Assessment of Anthropometric and Body Composition Risk Factors in Patients with both Hypertension and Stroke in the Korean Population
Abstract
1. Introduction
2. Materials and Methods
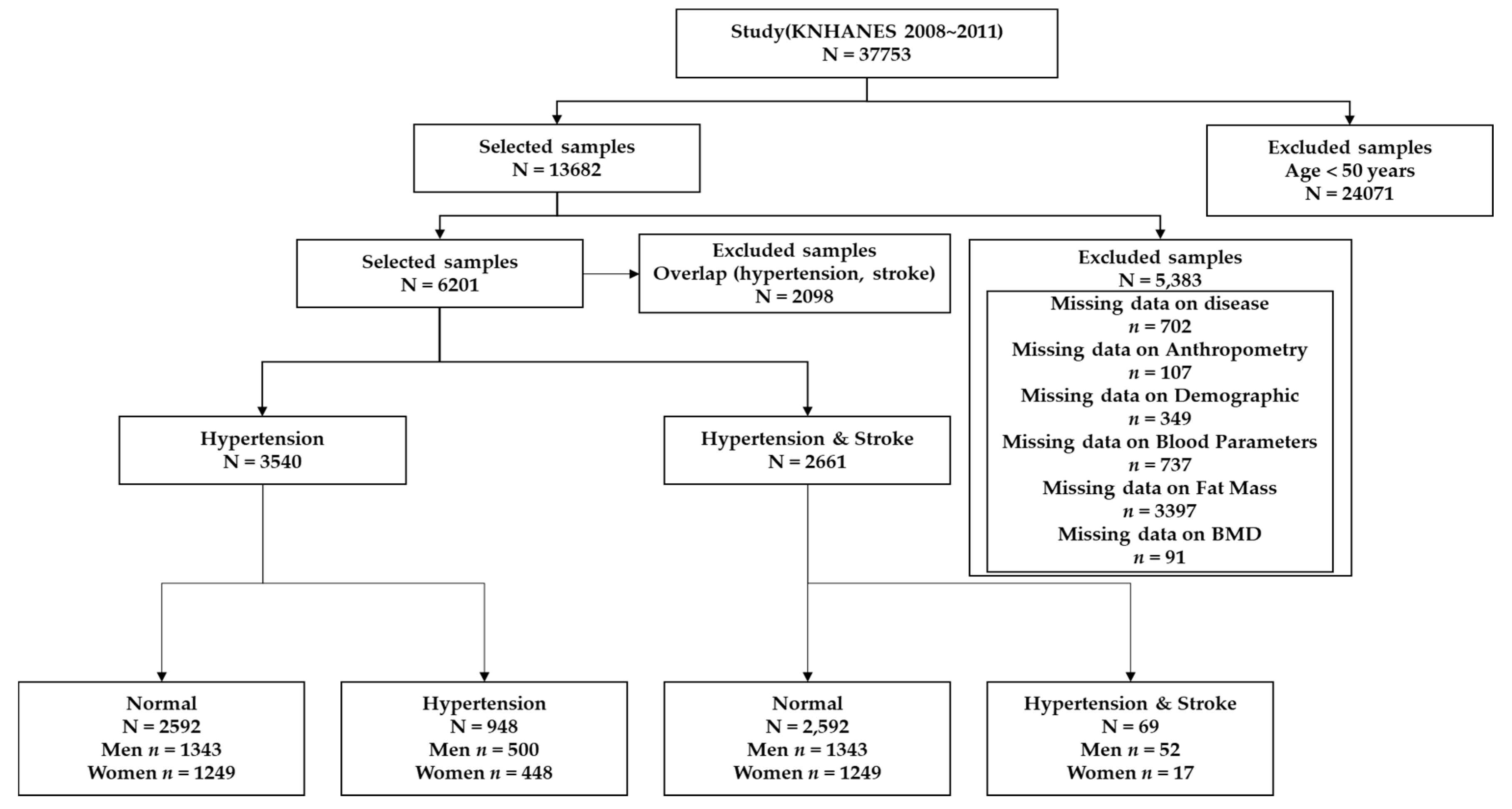
2.1. Subjects and Definitions
2.2. Measurements
2.3. Statistical Analysis
3. Results
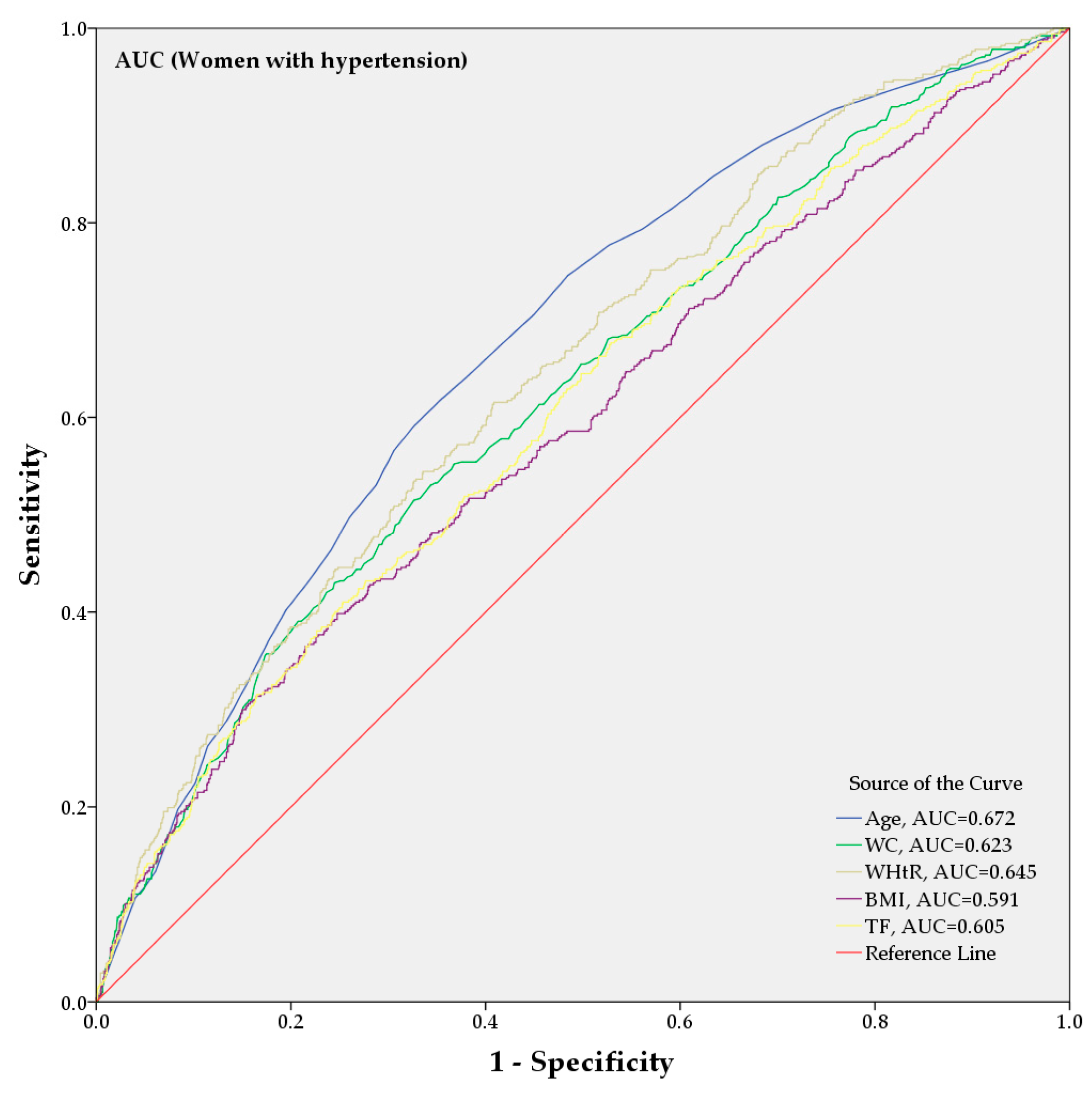
3.1. Associations of Hypertension with Anthropometric and Body Composition Indices
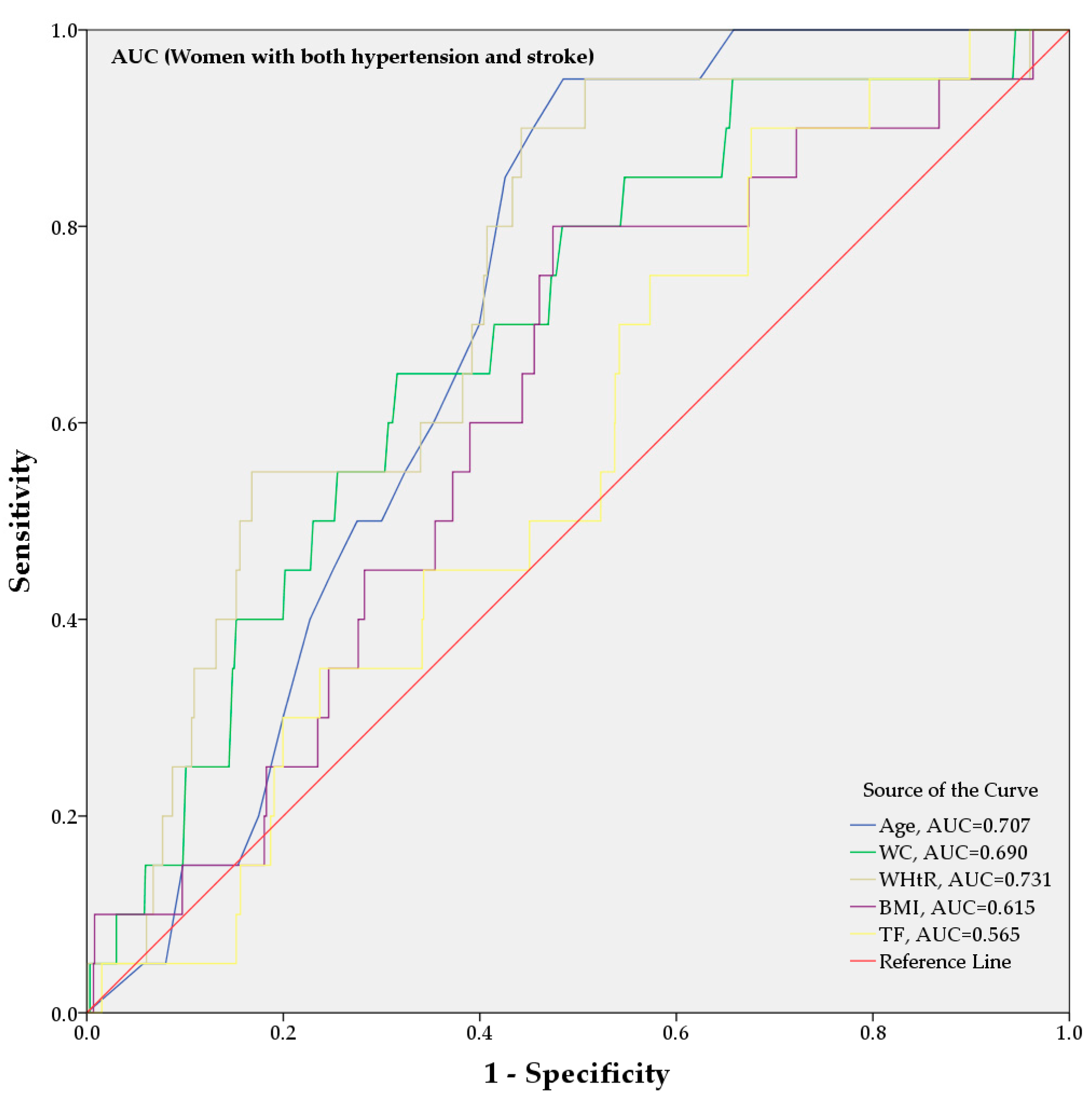
3.2. Comparison of Anthropometric and Body Composition Indices in Patients with Both Hypertension and Stroke
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ohishi, M.; Tatara, Y.; Ito, N.; Takeya, Y.; Onishi, M.; Maekawa, Y.; Kato, N.; Kamide, K.; Rakugi, H. The combination of chronic kidney disease and increased arterial stiffness is a predictor for stroke and cardiovascular disease in hypertensive patients. Hypertens. Res. 2011, 34, 1209–1215. [Google Scholar] [CrossRef]
- Staessen, J.A.; Wang, J.; Bianchi, G.; Birkenhäger, W.H. Essential hypertension. Lancet 2003, 361, 1629–1641. [Google Scholar] [CrossRef]
- Whitworth, J.A.; World Health Organization; International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J. Hypertens. 2003, 21, 1983–1992. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organization. 2013. Available online: https://www.who.int/nmh/publications/ncd-action-plan/en/ (accessed on 24 February 2020).
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics 2020 Update: A report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Hicks, K.A.; Mahaffey, K.W.; Mehran, R.; Nissen, S.E.; Wiviott, S.D.; Dunn, B.; Solomon, S.D.; Marler, J.R.; Teerlink, J.R.; Farb, A.; et al. Standardized Data Collection for Cardiovascular Trials Initiative (SCTI). 2017 Cardiovascular and stroke endpoint definitions for clinical trials. J. Am. Coll. Cardiol. 2018, 71, 1021–1034. [Google Scholar] [CrossRef] [PubMed]
- Mendis, S.; Davis, S.; Norrving, B. Organizational update: The World Health Organization global status report on noncommunicable diseases 2014; one more landmark step in the combat against stroke and vascular disease. Stroke 2015, 46, e121–e122. [Google Scholar] [CrossRef] [PubMed]
- Woo, D.; Haverbusch, M.; Sekar, P.; Kissela, B.; Khoury, J.; Schneider, A.; Kleindorfer, D.; Szaflarski, J.; Pancioli, A.; Jauch, E.; et al. Effect of untreated hypertension on hemorrhagic stroke. Stroke 2004, 35, 1703–1708. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; McNamee, R.; Cruickshank, K. Stroke risk from multiple risk factors combined with hypertension: A primary care based case-control study in a defined population of Northwest England. Ann. Epidemiol. 2000, 10, 380–388. [Google Scholar] [CrossRef]
- Kario, K.; Ishikawa, J.; Pickering, T.G.; Hoshide, S.; Eguchi, K.; Morinari, M.; Hoshide, Y.; Kuroda, T.; Shimada, K. Morning hypertension: The strongest independent risk factor for stroke in elderly hypertensive patients. Hypertens. Res. 2006, 29, 581–587. [Google Scholar] [CrossRef]
- Willmot, M.; Leonardi-Bee, J.; Bath, P.M. High blood pressure in acute stroke and subsequent outcome. Hypertension 2004, 43, 18–24. [Google Scholar] [CrossRef]
- Qureshi, A.I.; Suri, M.F.K.; Kirmani, J.F.; Divani, A.A.; Mohammad, Y. Is prehypertension a risk factor for cardiovascular diseases? Stroke 2005, 36, 1859–1863. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.G.; Fogacci, F.; Giovannini, M.; Grandi, E.; D’Addato, S.; Borghi, C. Interaction between low-density lipoprotein-cholesterolaemia, serum uric level and incident hypertension: Data from the Brisighella Heart Study. J. Hypertens. 2019, 37, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Verdecchia, P.; Reboldi, G.P.; Angeli, F.; Schillaci, G.; Schwartz, J.E.; Pickering, T.G.; Imai, Y.; Ohkubo, T.; Kario, K. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension 2005, 45, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Sarti, C.; Jousilahti, P.; Peltonen, M.; Qiao, Q.; Antikainen, R.; Tuomilehto, J. The impact of history of hypertension and type 2 diabetes at baseline on the incidence of stroke and stroke mortality. Stroke 2005, 36, 2538–2543. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G. Prevention and treatment of stroke in patients with hypertension. Clin. Ther. 2004, 26, 631–648. [Google Scholar] [CrossRef]
- Pringle, E.; Phillips, C.; Thijs, L.; Davidson, C.; Staessen, J.A.; de Leeuw, P.W.; Jaaskivi, M.; Nachev, C.; Parati, G.; O’Brien, E.T.; et al. Syst-Eur investigators. Systolic blood pressure variability as a risk factor for stroke and cardiovascular mortality in the elderly hypertensive population. J. Hypertens. 2003, 21, 2251–2257. [Google Scholar] [CrossRef]
- Brott, T.; Thalinger, K.; Hertzberg, V. Hypertension as a risk factor for spontaneous intracerebral hemorrhage. Stroke 1986, 17, 1078–1083. [Google Scholar] [CrossRef]
- Fuchs, F.D.; Gus, M.; Moreira, L.B.; Moraes, R.S.; Wiehe, M.; Pereira, G.M. Anthropometric indices and the incidence of hypertension: A comparative analysis. Obes. Res. 2005, 13, 1515–1517. [Google Scholar] [CrossRef]
- Dobbelsteyn, C.J.; Joffres, M.R.; MacLean, D.R.; Flowerdew, G.; The Canadian Heart Health Surveys Research Group. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The Canadian Heart Health Surveys. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 652–661. [Google Scholar] [CrossRef]
- Chandra, A.; Neeland, I.J.; Berry, J.D.; Ayers, C.R.; Rohatgi, A.; Das, S.R.; Khera, A.; McGuire, D.K.; de Lemos, J.A.; Turer, A.T. The relationship of body mass and fat distribution with incident hypertension. observations from the Dallas Heart Study. J. Am. Coll. Cardiol. 2014, 64, 997–1002. [Google Scholar] [CrossRef]
- Wiklund, P.; Toss, F.; Weinehall, L.; Hallmans, G.; Franks, P.W.; Nordstrӧm, A. Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J. Clin. Endocrinol. Metab. 2008, 93, 4360–4366. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, K.; Nishio, I.; Masuyama, Y. Bone mineral density in women with essential hypertension. Am. J. Hypertens. 2001, 14, 704–707. [Google Scholar] [CrossRef]
- Winter, Y.; Pieper, L.; Klotsche, J.; Riedel, O.; Wittchen, H.U. Obesity and abdominal fat markers in patients with a history of stroke and transient ischemic attacks. J. Stroke Cerebrovasc. Dis. 2016, 25, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Ye, W.; Adami, H.O.; Weiderpass, E. Prospective study of body size and risk for stroke amongst women below age 60. J. Int. Med. 2006, 260, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Toss, F.; Wiklund, P.; Franks, P.W.; Eriksson, M.; Gustafson, Y.; Hallmans, G.; Nordström, P.; Nordström, A. Abdominal and gynoid adiposity and the risk of stroke. Int. J. Obes. 2011, 35, 1427–1432. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nordström, A.; Eriksson, M.; Stegmayr, B.; Gustafson, Y.; Nordström, P. Low bone mineral density is an independent risk factor for stroke and death. Cerebrovasc. Dis. 2010, 29, 130–136. [Google Scholar] [CrossRef]
- Jørgensen, L.; Engstad, T.; Jacobsen, B.K. Bone mineral density in acute stroke patients: Low bone mineral density may predict first stroke in women. Stroke 2001, 32, 47–51. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare of Korea; Korea Centers for Disease Control and Prevention. The Fourth Korea National Health and Nutrition Examination Survey Data User Guide (KNHANES IV) 2007–2009; Korea Centers for Disease Control and Prevention Press: Cheongju, Korea, 2009.
- Ministry of Health and Welfare of Korea; Korea Centers for Disease Control and Prevention. The Fifth Korea National Health and Nutrition Examination Survey Data User Guide (KNHANES V) 2010–2012; Korea Centers for Disease Control and Prevention Press: Cheongju, Korea, 2012.
- Korea Centers for Disease Control and Prevention: Korea National Health and Nutrition Examination Survey. Available online: https://knhanes.cdc.go.kr/knhanes/eng/index.do (accessed on 20 January 2020).
- Statistics Korea Web Sites. Available online: http://kostat.go.kr (accessed on 24 February 2020).
- Amarbayasgalan, T.; Park, K.H.; Lee, J.Y.; Ryu, K.H. Reconstruction error based deep neural networks for coronary heart disease risk prediction. PLoS ONE 2019, 14, e0225991. [Google Scholar] [CrossRef]
- Ryu, K.S.; Bae, J.W.; Jeong, M.H.; Cho, M.C.; Ryu, K.H.; Other Korea Acute Myocardial Infarction Registry I. Risk scoring system for prognosis estimation of multivessel disease among patients with ST-segment elevation myocardial infarction. Int. Heart J. 2019, 60, 708–714. [Google Scholar] [CrossRef]
- Heo, B.M.; Ryu, K.H. Prediction of prehypertenison and hypertension based on anthropometry, blood parameters, and spirometry. Int. J. Environ. Res. Public Health 2018, 15, 2571. [Google Scholar] [CrossRef]



| Variable | Men | Women | ||
|---|---|---|---|---|
| Normal | Hypertension | Normal | Hypertension | |
| Subjects, no. (%) | 1343 (72.9%) | 500 (27.1%) | 1249 (73.6%) | 448 (26.4%) |
| Age, mean, (SD) † | 61.08 (8.43) | 64.72 (8.54) | 59.84 (8.54) | 65.04 (9.04) |
| Systolic BP (mmHg), mean, (SD) † | 124.90 (17.16) | 134.39 (16.14) | 122.55 (17.44) | 136.24 (16.39) |
| Diastolic BP (mmHg), mean, (SD) † | 80.05 (10.65) | 82.02 (10.68) | 77.03 (10.00) | 81.31 10.83) |
| Height (HT), (cm), mean, (SD) † | 166.84 (6.05) | 165.75 (5.85) | 153.93 (5.95) | 152.35 (6.10) |
| Weight (WT), (kg), mean, (SD) † | 65.09 (9.34) | 66.85 (9.21) | 55.43 (8.18) | 57.10 (9.00) |
| Waist circumference (WC), (cm), mean, (SD) † | 83.77 (7.93) | 86.70 (8.02) | 79.43 (8.61) | 83.59 (8.88) |
| Waist-to-height ratio (WHtR), mean, (SD) † | 0.502 (0.046) | 0.523 (0.049) | 0.517 (0.057) | 0.549 (0.059) |
| Body mass index (BMI) (kg/m2), mean, (SD) † | 23.33 (2.75) | 24.30 (2.84) | 23.36 (2.93) | 24.55 (3.29) |
| Glucose (mg/dL), mean, (SD) † | 97.68 (15.38) | 102.08 (16.62) | 94.83 (14.35) | 99.04 (15.44) |
| Total cholesterol (mg/dL), mean, (SD) * | 190.46 (35.12) | 185.41 (33.80) | 202.47 (33.82) | 203.99 (35.61) |
| High-density lipoprotein (HDL) (mg/dL), mean, (SD) † | 46.27 (11.63) | 44.35 (11.31) | 49.73 (11.03) | 47.32 (10.72) |
| Low-density lipoprotein (LDL) (mg/dL), mean, (SD) † | 113.70 (32.01) | 110.98 (31.16) | 127.70 (29.43) | 129.14 (29.48) |
| Triglycerides (mg/dL), mean, (SD) † | 155.98 (131.75) | 163.61 (123.06) | 121.76 (74.53) | 147.30 (95.62) |
| Body fat mass (g), mean, (SD) | ||||
| Head fat mass (HDF) † | 976.74 (120.53) | 997.59 (127.47) | 854.72 (99.12) | 863.06 (100.96) |
| Left arm fat mass (LAF) † | 723.80 (249.40) | 794.90 (247.05) | 1111.48 (344.13) | 1198.91 (388.46) |
| Right arm fat mass (RAF) † | 734.12 (257.21) | 801.82 (251.37) | 1116.30 (352.34) | 1208.20 (397.23) |
| Trunk fat mass (TF) † | 7749.64 (2945.93) | 9012.72 (3074.65) | 9577.91 (3131.95) | 10,961.25 (3397.55) |
| Left leg fat mass (LLF) † | 1868.20 (623.90) | 2009.38 (618.33) | 2806.96 (814.50) | 2860.79 (862.72) |
| Right leg fat mass (RLF) † | 1910.86 (643.61) | 2043.92 (630.45) | 2875.70 (844.39) | 2917.87 (883.51) |
| Total body fat mass without the head (TBFWH) † | 12,986.62 (4491.04) | 14,662.74 (4589.06) | 17,488.34 (4998.85) | 19,147.02 (5467.79) |
| Total body fat mass (TBF) † | 13,963.36 (4552.24) | 15,660.34 (4655.27) | 18,343.06 (5045.80) | 20,010.08 (5515.59) |
| Bone mineral density (g/cm2), mean, (SD) | ||||
| Head BMD (HDBMD) † | 2.23 (0.38) | 2.20 (0.35) | 2.13 (0.44) | 2.04 (0.41) |
| Left arm BMD (LABMD) * | 0.81 (0.08) | 0.81 (0.08) | 0.64 (0.07) | 0.63 (0.07) |
| Right arm BMD (RABMD) * | 0.82 (0.07) | 0.82 (0.07) | 0.65 (0.07) | 0.64 (0.08) |
| Left Rib BMD (LRibBMD) * | 0.69 (0.09) | 0.70 (0.12) | 0.60 (0.09) | 0.59 (0.07) |
| Right Rib BMD (RRibBMD) * | 0.69 (0.08) | 0.70 (0.08) | 0.60 (0.08) | 0.59 (0.07) |
| Thoracic spine BMD (TSBMD) * | 0.92 (0.15) | 0.95 (0.16) | 0.76 (0.14) | 0.76 (0.20) |
| Lumbar spine BMD (LSBMD) * | 1.06 (0.24) | 1.09 (0.26) | 0.95 (0.27) | 0.92 (0.21) |
| Pelvis BMD (PlvBMD) * | 1.08 (0.15) | 1.10 (0.18) | 0.98 (0.16) | 0.97 (0.17) |
| Left leg BMD (LLBMD) | 1.23 (0.16) | 1.22 (0.14) | 1.01 (0.12) | 1.00 (0.18) |
| Right leg BMD (RLBMD) * | 1.22 (0.14) | 1.23 (0.14) | 1.01 (0.14) | 1.00 (0.16) |
| Total BMD without the head (TBMDWH) * | 1.00 (0.10) | 1.00 (0.10) | 0.83 (0.10) | 0.82 (0.10) |
| Total BMD (TBMD) * | 1.16 (0.12) | 1.16 (0.11) | 1.02 (0.13) | 0.99 (0.12) |
| Variable | Men | Women | ||
|---|---|---|---|---|
| Normal | Hypertension + Stroke | Normal | Hypertension + Stroke | |
| Subjects, no. (%) | 1343 (96.3%) | 52 (3.7%) | 1249 (98.7%) | 17 (1.3%) |
| Age, mean, (SD) † | 61.08 (8.43) | 68.08 (9.05) | 59.84 (8.54) | 67.00 (5.44) |
| Systolic BP (mmHg), mean, (SD) † | 124.90 (17.16) | 135.27 (17.87) | 122.55 (17.44) | 133.47 (13.02) |
| Diastolic BP (mmHg), mean, (SD) | 80.05 (10.65) | 81.60 (11.27) | 77.03 (10.00) | 80.59 (7.71) |
| Height (HT), (cm), mean, (SD) * | 166.84 (6.05) | 164.00 (4.87) | 153.93 (5.95) | 150.65 (5.81) |
| Weight (WT), (kg), mean, (SD) | 65.09 (9.34) | 63.70 (9.11) | 55.43 (8.18) | 57.10 (10.20) |
| Waist circumference (WC), (cm), mean, (SD) * | 83.77 (7.93) | 85.27 (8.33) | 79.43 (8.61) | 86.11 (9.61) |
| Waist-to-height ratio (WHtR), mean, (SD) † | 0.502 (0.046) | 0.520 (0.048) | 0.517 (0.057) | 0.572 (0.069) |
| BMI (kg/m2), mean, (SD) * | 23.33 (2.75) | 23.65 (2.97) | 23.36 (2.93) | 25.08 (3.66) |
| Glucose (mg/dL), mean, (SD) | 97.68 (15.38) | 97.94 (12.42) | 94.83 (14.35) | 96.12 (12.39) |
| Total cholesterol (mg/dL), mean, (SD) | 190.46 (35.12) | 181.25 (33.90) | 202.47 (33.82) | 204.29 (39.79) |
| High-density lipoprotein (HDL) (mg/dL), mean, (SD) * | 46.27 (11.63) | 41.61 (8.51) | 49.73 (11.03) | 51.58 (14.67) |
| Low-density lipoprotein (LDL) (mg/dL), mean, (SD) * | 111.46 (31.00) | 104.64 (33.78) | 129.95 (28.91) | 92.00 (43.84) |
| Triglycerides (mg/dL) * | 155.98 (131.75) | 136.65 (64.45) | 121.76 (74.53) | 135.00 (79.83) |
| Body fat mass (g), mean, (SD) | ||||
| Head fat mass (HDF) | 976.74 (120.53) | 997.67 (144.56) | 854.72 (99.12) | 842.57 (112.95) |
| Left arm fat mass (LAF) | 723.80 (249.40) | 780.29 (283.85) | 1111.48 (344.13) | 1254.23 (510.04) |
| Right arm fat mass (RAF) | 734.12 (257.21) | 803.00 (318.78) | 1116.30 (352.34) | 1190.21 (534.52) |
| Trunk fat mass (TF) * | 7749.64 (2945.93) | 8641.31 (3435.56) | 9577.91 (3131.95) | 10,507.29 (2833.51) |
| Left leg fat mass (LLF) | 1868.20 (623.90) | 2001.40 (693.38) | 2806.96 (814.50) | 2620.02 (789.83) |
| Right leg fat mass (RLF) | 1910.86 (643.61) | 2024.60 (759.46) | 2875.70 (844.39) | 2747.47 (925.45) |
| Total body fat mass without the head (TBFWH) * | 12,986.62 (4491.04) | 14,250.60 (5295.67) | 17,488.34 (4998.85) | 18,319.22 (5029.55) |
| Total body fat mass (TBF) * | 13,963.36 (4552.24) | 15,248.26 (5352.16) | 18,343.06 (5045.80) | 19,161.78 (5111.43) |
| Bone mineral density (g/cm2), mean, (SD) | ||||
| Head BMD (HDBMD) * | 2.23 (0.38) | 2.20 (0.36) | 2.13 (0.44) | 1.88 (0.35) |
| Left arm BMD (LABMD) * | 0.81 (0.08) | 0.77 (0.07) | 0.64 (0.07) | 0.61 (0.07) |
| Right arm BMD (RABMD) * | 0.82 (0.07) | 0.77 (0.07) | 0.65 (0.07) | 0.62 (0.06) |
| Left Rib BMD (LRibBMD) * | 0.69 (0.09) | 0.65 (0.08) | 0.60 (0.09) | 0.57 (0.08) |
| Right Rib BMD (RRibBMD) | 0.69 (0.08) | 0.66 (0.09) | 0.60 (0.08) | 0.59 (0.07) |
| Thoracic spine BMD (TSBMD) | 0.92 (0.15) | 0.90 (0.19) | 0.76 (0.14) | 0.69 (0.11) |
| Lumbar spine BMD (LSBMD) | 1.06 (0.24) | 1.04 (0.23) | 0.95 (0.27) | 1.06 (0.61) |
| Pelvis BMD (PlvBMD) * | 1.08 (0.15) | 1.02 (0.19) | 0.98 (0.16) | 0.91 (0.11) |
| Left leg BMD (LLBMD) * | 1.23 (0.16) | 1.17 (0.21) | 1.01 (0.12) | 0.94 (0.11) |
| Right leg BMD (RLBMD) * | 1.22 (0.14) | 1.14 (0.12) | 1.01 (0.14) | 1.02 (0.28) |
| Total BMD without the head (TBMDWH) | 1.00 (0.10) | 0.95 (0.11) | 0.83 (0.10) | 0.80 (0.09) |
| Total BMD (TBMD) | 1.16 (0.12) | 1.11 (0.12) | 1.02 (0.13) | 0.95 (0.10) |
| Variable | Crude | Adjusted | AUC | ||
|---|---|---|---|---|---|
| p-Value | OR [95% CI] | p-Value | OR [95% CI] | ||
| Age | <0.0001 | 1.441 [1.301–1.597] | - | - | 0.615 [0.588–0.642] |
| Anthropometrics | |||||
| HT | 0.0131 | 0.886 [0.806–0.975] | 0.2930 | 0.941 [0.840–1.054] | 0.448 [0.420–0.477] |
| WT | <0.0001 | 1.404 [1.267–1.556] | 0.2204 | 0.868 [0.691–1.089] | 0.559 [0.531–0.587] |
| WC | <0.0001 | 1.721 [1.527–1.939] | 0.0285 | 1.262 [1.025–1.555] | 0.617 [0.589–0.645] |
| WHtR | <0.0001 | 1.836 [1.627–2.071] | 0.0021 | 1.390 [1.127–1.714] | 0.638 [0.610–0.666] |
| BMI | <0.0001 | 1.652 [1.478–1.847] | - | - | 0.602 [0.574–0.630] |
| Body fat mass | |||||
| HDF | <0.0001 | 1.275 [1.136–1.430] | 0.0999 | 1.130 [0.977–1.306] | 0.546 [0.517–0.574] |
| LAF | <0.0001 | 1.450 [1.291–1.629] | 0.6816 | 1.037 [0.870–1.237] | 0.595 [0.567–0.623] |
| RAF | <0.0001 | 1.421 [1.261–1.602] | 0.6520 | 0.960 [0.803–1.147] | 0.594 [0.566–0.622] |
| TF | <0.0001 | 1.626 [1.443–1.832] | 0.0780 | 1.216 [0.978–1.512] | 0.630 [0.602–0.657] |
| LLF | <0.0001 | 1.342 [1.198–1.503] | 0.3535 | 0.915 [0.758–1.105] | 0.576 [0.548–0.604] |
| RLF | <0.0001 | 1.334 [1.194–1.491] | 0.1414 | 0.872 [0.727–1.047] | 0.571 [0.542–0.599] |
| TBFWH | <0.0001 | 1.560 [1.388–1.754] | 0.4653 | 1.085 [0.871–1.352] | 0.616 [0.588–0.644] |
| TBF | <0.0001 | 1.561 [1.389–1.755] | 0.4338 | 1.092 [0.876–1.362] | 0.616 [0.588–0.644] |
| Bone mineral density | |||||
| HDBMD | 0.0849 | 0.896 [0.791–1.015] | 0.0892 | 0.892 [0.782–1.018] | 0.470 [0.442–0.497] |
| LABMD | 0.3028 | 0.941 [0.838–1.015] | 0.2067 | 0.910 [0.786–1.054] | 0.480 [0.452–0.509] |
| RABMD | 0.6692 | 0.975 [0.865–1.097] | 0.3560 | 0.936 [0.814–1.077] | 0.486 [0.458–0.515] |
| LRibBMD | 0.2566 | 1.064 [0.956–1.183] | 0.7654 | 0.981 [0.862–1.116] | 0.527 [0.498–0.556] |
| RRibBMD | 0.1740 | 1.086 [0.964–1.224] | 0.6772 | 0.972 [0.848–1.113] | 0.523 [0.495–0.552] |
| TSBMD | 0.0330 | 1.126 [1.010–1.256] | 0.6882 | 1.024 [0.910–1.153] | 0.546 [0.517–0.575] |
| LSBMD | 0.0362 | 1.126 [1.008–1.257] | 0.8706 | 1.010 [0.892–1.144] | 0.534 [0.506–0.563] |
| PlvBMD | 0.0079 | 1.183 [1.045–1.339] | 0.3526 | 1.078 [0.920–1.264] | 0.536 [0.507–0.565] |
| LLBMD | 0.5895 | 0.966 [0.853–1.095] | 0.0515 | 0.863 [0.744–1.001] | 0.488 [0.459–0.517] |
| RLBMD | 0.5789 | 1.034 [0.920–1.162] | 0.2969 | 0.932 [0.816–1.064] | 0.499 [0.470–0.528] |
| TBMDWH | 0.6387 | 1.028 [0.915–1.155] | 0.2437 | 0.921 [0.801–1.058] | 0.505 [0.476–0.533] |
| TBMD | 0.5088 | 0.960 [0.851–1.083] | 0.1429 | 0.905 [0.791–1.035] | 0.487 [0.459–0.516] |
| Variable | Crude | Adjusted | AUC | ||
|---|---|---|---|---|---|
| p-Value | OR [95% CI] | p-Value | OR [95% CI] | ||
| Age | <0.0001 | 1.832 [1.658–2.025] | - | - | 0.672 [0.645–0.699] |
| Anthropometrics | |||||
| HT | <0.0001 | 0.714 [0.641–0.794] | 0.6347 | 1.035 [0.898–1.192] | 0.424 [0.395–0.453] |
| WT | 0.0034 | 1.181 [1.057–1.319] | 0.7377 | 1.045 [0.808–1.352] | 0.543 [0.513–0.573] |
| WC | <0.0001 | 1.611 [1.440–1.802] | 0.0492 | 1.231 [1.001–1.515] | 0.623 [0.594–0.651] |
| WHtR | <0.0001 | 1.806 [1.612–2.022] | 0.1120 | 1.200 [0.958–1.503] | 0.645 [0.618–0.673] |
| BMI | <0.0001 | 1.506 [1.344–1.686] | - | - | 0.591 [0.561–0.621] |
| Body fat mass | |||||
| HDF | 0.2283 | 1.081 [0.952–1.228] | 0.9930 | 0.999 [0.854–1.169] | 0.514 [0.484–0.543] |
| LAF | 0.0034 | 1.214 [1.067–1.382] | 0.6388 | 1.061 [0.828–1.359] | 0.550 [0.520–0.580] |
| RAF | 0.0009 | 1.253 [1.097–1.432] | 0.3517 | 1.128 [0.875–1.454] | 0.551 [0.521–0.582] |
| TF | <0.0001 | 1.499 [1.318–1.704] | 0.0004 | 1.613 [1.237–2.104] | 0.605 [0.576–0.634] |
| LLF | 0.8341 | 0.986 [0.868–1.121] | 0.0334 | 0.810 [0.667–0.983] | 0.503 [0.473–0.533] |
| RLF | 0.7817 | 0.982 [0.865–1.115] | 0.0246 | 0.796 [0.652–0.971] | 0.502 [0.472–0.532] |
| TBFWH | <0.0001 | 1.324 [1.165–1.504] | 0.1845 | 1.224 [0.908–1.650] | 0.574 [0.544–0.603] |
| TBF | <0.0001 | 1.322 [1.164–1.503] | 0.1834 | 1.222 [0.909–1.643] | 0.573 [0.544–0.603] |
| Bone mineral density | |||||
| HDBMD | 0.0003 | 0.794 [0.703–0.898] | 0.5566 | 1.046 [0.899–1.218] | 0.435 [0.407–0.464] |
| LABMD | 0.0064 | 0.818 [0.708–0.945] | 0.4255 | 1.076 [0.899–1.287] | 0.432 [0.403–0.461] |
| RABMD | 0.0131 | 0.822 [0.704–0.959] | 0.1185 | 1.128 [0.970–1.311] | 0.427 [0.398–0.456] |
| LRibBMD | 0.0218 | 0.855 [0.748–0.977] | 0.9018 | 1.010 [0.860–1.186] | 0.457 [0.429–0.486] |
| RRibBMD | 0.0182 | 0.854 [0.750–0.973] | 0.8214 | 1.019 [0.868–1.195] | 0.454 [0.425–0.483] |
| TSBMD | 0.6423 | 0.966 [0.835–1.118] | 0.0152 | 1.250 [1.044–1.496] | 0.469 [0.439–0.498] |
| LSBMD | 0.0693 | 0.865 [0.740–1.012] | 0.9101 | 1.006 [0.902–1.123] | 0.462 [0.433–0.491] |
| PlvBMD | 0.0480 | 0.866 [0.750–0.999] | 0.0825 | 1.159 [0.981–1.369] | 0.446 [0.417–0.476] |
| LLBMD | 0.2998 | 0.920 [0.786–1.077] | 0.0237 | 1.189 [1.024–1.381] | 0.449 [0.419–0.478] |
| RLBMD | 0.0573 | 0.848 [0.715–1.005] | 0.5263 | 1.049 [0.904–1.218] | 0.438 [0.409–0.468] |
| TBMDWH | 0.0071 | 0.829 [0.723–0.950] | 0.1721 | 1.130 [0.948–1.348] | 0.438 [0.409–0.467] |
| TBMD | 0.0006 | 0.797 [0.701–0.907] | 0.2710 | 1.096 [0.931–1.291] | 0.430 [0.401–0.459] |
| Variable | Crude | Adjusted | AUC | ||
|---|---|---|---|---|---|
| p-Value | OR [95% CI] | p-Value | OR [95% CI] | ||
| Age | <0.0001 | 2.156 [1.644–2.828] | - | - | 0.689 [0.617–0.761] |
| Anthropometrics | |||||
| HT | 0.0003 | 0.666 [0.533–0.831] | 0.3166 | 0.859 [0.639–1.156] | 0.375 [0.308–0.441] |
| WT | 0.9359 | 1.010 [0.783–1.304] | 0.2595 | 0.707 [0.387–1.292] | 0.451 [0.379–0.523] |
| WC | 0.0026 | 1.519 [1.157–1.993] | 0.2111 | 1.404 [0.824–2.392] | 0.549 [0.470–0.627] |
| WHtR | <0.0001 | 1.797 [1.382–2.336] | 0.0217 | 1.689 [1.080–2.641] | 0.593 [0.514–0.671] |
| BMI | 0.0336 | 1.329 [1.022–1.728] | - | - | 0.513 [0.433–0.593] |
| Body fat mass | |||||
| HDF | 0.4369 | 1.149 [0.809–1.633] | 0.5465 | 1.156 [0.721–1.853] | 0.535 [0.455–0.615] |
| LAF | 0.0949 | 1.319 [0.953–1.827] | 0.9613 | 1.012 [0.634–1.614] | 0.535 [0.457–0.612] |
| RAF | 0.0471 | 1.411 [1.005–1.981] | 0.5363 | 1.194 [0.679–2.100] | 0.548 [0.469–0.628] |
| TF | 0.0265 | 1.506 [1.049–2.162] | 0.1542 | 1.664 [0.825–3.354] | 0.551 [0.475–0.627] |
| LLF | 0.0297 | 1.417 [1.035–1.940] | 0.5694 | 1.162 [0.693–1.947] | 0.544 [0.466–0.622] |
| RLF | 0.0447 | 1.409 [1.008–1.969] | 0.6374 | 1.137 [0.667–1.937] | 0.527 [0.447–0.607] |
| TBFWH | 0.0257 | 1.495 [1.050–2.128] | 0.2564 | 1.509 [0.741–3.075] | 0.547 [0.470–0.624] |
| TBF | 0.0256 | 1.493 [1.050–2.122] | 0.2454 | 1.518 [0.750–3.071] | 0.547 [0.470–0.624] |
| Bone mineral density | |||||
| HDBMD | 0.9911 | 0.999 [0.774–1.289] | 0.8488 | 1.027 [0.780–1.353] | 0.483 [0.413–0.553] |
| LABMD | <0.0001 | 0.542 [0.396–0.742] | 0.0031 | 0.504 [0.320–0.793] | 0.336 [0.264–0.408] |
| RABMD | <0.0001 | 0.531 [0.384–0.735] | 0.0054 | 0.528 [0.337–0.827] | 0.319 [0.246–0.391] |
| LRibBMD | 0.0591 | 0.693 [0.474–1.014] | 0.0668 | 0.626 [0.379–1.033] | 0.373 [0.304–0.443] |
| RRibBMD | 0.4213 | 0.879 [0.642–1.204] | 0.5078 | 0.890 [0.629–1.258] | 0.410 [0.334–0.487] |
| TSBMD | 0.9624 | 1.012 [0.624–1.640] | 0.8941 | 0.969 [0.606–1.548] | 0.426 [0.341–0.511] |
| LSBMD | 0.6851 | 1.063 [0.791–1.427] | 0.7056 | 0.944 [0.701–1.272] | 0.452 [0.368–0.537] |
| PlvBMD | 0.4977 | 0.837 [0.499–1.403] | 0.5975 | 0.866 [0.507–1.479] | 0.389 [0.312–0.466] |
| LLBMD | 0.5718 | 0.833 [0.442–1.571] | 0.6264 | 0.856 [0.456–1.605] | 0.343 [0.269–0.417] |
| RLBMD | 0.0078 | 0.570 [0.377–0.862] | 0.0117 | 0.537 [0.331–0.870] | 0.318 [0.248–0.388] |
| TBMDWH | 0.0872 | 0.692 [0.454–1.055] | 0.1221 | 0.689 [0.429–1.105] | 0.351 [0.276–0.426] |
| TBMD | 0.2079 | 0.800 [0.564–1.133] | 0.3021 | 0.833 [0.589–1.179] | 0.389 [0.319–0.458] |
| Variable | Crude | Adjusted | AUC | ||
|---|---|---|---|---|---|
| p-Value | OR [95% CI] | p-Value | OR [95% CI] | ||
| Age | <0.0001 | 2.097 [1.588–2.770] | - | - | 0.707 [0.640–0.774] |
| Anthropometrics | |||||
| HT | <0.0001 | 0.607 [0.474–0.778] | 0.6095 | 0.922 [0.674–1.261] | 0.370 [0.257–0.483] |
| WT | 0.5579 | 0.891 [0.604–1.313] | 0.8087 | 0.928 [0.506–1.701] | 0.521 [0.398–0.643] |
| WC | 0.0672 | 1.337 [0.980–1.824] | 0.8647 | 1.069 [0.494–2.315] | 0.690 [0.583–0.798] |
| WHtR | 0.0008 | 1.564 [1.204–2.031] | 0.7622 | 1.138 [0.493–2.624] | 0.731 [0.632–0.829] |
| BMI | 0.2297 | 1.202 [0.890–1.624] | - | - | 0.615 [0.503–0.728] |
| Body fat mass | |||||
| HDF | 0.7080 | 0.910 [0.554–1.493] | 0.6517 | 0.883 [0.515–1.515] | 0.468 [0.339–0.597] |
| LAF | 0.3996 | 1.280 [0.720–2.278] | 0.2710 | 1.588 [0.696–3.625] | 0.526 [0.404–0.649] |
| RAF | 0.6832 | 1.127 [0.634–2.005] | 0.7463 | 0.833 [0.274–2.529] | 0.460 [0.345–0.576] |
| TF | 0.1588 | 1.270 [0.910–1.771] | 0.3458 | 0.627 [0.238–1.656] | 0.565 [0.459–0.671] |
| LLF | 0.2851 | 0.785 [0.504–1.224] | 0.0036 | 0.391 [0.208–0.734] | 0.430 [0.309–0.550] |
| RLF | 0.4357 | 0.825 [0.508–1.339] | 0.0211 | 0.460 [0.237–0.890] | 0.436 [0.314–0.557] |
| TBFWH | 0.5755 | 1.121 [0.752–1.671] | 0.1221 | 0.367 [0.103–1.309] | 0.519 [0.409–0.629] |
| TBF | 0.5882 | 1.118 [0.747–1.672] | 0.1219 | 0.362 [0.100–1.313] | 0.517 [0.407–0.628] |
| Bone mineral density | |||||
| HDBMD | 0.2313 | 0.689 [0.373–1.270] | 0.6477 | 0.809 [0.326–2.011] | 0.356 [0.247–0.465] |
| LABMD | 0.2648 | 0.735 [0.427–1.264] | 0.7778 | 0.920 [0.513–1.649] | 0.392 [0.267–0.517] |
| RABMD | 0.1083 | 0.688 [0.436–1.086] | 0.6895 | 0.876 [0.458–1.678] | 0.395 [0.284–0.505] |
| LRibBMD | 0.5438 | 0.861 [0.532–1.396] | 0.9571 | 0.982 [0.498–1.936] | 0.426 [0.300–0.551] |
| RRibBMD | 0.9698 | 0.993 [0.676–1.458] | 0.3437 | 1.179 [0.838–1.660] | 0.472 [0.356–0.587] |
| TSBMD | 0.0802 | 0.647 [0.397–1.054] | 0.3423 | 0.756 [0.424–1.348] | 0.352 [0.246–0.457] |
| LSBMD | 0.3061 | 1.152 [0.878–1.510] | 0.1156 | 1.211 [0.954–1.539] | 0.430 [0.282–0.579] |
| PlvBMD | 0.0161 | 0.593 [0.387–0.907] | 0.1079 | 0.551 [0.266–1.140] | 0.375 [0.277–0.473] |
| LLBMD | 0.0445 | 0.542 [0.298–0.985] | 0.2716 | 0.656 [0.309–1.393] | 0.359 [0.245–0.473] |
| RLBMD | 0.8163 | 0.906 [0.391–2.095] | 0.5771 | 1.113 [0.764–1.620] | 0.388 [0.262–0.513] |
| TBMDWH | 0.1298 | 0.698 [0.438–1.112] | 0.5830 | 0.850 [0.475–1.520] | 0.403 [0.285–0.521] |
| TBMD | 0.1519 | 0.687 [0.411–1.149] | 0.5981 | 0.828 [0.411–1.670] | 0.374 [0.263–0.486] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Nam, G.H. Assessment of Anthropometric and Body Composition Risk Factors in Patients with both Hypertension and Stroke in the Korean Population. Appl. Sci. 2020, 10, 3046. https://doi.org/10.3390/app10093046
Kim SY, Nam GH. Assessment of Anthropometric and Body Composition Risk Factors in Patients with both Hypertension and Stroke in the Korean Population. Applied Sciences. 2020; 10(9):3046. https://doi.org/10.3390/app10093046
Chicago/Turabian StyleKim, Sang Yeob, and Gyeong Hee Nam. 2020. "Assessment of Anthropometric and Body Composition Risk Factors in Patients with both Hypertension and Stroke in the Korean Population" Applied Sciences 10, no. 9: 3046. https://doi.org/10.3390/app10093046
APA StyleKim, S. Y., & Nam, G. H. (2020). Assessment of Anthropometric and Body Composition Risk Factors in Patients with both Hypertension and Stroke in the Korean Population. Applied Sciences, 10(9), 3046. https://doi.org/10.3390/app10093046




