Biomechanical Evaluation of Sagittal Split Ramus Osteotomy Fixation Techniques in Mandibular Setback
Abstract
1. Introduction
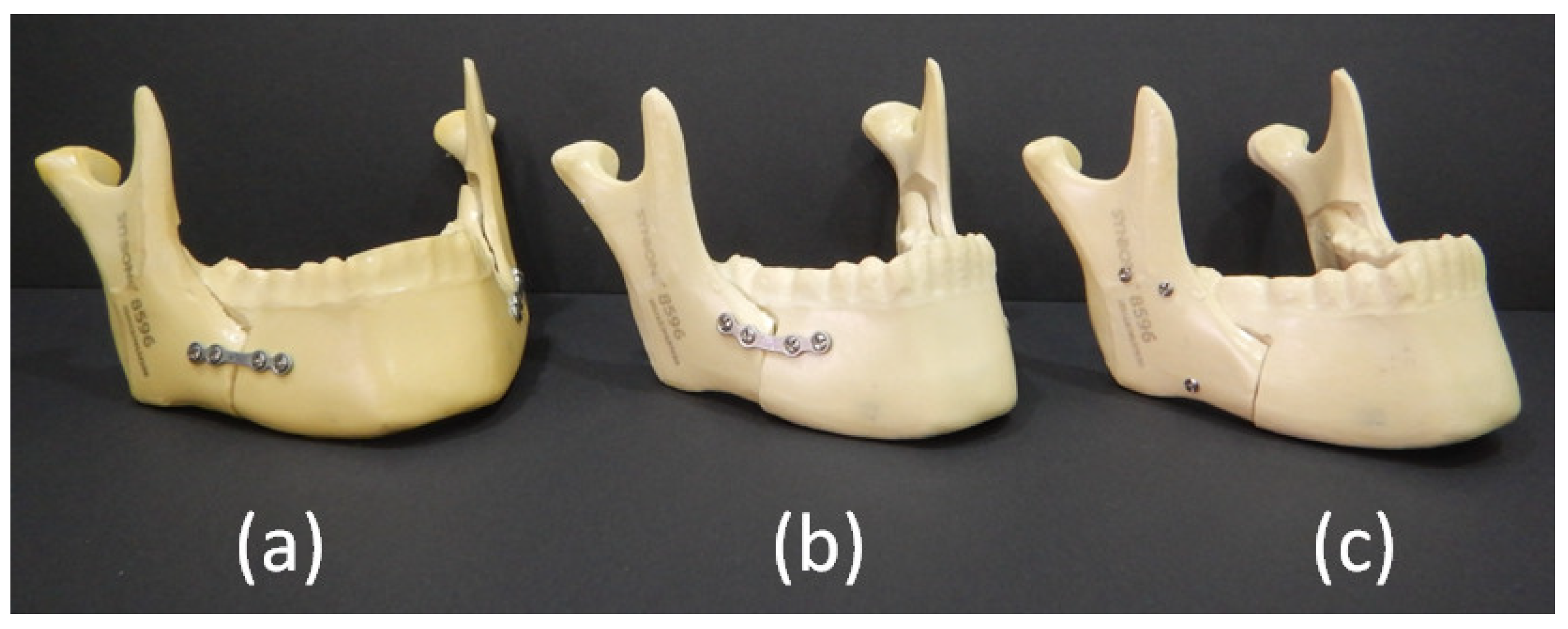
2. Materials and Methods
2.1. Specimen Preparation
2.2. Measurement of Fixation Ability
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- (1)
- The resistance force of Groups 2 and 3 indicated better bone fixation than Group 1.
- (2)
- The resistance force at 1, 3, and 5 mm displacement was significantly the same for Groups 2 and 3.
Author Contributions
Funding
Conflicts of Interest
References
- Islam, I.; Lim, A.; Wong, R.C.W. Changes in bite force after orthognathic surgical correction of mandibular prognathism: A systematic review. Int. J. Oral Maxillofac. Surg. 2017, 46, 746–755. [Google Scholar] [CrossRef] [PubMed]
- Verweij, J.; Houppermans, P.N.; Gooris, P.; Mensink, G.; Van Merkesteyn, J. Risk factors for common complications associated with bilateral sagittal split osteotomy: A literature review and meta-analysis. J. Cranio-Maxillofac. Surg. 2016, 44, 1170–1180. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.I.; Sinkford, J.C.; Sanders, C.F. The 100-year dilemma: What is a normal occlusion, and how is malocclusion classified? Quintessence Int. 1990, 21, 21. [Google Scholar]
- Obwegeser, H.L. Orthognathic Surgery and a Tale of How Three Procedures Came to Be: A Letter to the Next Generations of Surgeons. Clin. Plast. Surg. 2007, 34, 331–355. [Google Scholar] [CrossRef]
- Joss, C.U.; Vassalli, I.M. Stability After Bilateral Sagittal Split Osteotomy Advancement Surgery with Rigid Internal Fixation: A Systematic Review. J. Oral Maxillofac. Surg. 2009, 67, 301–313. [Google Scholar] [CrossRef]
- Hoffmannová, J.; Foltan, R.; Vlk, M.; Klíma, K.; Pavlíková, G.; Bulik, O. Factors affecting the stability of bilateral sagittal split osteotomy of a mandible. Prague Med. Rep. 2008, 109, 286–297. [Google Scholar]
- Eggensperger, N.; Raditsch, T.; Taghizadeh, F.; Iizuka, T. Mandibular setback by sagittal split ramus osteotomy: A 12-year follow-up. Acta Odontol. Scand. 2005, 63, 183–188. [Google Scholar] [CrossRef]
- Tharanon, W. Comparison between the rigidity of bicortical screws and a miniplate for fixation of a mandibular setback after a simulated bilateral sagittal split osteotomy. J. Oral Maxillofac. Surg. 1998, 56, 1055–1058. [Google Scholar] [CrossRef]
- Özden, B.; Alkan, A.; Arici, S.; Erdem, E. In vitro comparison of biomechanical characteristics of sagittal split osteotomy fixation techniques. Int. J. Oral Maxillofac. Surg. 2006, 35, 837–841. [Google Scholar] [CrossRef]
- Peterson, G.P.; Haug, R.H.; Van Sickels, J. A Biomechanical Evaluation of Bilateral Sagittal Ramus Osteotomy Fixation Techniques. J. Oral Maxillofac. Surg. 2005, 63, 1317–1324. [Google Scholar] [CrossRef]
- Van Sickels, J.E.; Peterson, G.P.; Holms, S.; Haug, R.H. An In Vitro Comparison of an Adjustable Bone Fixation System. J. Oral Maxillofac. Surg. 2005, 63, 1620–1625. [Google Scholar] [CrossRef] [PubMed]
- Hadi, G.; Karine, B.-G.; Yves, C.; Pierre, L. Stability of osteosynthesis with bicortical screws placed in a triangular shape in mandibular sagittal split 5mm advancement osteotomy: Biomechanical tests. Br. J. Oral Maxillofac. Surg. 2010, 48, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Dolanmaz, D.; Uçkan, S.; Isik, K.; Sağlam, H.; Saglam, H. Comparison of stability of absorbable and titanium plate and screw fixation for sagittal split ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2004, 42, 127–132. [Google Scholar] [CrossRef]
- Oguz, Y.; Sağlam, H.; Dolanmaz, D.; Uçkan, S.; Saglam, H. Comparison of stability of 2.0mm standard and 2.0mm locking miniplate/screws for the fixation of sagittal split ramus osteotomy on sheep mandibles. Br. J. Oral Maxillofac. Surg. 2011, 49, 135–137. [Google Scholar] [CrossRef] [PubMed]
- De Olivera, L.B.; Manzato, A.J.; Guerra, F.L.B.; Arnett, G.W. Biomechanical in vitro evaluation of three stable internal fixation techniques used in sagittal osteotomy of the mandibular ramus: A study in sheep mandibles. J. Appl. Oral Sci. 2012, 20, 419–426. [Google Scholar] [CrossRef]
- Brasileiro, B.F.; Grotta-Grempel, R.; Ambrosano, G.M.B.; Passeri, L.A. An In Vitro Evaluation of Rigid Internal Fixation Techniques for Sagittal Split Ramus Osteotomies: Setback Surgery. J. Oral Maxillofac. Surg. 2012, 70, 941–951. [Google Scholar] [CrossRef]
- Brasileiro, B.F.; Grempel, R.G.; Ambrosano, G.M.B.; Passeri, L.A. An In Vitro Evaluation of Rigid Internal Fixation Techniques for Sagittal Split Ramus Osteotomies: Advancement Surgery. J. Oral Maxillofac. Surg. 2009, 67, 809–817. [Google Scholar] [CrossRef]
- Filho, V.P.; Iamashita, H.; Monnazzi, M.; Gabrielli, M.; Vaz, L.G.; Passeri, L.A. In vitro biomechanical evaluation of sagittal split osteotomy fixation with a specifically designed miniplate. Int. J. Oral Maxillofac. Surg. 2013, 42, 316–320. [Google Scholar] [CrossRef]
- Şener, I.; Arici, S.; Bereket, C.; Tek, M. In Vitro Biomechanical Evaluation of Modified Plating Techniques for Bilateral Sagittal Split Ramus Osteotomy in Mandibular Advancement. J. Craniofacial Surg. 2012, 23, 1573–1576. [Google Scholar] [CrossRef]
- Oguz, Y.; Watanabe, E.; Reis, J.; Spin-Neto, R.; Gabrielli, M.; Filho, V.P. In vitro biomechanical comparison of six different fixation methods following 5-mm sagittal split advancement osteotomies. Int. J. Oral Maxillofac. Surg. 2015, 44, 984–988. [Google Scholar] [CrossRef]
- Sato, F.; Asprino, L.; Noritomi, P.; Da Silva, J.V.L.; De Moraes, M. Comparison of five different fixation techniques of sagittal split ramus osteotomy using three-dimensional finite elements analysis. Int. J. Oral Maxillofac. Surg. 2012, 41, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Elfar, J.; Stanbury, S.; Menorca, R.M.G.; Reed, J.D. Composite bone models in orthopaedic surgery research and education. J. Am. Acad. Orthop. Surg. 2014, 22, 111. [Google Scholar] [PubMed]
- Chiu, Y.-C.; Tsai, M.-T.; Hsu, C.-E.; Hsu, H.-C.; Huang, H.-L.; Hsu, J.-T. New fixation approach for transverse metacarpal neck fracture: A biomechanical study. J. Orthop. Surg. Res. 2018, 13, 183. [Google Scholar] [CrossRef] [PubMed]
- Bredbenner, T.L.; Haug, R.H. Substitutes for human cadaveric bone in maxillofacial rigid fixation research. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2000, 90, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro-Junior, P.D.; Magro-Filho, O.; Shastri, K.A.; Papageorge, M.B. In Vitro Biomechanical Evaluation of the Use of Conventional and Locking Miniplate/Screw Systems for Sagittal Split Ramus Osteotomy. J. Oral Maxillofac. Surg. 2010, 68, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Kim, S.-G. In vitro biomechanical evaluation of fixation methods of sagittal split ramus osteotomy in mandibular setback. J. Cranio-Maxillofac. Surg. 2015, 43, 186–191. [Google Scholar] [CrossRef]
- Al-Bishri, A.; Barghash, Z.; Rosenquist, J.; Sunzel, B. Neurosensory disturbance after sagittal split and intraoral vertical ramus osteotomy: As reported in questionnaires and patients’ records. Int. J. Oral Maxillofac. Surg. 2005, 34, 247–251. [Google Scholar] [CrossRef]
- Jacks, S.C.; Zuniga, J.; Turvey, T.A.; Schalit, C. A retrospective analysis of lingual nerve sensory changes after mandibular bilateral sagittal split osteotomy. J. Oral Maxillofac. Surg. 1998, 56, 700–704. [Google Scholar] [CrossRef]
- Ingeborg, M. Watzke. Mandibular Surgery: Prevention and Management of Complications. Oral and Maxillofacial Surgery, 3rd. ed.; Fonseca, R., Ed.; WB Saunders: Philadelphia, PA, USA, 2018; Volume 3, pp. 317–318. [Google Scholar]

| Type of Fixation | Model No. | Resistance Force | |||
|---|---|---|---|---|---|
| 1 mm | 3 mm | 5 mm | 10 mm | ||
| Group 1 (Straight plate) | 1 | 15 | 29.4 | 40.2 | 57.1 |
| 2 | 5.1 | 18.5 | 36.6 | 91.2 | |
| 3 | 11.0 | 27.2 | 41.2 | 66.3 | |
| 4 | 10.2 | 19.0 | 41.7 | 67.0 | |
| 5 | 11.3 | 19.2 | 40 | 59.2 | |
| 6 | 16.0 | 21.0 | 39.2 | 61.0 | |
| 7 | 12.1 | 20.2 | 38 | 63.2 | |
| 8 | 9.1 | 17.3 | 38 | 71.1 | |
| Group 2 (Curved plate) | 1 | 22.6 | 44.5 | 63.1 | 105.0 |
| 2 | 9.7 | 43.5 | 78.2 | 125.9 | |
| 3 | 18.1 | 51.0 | 71.3 | 110.0 | |
| 4 | 20.2 | 55.2 | 69 | 108.2 | |
| 5 | 21.0 | 49.6 | 77.1 | 113.0 | |
| 6 | 23.2 | 50.0 | 76.1 | 103.0 | |
| 7 | 27.1 | 52.6 | 75.8 | 102.2 | |
| 8 | 25.2 | 57.1 | 68.2 | 109.3 | |
| Group 3 (Inverted-L bicortical screw) | 1 | 18.2 | 49.3 | 78.7 | 145.0 |
| 2 | 19.1 | 52.3 | 74.3 | 139.1 | |
| 3 | 22.0 | 56.2 | 77.4 | 141.2 | |
| 4 | 24.1 | 61.1 | 80.1 | 148.2 | |
| 5 | 21.2 | 59.3 | 81.0 | 150.0 | |
| 6 | 19.8 | 55.8 | 77.9 | 139.2 | |
| 7 | 21.5 | 58.0 | 78.2 | 147.7 | |
| 8 | 21.9 | 59.2 | 72.0 | 148.0 | |
| Unit: N | |||||
| Amount of Displacement | Group 1 (Straight Plate) | Group 2 (Curved Plate) | Group 3 (Inverted-L Bicortical Screw) |
|---|---|---|---|
| 1 mm | 11.15 ± 4.90 | 21.80 ± 6.08 | 21.35 ± 2.70 |
| 3 mm | 19.70 ± 7.03 | 50.50 ± 8.78 | 57.10 ± 6.10 |
| 5 mm | 39.60 ± 2.95 | 73.55 ± 8.45 | 78.05 ± 4.68 |
| 10 mm | 64.75 ± 10.43 | 108.75 ± 8.75 | 146.35 ± 8.45 |
| Unit: N | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, M.Y.C.; Wu, Y.-F.; Huang, H.-L.; Hsu, J.-T. Biomechanical Evaluation of Sagittal Split Ramus Osteotomy Fixation Techniques in Mandibular Setback. Appl. Sci. 2020, 10, 3031. https://doi.org/10.3390/app10093031
Chen MYC, Wu Y-F, Huang H-L, Hsu J-T. Biomechanical Evaluation of Sagittal Split Ramus Osteotomy Fixation Techniques in Mandibular Setback. Applied Sciences. 2020; 10(9):3031. https://doi.org/10.3390/app10093031
Chicago/Turabian StyleChen, Michael Y. C., Yi-Fan Wu, Heng-Li Huang, and Jui-Ting Hsu. 2020. "Biomechanical Evaluation of Sagittal Split Ramus Osteotomy Fixation Techniques in Mandibular Setback" Applied Sciences 10, no. 9: 3031. https://doi.org/10.3390/app10093031
APA StyleChen, M. Y. C., Wu, Y.-F., Huang, H.-L., & Hsu, J.-T. (2020). Biomechanical Evaluation of Sagittal Split Ramus Osteotomy Fixation Techniques in Mandibular Setback. Applied Sciences, 10(9), 3031. https://doi.org/10.3390/app10093031





