Donning/Doffing and Arm Positioning Influence in Upper Limb Adaptive Prostheses Control
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Acquisition
2.2. Method
- Estimate the new predicted position :
- Calculate the error between the real position and the estimated one for each direction:
- Update the vectors filtering the output and input signals with the AR part of the model, obtaining the new signals and :
- Update the matrices and the model parameters:where is a forgetting factor, typically , that establishes the importance of previous observations when obtaining the new estimate. In terms of the cost function:If , the algorithm has an everlasting memory, and all samples are considered to estimate the present coefficients. The parameter is the convergence factor, and usually .
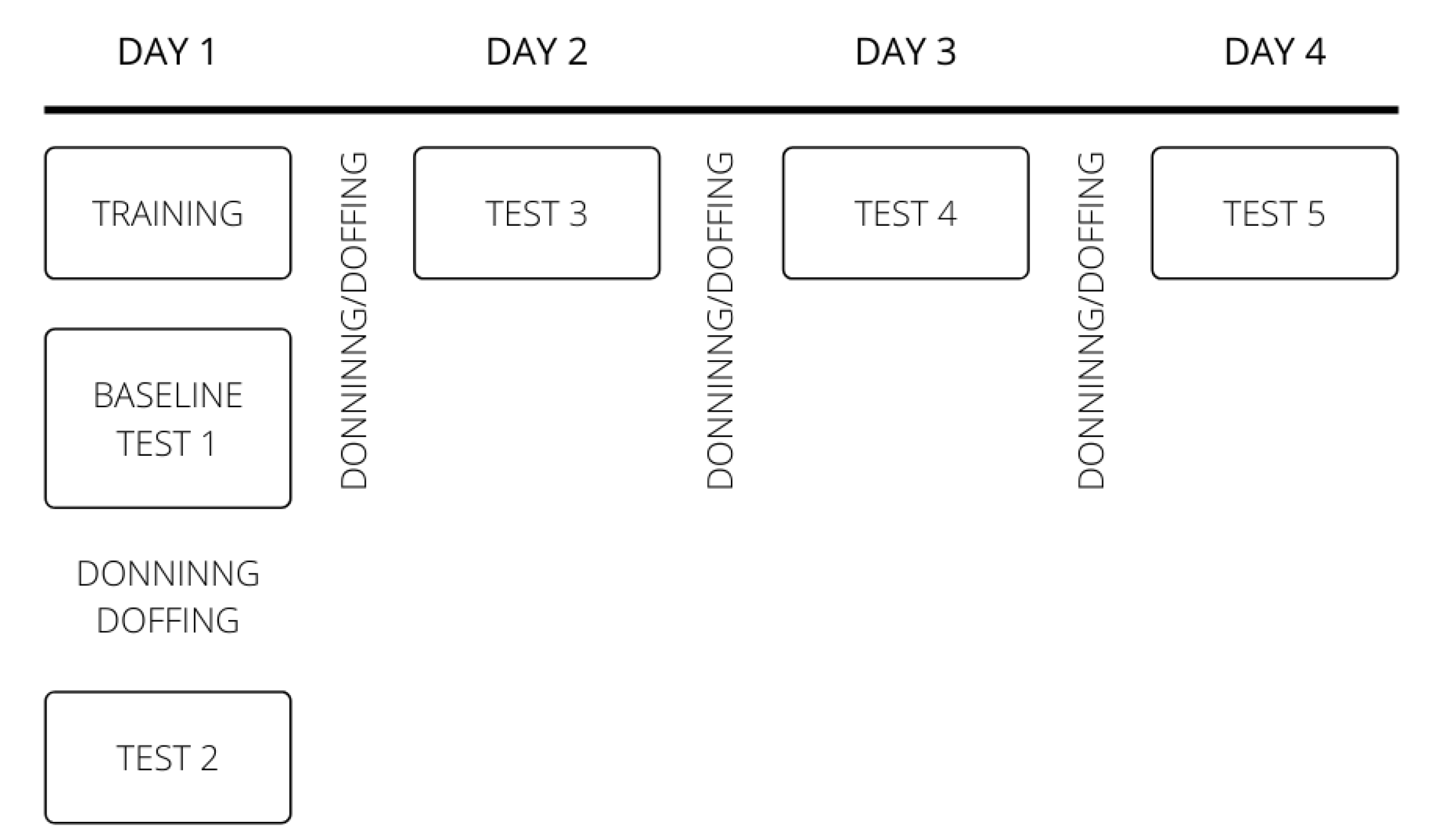
2.3. Study Design
2.3.1. Training Phase
2.3.2. Test Phase
2.4. Experimental Paradigm
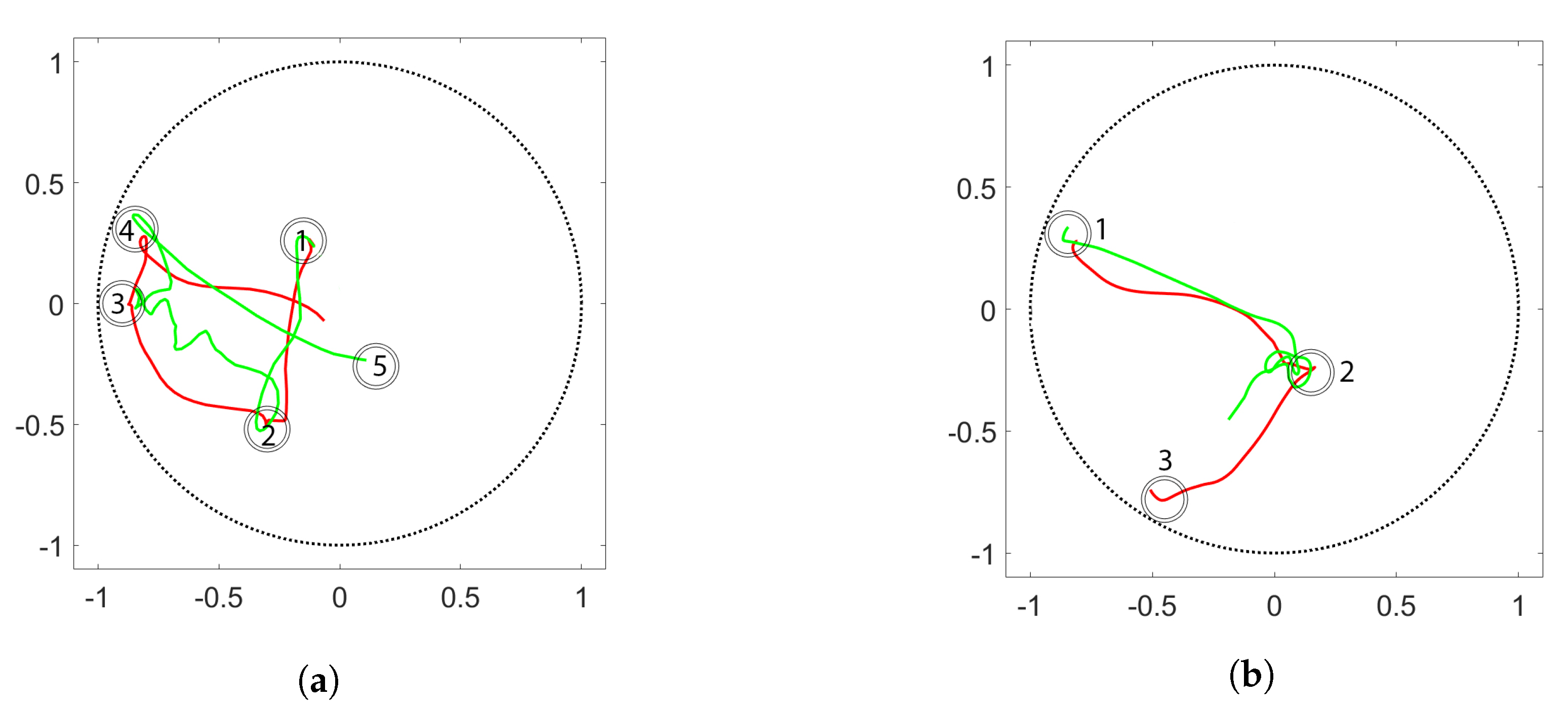
2.4.1. Donning and Doffing Protocol
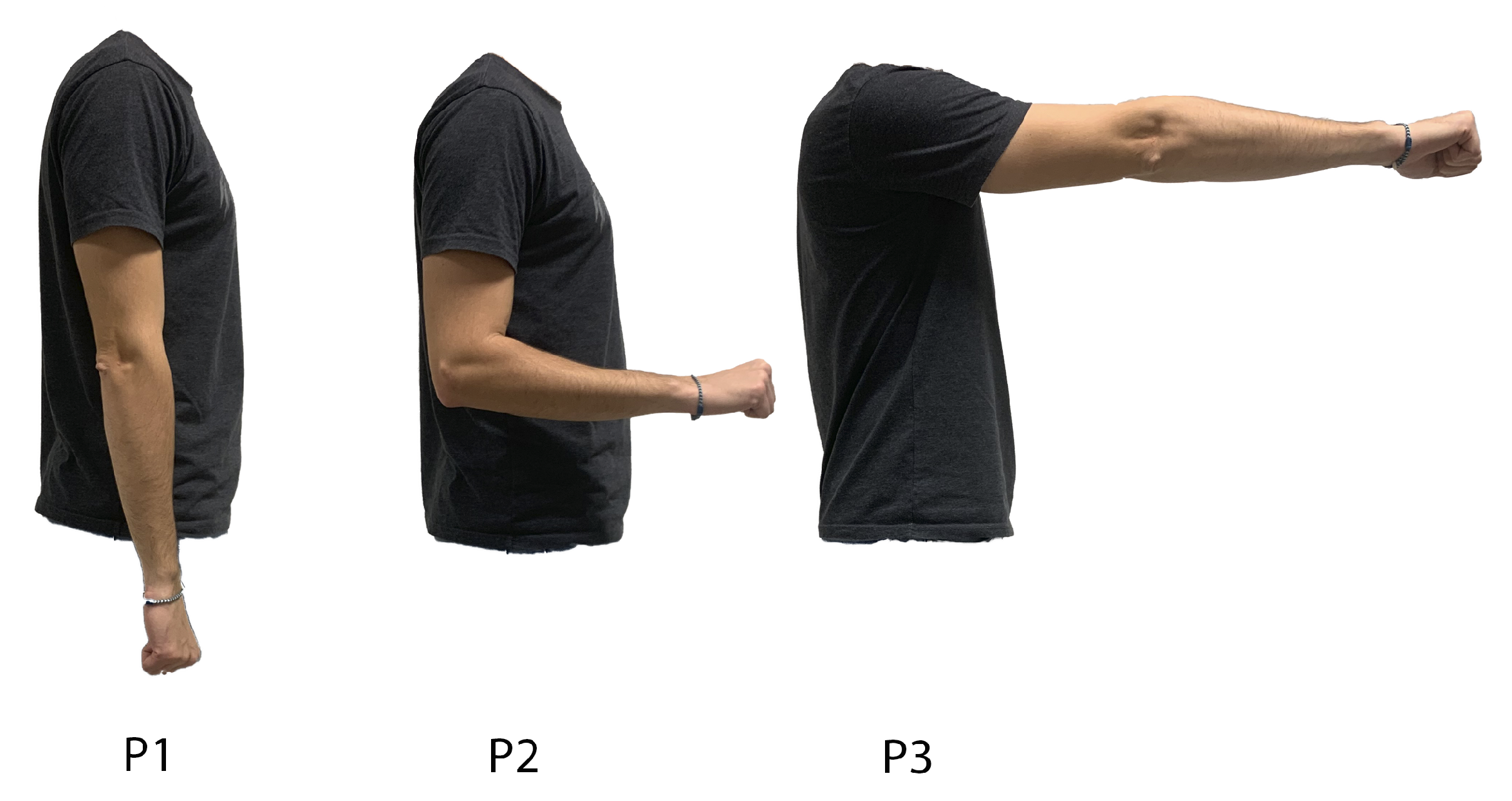
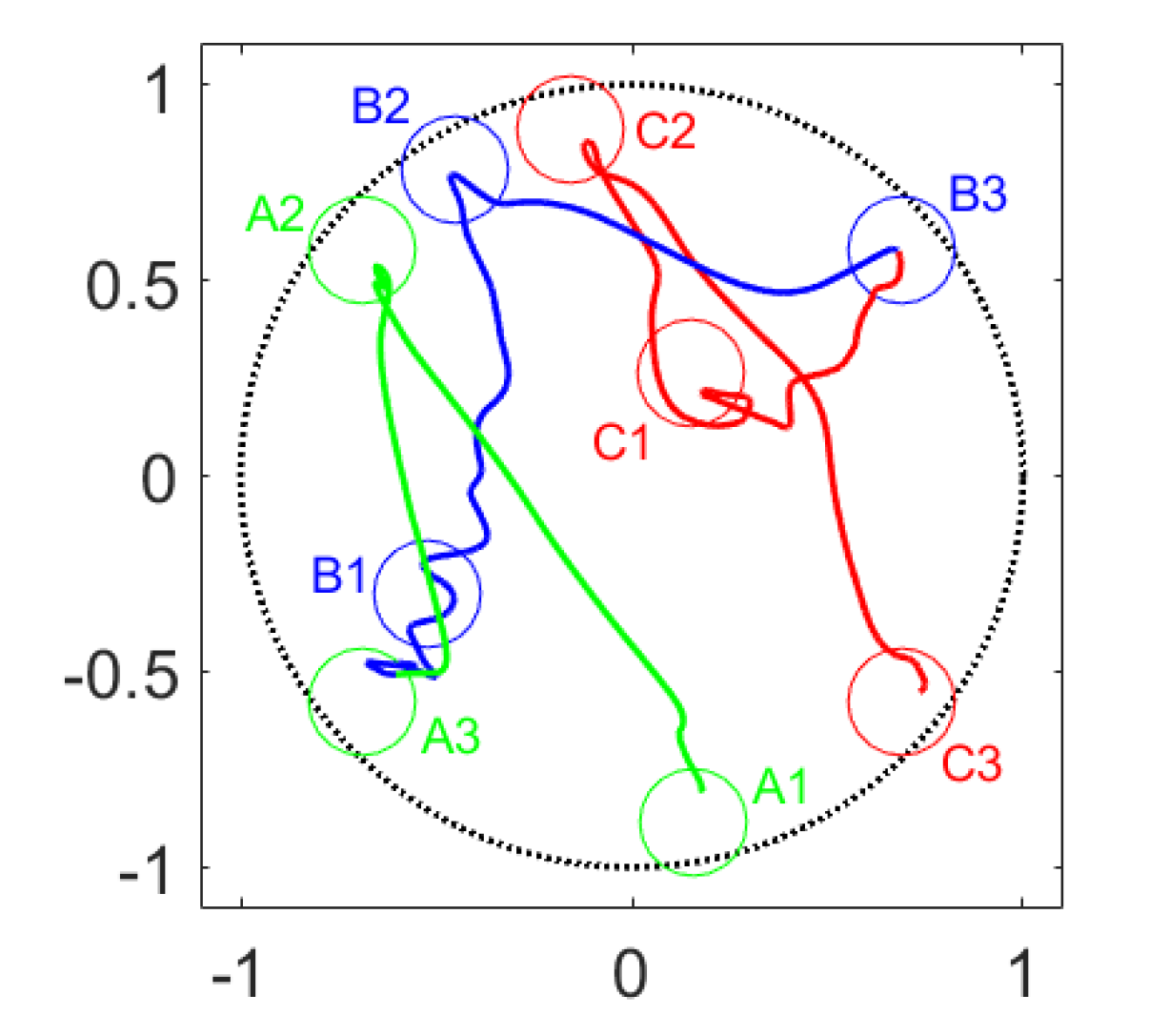
2.4.2. Arm Position Protocol
2.5. Performance Metrics
3. Results
3.1. Donning and Doffing Experiment
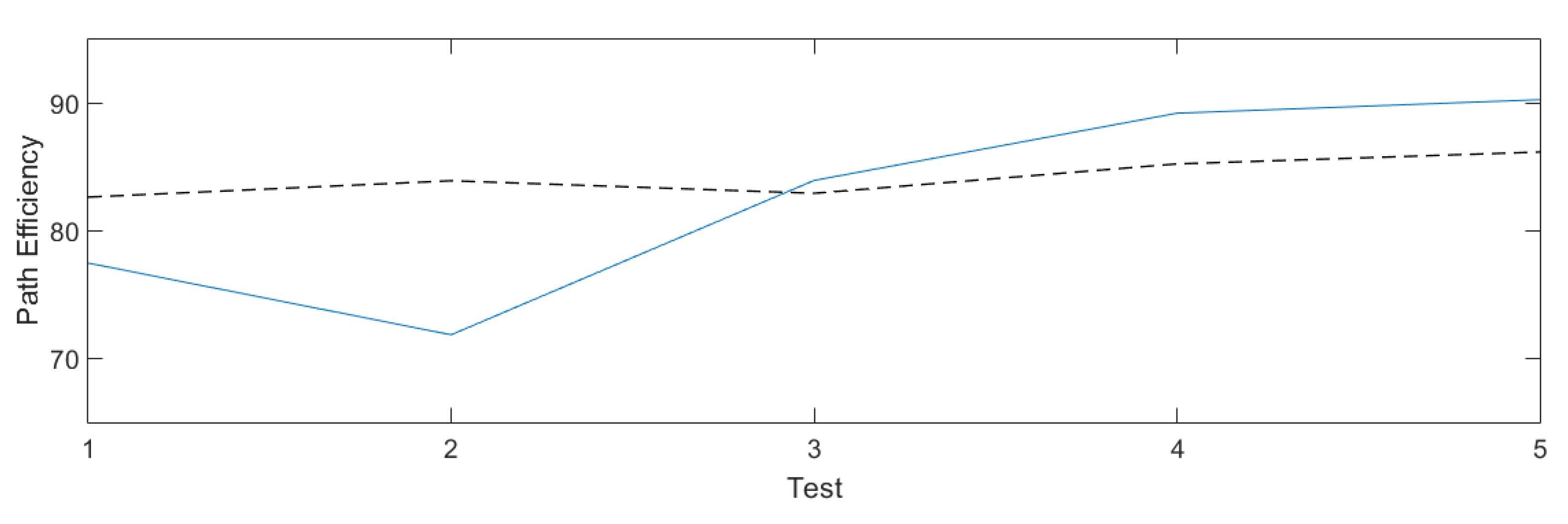
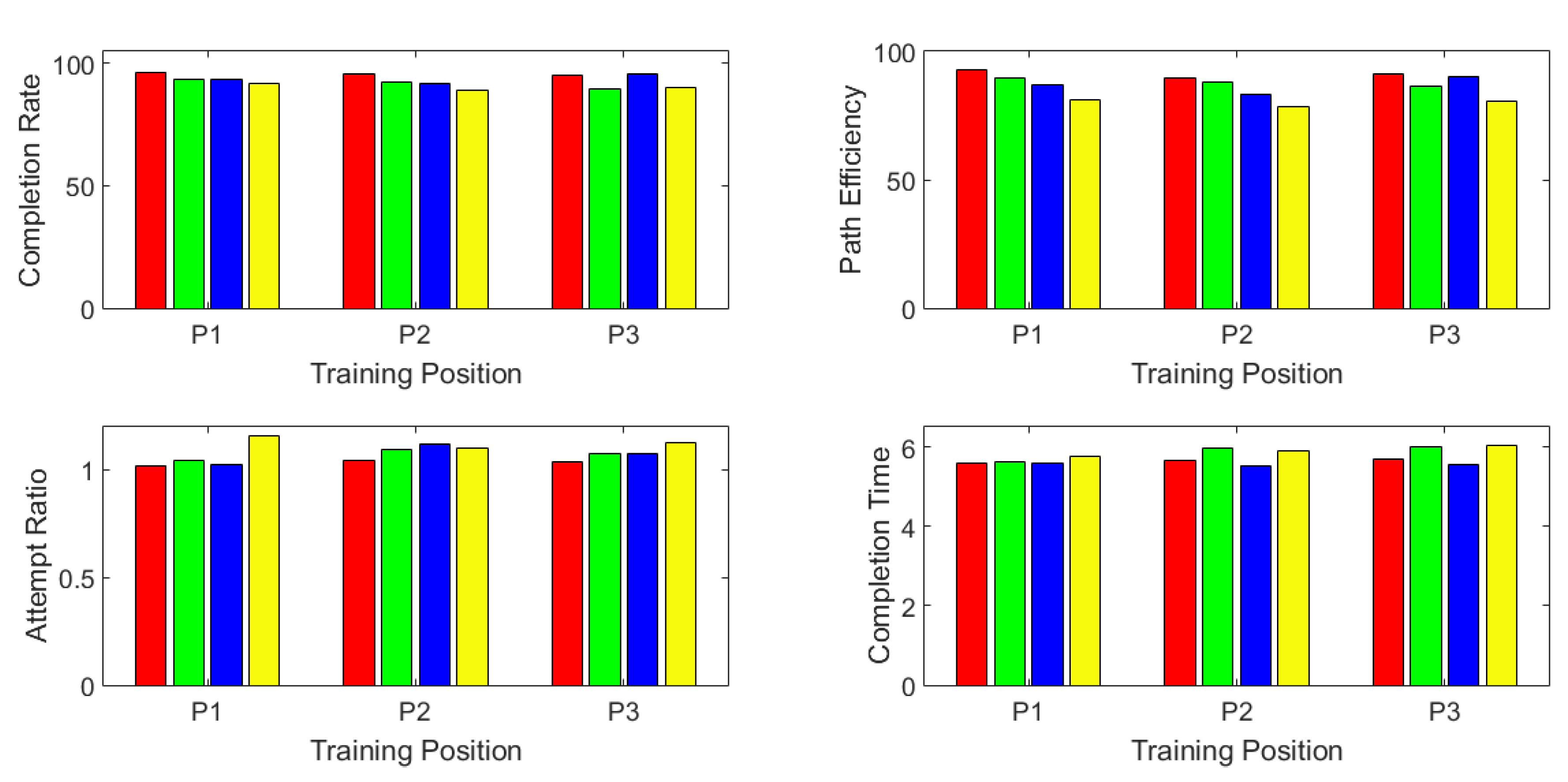
3.2. Arm Position Experiment
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Esquenazi, A. Amputation rehabilitation and prosthetic restoration. From surgery to community reintegration. Disabil. Rehabil. 2004, 26, 831–836. [Google Scholar] [CrossRef]
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Igual, C.; Pardo, L.A.; Hahne, J.M.; Igual, J.M. Myoelectric Control for Upper Limb Prostheses. Electronics 2019, 8, 1244. [Google Scholar] [CrossRef]
- Biddiss, E.; Chau, T. Upper-limb prosthetics: Critical factors in device abandonment. Am. J. Phys. Med. Rehabil. 2007, 86, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.A.; Chau, T.T. Upper limb prosthesis use and abandonment: A survey of the last 25 years. Prosthetics Orthot. Int. 2007, 31, 236–257. [Google Scholar] [CrossRef]
- Davidson, J. A survey of the satisfaction of upper limb amputees with their prostheses, their lifestyles, and their abilities. J. Hand Ther. 2002, 15, 62–70. [Google Scholar] [CrossRef]
- Datta, D.; Selvarajah, K.; Davey, N. Functional outcome of patients with proximal upper limb deficiency–acquired and congenital. Clin. Rehabil. 2004, 18, 172–177. [Google Scholar] [CrossRef]
- Vujaklija, I.; Farina, D.; Aszmann, O.C. New developments in prosthetic arm systems. Orthop. Res. Rev. 2016, 8, 31–39. [Google Scholar] [CrossRef]
- Scheme, E.J.; Englehart, K.B.; Hudgins, B.S. Selective classification for improved robustness of myoelectric control under nonideal conditions. IEEE Trans. Biomed. Eng. 2011, 58, 1698–1705. [Google Scholar] [CrossRef]
- Englehart, K.; Hudgins, B. A robust, real-time control scheme for multifunction myoelectric control. IEEE Trans. Biomed. Eng. 2003, 50, 848–854. [Google Scholar] [CrossRef]
- Parker, P.; Englehart, K.; Hudgins, B. Myoelectric signal processing for control of powered limb prostheses. J. Electromyogr. Kinesiol. 2006, 16, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Fougner, A.; Stavdahl, Ø.; Kyberd, P.J.; Losier, Y.G.; Parker, P.A. Control of upper limb prostheses: Terminology and proportional myoelectric control—A review. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 20, 663–677. [Google Scholar] [CrossRef] [PubMed]
- Resnik, L.; Huang, H.H.; Winslow, A.; Crouch, D.L.; Zhang, F.; Wolk, N. Evaluation of EMG pattern recognition for upper limb prosthesis control: A case study in comparison with direct myoelectric control. J. Neuroeng. Rehabil. 2018, 15, 23. [Google Scholar] [CrossRef] [PubMed]
- Sartori, M.; Durandau, G.; Došen, S.; Farina, D. Robust simultaneous myoelectric control of multiple degrees of freedom in wrist-hand prostheses by real-time neuromusculoskeletal modeling. J. Neural Eng. 2018, 15, 066026. [Google Scholar] [CrossRef] [PubMed]
- Velliste, M.; Perel, S.; Spalding, M.C.; Whitford, A.S.; Schwartz, A.B. Cortical control of a prosthetic arm for self-feeding. Nature 2008, 453, 1098. [Google Scholar] [CrossRef] [PubMed]
- Amsuess, S.; Vujaklija, I.; Goebel, P.; Roche, A.D.; Graimann, B.; Aszmann, O.C.; Farina, D. Context-Dependent Upper Limb Prosthesis Control for Natural and Robust Use. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 744–753. [Google Scholar] [CrossRef]
- Kuiken, T.A.; Miller, L.A.; Turner, K.; Hargrove, L.J. A comparison of pattern recognition control and direct control of a multiple degree-of-freedom transradial prosthesis. IEEE J. Transl. Eng. Health Med. 2016, 4, 1–8. [Google Scholar] [CrossRef]
- Phinyomark, A.N.; Khushaba, R.; Scheme, E. Feature Extraction and Selection for Myoelectric Control Based on Wearable EMG Sensors. Sensors 2018, 18, 1615. [Google Scholar] [CrossRef]
- Oskoei, M.A.; Hu, H. Myoelectric control systems—A survey. Biomed. Signal Process. Control 2007, 2, 275–294. [Google Scholar] [CrossRef]
- Spanias, J.A.; Perreault, E.J.; Hargrove, L.J. Detection of and compensation for EMG disturbances for powered lower limb prosthesis control. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 226–234. [Google Scholar] [CrossRef]
- Rahimi, A.; Benatti, S.; Kanerva, P.; Benini, L.; Rabaey, J.M. Hyperdimensional biosignal processing: A case study for EMG-based hand gesture recognition. In Proceedings of the 2016 IEEE International Conference on Rebooting Computing (ICRC), Washington, DC, USA, 7–9 November 2016; pp. 1–8. [Google Scholar]
- Castellini, C.; van der Smagt, P. Surface EMG in advanced hand prosthetics. Biol. Cybern. 2009, 100, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Ameri, A.; Akhaee, M.A.; Scheme, E.; Englehart, K. Regression convolutional neural network for improved simultaneous EMG control. J. Neural Eng. 2019, 16, 036015. [Google Scholar] [CrossRef] [PubMed]
- Hahne, J.; Biessmann, F.; Jiang, N.; Rehbaum, H.; Farina, D.; Meinecke, F.; Muller, K.R.; Parra, L. Linear and nonlinear regression techniques for simultaneous and proportional myoelectric control. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Jiang, N.; Dosen, S.; Muller, K.; Farina, D. Myoelectric Control of Artificial Limbs—Is There a Need to Change Focus? IEEE Signal Process. Mag. 2012, 29. Available online: https://ieeexplore.ieee.org/document/6279589 (accessed on 20 February 2020).
- Ameri, A.; Scheme, E.; Kamavuako, E.; Englehart, K.; Parker, P. Real-Time, Simultaneous Myoelectric Control Using Force and Position-Based Training Paradigms. IEEE Trans. Biomed. Eng. 2014, 61, 279–287. [Google Scholar] [CrossRef]
- Hochberg, L.R.; Serruya, M.D.; Friehs, G.M.; Mukand, J.A.; Saleh, M.; Caplan, A.H.; Branner, A.; Chen, D.; Penn, R.D.; Donoghue, J.P. Neuronal ensemble control of prosthetic devices by a human with tetraplegia. Nature 2006, 442, 164. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Zhou, D.; Li, K.; Liu, H. Interface Prostheses With Classifier-Feedback-Based User Training. IEEE Trans. Biomed. Eng. 2017, 64, 2575–2583. [Google Scholar] [CrossRef]
- Thomas, N.; Ung, G.; McGarvey, C.; Brown, J.D. Comparison of vibrotactile and joint-torque feedback in a myoelectric upper-limb prosthesis. J. Neuroeng. Rehabil. 2019, 16, 70. [Google Scholar] [CrossRef]
- Guémann, M.; Bouvier, S.; Halgand, C.; Borrini, L.; Paclet, F.; Lapeyre, E.; Ricard, D.; Cattaert, D.; de Rugy, A. Sensory and motor parameter estimation for elbow myoelectric control with vibrotactile feedback. Ann. Phys. Rehabil. Med. 2018, 61, e467. [Google Scholar] [CrossRef]
- Markovic, M.; Schweisfurth, M.A.; Engels, L.F.; Farina, D.; Dosen, S. Myocontrol is closed-loop control: Incidental feedback is sufficient for scaling the prosthesis force in routine grasping. J. Neuroeng. Rehabil. 2018, 15, 81. [Google Scholar] [CrossRef]
- Pasquina, P.F.; Perry, B.N.; Miller, M.E.; Ling, G.S.; Tsao, J.W. Recent advances in bioelectric prostheses. Neurol. Clin. Pract. 2015, 5, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Jiang, N.; Farina, D. Myoelectric control of upper limb prosthesis: Current status, challenges and recent advances. Front. Neuroeng. 2014, 4. [Google Scholar] [CrossRef]
- Lendaro, E.; Mastinu, E.; Håkansson, B.; Ortiz-Catalan, M. Real-time Classification of Non-Weight Bearing Lower-Limb Movements Using EMG to Facilitate Phantom Motor Execution: Engineering and Case Study Application on Phantom Limb Pain. Front. Neurol. 2017, 8, 470. [Google Scholar] [CrossRef] [PubMed]
- Mastinu, E.; Ortiz-Catalan, M.; Håkansson, B. Analog front-ends comparison in the way of a portable, low-power and low-cost EMG controller based on pattern recognition. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 2111–2114. [Google Scholar] [CrossRef]
- Beck, T.W.; Housh, T.J.; Cramer, J.T.; Malek, M.H.; Mielke, M.; Hendrix, R.; Weir, J.P. Electrode shift and normalization reduce the innervation zone’s influence on EMG. Med. Sci. Sport. Exerc. 2008, 40, 1314–1322. [Google Scholar] [CrossRef] [PubMed]
- Pasquina, P.F.; Evangelista, M.; Carvalho, A.; Lockhart, J.; Griffin, S.; Nanos, G.; McKay, P.; Hansen, M.; Ipsen, D.; Vandersea, J.; et al. First-in-man demonstration of a fully implanted myoelectric sensors system to control an advanced electromechanical prosthetic hand. J. Neurosci. Methods 2015, 244, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Fougner, A.; Scheme, E.; Chan, A.D.C.; Englehart, K.; Stavdahl, O. Resolving the Limb Position Effect in Myoelectric Pattern Recognition. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.J.; Hahne, J.; Mueller, K.R. Real-time robustness evaluation of regression based myoelectric control against arm position change and donning/doffing. PLoS ONE 2017, 12, e0186318. [Google Scholar] [CrossRef]
- Young, A.J.; Hargrove, L.J.; Kuiken, T.A. The effects of electrode size and orientation on the sensitivity of myoelectric pattern recognition systems to electrode shift. IEEE Trans. Biomed. Eng. 2011, 58, 2537–2544. [Google Scholar] [CrossRef]
- Prahm, C.; Schulz, A.; Paaßen, B.; Schoisswohl, J.; Kaniusas, E.; Dorffner, G.; Hammer, B.; Aszmann, O. Counteracting Electrode Shifts in Upper-Limb Prosthesis Control via Transfer Learning. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 956–962. [Google Scholar] [CrossRef]
- Cipriani, C.; Sassu, R.; Controzzi, M.; Carrozza, M.C. Influence of the weight actions of the hand prosthesis on the performance of pattern recognition based myoelectric control: Preliminary study. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 1620–1623. [Google Scholar] [CrossRef]
- Amsuess, S.; Paredes, L.P.; Rudigkeit, N.; Graimann, B.; Herrmann, M.J.; Farina, D. Long term stability of surface EMG pattern classification for prosthetic control. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 3622–3625. [Google Scholar] [CrossRef]
- Scheme, E.; Englehart, K. Electromyogram pattern recognition for control of powered upper-limb prostheses: State of the art and challenges for clinical use. J. Rehabil. Res. Dev. 2011, 48, 643–659. [Google Scholar] [CrossRef]
- Scheme, E.; Fougner, A.; Stavdahl, O.; Chan, A.D.C.; Englehart, K. Examining the adverse effects of limb position on pattern recognition based myoelectric control. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 6337–6340. [Google Scholar] [CrossRef]
- Dohnálek, P.; Gajdoš, P.; Peterek, T. Human activity recognition on raw sensor data via sparse approximation. In Proceedings of the 2013 36th International Conference on Telecommunications and Signal Processing (TSP), Rome, Italy, 2–4 July 2013; pp. 700–703. [Google Scholar] [CrossRef]
- Marasco, P.D.; Hebert, J.S.; Sensinger, J.W.; Shell, C.E.; Schofield, J.S.; Thumser, Z.C.; Nataraj, R.; Beckler, D.T.; Dawson, M.R.; Blustein, D.H.; et al. Illusory movement perception improves motor control for prosthetic hands. Sci. Transl. Med. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Mastinu, E.; Doguet, P.; Botquin, Y.; Håkansson, B.; Ortiz-Catalan, M. Embedded System for Prosthetic Control Using Implanted Neuromuscular Interfaces Accessed Via an Osseointegrated Implant. IEEE Trans. Biomed. Circuits Syst. 2017, 11, 867–877. [Google Scholar] [CrossRef] [PubMed]
- Igual, C.; Igual, J.; Hahne, J.M.; Parra, L.C. Adaptive Auto-Regressive Proportional Myoelectric Control. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Englehart, K.B.; Hudgins, B.; Chan, A.D. A Gaussian mixture model based classification scheme for myoelectric control of powered upper limb prostheses. IEEE Trans. Biomed. Eng. 2005, 52, 1801–1811. [Google Scholar] [CrossRef]
- Hahne, J.M.; Dähne, S.; Hwang, H.J.; Müller, K.R.; Parra, L.C. Concurrent adaptation of human and machine improves simultaneous and proportional myoelectric control. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 618–627. [Google Scholar] [CrossRef]


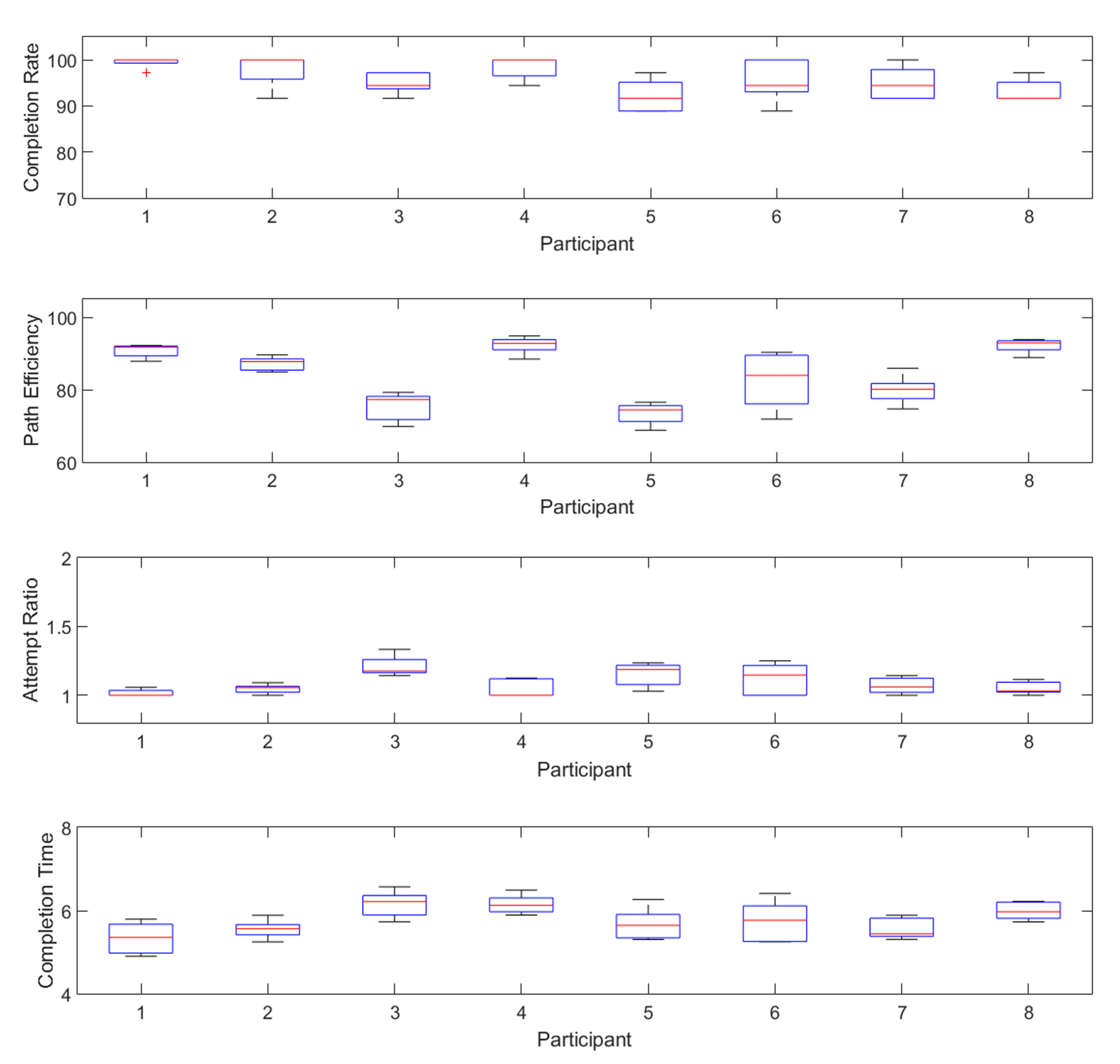
| Participant | Completion Rate (%) | Path Efficiency (%) | Completion Time (s) | Attempt Ratio |
|---|---|---|---|---|
| 1 | 99.44 ± 1.24 | 90.75 ± 1.86 | 5.338 ± 0.387 | 1.017 ± 0.025 |
| 2 | 97.78 ± 3.62 | 87.20 ± 1.95 | 5.554 ± 0.230 | 1.046 ± 0.034 |
| 3 | 95.00 ± 2.32 | 75.32 ± 4.00 | 6.153 ± 0.321 | 1.212 ± 0.076 |
| 4 | 98.33 ± 2.49 | 92.28 ± 2.40 | 6.151 ± 0.230 | 1.049 ± 0.066 |
| 5 | 92.22 ± 3.62 | 73.42 ± 3.07 | 5.673 ± 0.388 | 1.151 ± 0.087 |
| 6 | 95.55 ± 4.65 | 82.56 ± 7.85 | 5.740 ± 0.499 | 1.121 ± 0.116 |
| 7 | 95.00 ± 3.62 | 79.90 ± 4.03 | 5.568 ± 0.257 | 1.070 ± 0.060 |
| 8 | 93.33 ± 2.48 | 92.14 ± 1.98 | 5.994 ± 0.217 | 1.053 ± 0.047 |
| Avg | 95.83 ± 3.00 | 84.19 ± 3.39 | 5.771 ± 0.316 | 1.090 ± 0.064 |
| Training | Test P1 | Test P2 | Test P3 | Test P4 |
|---|---|---|---|---|
| P1 | 96.53 | 93.75 | 93.75 | 91.67 |
| P2 | 95.83 | 92.36 | 91.67 | 88.89 |
| P3 | 95.14 | 89.58 | 95.84 | 90.28 |
| Training | Test P1 | Test P2 | Test P3 | Test P4 |
|---|---|---|---|---|
| P1 | 92.91 | 89.85 | 86.87 | 81.32 |
| P2 | 89.78 | 88.06 | 83.50 | 78.22 |
| P3 | 91.30 | 86.34 | 90.31 | 80.84 |
| Training | Test P1 | Test P2 | Test P3 | Test P4 |
|---|---|---|---|---|
| P1 | 1.022 | 1.045 | 1.022 | 1.159 |
| P2 | 1.045 | 1.094 | 1.118 | 1.104 |
| P3 | 1.038 | 1.074 | 1.076 | 1.128 |
| Training | Test P1 | Test P2 | Test P3 | Test P4 |
|---|---|---|---|---|
| P1 | 5.573 | 5.632 | 5.590 | 5.776 |
| P2 | 5.643 | 5.950 | 5.536 | 5.908 |
| P3 | 5.690 | 6.001 | 5.549 | 6.037 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Igual, C.; Camacho, A.; Bernabeu, E.J.; Igual, J. Donning/Doffing and Arm Positioning Influence in Upper Limb Adaptive Prostheses Control. Appl. Sci. 2020, 10, 2892. https://doi.org/10.3390/app10082892
Igual C, Camacho A, Bernabeu EJ, Igual J. Donning/Doffing and Arm Positioning Influence in Upper Limb Adaptive Prostheses Control. Applied Sciences. 2020; 10(8):2892. https://doi.org/10.3390/app10082892
Chicago/Turabian StyleIgual, Carles, Andrés Camacho, Enrique J. Bernabeu, and Jorge Igual. 2020. "Donning/Doffing and Arm Positioning Influence in Upper Limb Adaptive Prostheses Control" Applied Sciences 10, no. 8: 2892. https://doi.org/10.3390/app10082892
APA StyleIgual, C., Camacho, A., Bernabeu, E. J., & Igual, J. (2020). Donning/Doffing and Arm Positioning Influence in Upper Limb Adaptive Prostheses Control. Applied Sciences, 10(8), 2892. https://doi.org/10.3390/app10082892






