Basic Knowledge and New Advances in Panoramic Radiography Imaging Techniques: A Narrative Review on What Dentists and Radiologists Should Know
Abstract
:1. Introduction
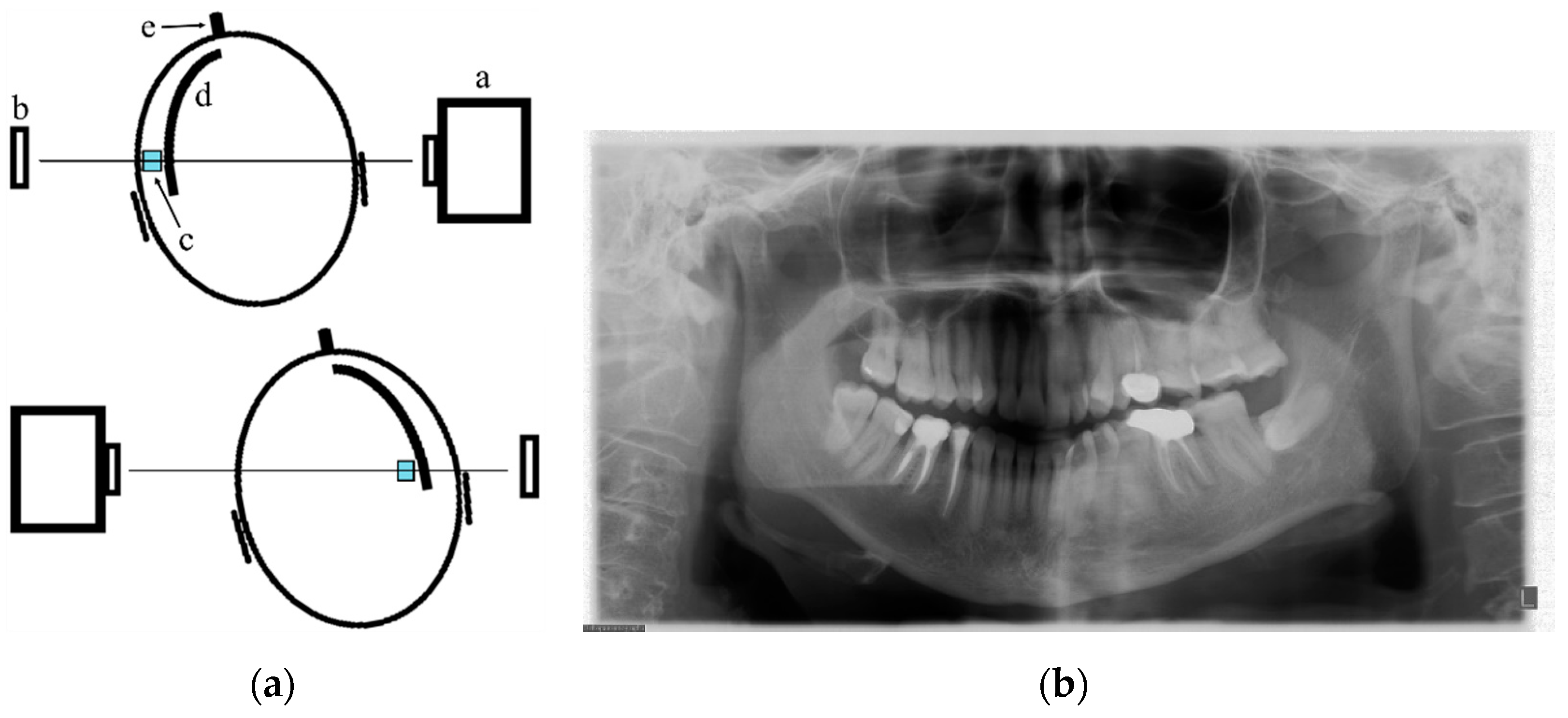
2. PAN Acquisition Principles
3. The Variables of a Correct PAN Examination
4. Frequency of Errors in PAN Performance and Interpretation
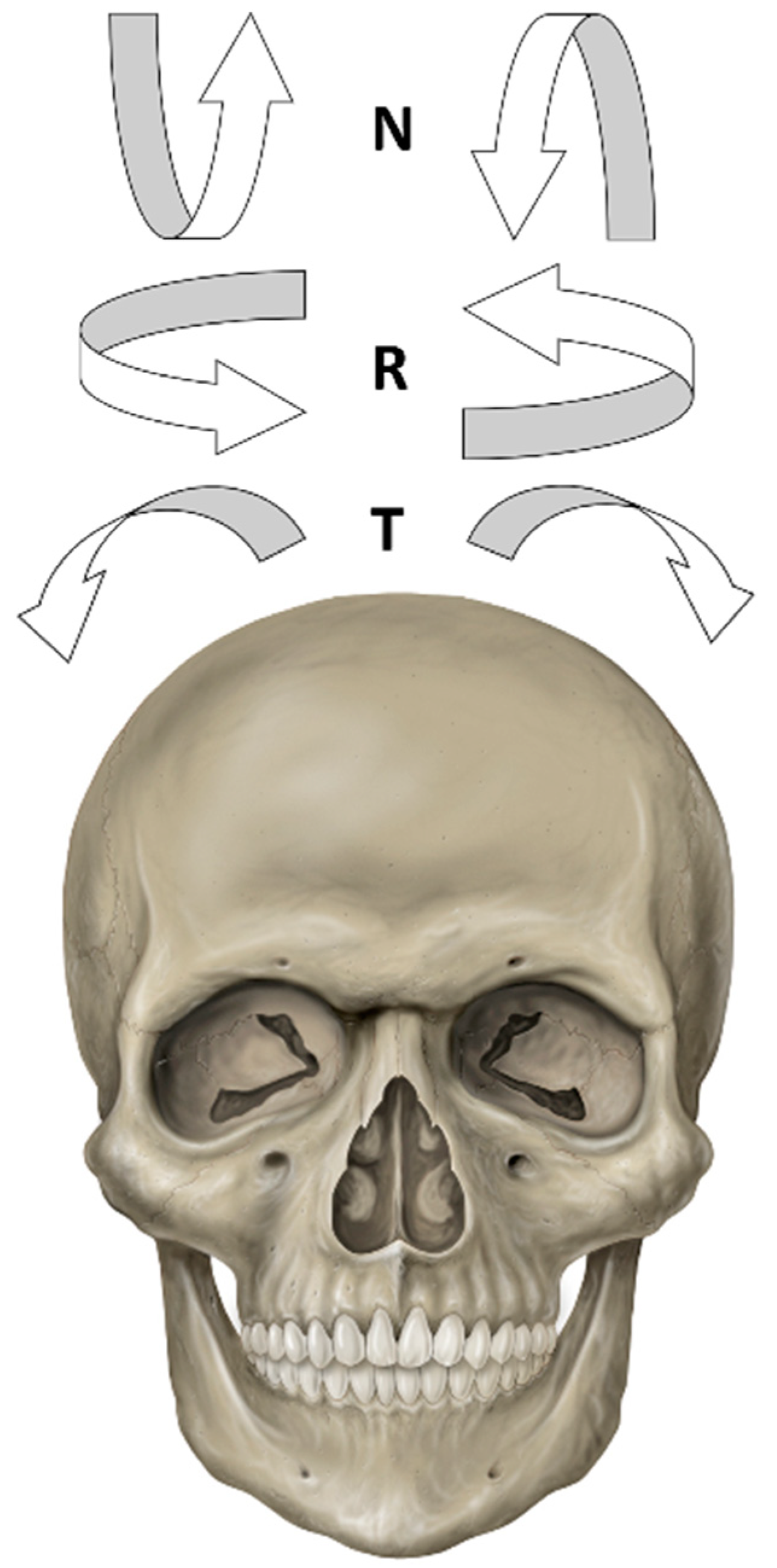
5. The Importance of Head Orientation
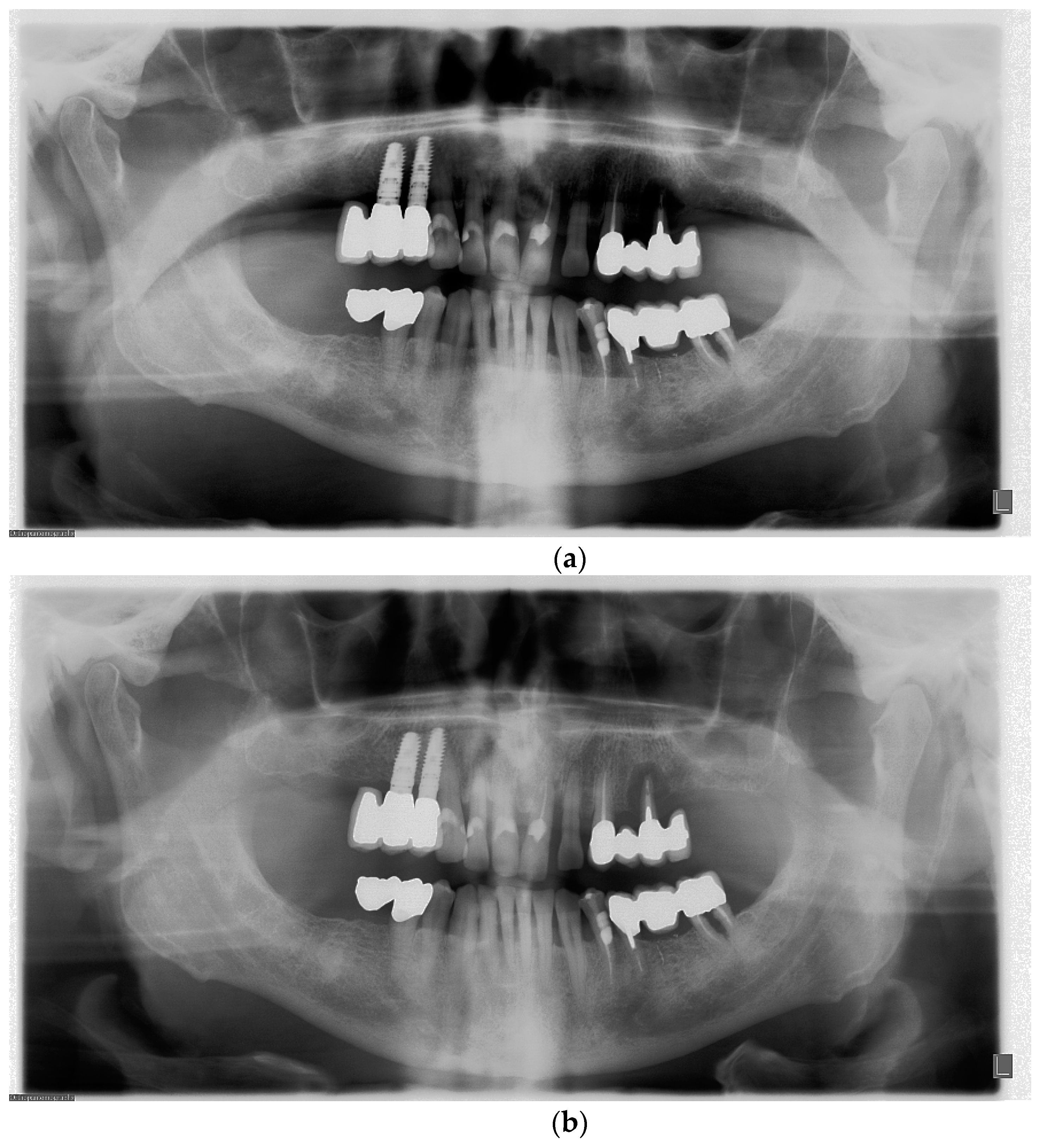
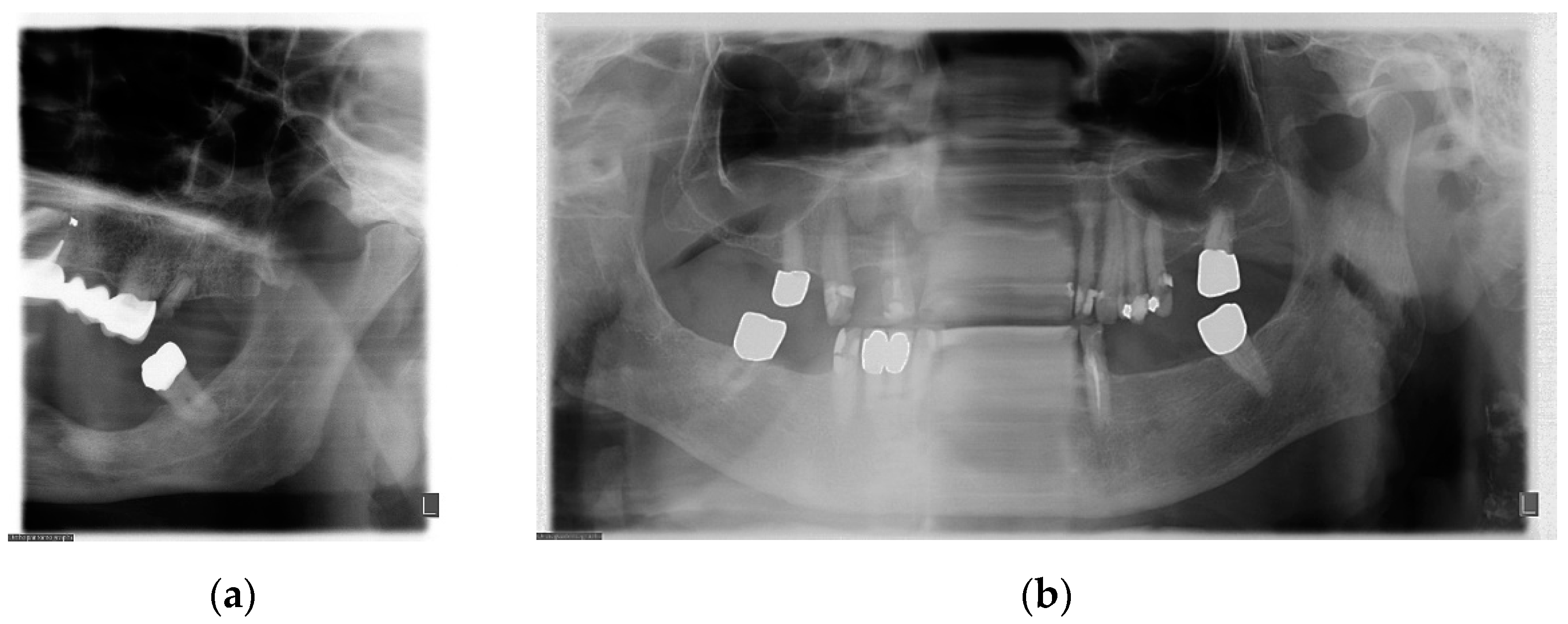
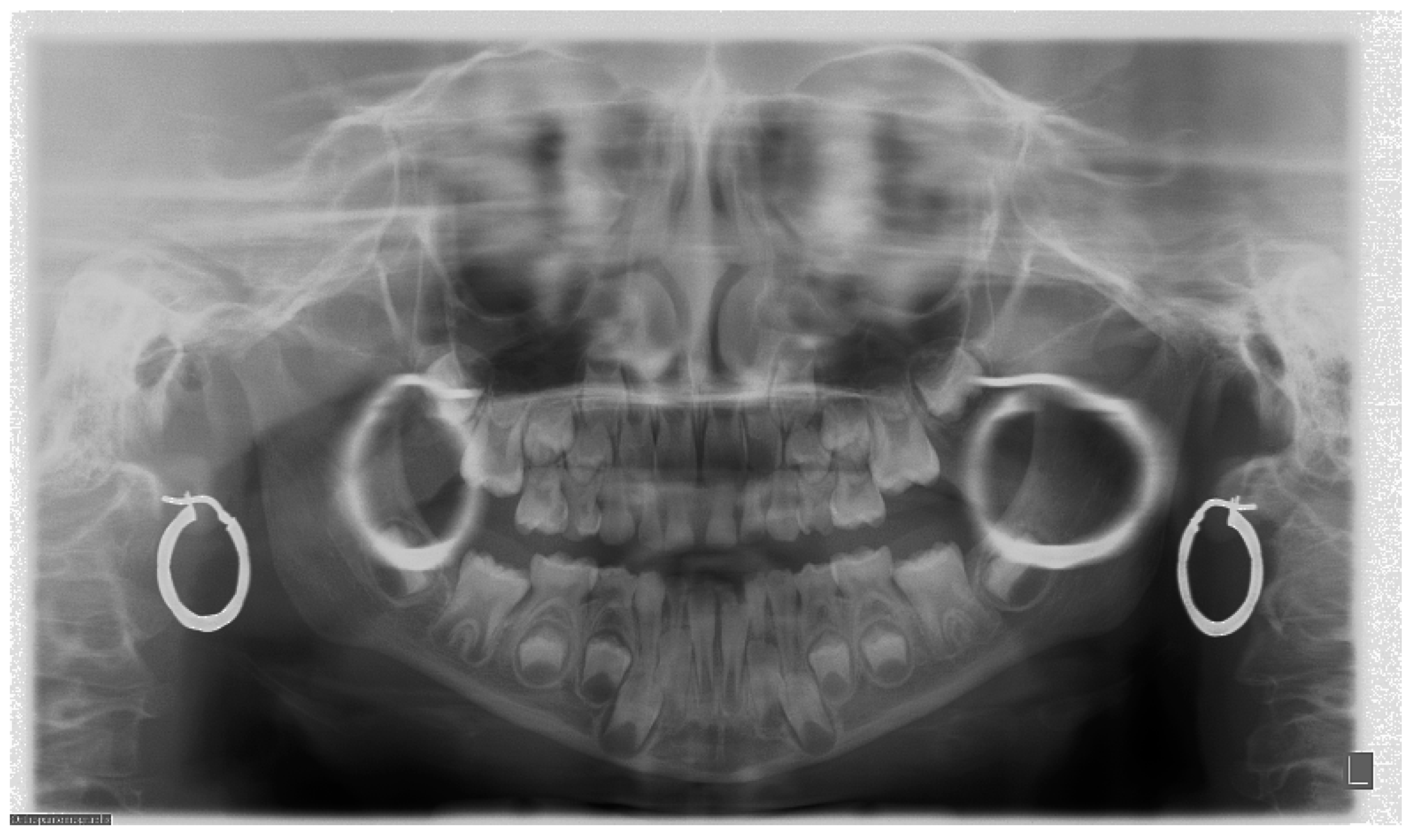
6. Evaluation of PAN Examination
6.1. Symmetry
6.2. Inclination of the Occlusal Plane
6.3. Localization of Mandibular Condyles
6.4. Aspect of Upper Teeth Root Apexes
6.5. Position of the Cervical Spine
6.6. Exposure Parameters and Radiation Dose
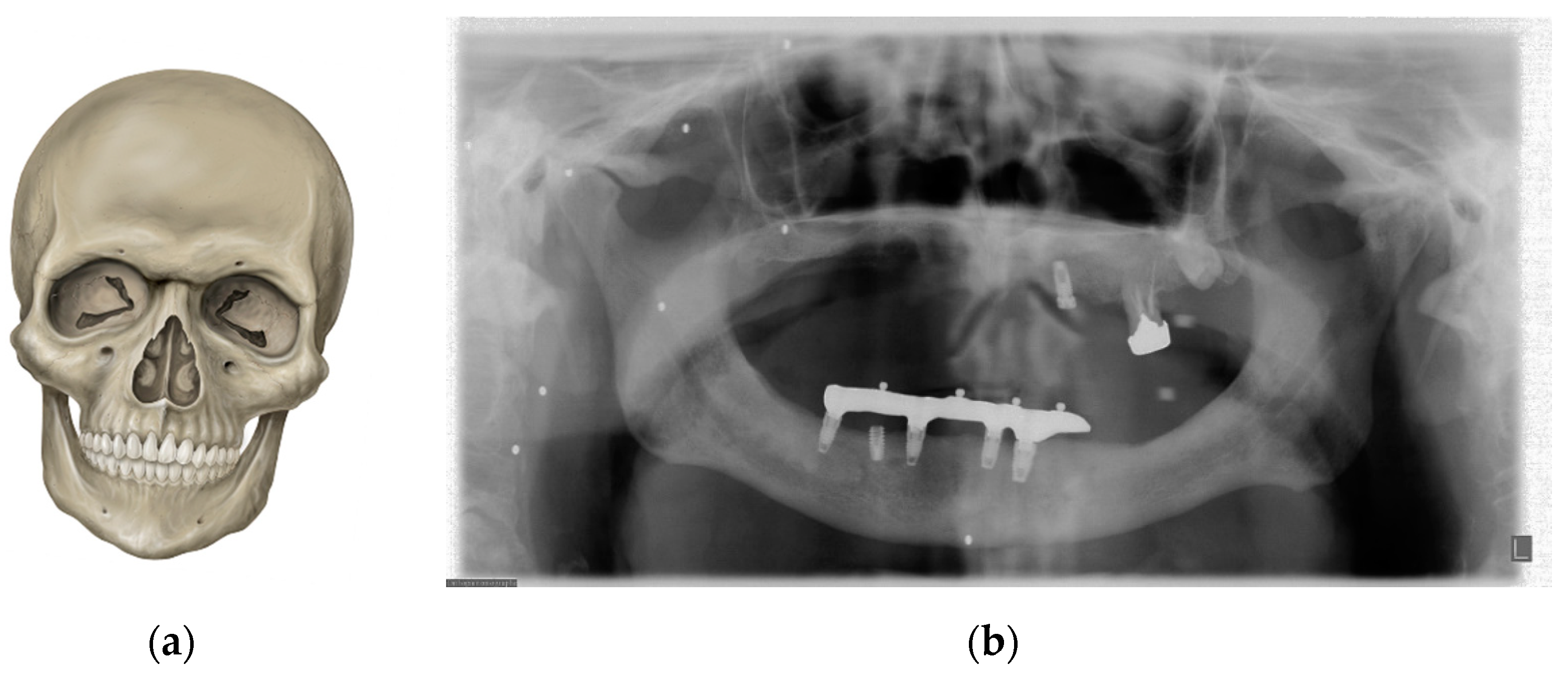
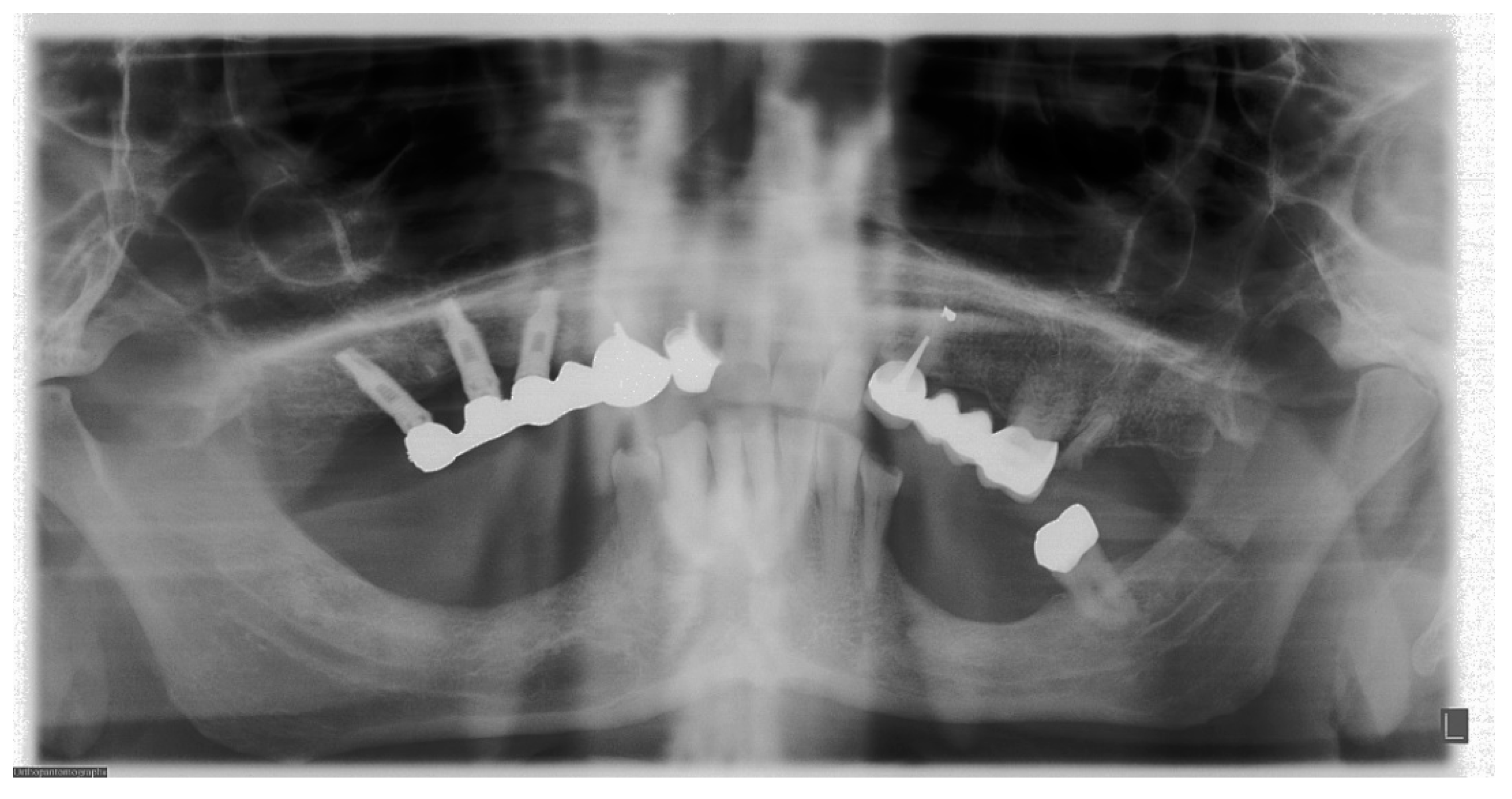
7. Metal and Motion Artefacts
8. Newest Advances for PAN in a Digital Era
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Dental Association Council on Scientific Affairs. The use of dental radiographs: Update and recommendations. J. Am. Dent. Assoc. 2006, 137, 1304–1312. [Google Scholar] [CrossRef]
- Nardi, C.; Calistri, L.; Pradella, S.; Desideri, I.; Lorini, C.; Colagrande, S. Accuracy of Orthopantomography for Apical Periodontitis without Endodontic Treatment. J. Endod. 2017, 43, 1640–1646. [Google Scholar] [CrossRef]
- Sun, W.; Xia, K.; Tang, L.; Liu, C.; Zou, L.; Liu, J. Accuracy of panoramic radiography in diagnosing maxillary sinus-root relationship: A systematic review and meta-analysis. Angle Orthod. 2018, 88, 819–829. [Google Scholar] [CrossRef]
- DeAngelis, A.F.; Barrowman, R.A.; Harrod, R.; Nastri, A.L. Review article: Maxillofacial emergencies: Maxillofacial trauma. Emerg. Med. Australas. 2014, 26, 530–537. [Google Scholar] [CrossRef]
- Chayra, G.A.; Meador, L.R.; Laskin, D.M. Comparison of panoramic and standard radiographs for the diagnosis of mandibular fractures. J. Oral Maxillofac. Surg. 1986, 44, 677. [Google Scholar] [CrossRef]
- Commission, I.E. Evaluation and Routine Testing in Medical Imaging Departments-Part 3–4: Acceptance Tests-Imaging Performance of Dental X-ray Equipment. IEC 61223–3–4; International Electrotechnical Commission: Geneva, Switzerland, 2000. [Google Scholar]
- Yeom, H.G.; Kim, J.E.; Huh, K.H.; Yi, W.-J.; Heo, M.-S.; Lee, S.-S.; Choi, S.-C.; Lee, S.-J. Development of panorama resolution phantom for comprehensive evaluation of the horizontal and vertical resolution of panoramic radiography. Sci. Rep. 2020, 10, 16529. [Google Scholar] [CrossRef]
- Brüllmann, D.; Schulze, R.K. Spatial resolution in CBCT machines for dental/maxillofacial applications-what do we know today? Dentomaxillofacial Radiol. 2015, 44, 20140204. [Google Scholar] [CrossRef] [Green Version]
- Edge, M.B.; Champion, C. Interpretation of the orthopantomogram. Complications due to radiographic artifacts. Br. Dent. J. 1972, 133, 289–296. [Google Scholar] [CrossRef]
- Sklavos, A.; Beteramia, D.; Delpachitra, S.N.; Kumar, R. The panoramic dental radiograph for emergency physicians. Emerg. Med. J. 2019, 36, 565–571. [Google Scholar] [CrossRef]
- Nardi, C.; Talamonti, C.; Pallotta, S.; Saletti, P.; Calistri, L.; Cordopatri, C.; Colagrande, S. Head and neck effective dose and quantitative assessment of image quality: A study to compare cone beam CT and multislice spiral CT. Dentomaxillofacial Radiol. 2017, 46, 20170030. [Google Scholar] [CrossRef]
- Schiff, T.; D’Ambrosio, J.; Glass, B.J.; Langlais, R.P.; McDavid, W.D. Common positioning and technical errors in panoramic radiography. J. Am. Dent. Assoc. 1986, 113, 422–426. [Google Scholar] [CrossRef]
- Akarslan, Z.Z.; Erten, H.; Güngör, K.; Çelik, L. Common errors on panoramic radiographs taken in a dental school. J. Contemp. Dent. Pract. 2003, 4, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, P.; Bewersdorf, S.; Schmage, P. The effect of changes in head position on enlargement of structures during panoramic radiography. Int. J. Oral Maxillofac. Implant. 2012, 27, 55–63. [Google Scholar]
- Dhillon, M.; Raju, S.M.; Verma, S.; Tomar, D.; Mohan, R.S.; Lakhanpal, M.; Krishnamoorthy, B. Positioning errors and quality assessment in panoramic radiography. Imaging Sci. Dent. 2012, 42, 207–212. [Google Scholar] [CrossRef] [Green Version]
- Rondon, R.H.; Pereira, Y.C.; do Nascimento, G.C. Common positioning errors in panoramic radiography: A review. Imaging Sci. Dent. 2014, 44, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Peretz, B.; Gotler, M.; Kaffe, I. Common errors in digital panoramic radiographs of patients with mixed dentition and patients with permanent dentition. Int. J. Dent. 2012, 2012, 584138. [Google Scholar] [CrossRef] [PubMed]
- Ekströmer, K.; Hjalmarsson, L. Positioning errors in panoramic images in general dentistry in Sormland County, Swedan. Swed. Dent. J. 2014, 38, 31–38. [Google Scholar] [PubMed]
- Riecke, B.; Friedrich, R.E.; Schulze, D.; Loos, C.; Blessmann, M.; Heiland, M.; Wikner, J. Impact of malpositioning on panoramic radiography in implant dentistry. Clin. Oral Investig. 2015, 19, 781–790. [Google Scholar] [CrossRef]
- Subbulakshmi, A.C.; Mohan, N.; Thiruneervannan, R.; Naveen, S.; Gokulraj, S. Positioning errors in digital panoramic radiographs: A study. J. Orofac. Sci. 2016, 8, 22–26. [Google Scholar] [CrossRef]
- Asha, V.; Kavya Shankar, M.; Shalma, H.; Sushmini, H. Positioning errors in digital panoramic radiographs-A retrospective analysis. Int. J. Adv. Res. Ideas Innov. Technol. 2018, 4, 517–521. [Google Scholar]
- Numata, H. Consideration of the parabolic radiography of the dental arch. J. Shimazu Stud. 1933, 10, 13. [Google Scholar]
- Paatero, Y.V. A new tomographical method for radiographing curved outer surfaces. Acta Radiol. 1949, 32, 177–184. [Google Scholar] [CrossRef] [Green Version]
- Paatero, Y.V. Pantomography in theory and use. Acta Radiol. 1954, 4, 321–335. [Google Scholar]
- Boeddinghaus, R.; Whyte, A. Dental panoramic tomography: An approach for the general radiologist. Australas. Radiol. 2006, 50, 526–533. [Google Scholar] [CrossRef] [PubMed]
- White, S.C.; Pharoah, M.J. Oral Radiology: Principles and Interpretation; Mosby: St. Louis, MO, USA, 2014. [Google Scholar]
- Rozylo-Kalinowska, I. Technical Errors and Artefacts in Dental Radiography. In Imaging Techniques in Dental Radiology; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Wong, N.S.M. Reject Rates of Radiographic Images in Dentomaxillofacial Radiology: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 8076. [Google Scholar] [CrossRef] [PubMed]
- Loughlin, A.; Drage, N.; Greenall, C.; Farnell, D.J.J. An investigation in to the impact of acquisition location on error type and rate when undertaking panoramic radiography. Radiography 2017, 23, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, A.; Matzen, L.H.; Spin-Neto, R.; Schropp, L. Effect of computer-assisted-learning and simulation clinics on dental students’ cognitive and performance skills: Panoramic image errors related to patient’s head position. Dentomaxillofacial Radiol. 2020, 49, 20200154. [Google Scholar] [CrossRef]
- Rushton, V.E.; Horner, K.; Worthington, H.V. The quality of panoramic radiographs in a sample of general dental practices. Br. Dent. J. 1999, 186, 630–633. [Google Scholar] [CrossRef] [PubMed]
- Nardi, C.; Molteni, R.; Lorini, C.; Taliani, G.G.; Matteuzzi, B.; Mazzoni, E.; Colagrande, S. Motion artefacts in cone beam CT: An in vitro study about the effects on the images. Br. J. Radiol. 2016, 89, 20150687. [Google Scholar] [CrossRef] [Green Version]
- Farman, A.G. Panoramic Radiology: Seminars on Maxillofacial Imaging and Interpretation; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Goren, A.D.; Lundeen, R.C.; Deahl, S.T., 2nd; Hashimoto, K.; Kapa, S.F.; Katz, J.O.; Ludlow, J.B.; Platin, E.; Van Der Stelt, P.F.; Wolfgang, L.; et al. Updated quality assurance self-assessment exercise in intraoral and panoramic radiography. American Academy of Oral and Maxillofacial Radiology, Radiology Practice Committee. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 89, 369–374. [Google Scholar] [CrossRef]
- Abdul-Wahab, H.; Ferguson, D.J.; Abou-Kheir, N. Assessment of panoral radiograph quality in a dental treatment center. APOS Trends Orthod. 2016, 6, 85–94. [Google Scholar] [CrossRef]
- Gavala, S.; Donta, C.; Tsiklakis, K.; Boziari, A.; Kamenopoulou, V.; Stamatakis, H.C. Radiation dose reduction in direct digital panoramic radiography. Eur. J. Radiol. 2009, 71, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Kühnisch, J.; Anttonen, V.; Duggal, M.S.; Spyridonos, M.L.; Rajasekharan, S.; Sobczak, M.; Stratigaki, E.; Van Acker, J.; Aps, J.K.M.; Horner, K.; et al. Best clinical practice guidance for prescribing dental radiographs in children and adolescents: An EAPD policy document. Eur. Arch. Paediatr. Dent. 2020, 21, 375–386. [Google Scholar] [CrossRef] [PubMed]





| Digital Panoramic Radiography | |
|---|---|
| Advantages | Disadvantages |
| Ease of execution | One-time high cost of implementation of the digital system |
| Significant reduction in time between exposure and ready radiograph | Need for knowledge of computing technology by operators |
| Image post-processing options | Lack of control over radiographs with too many retaking examinations |
| Long-lasting archive of images with the easy retrieval of multiple copies | Need to protect sensitive patient data |
| Teleradiology. Image transfer and reporting via internet | Possibility of tampering with images |
| Wide dynamic range of X-ray exposures | |
| Automatic modulation of X-ray beam energy | |
| Decrease in radiation dose | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Izzetti, R.; Nisi, M.; Aringhieri, G.; Crocetti, L.; Graziani, F.; Nardi, C. Basic Knowledge and New Advances in Panoramic Radiography Imaging Techniques: A Narrative Review on What Dentists and Radiologists Should Know. Appl. Sci. 2021, 11, 7858. https://doi.org/10.3390/app11177858
Izzetti R, Nisi M, Aringhieri G, Crocetti L, Graziani F, Nardi C. Basic Knowledge and New Advances in Panoramic Radiography Imaging Techniques: A Narrative Review on What Dentists and Radiologists Should Know. Applied Sciences. 2021; 11(17):7858. https://doi.org/10.3390/app11177858
Chicago/Turabian StyleIzzetti, Rossana, Marco Nisi, Giacomo Aringhieri, Laura Crocetti, Filippo Graziani, and Cosimo Nardi. 2021. "Basic Knowledge and New Advances in Panoramic Radiography Imaging Techniques: A Narrative Review on What Dentists and Radiologists Should Know" Applied Sciences 11, no. 17: 7858. https://doi.org/10.3390/app11177858
APA StyleIzzetti, R., Nisi, M., Aringhieri, G., Crocetti, L., Graziani, F., & Nardi, C. (2021). Basic Knowledge and New Advances in Panoramic Radiography Imaging Techniques: A Narrative Review on What Dentists and Radiologists Should Know. Applied Sciences, 11(17), 7858. https://doi.org/10.3390/app11177858







