Abstract
At present, complete dentures (CDs) remain the only treatment available for the majority of edentulous patients. CDs are primarily fabricated using a conventional method using polymethylmethacrylate (PMMA) resin. The steps involved in PMMA polymerisation directly affect the quality of the resin prosthetic base and any error reduces retention and occlusal accuracy of CDs. Furthermore, when using the conventional technique, the residual monomer alters the resin mechanical properties and may cause mucosal reactions. Recently, computer aided design and computer aided manufacture (CAD/CAM) techniques were increasingly used to fabricate CDs by machining resin discs that have been manufactured under high pressure and temperature. This systematic review compares CAD/CAM and conventional CDs according to their mechanical, physical and chemical characteristics, as well as the clinical impact of any differences between them. A review was conducted according to the preferred reporting items for systematic reviews and meta-analyses checklist on 392 publications from both PubMed and backward research. Fifteen studies have been included. Results showed that CAD/CAM resins had globally better physical and mechanical properties than conventional resins. The use of machined resin could improve the clinical performance, maintenance and longevity of CDs. Further studies in clinical use would be required to complement these results.
1. Introduction
Due to anatomical, physiological or financial restrictions, complete dentures (CDs) still represent the only treatment available for the majority of edentulous patients. Since the 1950s, complete dentures have been primarily designed and fabricated by hand, using conventional methods that follow well-defined clinical protocols and laboratory techniques. To produce a set of complete dentures, edentulous patients must have at least five clinical appointments with their dentist to (1) make preliminary and (2) final impressions to make a replica of the oral tissues (gypsum cast), (3) record the maxillomandibular relationship and select the appropriate denture teeth, (4) test the trial wax prostheses and (5) insert the complete prostheses. Once the trial wax dentures are deemed appropriate, the laboratory steps to make the final prostheses begin. The gypsum cast and the trial wax replica are flasked in more gypsum to produce the external surface form. Once all the gypsum is solidified, the trial wax is removed using hot water, producing a mold cavity. The resin to fabricate the final denture is then introduced into the mold cavity within the flask by either pressure or injection. Each technique has advantages and disadvantages. The quality of the prosthetic resin material obtained is strongly influenced by the steps involved in handling the resin.
To date, acrylic resin polymethylmethacrylate (PMMA) is the most popular denture base material [1]. PMMA resin best meets all the specifications for an ideal denture base material. Its advantages range from easy repair to good appearance and reasonable cost. It has simple handling characteristics and polymerization is initiated by mixing polymethyl methacrylate (polymer) and methyl methacrylate (monomer) [2]. The polymerization of this type of PMMA resin is completed by application of heat. When this resin is used for dental prostheses, it shows linear distortions by contraction with a theoretical shrinkage of 6%. When using the conventional technique, internal stresses are created during the final heat application during polymerization. These stresses are released when the prosthesis is removed from the gypsum mold and flask, resulting in twisting, bending and dimensional variations of the denture bases compared to the cast. Clinically, these deformations result in a loss of accuracy and retention of the complete dentures.
There is also a loss of precision in the occlusal relationship as compared to the wax trial prosthesis [3]. Furthermore, the chemical reaction between the monomer and the polymer is never complete. The residual monomer that remains after the polymerization process can alter the mechanical properties of the resin [4]. The released monomer is also suspected of being responsible for allergic or irritating chemical reactions such as burning sensations in the mouth, stomatitis, edema or ulceration of the oral mucosa [5].
With the development of digital technology, computer aided design and manufacture (CAD/CAM) techniques are increasingly popular in dentistry. Thirty years after the first articles on digital removable prostheses, many systems now exist to both reduce the number of patient appointments needed and the laboratory time needed for prothesis fabrication [6,7,8,9]. The process of manufacturing CDs with computer-assisted technology involves the acquisition of clinical information and the digital design of prostheses on computer software. CDs can be produced using an additive (3D printing) or subtractive (milling) process. The most commonly used method at present is the subtractive method [10,11,12,13]. In the subtractive method, the prostheses are milled from proprietary resin discs that are polymerized under high pressure and high temperature [14]. CAD/CAM techniques for denture fabrication have many clinical and laboratory advantages [15,16,17,18]. The computer-aided design and manufacture of complete prostheses simplifies the laboratory protocol, stores data and reduces the number of appointments required. A literature review by Wang et al. [19] studied the impact of this manufacturing process on the adaptation of CDs and occlusion. Their review showed that all prostheses tested had a clinically acceptable fit. The CAD/CAM CDs showed a similar adaptation to conventional prostheses, sometimes even better. Recently, Baba et al. [20] reviewed currently available techniques to manufacture CAD/CAM complete dentures and concluded that their physical properties were improved over those fabricated by conventional laboratory techniques. With these results in mind, the present literature review is aimed at expanding the evaluation of CAD/CAM dentures by comparing their mechanical, physical and chemical characteristics with those of conventional dentures. For the first time, the clinical repercussions of the CAD/CAM machining process were assessed and discussed.
2. Materials and Methods
A thorough search of the literature was conducted using the Medline database (via PubMed). A search strategy developed for Medline via PubMed was employed using the following keywords: (CAD/CAM complete denture base); (CAD/CAM complete denture) NOT (implant); (CAD/CAM complete denture base) AND (resin properties). A systematic review according to the PRISMA checklist was applied. A manual search of the included articles was also performed to identify further eligible studies not detected by keyword search and this strategy is outlined in Figure 1. In January 2021, 392 titles listed in PubMed were identified. After screening the initial articles and backward searching, some publications were excluded based on the following criteria: papers not written in English, animal and in vivo studies, case reports, systematic reviews and when only abstracts were available.
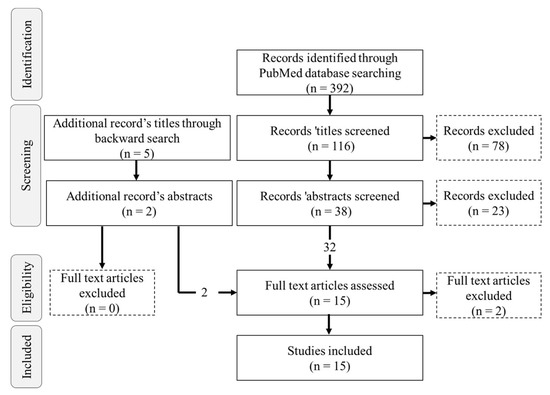
Figure 1.
PRISMA flow chart of records based on initial PubMed database searches and backward searching.
Studies comparing the properties of CD resins manufactured conventionally to those manufactured digitally by milling were targeted. Articles dealing with CDs digitally manufactured by 3D printing methods were excluded, leaving only the manufacturing process by machining for comparison to the conventional manufacturing method. Studies comparing the manufacturing techniques of complete removable prostheses based on criteria other than the properties of resins were also excluded, as well as studies on implant-supported prostheses, immediate dentures, or partial removable prostheses.
Full-text analysis was performed independently by two reviewers. Finally, fifteen articles were included.
3. Results
Three hundred and ninety-two titles were identified from the PubMed electronic search. The PRISMA selection methodology resulted in the inclusion of fifteen studies is summarized in Table 1.

Table 1.
Included articles (HP: Heat_polymerising; IM: Injected molding).
The objective of this literature review was to compare the characteristics of manufactured CAD/CAM PMMA resins with those of PMMA resins produced by conventional laboratory techniques. For this purpose, the results are presented according to the mechanical, physical and chemical properties of the resins. In all the studies, the conventional resins were produced using clamping pressure or injection techniques, followed by polymerization by heat using common dental laboratory techniques. The CAD/CAM resins were obtained from industrially manufactured resin discs that were polymerized under high pressure and high temperature.
3.1. Mechanical Properties
Seven articles have focused on the surface hardness of the PMMA resins. Hardness is a measure of the resistance of a material to plastic deformation, induced by either abrasion or mechanical indentation. The data are presented in Table 2. Two studies have shown that resins for CAD/CAM prostheses have a higher microhardness than conventional resins [21,22,23]. Others studies showed no significant difference in hardness between the two types of resins when tested for nano-hardness [24,25]. Recently, however, one study showed that the hardness of CAD/CAM resin was significantly lower than that of hot-pressed conventional resin [26]. Perea–Lowery [27] revealed differences in material-related hardness and microhardness between CAD/CAM and conventional resins

Table 2.
Hardness test results.
The resistance to deformation was studied by three-point bending tests in nine studies [21,23,24,26,27,29,31,33,34]. Results showed that CAD/CAM resins have superior mechanical properties; higher elastic moduli [21,24,26,29,33], flexural strength [23,24,26,31,33,34], impact strength [34] and yield strength [24,25] as compared to conventional resins. However, two studies [21,27] revealed that the mechanical properties of CAD/CAM resins were not always superior to that of conventional resins. Arslan et al. showed that the flexural strength of all the resins tested was significantly lower after thermocycling [31]. Most CAD/CAM resins have a higher toughness than conventional resins [24,29].
Only one study focused on the analysis of the load at fracture of resins using a 3-point bending test on rectangular resin samples (4 mm-thick). The maximum load at fracture of six CAD/CAM resins was then compared with that of conventional heat-cured and self-curing resins [29]. Table 3 shows the results of the fracture tests. The fracture resistance of CAD/CAM resins was not always superior to that of conventional heat-cured or self-curing resins. Indeed, fracture resistance is highly variable within CAD/CAM resins. The average breaking loads ranged from 40.27 N ± 3.40 to 82.49 N ± 7.47 for CAD/CAM resins. Of the six CAD/CAM resins tested, only the Wieland digital dentures (WWD) resin had significantly higher values than conventional resins. This study also showed that there was a positive correlation between fracture surface roughness and the maximum load at fracture of the resin. For example, the WDD CAD/CAM resin had the roughest fracture surface with the highest maximum breaking load.

Table 3.
Breaking load test results.
The study by Steinmassl et al. [29] highlighted the differences in mechanical properties between CAD/CAM resins.
3.2. Physical Properties
Seven studies compared the surface roughness of CAD/CAM and conventional resins [22,24,28,29,30,31,32]. Surface roughness was measured using laser or contact profilometers. Three of the seven studies showed that conventional resins had significantly higher surface roughness than CAD/CAM resins [22,28,32]. Another study also showed that conventional resins had a higher roughness, except for one brand of CAD/CAM resin that showed a slightly lower roughness that was not statistically significant [30]. The study by Steinmassl et al. showed that two of the five CAD/CAM resins tested had lower roughness than conventional resins [29]. One study showed that surface roughness was significantly higher for CAD/CAM resins [24]. The study by Arslan et al. showed that the resins did not exhibit different roughness values before and after thermal cycling [31]. The data are summarized in Table 4.

Table 4.
Surface roughness test results.
Four studies have focused on the hydrophobicity of resins using the sessile drop technique with calculation of the contact angle [22,30,31,32]. The results of the studies are presented in Table 5. Two studies showed that most CAD/CAM resins were more hydrophobic than conventional resins [22,31], while another study showed a higher hydrophobicity rate for conventional resins [30]. All the studies highlighted variations in hydrophobicity according to the CAD/CAM resin used [22,30,31,32].

Table 5.
Hydrophobicity test results.
One study used thermocycling to simulate the clinical aging process and found that conventional resins become more hydrophobic and CAD/CAM resins become more hydrophilic after aging [31].
3.3. Chemical Properties
Two studies have investigated the content of residual monomer in industrially polymerized CAD/CAM resins [14,21]. The results are presented in Table 6. Steinmassl et al. showed that CAD/CAM resins release very little free monomer after milling. However, their residual monomer content was not statistically lower than that of conventional laboratory-polymerized resins, regardless of the CAD/CAM process tested (BalticDenture, Whole You Nexteeth, Wieland Digital Dentures or Vita) for the manufacture of CDs. Another study showed lower free monomer content in industrially polymerized resin specimens, compared to conventionally polymerized resins [21].

Table 6.
Residual monomer content test results.
4. Discussion
The objective of this literature review was to compare the characteristics of CAD/CAM resins with those of conventional resins in order to assess the impact of CAD/CAM resins on the CDs’ clinical performance and durability. Results showed that switching to digital technology for the manufacturing process of resins led to different properties between conventional and CAD/CAM resins. Throughout this discussion, the effect of the physical property differences of these resins on the success of clinical denture treatment will be highlighted.
4.1. Retention of Denture Bases
The clinical performance of CDs is partly determined by their retention within the oral cavity. Lack of retention and instability are two of the main complaints from people wearing CDs. Retention refers to the amount of vertical force needed to resist the dislodgement of the prosthesis away from its supporting structures, similar to the force needed to remove a suction cup. As with a suction cup, wettability of the resins influences the prostheses’ retention to the supporting mucosa and has to be taken into account in the manufacturing process. Wettability indicates whether saliva is able to spread more or less easily on a surface and reflects whether fluids aid retention of the denture surface to oral mucosa, thus affecting retention. CDs with good wettability therefore optimize retention. The wettability of a material is defined by observing the angle of contact between the material and a drop of water: the greater the angle, the lower the wettability and therefore, the more hydrophobic the material will be. In the studies included in the review, hydrophobicity varied according to the type of resin used and could be explained by several hypotheses. Hydrophobicity could be correlated with the rate of monomer released by the resins during polymerization [31]. Another hypothesis could call into question the additives contained in the resins. Indeed, dentures are not made of pure PMMA. They contain numerous additives such as polymerization initiators, cross-linking agents, fillers and dyes, which can all influence the hydrophobicity of the resins [31]. The origin of these variations in hydrophobicity value in dental resins, as well as the effect of aging on resin hydrophobicity, should be investigated.
On the one hand, these results on hydrophobicity do not clearly explain why some studies show that digital CDs are more retentive than conventional CDs. On the other hand, one study has shown through adhesion tests that the retention of digital CDs is better [35]. If the resins’ physical properties do not play a major role in CAD/CAM denture retention, then the manufacturing process itself could favor the precision of adaptation and the adhesion of digital CDs. Still, the precision of the manufacturing process of these resins favors adaptation and the adhesion of digital CDs and has shown that the retention of digital CDs is better than that of conventional prostheses [35]. The review by Wang et al. [19] on the accuracy of digital full dentures showed that digital CDs have a similar or better fit than conventionally manufactured CDs. The manufacture of CDs using digital techniques helps to meet the three biomechanical requirements to ensure CD success; namely retention, stability and support (accuracy of fit to the oral tissues) as defined in Housset’s triad.
4.2. Resistance to Deformation and Breakage
When worn, complete dentures are subjected to high stresses during chewing. This creates cyclic deformation of the denture polymer, which in turn can lead to crack formation and possible fatigue fracture of the denture [36]. Therefore, good resistance of the resins to deformation is very important. The results of this literature review showed that CAD/CAM resins have superior mechanical properties to conventional resins.
First of all, conventional resins had a lower modulus of elasticity than CAD/CAM resins. The elastic modulus is an important property in characterizing the material’s rigidity. Resins with a higher modulus of elasticity will be more resistant to elastic deformation. A high elastic modulus may make it possible to fabricate prostheses with reduced thickness without compromising the mechanical properties, an important attribute for patient comfort and acceptance of the prosthesis. In addition, a deformation-resistant prosthesis will have a more stable occlusion. These differences in rigidity between CAD/CAM and conventional resins are probably due to the manufacturing process. The modulus of elasticity would be related to the residual monomer content. It has been shown that a high monomer content reduces the glass transition temperature, making the resin more flexible. The high-temperature, high-pressure polymerization of CAD/CAM resins leads to higher monomer conversion with lower residual monomer values, thus resulting in a more rigid resin. High-pressure and high-temperature polymerization also allows a different arrangement of the polymer chains. Previous studies had shown that the use of high pressure during polymerization increased crosslinks between polymer chains [15,37].
Secondly, fracture resistance characterizes the maximum stress a material can withstand before breaking. Results have shown that fracture resistance varied within CAD/CAM resins. For example, in the study by Steinmassl et al. [29], the Wieland digital denture (WDD) resin exhibited higher loads to fracture but had a lower elastic modulus than the others. Thus, it had lower rigidity and more susceptible to plastic deformation. It would therefore be preferable not to reduce the bases thickness too much to compensate for the risk of plastic deformation. Of the six CAD/CAM resins tested, only the WWD resin had significantly higher yield strength values compared to conventional resins. WDD also exhibited the roughest fracture surface. It was the only resin with fine grains on the fracture surface. This difference in resin surfaces is thought to be due to the geometry, size and distribution of the polymer powders used to make the resins. In the study by Steinmassl et al. [29] the measured maximum breaking loads were all greater than 40 N. However, the maximum bite force was reduced to 40 N in complete prosthesis wearers with high resorption of the mandibular alveolar bone [38]. Based on these results, some manufacturers encourage the fabrication of full dentures with reduced resin thickness. It is imperative to remain skeptical regarding this commercial argument, especially since in the study, the tests were performed on 4 mm thick resin samples, which is much thicker than a prosthetic base. Furthermore, CDs are subjected to much more complex stresses in the mouth, involving different types of forces in different directions (such as chewing). For a valid prediction of clinical fatigue resistance, further studies on cyclic loading behavior and fracture toughness are necessary.
The results highlighted differences in mechanical properties between CAD/CAM resins. More information on the composition and manufacturing processes of CAD/CAM resins would help to better understand some of the results.
4.3. Adhesion of Microorganisms
Preventing the adhesion of microorganisms to dentures helps preserve the health of tissues in the oral cavity. The prevalence of denture stomatitis among denture wearers has been shown average around 28% [39]. Microorganisms can cause pathology in the mucosa supporting the prosthesis, such as candidiasis (induced mainly by Candida albicans). Microorganisms accumulate more easily on prostheses than on natural tissue. The surfaces of removable maxillary prostheses are the main reservoir of Candida albicans [40,41]. The physical properties of the prosthetic resin influence this adhesion, including surface roughness and hardness. The results of this literature review showed that CAD/CAM machined resins had globally more advantageous physical properties than conventional resins.
Surface roughness is the most important factor for Candida albicans’ adhesion to the prosthesis surface. Optical and electron microscopy studies revealed that initial adhesion of microorganisms usually begins in the microscopic pits and cracks of rough surfaces. This surface roughness provides protection against removal (shear) forces and gives time for microbes to irreversibly adhere to the surface [42,43,44,45]. A smoother surface might reduce Candida albicans adhesion, which ultimately lowers the risk of prosthetic stomatitis. It has been demonstrated that CAD/CAM resins have significantly lower surface roughness than conventional resins [22,28,29,32]. The polishing technique and the operator’s ability to polish both affect the roughness of the resins’ cameo (external) surface [46]. However, the prosthetic intaglio (internal surface in contact with the supporting mucosa) is never polished, and only the polymerization of the resins would determine surface roughness. Therefore, irregularities in conventionally fabricated dentures would be due to the evaporation of monomers during polymerization. This can be avoided by applying high-pressure polymerization, as seen when utilizing proprietary CAD/CAM resins [32]. In case of conventional resin polymerization, the amount of pressure applied is limited to avoid fracturing the gypsum mold in which resins are polymerized. Conversely, machined resins for CAD/CAM prosthetics are made from resin discs that are polymerized at very high pressure, which could explain their lower roughness [30]. Furthermore, in order to avoid the accumulation and colonization of microorganisms on the prostheses’ surface, roughness of the resins should not exceed 0.2 μm [47]. In this review, most of the resins had roughness above 0.2 μm. This characteristic should be improved in the future, taking into consideration that the surface profile of the prosthetic intaglio surface always exhibits striations due to milling process used for CAD/CAM resins.
In addition to the biofilm adhesion onto the resins, surface roughness also tends to induce halitosis and mucosal inflammation [48], and reduces patient comfort. Thus, milling resins could reduce these nuisances and facilitate denture maintenance.
Hardness is another factor influencing bacterial adhesion to the prostheses over time. Surface hardness is defined as the ability of the material to resist penetration or permanent indentation related to the wear and scratches appearing as the dentures are worn and cleaned. A prosthesis should have a hard surface to reduce denture deterioration and therefore limit the adhesion of microorganisms [37,49]. Included studies focused on the microhardness as well as the nanohardness of resins. For the most part, surface micro-hardness was higher in CAD/CAM prosthetic resin blocks and no significant difference was found between nanohardness values. These results could be related to the polymerization process because the polymerization conditions of the CAD/CAM resin discs (high temperature and pressure) and the addition of inorganic substances promote the formation of longer polymer chains and limit the dimensional shrinkage of polymerization [50]. This high-temperature, high-pressure polymerization leads to higher monomer conversion, minimizing the plasticizing effect of the residual monomer [51,52]. Thus, CAD/CAM resins seem to be harder than conventional resins, which could help prevent bacterial adhesion and therefore increase the long-term comfort of the dentures.
4.4. Residual Monomer Content
The residual monomer alters the resins’ mechanical properties. It is also suspected of being responsible for allergic or irritating chemical reactions such as burning sensations in the mouth, stomatitis, edema or ulcerations of the oral mucosa. A certain amount of residual monomer is unavoidable due to the monomer-polymer balance required for the radical polymerization of resins [53]. Although the ISO 20795-1 norm (2013) allows a maximum residual monomer content of 2.2% by weight [54], the presence of residual monomer in the denture base resins should be reduced to a least amount possible.
In the study by Steinmassl et al. [14], the amount of residual monomer in industrially-polymerized and then machined CAD/CAM resins was not statistically different from that of conventional resins. Four CAD/CAM resins were tested (BalticDenture, Whole You Nexteeth, Wieland digital dentures and Vita). The BalticDenture process exhibited the least residual monomer of the resins tested. In the BalticDenture system, the prosthetic teeth are incorporated into the base during polymerization. In the other systems, the prosthetic teeth are bonded separately to the base after milling, using a PMMA bonding agent. These results suggest that the bonding agents used to attach the teeth to the milled resin base are a source of methacrylate monomer release. Thus, industrially polymerized resins would contain less residual monomer than laboratory-cured resins [21]. PMMA discs are polymerized industrially at high temperature and high pressure. This type of polymerization promotes the formation of longer polymer chains and would therefore lead to a higher level of monomer conversion with lower residual monomer values [37]. Assembling the prosthetic teeth to the machined bases during the CD manufacturing process would explain why the residual monomer content of some machined CDs is not that different from that of conventional CDs. Further studies need to be conducted to confirm this hypothesis, using, for example, Ivotion (Ivoclar’s newest monolithic CD material).
5. Conclusions
This review showed that CAD/CAM resins have similar or even superior characteristics to conventional resins, particularly in terms of mechanical properties. However, it should be noted that the variabilities of the characteristics are not only due to the manufacturing techniques but could also be due to the composition of resins. This entails that manufacturers should provide more complete information in terms of resin composition, and their manufacturing process, as it often remains confidential. CAD/CAM resins exhibit properties that can improve patient satisfaction and clinical success of CDs. The longevity of CDs should also be investigated in future studies in clinical use by investigating the resins’ aging process and fatigue resistance.
Using digital techniques to manufacture CDs would help meet the three biomechanical requirements to ensure CDs balance, namely retention, stability and support (Housset’s triad). Ultimately, this literature review is encouraging for more frequent utilization of CAD/CAM resins in the future, to become the new standard protocol.
Author Contributions
Conceptualization, C.B. and E.N.; methodology, C.B.; validation, C.B. and E.N.; formal analysis, C.B.; investigation, C.B.; original draft preparation, C.B.; writing—review and editing, C.B and E.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank Caroline Eschevins for her valuable technical support, Isabelle Denry and Julie A Holloway for their help in revising the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gharechahi, J.; Asadzadeh, N.; Shahabian, F.; Gharechahi, M. Dimensional Changes of Acrylic Resin Denture Bases: Conventional versus Injection-Molding Technique. J. Dent. Tehran Iran 2014, 11, 398–405. [Google Scholar]
- Takamata, T.; Setcos, J.C. Resin Denture Bases: Review of Accuracy and Methods of Polymerization. Int. J. Prosthodont. 1989, 2, 555–562. [Google Scholar]
- Keenan, P.L.J.; Radford, D.R.; Clark, R.K.F. Dimensional Change in Complete Dentures Fabricated by Injection Molding and Microwave Processing. J. Prosthet. Dent. 2003, 89, 37–44. [Google Scholar] [CrossRef]
- Kalipçilar, B.; Karaağaçlioğlu, L.; Hasanreisoğlu, U. Evaluation of the Level of Residual Monomer in Acrylic Denture Base Materials Having Different Polymerization Properties. J. Oral Rehabil. 1991, 18, 399–401. [Google Scholar] [CrossRef]
- Lee, H.-J.; Kim, C.-W.; Kim, Y.-S. The Level of Residual Monomer in Injection Molded Denture Base Materials. J. Korean Acad. Prosthodont. 2003, 41, 360–368. [Google Scholar]
- Kattadiyil, M.T.; AlHelal, A. An Update on Computer-Engineered Complete Dentures: A Systematic Review on Clinical Outcomes. J. Prosthet. Dent. 2017, 117, 478–485. [Google Scholar] [CrossRef]
- Steinmassl, P.-A.; Klaunzer, F.; Steinmassl, O.; Dumfahrt, H.; Grunert, I. Evaluation of Currently Available CAD/CAM Denture Systems. Int. J. Prosthodont. 2017, 30, 116–122. [Google Scholar] [CrossRef] [Green Version]
- Kattadiyil, M.T.; Goodacre, C.J.; Baba, N.Z. CAD/CAM Complete Dentures: A Review of Two Commercial Fabrication Systems. J. Calif. Dent. Assoc. 2013, 41, 407–416. [Google Scholar]
- Schwindling, F.S.; Stober, T. A Comparison of Two Digital Techniques for the Fabrication of Complete Removable Dental Prostheses: A Pilot Clinical Study. J. Prosthet. Dent. 2016, 116, 756–763. [Google Scholar] [CrossRef]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. CAD-CAM Milled versus Rapidly Prototyped (3D-Printed) Complete Dentures: An in Vitro Evaluation of Trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- Takeda, Y.; Lau, J.; Nouh, H.; Hirayama, H. A 3D Printing Replication Technique for Fabricating Digital Dentures. J. Prosthet. Dent. 2020, 124, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Bilgin, M.S.; Baytaroğlu, E.N.; Erdem, A.; Dilber, E. A Review of Computer-Aided Design/Computer-Aided Manufacture Techniques for Removable Denture Fabrication. Eur. J. Dent. 2016, 10, 286–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janeva, N.M.; Kovacevska, G.; Elencevski, S.; Panchevska, S.; Mijoska, A.; Lazarevska, B. Advantages of CAD/CAM versus Conventional Complete Dentures-A Review. Open Access Maced. J. Med. Sci. 2018, 6, 1498–1502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinmassl, P.-A.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do CAD/CAM Dentures Really Release Less Monomer than Conventional Dentures? Clin. Oral Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef] [Green Version]
- Bidra, A.S.; Taylor, T.D.; Agar, J.R. Computer-Aided Technology for Fabricating Complete Dentures: Systematic Review of Historical Background, Current Status, and Future Perspectives. J. Prosthet. Dent. 2013, 109, 361–366. [Google Scholar] [CrossRef]
- Infante, L.; Yilmaz, B.; McGlumphy, E.; Finger, I. Fabricating Complete Dentures with CAD/CAM Technology. J. Prosthet. Dent. 2014, 111, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Saponaro, P.C.; Yilmaz, B.; Heshmati, R.H.; McGlumphy, E.A. Clinical Performance of CAD-CAM-Fabricated Complete Dentures: A Cross-Sectional Study. J. Prosthet. Dent. 2016, 116, 431–435. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Garbacea, A.; Naylor, W.P.; Daher, T.; Marchack, C.B.; Lowry, J. CAD/CAM Fabricated Complete Dentures: Concepts and Clinical Methods of Obtaining Required Morphological Data. J. Prosthet. Dent. 2012, 107, 34–46. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.-F.; Xie, P.-J.; Wu, J.-H. Accuracy of Digital Complete Dentures: A Systematic Review of in Vitro Studies. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Baba, N.Z. CAD/CAM Complete Denture Systems and Physical Properties: A Review of the Literature. J. Prosthodont. 2021, 30, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Ayman, A.-D. The Residual Monomer Content and Mechanical Properties of CAD\CAM Resins Used in the Fabrication of Complete Dentures as Compared to Heat Cured Resins. Electron. Physician 2017, 9, 4766–4772. [Google Scholar] [CrossRef] [Green Version]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A Comparison of the Surface Properties of CAD/CAM and Conventional Polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef] [Green Version]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Gjengedal, H.; Cattani-Lorente, M.; Moussa, M.; Durual, S.; Schimmel, M.; Müller, F. CAD/CAM Milled Complete Removable Dental Prostheses: An in Vitro Evaluation of Biocompatibility, Mechanical Properties, and Surface Roughness. Dent. Mater. J. 2018, 37, 526–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pacquet, W.; Benoit, A.; Hatège-Kimana, C.; Wulfman, C. Mechanical Properties of CAD/CAM Denture Base Resins. Int. J. Prosthodont. 2019, 32, 104–106. [Google Scholar] [CrossRef]
- Becerra, J.; Mainjot, A.; Hüe, O.; Sadoun, M.; Nguyen, J.-F. Influence of High-Pressure Polymerization on Mechanical Properties of Denture Base Resins. J. Prosthodont. 2021, 30, 128–134. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Minja, I.K.; Lassila, L.; Ramakrishnaiah, R.; Vallittu, P.K. Assessment of CAD-CAM Polymers for Digitally Fabricated Complete Dentures. J. Prosthet. Dent. 2021, 125, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Al-Fouzan, A.F.; Al-mejrad, L.A.; Albarrag, A.M. Adherence of Candida to Complete Denture Surfaces in Vitro: A Comparison of Conventional and CAD/CAM Complete Dentures. J. Adv. Prosthodont. 2017, 9, 402–408. [Google Scholar] [CrossRef] [Green Version]
- Steinmassl, O.; Offermanns, V.; Stöckl, W.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.-A. In Vitro Analysis of the Fracture Resistance of CAD/CAM Denture Base Resins. Mater. Basel Switz. 2018, 11, 401. [Google Scholar] [CrossRef] [Green Version]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.-A. Influence of CAD/CAM Fabrication on Denture Surface Properties. J. Oral Rehabil. 2018, 45, 406–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arslan, M.; Murat, S.; Alp, G.; Zaimoglu, A. Evaluation of Flexural Strength and Surface Properties of Prepolymerized CAD/CAM PMMA-Based Polymers Used for Digital 3D Complete Dentures. Int. J. Comput. Dent. 2018, 21, 31–40. [Google Scholar]
- Murat, S.; Alp, G.; Alatalı, C.; Uzun, M. In Vitro Evaluation of Adhesion of Candida Albicans on CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, e873–e879. [Google Scholar] [CrossRef]
- Aguirre, B.C.; Chen, J.-H.; Kontogiorgos, E.D.; Murchison, D.F.; Nagy, W.W. Flexural Strength of Denture Base Acrylic Resins Processed by Conventional and CAD-CAM Methods. J. Prosthet. Dent. 2020, 123, 641–646. [Google Scholar] [CrossRef] [Green Version]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J. A Comparison of the Flexural and Impact Strengths and Flexural Modulus of CAD/CAM and Conventional Heat-Cured Polymethyl Methacrylate (PMMA). J. Prosthodont. 2020, 29, 341–349. [Google Scholar] [CrossRef] [PubMed]
- AlRumaih, H.S.; AlHelal, A.; Baba, N.Z.; Goodacre, C.J.; Al-Qahtani, A.; Kattadiyil, M.T. Effects of Denture Adhesive on the Retention of Milled and Heat-Activated Maxillary Denture Bases: A Clinical Study. J. Prosthet. Dent. 2018, 120, 361–366. [Google Scholar] [CrossRef]
- Takamiya, A.S.; Monteiro, D.R.; Marra, J.; Compagnoni, M.A.; Barbosa, D.B. Complete Denture Wearing and Fractures among Edentulous Patients Treated in University Clinics. Gerodontology 2012, 29, e728–e734. [Google Scholar] [CrossRef] [PubMed]
- Murakami, N.; Wakabayashi, N.; Matsushima, R.; Kishida, A.; Igarashi, Y. Effect of High-Pressure Polymerization on Mechanical Properties of PMMA Denture Base Resin. J. Mech. Behav. Biomed. Mater. 2013, 20, 98–104. [Google Scholar] [CrossRef]
- Fontijn-Tekamp, F.A.; Slagter, A.P.; Van Der Bilt, A.; Van ’T Hof, M.A.; Witter, D.J.; Kalk, W.; Jansen, J.A. Biting and Chewing in Overdentures, Full Dentures, and Natural Dentitions. J. Dent. Res. 2000, 79, 1519–1524. [Google Scholar] [CrossRef]
- Shulman, J.D.; Rivera-Hidalgo, F.; Beach, M.M. Risk Factors Associated with Denture Stomatitis in the United States. J. Oral Pathol. Med. 2005, 34, 340–346. [Google Scholar] [CrossRef]
- Coco, B.J.; Bagg, J.; Cross, L.J.; Jose, A.; Cross, J.; Ramage, G. Mixed Candida Albicans and Candida Glabrata Populations Associated with the Pathogenesis of Denture Stomatitis. Oral Microbiol. Immunol. 2008, 23, 377–383. [Google Scholar] [CrossRef]
- Gleiznys, A.; Zdanavičienė, E.; Žilinskas, J. Candida Albicans Importance to Denture Wearers. A Literature Review. Stomatologija 2015, 17, 54–66. [Google Scholar]
- Radford, D.R.; Sweet, S.P.; Challacombe, S.J.; Walter, J.D. Adherence of Candida Albicans to Denture-Base Materials with Different Surface Finishes. J. Dent. 1998, 26, 577–583. [Google Scholar] [CrossRef]
- da Silva, W.J.; Leal, C.M.B.; Viu, F.C.; Gonçalves, L.M.; Barbosa, C.M.R.; Del Bel Cury, A.A. Influence of Surface Free Energy of Denture Base and Liner Materials on Candida Albicans Biofilms. J. Investig. Clin. Dent. 2015, 6, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Satpathy, A.; Dhakshaini, M.R.; Gujjari, A.K. An Evaluation of the Adherence of Candida Albicans on the Surface of Heat Cure Denture Base Material Subjected to Different Stages of Polishing. J. Clin. Diagn. Res. JCDR 2013, 7, 2360–2363. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Cenci, T.; Pereira, T.; Cury, A.A.D.B.; Cenci, M.S.; Rodrigues-Garcia, R.C.M. In Vitro Candida Colonization on Acrylic Resins and Denture Liners: Influence of Surface Free Energy, Roughness, Saliva, and Adhering Bacteria. Int. J. Prosthodont. 2007, 20, 308–310. [Google Scholar]
- Kuhar, M.; Funduk, N. Effects of Polishing Techniques on the Surface Roughness of Acrylic Denture Base Resins. J. Prosthet. Dent. 2005, 93, 76–85. [Google Scholar] [CrossRef]
- Bollenl, C.M.L.; Lambrechts, P.; Quirynen, M. Comparison of Surface Roughness of Oral Hard Materials to the Threshold Surface Roughness for Bacterial Plaque Retention: A Review of the Literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef]
- Harrison, Z.; Johnson, A.; Douglas, C.W.I. An in Vitro Study into the Effect of a Limited Range of Denture Cleaners on Surface Roughness and Removal of Candida Albicans from Conventional Heat-Cured Acrylic Resin Denture Base Material. J. Oral Rehabil. 2004, 31, 460–467. [Google Scholar] [CrossRef]
- Susewind, S.; Lang, R.; Hahnel, S. Biofilm Formation and Candida Albicans Morphology on the Surface of Denture Base Materials. Mycoses 2015, 58, 719–727. [Google Scholar] [CrossRef] [Green Version]
- Consani, R.L.X.; Pucciarelli, M.G.R.; Mesquita, M.F.; Nogueira, M.C.F.; Barão, V.A.R. Polymerization Cycles on Hardness and Surface Gloss of Denture Bases. Int. J. Contemp. Dent. Med. Rev. 2014, 2014, ID041114. [Google Scholar]
- Farina, A.P.; Cecchin, D.; Soares, R.G.; Botelho, A.L.; Takahashi, J.M.F.K.; Mazzetto, M.O.; Mesquita, M.F. Evaluation of Vickers Hardness of Different Types of Acrylic Denture Base Resins with and without Glass Fibre Reinforcement. Gerodontology 2012, 29, e155–e160. [Google Scholar] [CrossRef]
- Azevedo, A.; Machado, A.L.; Vergani, C.E.; Giampaolo, E.T.; Pavarina, A.C. Hardness of Denture Base and Hard Chair-Side Reline Acrylic Resins. J. Appl. Oral Sci. 2005, 13, 291–295. [Google Scholar] [CrossRef] [Green Version]
- Lung, C.Y.K.; Darvell, B.W. Minimization of the Inevitable Residual Monomer in Denture Base Acrylic. Dent. Mater. 2005, 21, 1119–1128. [Google Scholar] [CrossRef]
- International Organization for Standardization. Dentistry-Base Polymers Part I: Denture Base Polymers; ISO 20795-1; ISO: Geneva, Switzerland, 2013; p. 35. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).