Mechanical Properties and Corrosion Resistance of TiAl6V4 Alloy Produced with SLM Technique and Used for Customized Mesh in Bone Augmentations
Abstract
1. Introduction
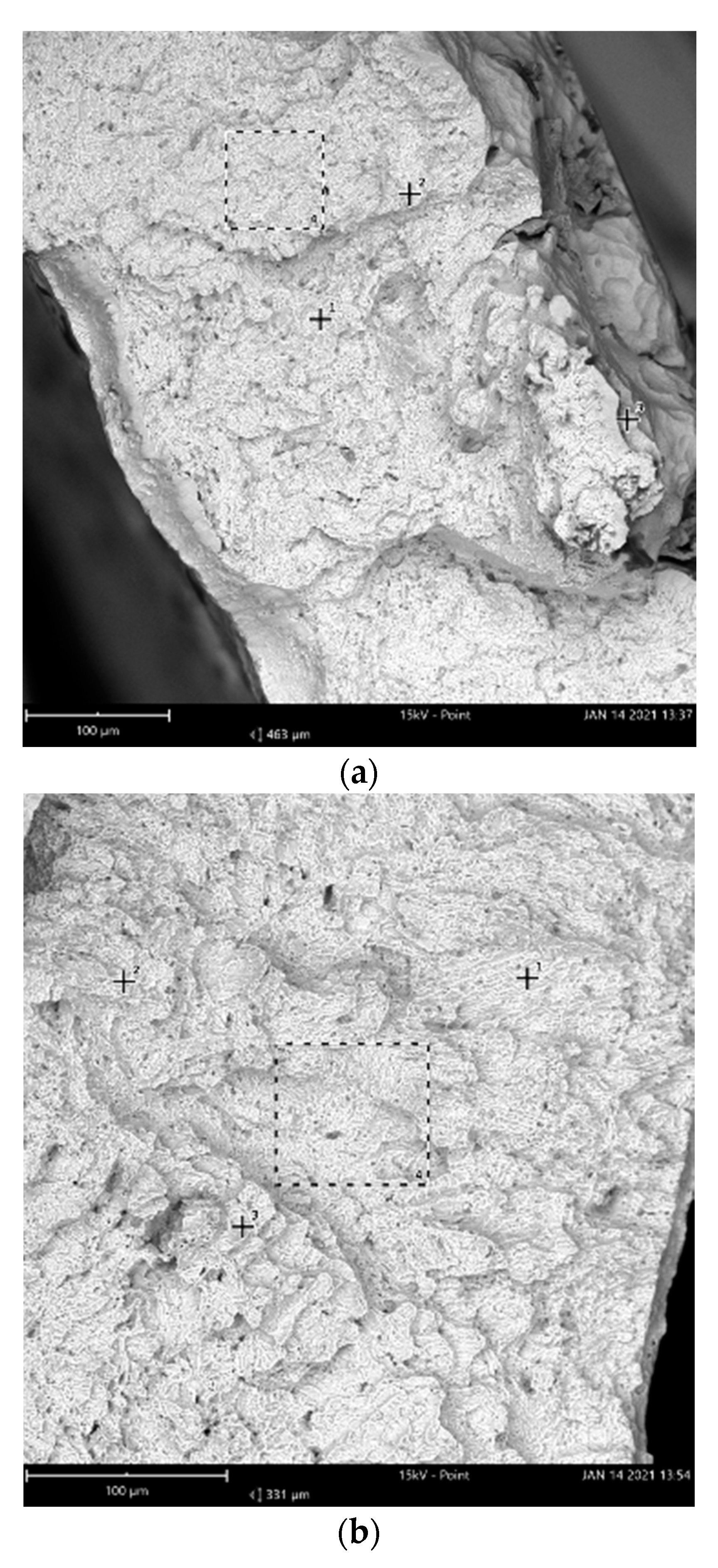
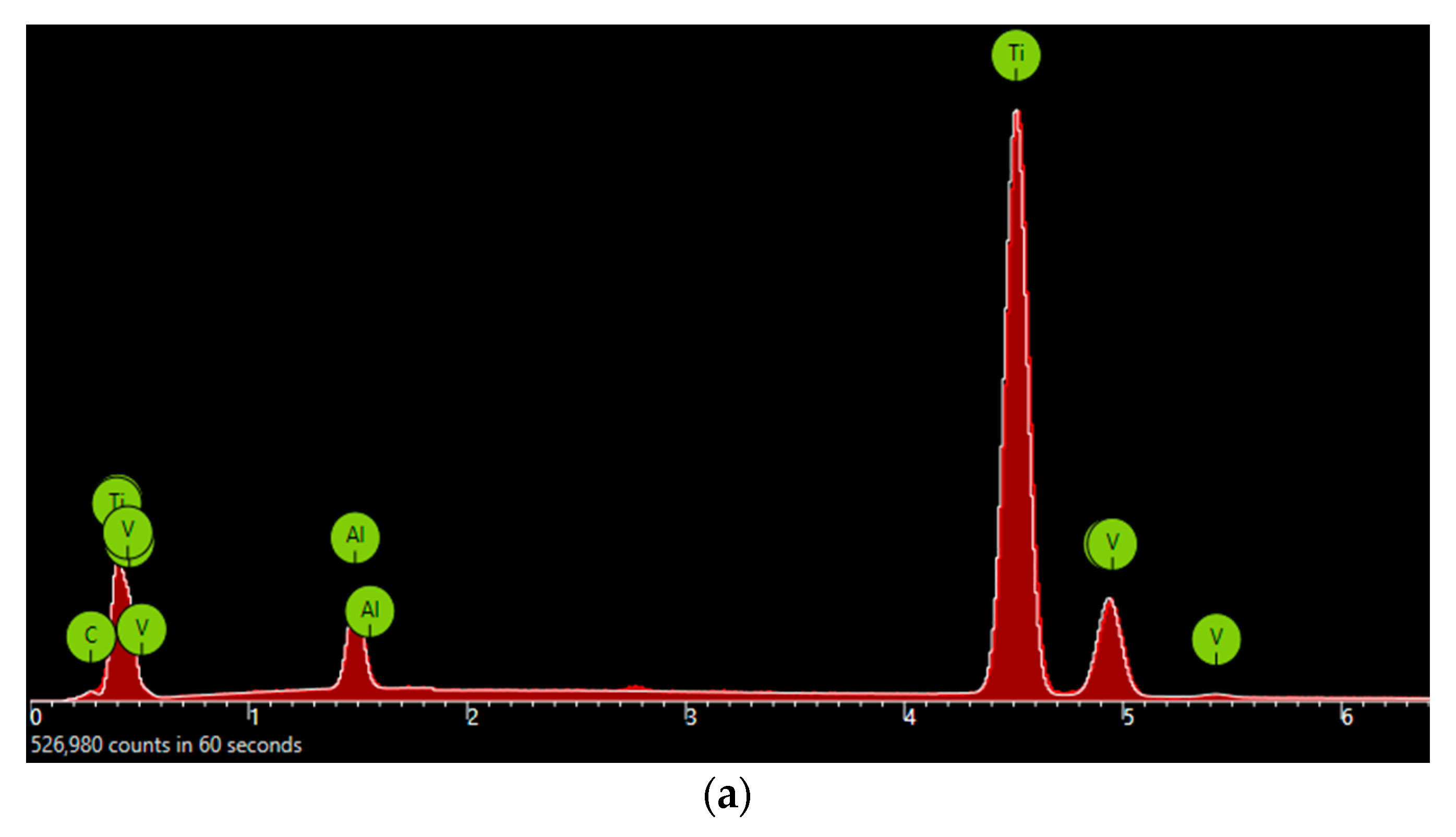
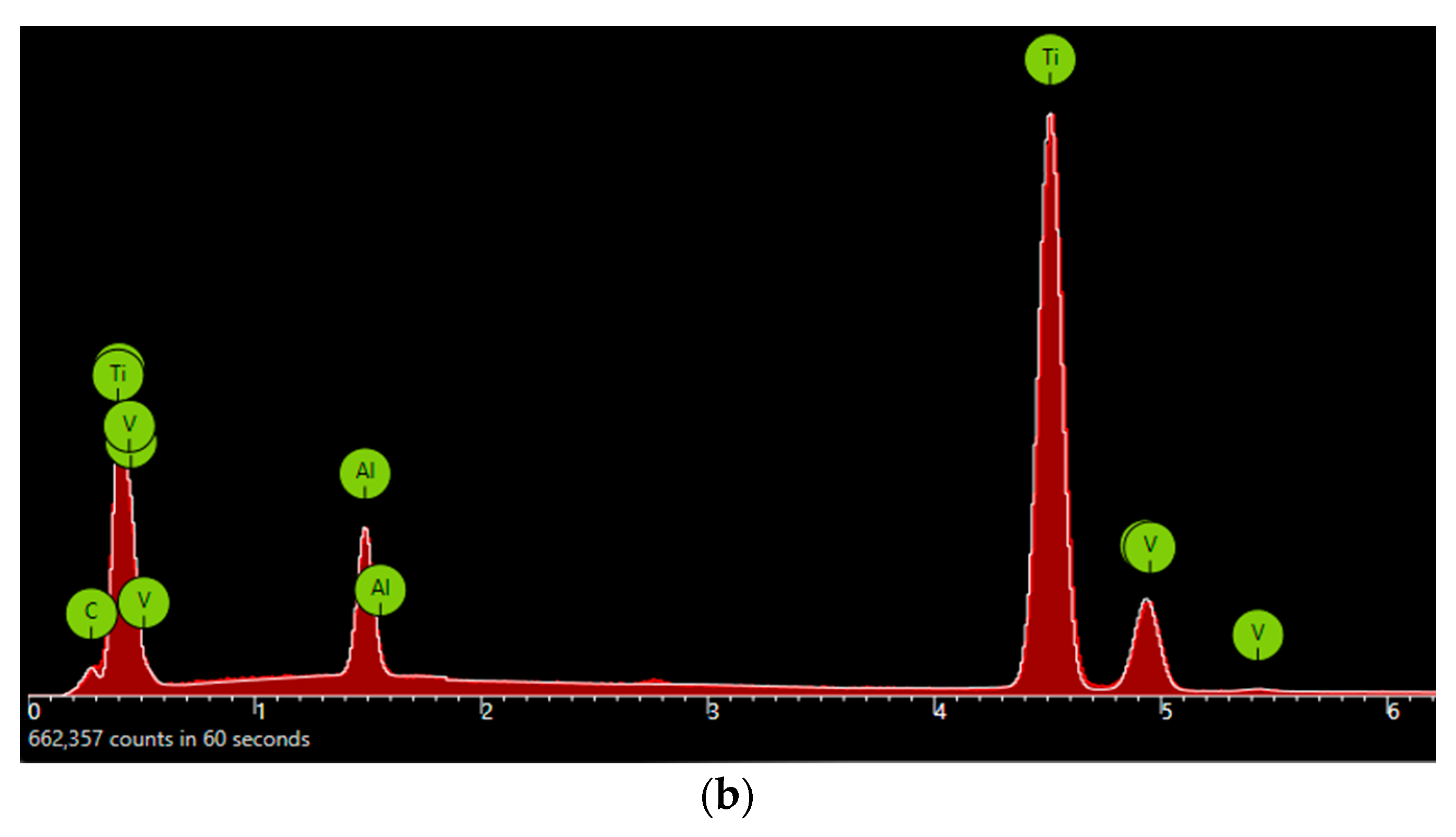
2. Materials and Methods
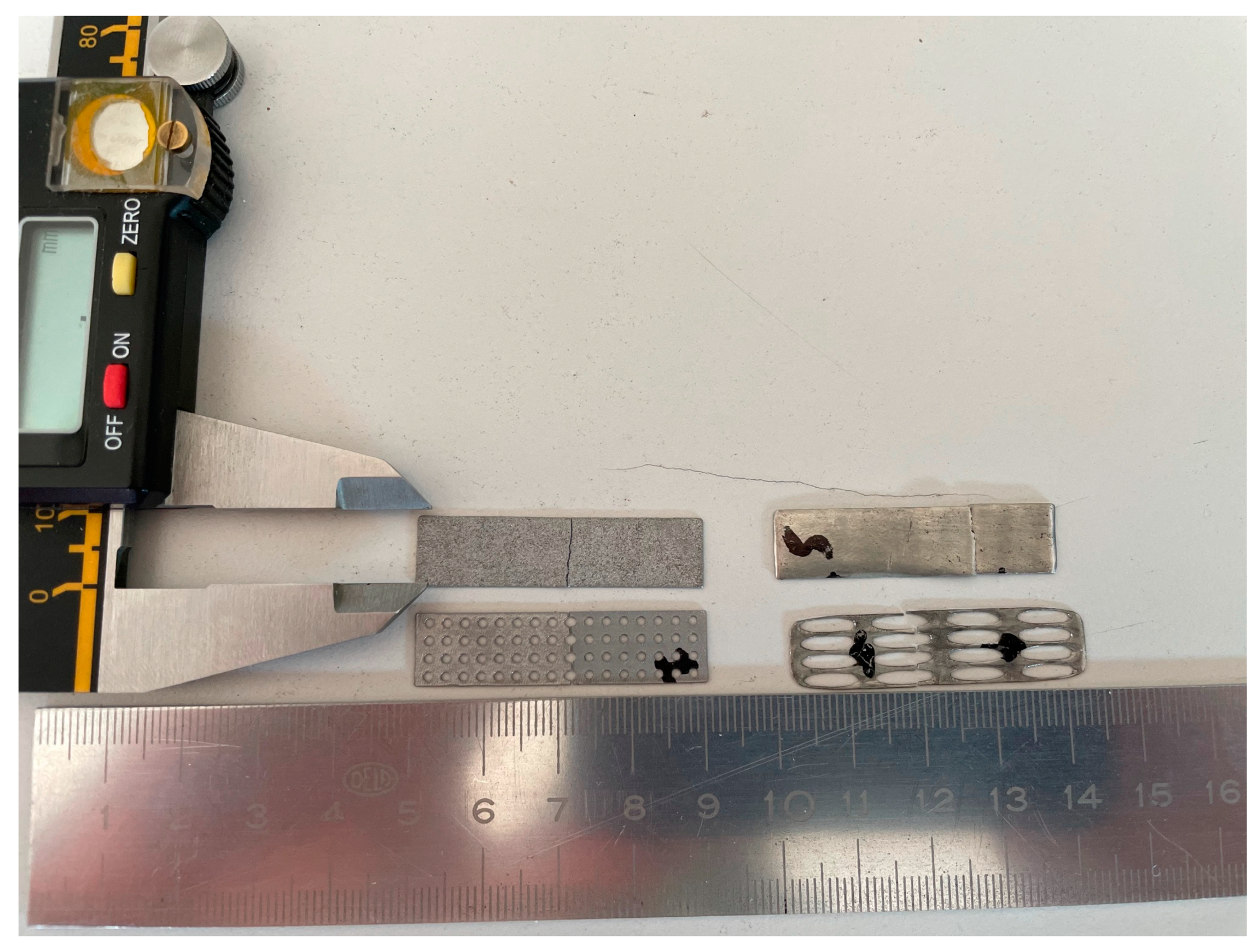
2.1. Samples’ Preparation
- Three BoneEasy specimens (BE) without perforations,
- Three Biotek specimens (BTK) without perforations,
- Three BoneEasy specimens (BE) with perforations, and
- Three Biotek specimens (BTK) with perforations.
2.2. Experiments
2.3. Analysis
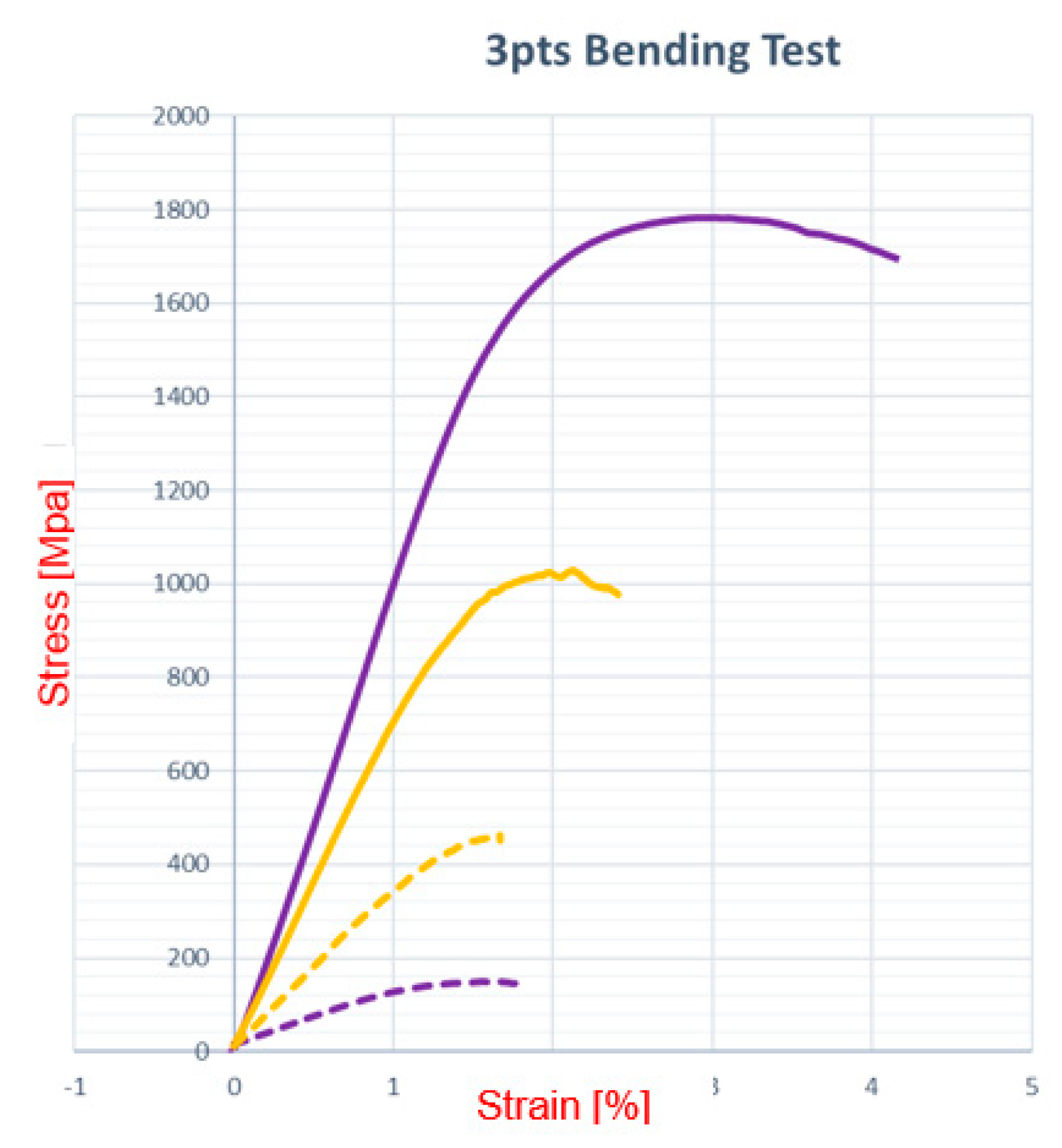
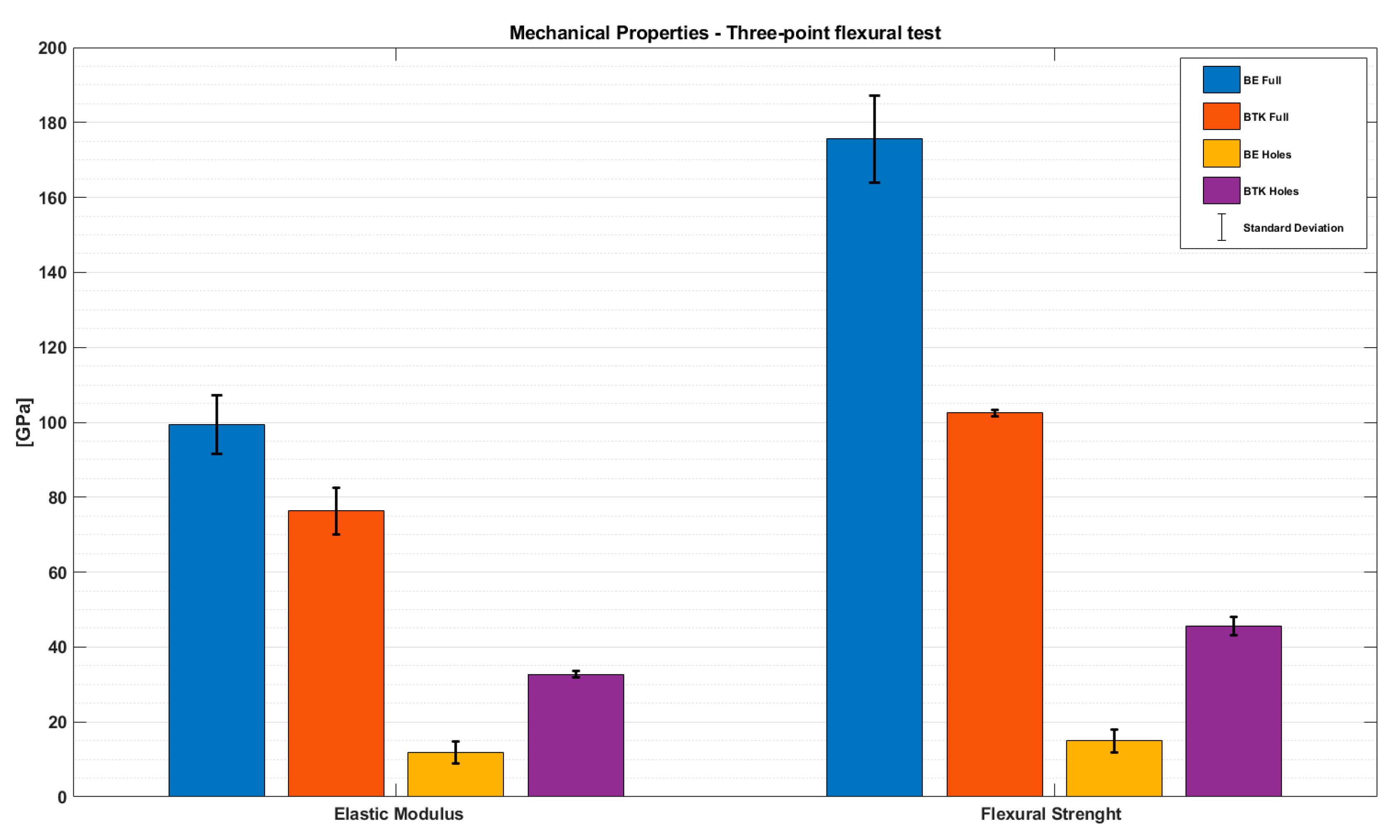
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smeet, R.; Stadlinger, B.; Frank, S. Impact of dental implant surface modifications on osseointegration. Biomed. Res. Int. 2016, 2, 1–16. [Google Scholar] [CrossRef]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Jegham, H.; Masmoudi, R.; Ouertani, H.; Blouza, I.; Turki, S.; Khattech, M. Ridge augmentation with titanium mesh: A case report. J. Stomatol. Oral Maxillofac. Surg. 2017, 118, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Rocchietta, I.; Fontana, F.; Simion, M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: A systematic review. J. Clin. Periodontol. 2008, 35, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Rakhmatia, Y.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Current barrier membranes: Titanium mesh and other membranes for guided bone regeneration in dental applications. J. Prosthodont. Res. 2013, 57, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zheng, J.; Zhang, S.; Yang, C.; Kwon, Y.-D.; Kim, Y.-J. Experiment of GBR for repair of peri-implant alveolar defects in beagle dogs. Sci. Rep. 2018, 8, 16532. [Google Scholar] [CrossRef]
- Donos, N.; Kostopoulos, L.; Tonetti, M.; Karring, T. Long-term stability of autogenous bone grafts following combined appli-cation with guided bone regeneration. Clin. Oral Implants Res. 2005, 16, 133–139. [Google Scholar] [CrossRef]
- Rakhmatia, Y.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Fibroblast attachment onto novel titanium mesh membranes for guided bone regeneration. Odontology 2015, 103, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, D.A.; Greco, G.B.; Cinci, L.; Pieri, L. Horizontal-guided Bone Regeneration using a Titanium Mesh and an Equine Bone Graft. J. Contemp. Dent. Pract. 2015, 16, 154–162. [Google Scholar] [CrossRef] [PubMed]
- De Moraes, P.H.; Olate, S.; De Albergaria-Barbosa, J.R. Maxillary Reconstruction Using rhBMP-2 and Titanium Mesh: Technical Note About the Use of Stereolithographic Model. Int. J. Odontostomatol. 2015, 9, 149–152. [Google Scholar] [CrossRef]
- Sumida, T.; Otawa, N.; Kamata, Y.; Kamakura, S.; Mtsushita, T.; Kitagaki, H.; Mori, S.; Sasaki, K.; Fujibayashi, S.; Takemoto, M.; et al. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Clinical application and the comparison with conventional titanium mesh. J. Cranio-Maxillofac. Surg. 2015, 43, 2183–2188. [Google Scholar] [CrossRef]
- Saini, M.; Singh, Y.; Arora, P.; Arora, V.; Jain, K. Implant biomaterials: A comprehensive review. World J. Clin. Cases 2015, 3, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Ciocca, L.; Ragazzini, S.; Fantini, M.; Corinaldesi, G.; Scotti, R. Work flow for the prosthetic rehabilitation of atrophic patients with a minimal-intervention CAD/CAM approach. J. Prosthet. Dent. 2015, 114, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Al-Radha, A.S.D.; Dymock, D.; Younes, C.; O’Sullivan, D. Surface properties of titanium and zirconia dental implant materials and their effect on bacterial adhesion. J. Dent. 2012, 40, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Ponsonnet, L.; Reybier, K.; Jaffrezic, N.; Comte, V.; Lagneau, C.; Lissac, M.; Martelet, C. Relationship between surface properties (roughness, wettability) of titanium and titanium alloys and cell behaviour. Mater. Sci. Eng. C 2003, 23, 551–560. [Google Scholar] [CrossRef]
- Elias, C.N.; Oshida, Y.; Lima, J.H.C.; Muller, C.A. Relationship between surface properties (roughness, wettability and morphology) of titanium and dental implant removal torque. J. Mech. Behav. Biomed. Mater. 2008, 1, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Le Guehennec, L.; Soueidan, A.; Layrolle, P.; Amouriq, Y. Surface treatments of titanium dental implants for rapid osseointe-gration. Dent. Mater. 2007, 23, 844–854. [Google Scholar] [CrossRef]
- Dank, A.; Aartman, I.H.A.; Wismeijer, D.; Tahmaseb, A. Effect of dental implant surface roughness in patients with a history of periodontal disease: A systematic review and meta-analysis. Int. J. Implant. Dent. 2019, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Rosales-Leal, J.I.; Rodríguez-Valverde, M.A.; Mazzaglia, G.; Ramón-Torregrosa, P.J.; Diaz Rodriguez, L.; García-Martínez, O.; Vallecillo-Capilla, M.; Ruiz, C.; Cabrerizo-Vílchez, M.A. Effect of roughness, wettability and morphology of engineered tita-nium surfaces on osteoblast-like cell adhesion. Colloids Surf. A Physicochem. Eng. Asp. 2010, 365, 222–229. [Google Scholar] [CrossRef]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for 3D Metal Printing in Dentistry. Curr. Oral Health Rep. 2017, 4, 201–208. [Google Scholar] [CrossRef]
- Ciocca, L.; Fantini, M.; De Crescenzio, F. Direct metal laser sintering (DMLS) of a customized titanium mesh for pros-thetically guided bone regeneration of atrophic maxillary arches. Med. Biol. Eng. Comput. 2011, 49, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, A.; Seiler, M. Minimizing risk of customized titanium mesh exposures—A retrospective analysis. BMC Oral Health 2020, 20, 36. [Google Scholar] [CrossRef]
- Otawa, N.; Sumida, T.; Kitagaki, H.; Sasaki, K.; Fujibayashi, S.; Takemoto, M.; Nakamura, T.; Yamada, T.; Mori, Y.; Matsushita, T. Custom-made titanium devices as membranes for bone augmentation in implant treatment: Modeling accuracy of titanium products constructed with selective laser melting. J. Cranio-Maxillofac. Surg. 2015, 43, 1289–1295. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, F.; Calignano, F.; Aversa, A.; Marchese, G.; Lombardi, M.; Biamino, S.; Ugues, D.; Manfredi, D. Additive manufacturing of titanium alloys in the biomedical field: Processes, properties and applications. J. Appl. Biomater. Funct. Mater. 2018, 16, 57–67. [Google Scholar] [CrossRef]
- Inoue, K.; Nakajima, Y.; Omori, M. Reconstruction of the alveolar bone using bone augmentation with selective laser melting titanium mesh sheet: A report of 2 cases. Implant Dent. 2018, 27, 602–607. [Google Scholar] [CrossRef]
- Ortuğ, G. A new device for measuring mastication force (Gnathodynamometer). Ann. Anat. Anat. Anz. 2002, 184, 393–396. [Google Scholar] [CrossRef]
- Shan, X.-F.; Chen, H.-M.; Liang, J.; Huang, J.-W.; Cai, Z.-G. Surgical Reconstruction of Maxillary and Mandibular Defects Using a Printed Titanium Mesh. J. Oral Maxillofac. Surg. 2015, 73, 1437–e1. [Google Scholar] [CrossRef] [PubMed]
- Ciocca, L.; Lizio, G.; Baldissara, P.; Sambuco, A.; Scotti, R.; Corinaldesi, G. Prosthetically CAD-CAM–Guided Bone Augmentation of Atrophic Jaws Using Customized Titanium Mesh: Preliminary Results of an Open Prospective Study. J. Oral Implant. 2018, 44, 131–137. [Google Scholar] [CrossRef]
- Cruz, N.; Martins, M.I.; Santos, J.D.; Gil Mur, J.; Tondela, J.P. Surface Comparison of Three Different Commercial Custom-Made Titanium Meshes Produced by SLM for Dental Applications. Materials 2020, 13, 2177. [Google Scholar] [CrossRef]
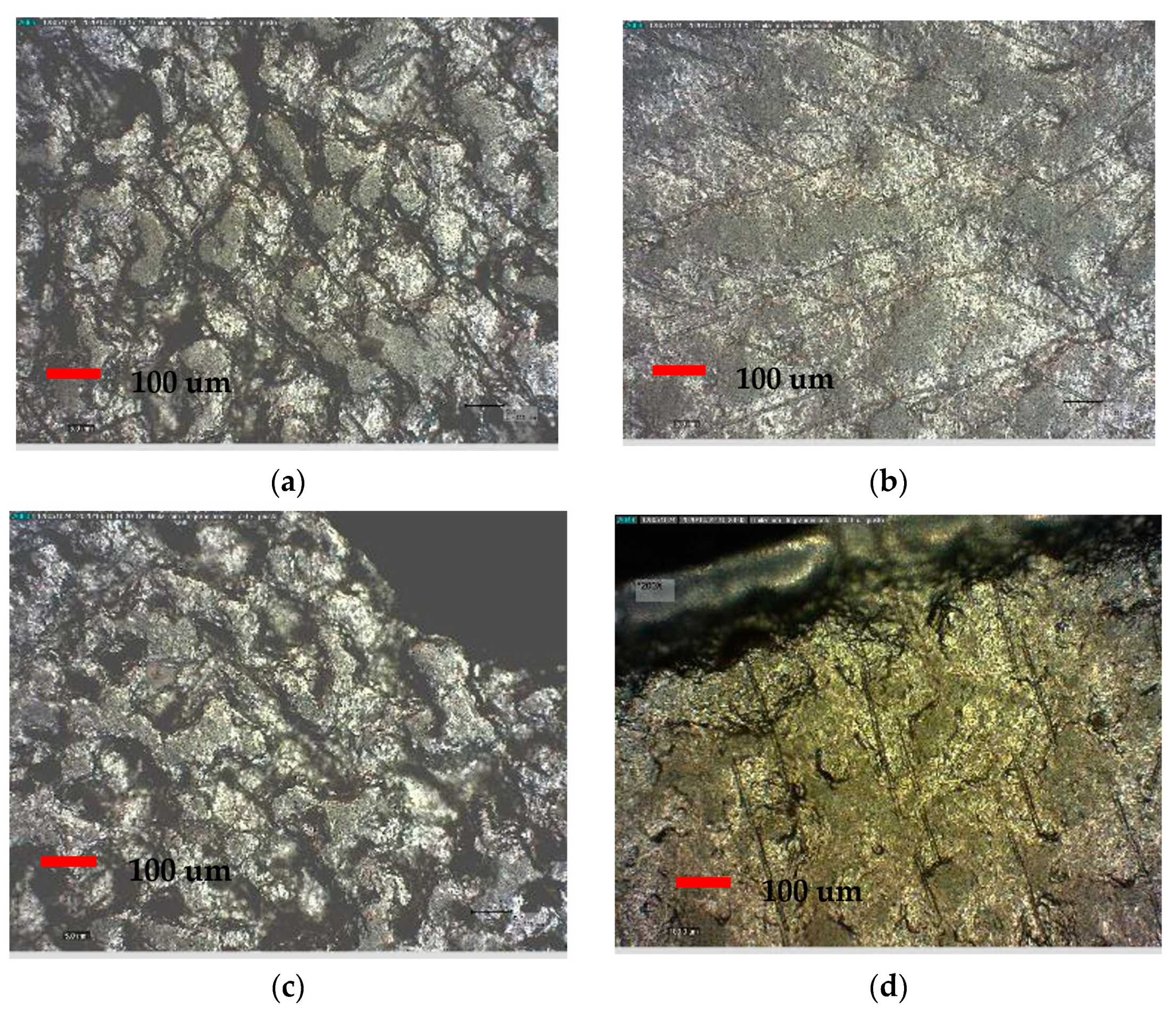


| Lower Face | BTK 7 | BTK 4 | BE 7 | BE 4 |
|---|---|---|---|---|
| Ra | 17.673 μm | 15.636 μm | 1.466 μm | 1.126 μm |
| Rq | 21.553 μm | 19.683 μm | 1.945 μm | 1.474 μm |
| Sigma | 21.555 μm | 19.685 μm | 1.165 μm | 0.883 μm |
| Upper Face | BTK 7 | BTK 4 | BE 7 | BE 4 |
|---|---|---|---|---|
| Ra | 12.125 μm | 7.601 μm | 2.387 μm | 2.103 μm |
| Rq | 13.754 μm | 9.072 μm | 2.833 μm | 2.644 μm |
| Sigma | 13.756 μm | 9.073 μm | 1.697 μm | 1.583 μm |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Angelis, N.; Solimei, L.; Pasquale, C.; Alvito, L.; Lagazzo, A.; Barberis, F. Mechanical Properties and Corrosion Resistance of TiAl6V4 Alloy Produced with SLM Technique and Used for Customized Mesh in Bone Augmentations. Appl. Sci. 2021, 11, 5622. https://doi.org/10.3390/app11125622
De Angelis N, Solimei L, Pasquale C, Alvito L, Lagazzo A, Barberis F. Mechanical Properties and Corrosion Resistance of TiAl6V4 Alloy Produced with SLM Technique and Used for Customized Mesh in Bone Augmentations. Applied Sciences. 2021; 11(12):5622. https://doi.org/10.3390/app11125622
Chicago/Turabian StyleDe Angelis, Nicola, Luca Solimei, Claudio Pasquale, Lorenzo Alvito, Alberto Lagazzo, and Fabrizio Barberis. 2021. "Mechanical Properties and Corrosion Resistance of TiAl6V4 Alloy Produced with SLM Technique and Used for Customized Mesh in Bone Augmentations" Applied Sciences 11, no. 12: 5622. https://doi.org/10.3390/app11125622
APA StyleDe Angelis, N., Solimei, L., Pasquale, C., Alvito, L., Lagazzo, A., & Barberis, F. (2021). Mechanical Properties and Corrosion Resistance of TiAl6V4 Alloy Produced with SLM Technique and Used for Customized Mesh in Bone Augmentations. Applied Sciences, 11(12), 5622. https://doi.org/10.3390/app11125622








