the deep circumflex iliac artery: A rare complication at an anterior iliac bone graft donor site. Spine 2000, 25, 1848–1851. [Google Scholar] [CrossRef]
- Friend, K.D.; Koval, K.J.; Mirovsky, Y.; Remer, S.S.; Bloom, N.; Neuwirth, M.G. Fracture of the iliac crest following bone grafting: A case report and literature review. Bull. Hosp. Jt. Dis. 1995, 54, 49–51. [Google Scholar]
| Non-Fracture | Fracture | Total | |
|---|---|---|---|
| Male | 9 | 2 | 11 |
| Female | 10 | 1 | 11 |
| Total | 19 | 3 | 22 |
| p-value | 0.295 | ||
| Age | Non-Fracture | Fracture | Total |
|---|---|---|---|
| 10–19 | 2 | 0 | 2 |
| 20–29 | 1 | 0 | 1 |
| 30–39 | 1 | 0 | 1 |
| 40–49 | 2 | 0 | 2 |
| 50–59 | 4 | 1 | 5 |
| 60–69 | 7 | 0 | 7 |
| 70–79 | 6 | 2 | 8 |
| <80 | 1 | 0 | 1 |
| p-value | 0.557 | ||
| (Mean ± S.D.) | ||||
|---|---|---|---|---|
| (mm) | DA | DB | WA | WB |
| 1 | 33.36 | 29.12 | 14.84 | 11.15 |
| 2 | 14.78 | 13.92 | 14.98 | 9.32 |
| 3 | 18.69 | 19.80 | 21.34 | 19.67 |
| Mean | 22.28 ± 9.80 | 20.95 ± 7.66 | 17.05 ± 3.71 | 13.38 ± 5.52 |
| (Mean ± S.D.) | ||||
|---|---|---|---|---|
| (mm) | Height | Length | SW | IW |
| 1 | 33.36 | 29.12 | 14.84 | 11.15 |
| 2 | 14.78 | 13.92 | 14.98 | 9.32 |
| 3 | 18.69 | 19.80 | 21.34 | 19.67 |
| Mean | 22.28 ± 9.80 | 20.95 ± 7.66 | 17.05 ± 3.71 | 13.38 ± 5.52 |
| (Mean ± S.D.) | ||||
|---|---|---|---|---|
| (mm) | DA | DB | WA | WB |
| Non-fracture | 16.88 ± 4.54 | 17.29 ± 4.44 | 13.63 ± 1.58 | 10.74 ± 1.63 |
| Fracture | 22.28 ± 9.80 | 20.95 ± 7.66 | 17.05 ± 3.71 | 13.38 ± 5.52 |
| p-value | 0.237 | 0.586 | 0.032 * | 0.705 |
| (Mean ± S.D.) | ||||
|---|---|---|---|---|
| (mm) | Height | Length | SW | IW |
| Non-fracture | 22.00 ± 5.37 | 11.86 ± 2.04 | 16.75 ± 2.01 | 11.86 ± 2.04 |
| Fracture | 22.85 ± 5.83 | 10.07 ± 4.31 | 13.65 ± 2.77 | 10.07 ± 4.31 |
| p-value | 0.953 | 0.441 | 0.110 | 0.441 |
| (Mean ± S.D.) | |
|---|---|
| ABR Period | |
| Non-fracture | 10.50 ± 3.61 |
| Fracture | 5.67 ± 2.31 |
| p-value | 0.045 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, Y.-J.; Choi, J.-S.; Bang, J.-A.; Kim, J.; Moon, S.-Y. Risk Factors of Avulsion Fracture after Iliac Crestal Flap for Jaw Reconstruction. Appl. Sci. 2021, 11, 8081. https://doi.org/10.3390/app11178081
Jo Y-J, Choi J-S, Bang J-A, Kim J, Moon S-Y. Risk Factors of Avulsion Fracture after Iliac Crestal Flap for Jaw Reconstruction. Applied Sciences. 2021; 11(17):8081. https://doi.org/10.3390/app11178081
Chicago/Turabian StyleJo, Ye-Joon, Jun-Seok Choi, Jin-Ah Bang, Jin Kim, and Seong-Yong Moon. 2021. "Risk Factors of Avulsion Fracture after Iliac Crestal Flap for Jaw Reconstruction" Applied Sciences 11, no. 17: 8081. https://doi.org/10.3390/app11178081
APA StyleJo, Y.-J., Choi, J.-S., Bang, J.-A., Kim, J., & Moon, S.-Y. (2021). Risk Factors of Avulsion Fracture after Iliac Crestal Flap for Jaw Reconstruction. Applied Sciences, 11(17), 8081. https://doi.org/10.3390/app11178081









