Support Group as a Management Modality for Burning Mouth Syndrome: A Randomized Prospective Study
Abstract
:1. Introduction
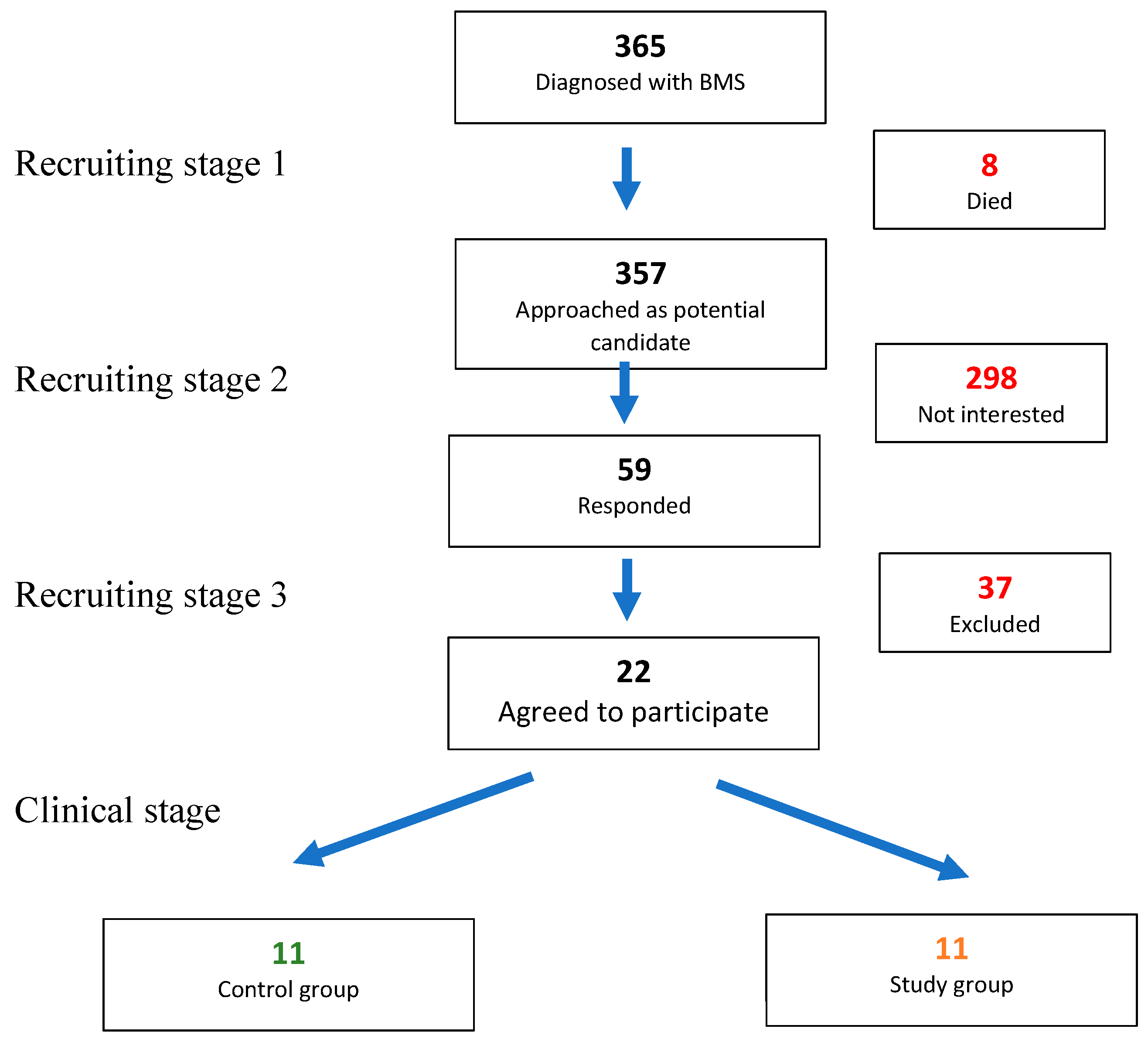
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Life-Quality Questionnaire
References
- Suarez, P.; Clark, G.T. Burning mouth syndrome: An update on diagnosis and treatment methods. J. Calif. Dent. Assoc. 2006, 34, 611–622. [Google Scholar]
- Kim, Y.; Yoo, T.; Han, P.; Liu, Y.; Inman, J.C. A pragmatic evidence-based clinical management algorithm for burning mouth syndrome. J. Clin. Exp. Dent. 2018, 10, e321–e326. [Google Scholar] [CrossRef] [Green Version]
- Scala, A.; Checchi, L.; Montevecchi, M.; Marini, I.; Giamberardino, M. Update on Burning Mouth Syndrome: Overview and Patient Management. Crit. Rev. Oral Biol. Med. 2003, 14, 275–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patton, L.L.; Siegel, M.A.; Benoliel, R.; De Laat, A. Management of burning mouth syndrome: Systematic review and management recommendations. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 103, S39.e1–S39.e13. [Google Scholar] [CrossRef] [PubMed]
- Barry, A.; O’Halloran, K.; McKenna, J.P.; McCreary, C.; Downer, E.J. Plasma IL-8 signature correlates with pain and depressive symptomatology in patients with burning mouth syndrome: Results from a pilot study. J. Oral Pathol. Med. 2017, 47, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Bergdahl, M.; Bergdahl, J. Burning mouth syndrome: Prevalence and associated factors. J. Oral Pathol. Med. 2007, 28, 350–354. [Google Scholar] [CrossRef]
- Iv, L.C.; Charleston, L. Burning Mouth Syndrome: A Review of Recent Literature. Curr. Pain Headache Rep. 2013, 17, 1–9. [Google Scholar] [CrossRef]
- Gorsky, M.; Silverman, S.; Chinn, H. Clinical characteristics and management outcome in the burning mouth syndrome. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 192–195. [Google Scholar] [CrossRef]
- Maltsman-Tseikhin, A.; Moricca, P.; Niv, D. Burning Mouth Syndrome: Will Better Understanding Yield Better Management? Pain Pract. 2007, 7, 151–162. [Google Scholar] [CrossRef]
- Schiavone, V.; Adamo, D.; Ventrella, G.; Morlino, M.; De Notaris, E.B.; Ravel, M.G.; Kusmann, F.; Piantadosi, M.; Pollio, A.; Fortuna, G.; et al. Anxiety, Depression, and Pain in Burning Mouth Syndrome: First Chicken or Egg? Headache J. Head Face Pain 2012, 52, 1019–1025. [Google Scholar] [CrossRef]
- Marino, R.; Capaccio, P.; Pignataro, L.; Spadari, F. Burning mouth syndrome: The role of contact hypersensitivity. Oral Dis. 2009, 15, 255–258. [Google Scholar] [CrossRef]
- Hagelberg, N.; Forssell, H.; Aalto, S.; Rinne, J.O.; Scheinin, H.; Taiminen, T.; Någren, K.; Eskola, O.; Jääskeläinen, S.K. Altered dopamine D2 receptor binding in atypical facial pain. Pain 2003, 106, 43–48. [Google Scholar] [CrossRef]
- Grémeau-Richard, C.; DuBray, C.; Aublet-Cuvelier, B.; Ughetto, S.; Woda, A. Effect of lingual nerve block on burning mouth syndrome (stomatodynia): A randomized crossover trial. Pain 2010, 149, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Pezelj-Ribarić, S.; Kqiku, L.; Brumini, G.; Urek, M.M.; Antonić, R.; Kuiš, D.; Glažar, I.; Städtler, P. Proinflammatory cytokine levels in saliva in patients with burning mouth syndrome before and after treatment with low-level laser therapy. Lasers Med. Sci. 2012, 28, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Simcic, D.; Pezelj-Ribaric, S.; Gržic, R.; Horvat, J.; Brumini, G.; Urek, M.M. Detection of Salivary Interleukin 2 and Interleukin 6 in Patients With Burning Mouth Syndrome. Mediat. Inflamm. 2006, 2006, 1–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guimarães, A.L.; de Sá, A.R.; Victoria, J.M.; de Fátima Correia-Silva, J.; Gomez, M.V.; Gomez, R.S. Interleukin-1beta and serotonin transporter gene polymorphisms in burning mouth syndrome patients. J. Pain 2006, 7, 654–658. [Google Scholar] [CrossRef]
- Carlson, C.R.; Miller, C.S.; Reid, K.I. Psychosocial profiles of patients with burning mouth syndrome. J. Orofac. Pain 2000, 14, 59–64. [Google Scholar]
- Kenchadze, R.; Iverieli, M.; Okribelashvili, N.; Geladze, N.; Khachapuridze, N. The psychological aspects of burning mouth syndrome. Georgian Med. News 2011, 194, 24–28. [Google Scholar]
- Nicholson, M.; Wilkinson, G.; Field, E.; Longman, L.; Fitzgerald, B. A pilot study: Stability of psychiatric diagnoses over 6 months in burning mouth syndrome. J. Psychosom. Res. 2000, 49, 1–2. [Google Scholar] [CrossRef]
- Miziara, I.D.; Filho, B.C.A.; Oliveira, R.; dos Santos, R.M.R. Group psychotherapy: An additional approach to burning mouth syndrome. J. Psychosom. Res. 2009, 67, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Bergdahl, J.; Anneroth, G.; Perris, H.; Ferris, H. Cognitive therapy in the treatment of patients with resistant burning mouth syndrome: A controlled study. J. Oral Pathol. Med. 1995, 24, 213–215. [Google Scholar] [CrossRef]
- Bergdahl, J.; Anneroth, G.; Perris, H. Personality characteristics of patients with resistant burning mouth syndrome. Acta Odontol. Scand. 1995, 53, 7–11. [Google Scholar] [CrossRef]
- Bergdahl, J. Psychologic aspects of patients with symptoms presumed to be caused by electricity or visual display units. Acta Odontol. Scand. 1995, 53, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-J.; Kho, H.-S. Understanding of Burning Mouth Syndrome Based on Psychological Aspects. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. (CSA) 2018, 21, 9–19. [Google Scholar]
- Komiyama, O.; Nishimura, H.; Makiyama, Y.; Iida, T.; Obara, R.; Shinoda, M.; Kobayashi, M.; Noma, N.; Abe, O.; De Laat, A.; et al. Group cognitive-behavioral intervention for patients with burning mouth syndrome. J. Oral Sci. 2013, 55, 17–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMillan, R.; Forssell, H.; Buchanan, J.A.; Glenny, A.-M.; Weldon, J.C.; Zakrzewska, J. Interventions for treating burning mouth syndrome. Cochrane Database Syst. Rev. 2016, 11, CD002779. [Google Scholar] [CrossRef] [Green Version]
- Chaushu, G.; Becker, A.; Zeltser, R.; Vasker, N.; Branski, S.; Chaushu, S. Patients’ perceptions of recovery after routine extraction of healthy premolars. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 170–175. [Google Scholar] [CrossRef]
- Marsland, A.L.; Walsh, C.; Lockwood, K.; John-Henderson, N.A. The effects of acute psychological stress on circulating and stimulated inflammatory markers: A systematic review and meta-analysis. Brain Behav. Immun. 2017, 64, 208–219. [Google Scholar] [CrossRef]
- Reinecke, A.; Thilo, K.V.; Croft, A.; Harmer, C.J. Early effects of exposure-based cognitive behaviour therapy on the neural correlates of anxiety. Transl. Psychiatry 2018, 8, 225. [Google Scholar] [CrossRef]
- Goossens, L.; Sunaert, S.; Peeters, R.; Griez, E.J.; Schruers, K.R. Amygdala Hyperfunction in Phobic Fear Normalizes After Exposure. Biol. Psychiatry 2007, 62, 1119–1125. [Google Scholar] [CrossRef]
- Morgiève, M.; N’Diaye, K.; Haynes, W.; Granger, B.; Clair, A.-H.; Pelissolo, A.; Mallet, L. Dynamics of psychotherapy-related cerebral haemodynamic changes in obsessive compulsive disorder using a personalized exposure task in functional magnetic resonance imaging. Psychol. Med. 2013, 44, 1461–1473. [Google Scholar] [CrossRef] [Green Version]
- Paquette, V.; Lévesque, J.; Mensour, B.; Leroux, J.-M.; Beaudoin, G.; Bourgouin, P.; Beauregard, M. “Change the mind and you change the brain”: Effects of cognitive-behavioral therapy on the neural correlates of spider phobia. NeuroImage 2003, 18, 401–409. [Google Scholar] [CrossRef]
- Candela, C.-F.; Pia, L.-J.; Pons-Fuster, E.; Tvarijonaviciute, A. Impact of the COVID-19 pandemic upon patients with burning mouth syndrome. J. Stomatol. Oral Maxillofac. Surg. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Dale, R.; Stacey, B. Multimodal Treatment of Chronic Pain. Med. Clin. N. Am. 2016, 100, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Graper, M.L.; Schilsky, M.L. Patient support groups in the management of Wilson disease. Hum. Hypothal. Middle Posterior Reg. 2017, 142, 231–240. [Google Scholar] [CrossRef]
- Zabetian, S.; Jacobson, G.; Lim, H.W.; Eide, M.J.; Huggins, R.H. Quality of Life in a Vitiligo Support Group. J. Drugs Dermatol. 2017, 16, 344–350. [Google Scholar]
- Strøm, J.; Høybye, M.T.; Laursen, M.; Jørgensen, L.B.; Nielsen, C.V.; Amann, J.; Bossen, D.; Nicholls, J.; Coulson, N. Lumbar Spine Fusion Patients’ Use of an Internet Support Group: Mixed Methods Study. J. Med. Internet Res. 2019, 21, e9805. [Google Scholar] [CrossRef]
- Haack, M.; Kofahl, C.; Kramer, S.; Seidel, G.; Knesebeck, O.V.D.; Dierks, M.-L. Participation in a prostate cancer support group and health literacy. Psychooncology 2018, 27, 2473–2481. [Google Scholar] [CrossRef]
- McCaughan, E.; Parahoo, K.; Hueter, I.; Northouse, L.; Bradbury, I. Online support groups for women with breast cancer. Cochrane Database Syst. Rev. 2015, 3, 011652. [Google Scholar] [CrossRef]
- Zeigler, L.; Smith, P.A.; Fawcett, J.; Common Journey Breast Cancer Support Group. Breast cancer: Evaluation of the Common Journey Breast Cancer Support Group. J. Clin. Nurs. 2004, 13, 467–478. [Google Scholar] [CrossRef]
- Stevinson, C.; Lydon, A.; Amir, Z. Cancer support group participation in the United Kingdom: A national survey. Support. Care Cancer 2010, 19, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Henien, M.; Sproat, C. Interactive group therapy for the management of myofascial temporomandibular pain. Br. Dent. J. 2017, 223, 90–95. [Google Scholar] [CrossRef]
- Bogetto, F.; Maina, G.; Ferro, G.; Carbone, M.; Gandolfo, S. Psychiatric Comorbidity in Patients With Burning Mouth Syndrome. Psychosom. Med. 1998, 60, 378–385. [Google Scholar] [CrossRef]
- Buckelew, S.P.; Parker, J.; Keefe, F.J.; Deuser, W.E.; Crews, T.M.; Conway, R.; Kay, D.R.; Hewett, J.E. Self-efficacy and pain behavior among subjects with fibromyalgia. Pain 1994, 59, 377–384. [Google Scholar] [CrossRef]
- Vanhaudenhuyse, A.; Gillet, A.; Malaise, N.; Salamun, I.; Grosdent, S.; Maquet, D.; Nyssen, A.-S.; Faymonville, M.-E. Psychological interventions influence patients’ attitudes and beliefs about their chronic pain. J. Tradit. Complement. Med. 2018, 8, 296–302. [Google Scholar] [CrossRef] [PubMed]
| Study Parameter | Study Group | p Value * | Control Group | p Value * | ||
|---|---|---|---|---|---|---|
| Before Interv. | After Interv. | Before Interv. | After Interv. | |||
| Total pain score | 2.36 (1.027) | 2 (1) | 0.046 | 1.73 (1.009) | 1.6 (0.516) | 0.655 |
| Medication use | 2 (1.612) | 1.55 (0.688) | 0.276 | 1 (0) | 1.2 (0.632) | 0.317 |
| Swallowing problems | 1.64 (1.286) | 1.27 (0.647) | 0.194 | 1.55 (1.293) | 1.7 (1.160) | 0.180 |
| Avoidance of certain foods | 2.36 (1.690) | 1.64 (1.027) | 0.129 | 2.18 (1.601) | 2.5 (1.434) | 0.336 |
| Difficulty enjoying food | 2.55 (1.809) | 1.64 (0.924) | 0.026 | 2.45 (1.440) | 1.8 (0.789) | 0.131 |
| Difficulty talking | 1.64 (0.924) | 1.64 (0.924) | 0.063 | 1.64 (1.206) | 1.3 (0.949) | 0.317 |
| Sleep deprivation | 2.09 (1.700) | 1.09 (0.302) | 0.066 | 1.55 (1.036) | 1.4 (0.843) | 0.705 |
| Inability to work | 1.36 (1.206) | 1 (0) | 0.317 | 1 (0) | 1 (0) | 1.000 |
| Difficulty performing everyday activities | 1.18 (0.405) | 1.09 (0.302) | 0.317 | 1 (0) | 1 (0) | 1.000 |
| Change in taste or odor sensation | 2.55 (1.572) | 2.09 (1.514) | 0.461 | 2.55 (1.695) | 2.4 (0.966) | 0.864 |
| Malaise | 2.64 (1.502) | 1.82 (1.079) | 0.041 | 2.18 (1.537) | 2.1 (1.101) | 0.854 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becker, T.; Hamzani, Y.; Chaushu, G.; Perry, S.; Haj Yahya, B. Support Group as a Management Modality for Burning Mouth Syndrome: A Randomized Prospective Study. Appl. Sci. 2021, 11, 7207. https://doi.org/10.3390/app11167207
Becker T, Hamzani Y, Chaushu G, Perry S, Haj Yahya B. Support Group as a Management Modality for Burning Mouth Syndrome: A Randomized Prospective Study. Applied Sciences. 2021; 11(16):7207. https://doi.org/10.3390/app11167207
Chicago/Turabian StyleBecker, Talia, Yafit Hamzani, Gavriel Chaushu, Shlomit Perry, and Bahaa Haj Yahya. 2021. "Support Group as a Management Modality for Burning Mouth Syndrome: A Randomized Prospective Study" Applied Sciences 11, no. 16: 7207. https://doi.org/10.3390/app11167207
APA StyleBecker, T., Hamzani, Y., Chaushu, G., Perry, S., & Haj Yahya, B. (2021). Support Group as a Management Modality for Burning Mouth Syndrome: A Randomized Prospective Study. Applied Sciences, 11(16), 7207. https://doi.org/10.3390/app11167207








