Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach
Abstract
Featured Application
Abstract
1. Introduction
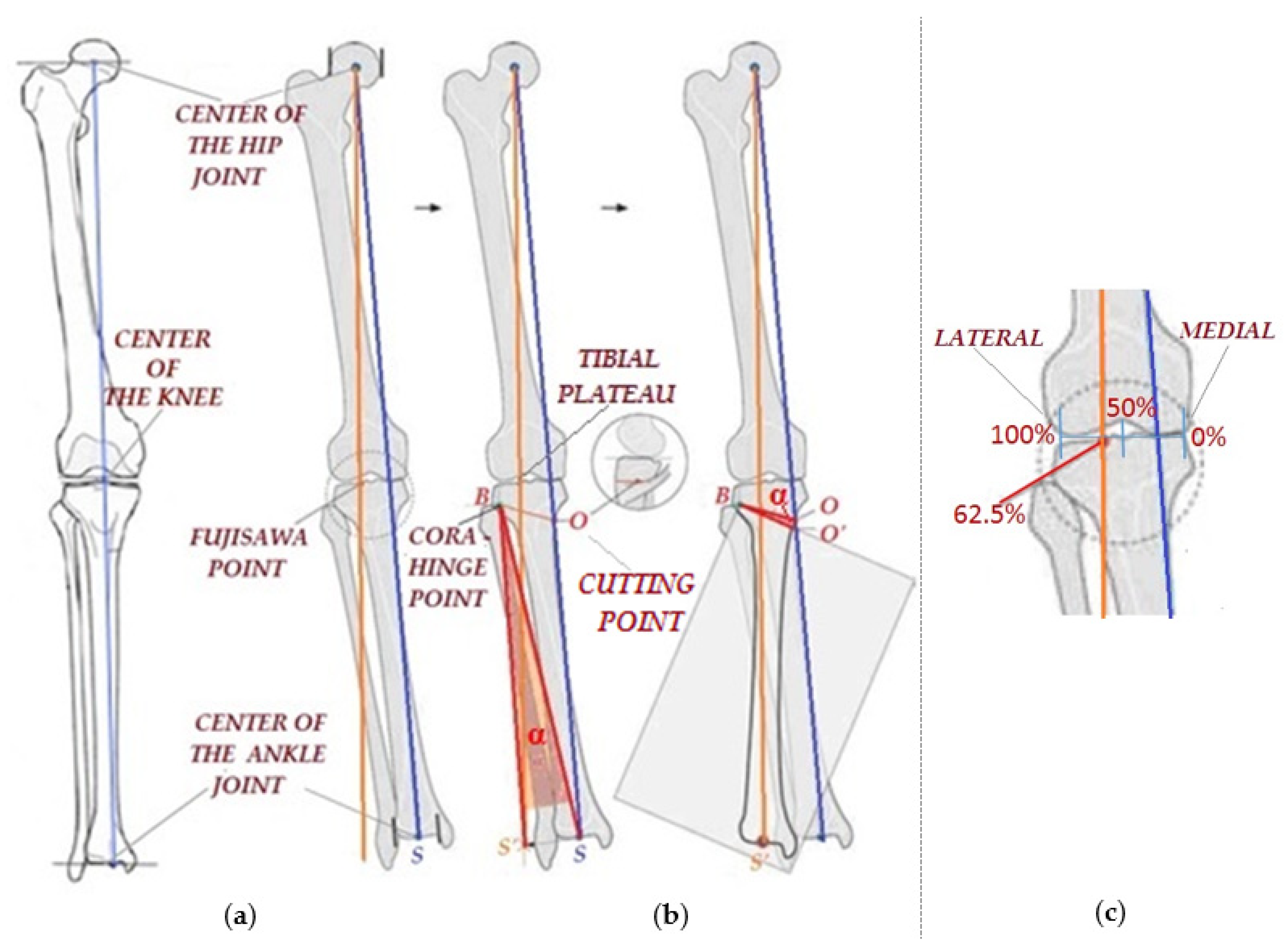
- Draw a line (orange) that passes through the center of the femoral head and through a point known in the scientific literature as the “FUJISAWA point” (Figure 1b) [19,21,22,23]. As can be observed from Figure 1b,c the Fujisawa point is a point positioned at 62.5% on the medial to lateral transverse knee line (hereinafter, “the FUJISAWA point”). The precise positioning of this point is still a controversial topic among specialists. It should normally be positioned halfway between the medial compartment and the lateral part (Figure 1c), but due to the predisposition of the affected patient to a continuous wear of the intra-articular cartilage, an overcorrection is preferred in the sense that the point is positioned at 62.5% of the distance. There is also the possibility that the surgeon chooses to set this point between 50 and 70%, depending on the degree of cartilage wear [21].
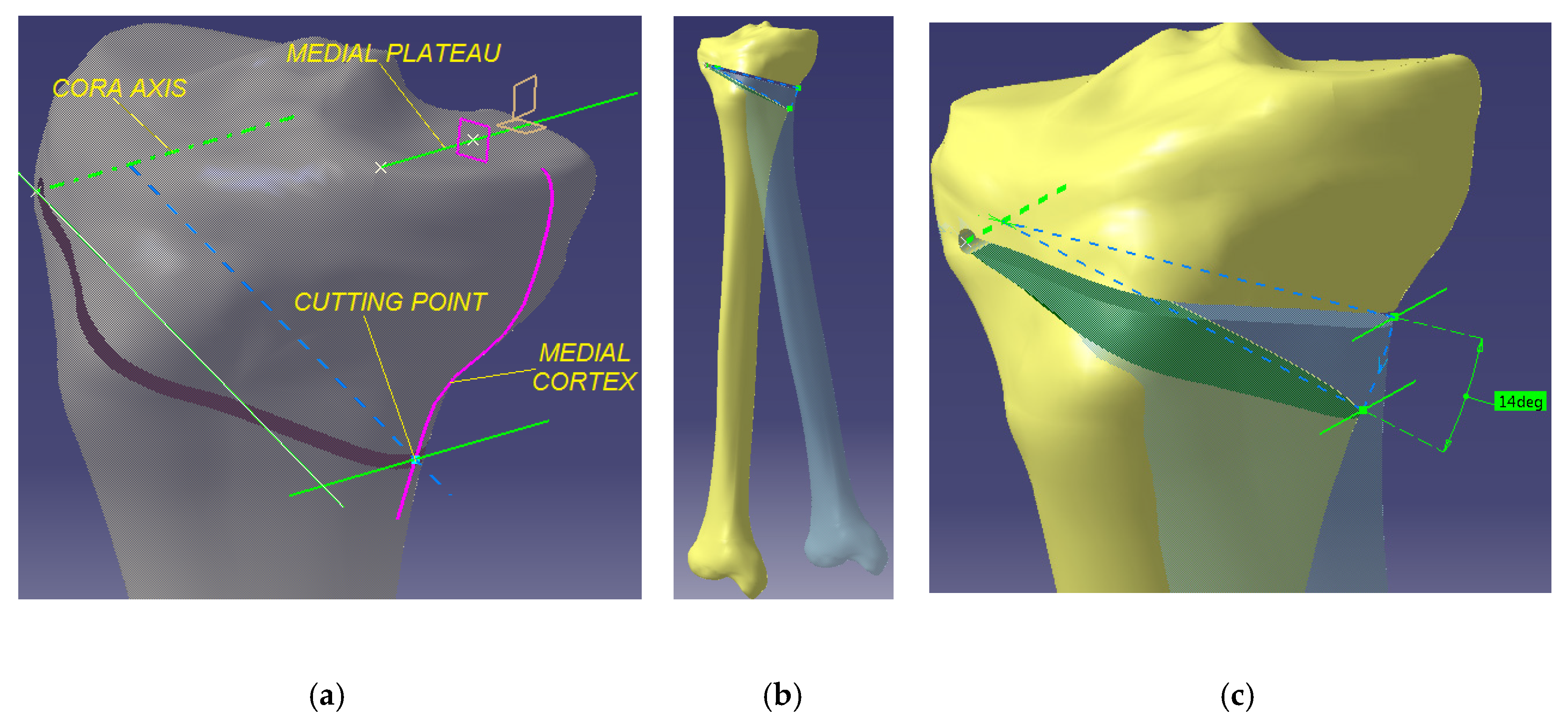
- Determine the position of the “hinge” point B relative to the tibial plateau and to the lateral cortex of the tibia (Figure 1b). This is the point around which the angulation is made, i.e., the center of the rotation of the angulation (hereinafer, “CORA”). This point is important because one needs a stable lateral hinge, and a fracture line though the articular surface should be avoided. There are no specifically defined values on this matter in the operative technique, but rather ranges of values are taken into consideration: 15–20 mm relative to the articular plane and 5–10 mm relative to the lateral cortex of the tibia [20,24,25,26].
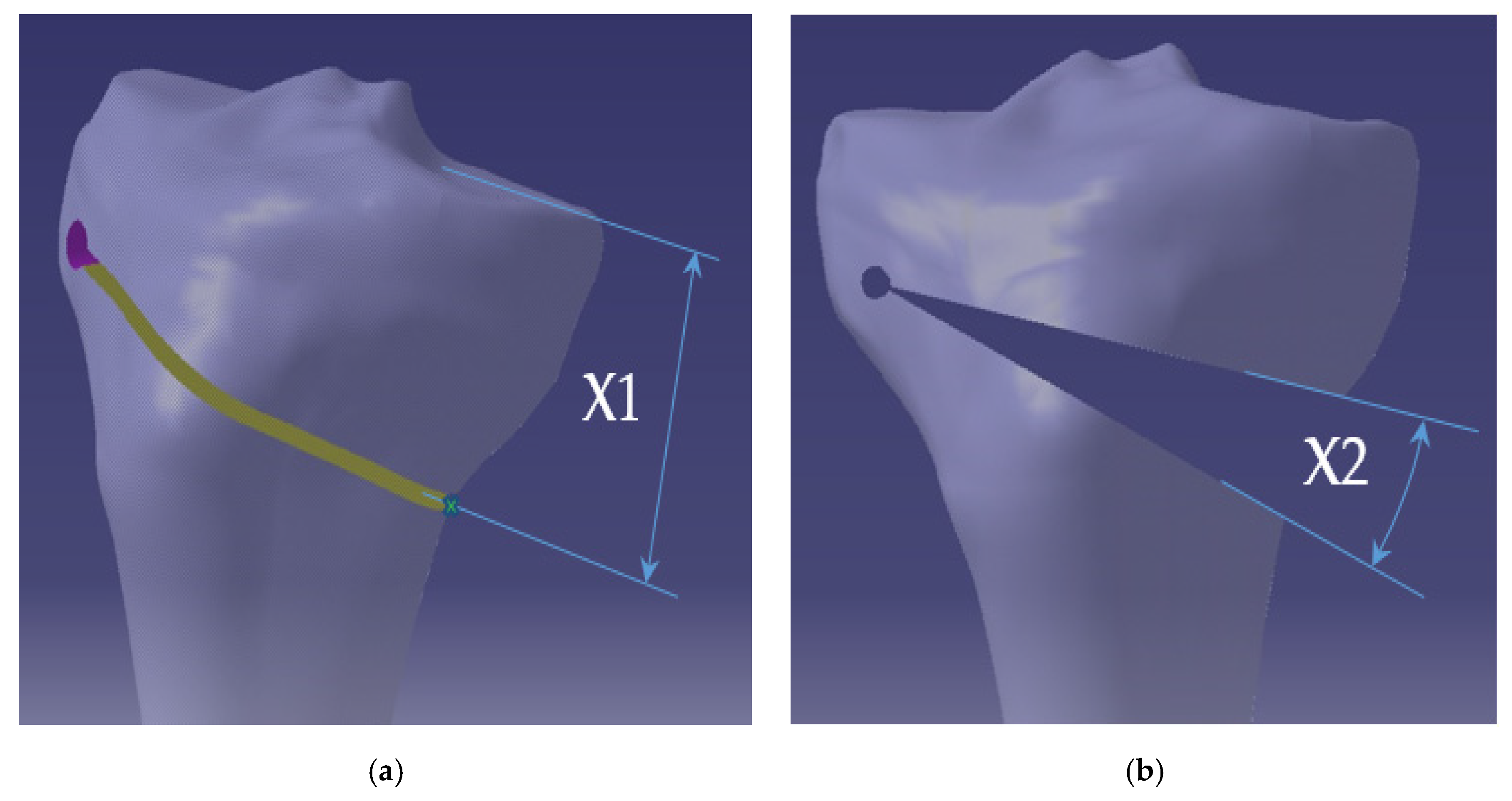
- Afterwards, the point of initiation of the cut for performing the osteotomy, situated on the medial cortex, is established (depicted as “point O” in Figure 1b, hereinafter “cutting point”). There are no studies suggesting the accurate positioning of the cutting point. However, given the limitations generated by the surrounding anatomic structures, the cutting point should be placed at a minimum of 30 mm and at a maximum of 50–60 mm from the articular line [20,24,25,26,27,28]. The osteotomy line is depicted as BO line in Figure 1b.
- Further on, the opening correction angle α is determined (hereinafter, “correction angle”) (Figure 1b). For this, a line is drawn from point B to point S, the center of the ankle joint, and then a circular arc is drawn with the center in point B of radius BS from point S to the intersection with the previously drawn orange line, resulting in point S’. Angle α, formed between line BS and line BS’, is the correction angle. The line joining the center of the femoral head and point S’ is the new corrected mechanical axis. To actually obtain the correction, a wedge osteotomy (depicted as “OBO’” in Figure 1b) is performed, having at its tip the angle α, which displaces the mechanical axis to the desired position. The 3D rotation of the proximal fragment of the tibia around the hinge is presented in Section 2.
- The correction angle.
- The position of the cutting point relative to the corresponding tibial plateau.
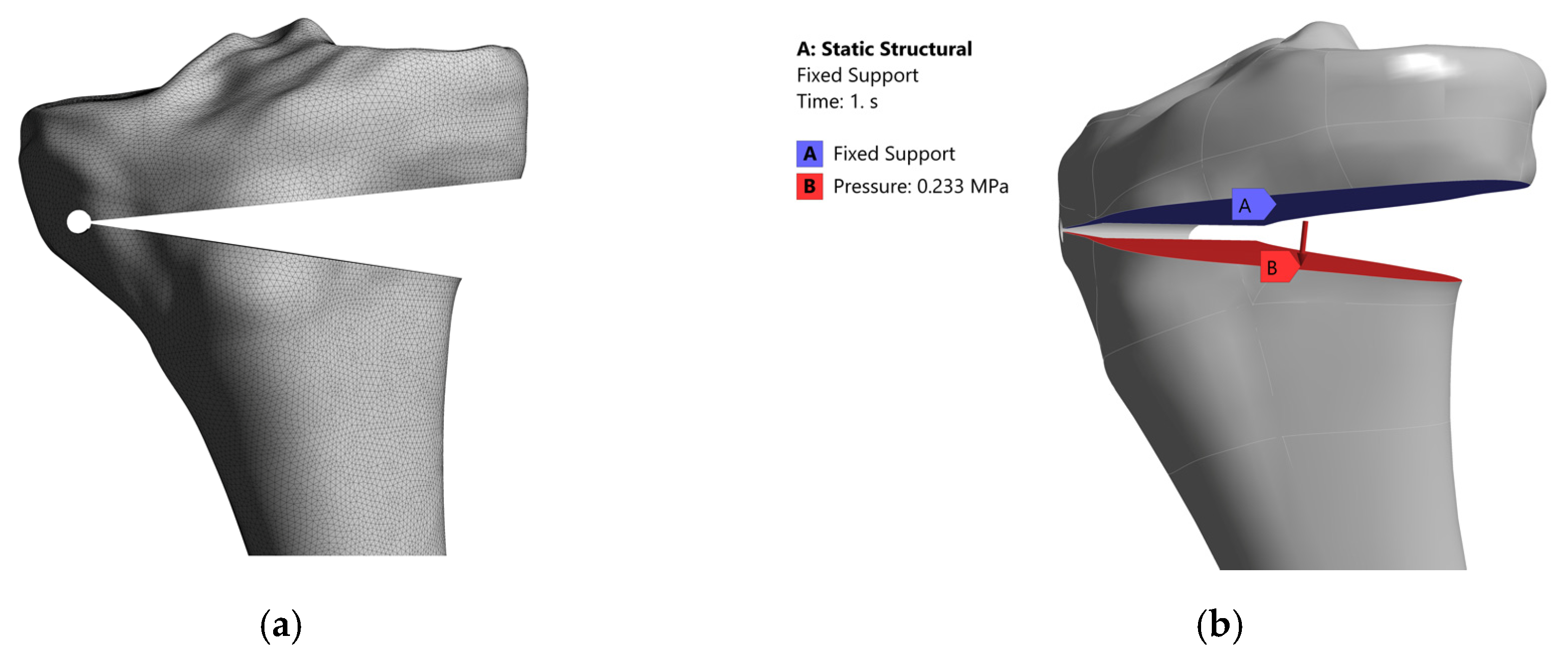
- To conduct a numerical research using the finite element method (hereinafter, “FEM”) to study the intraoperative behavior of the CORA area for different positions of the cutting point and for different correction angles. The FEM analysis may predict the mechanical stresses developed at the lateral hinge and the risk of fracture.
- To conduct a similar experiment on mechanical loading behavior.
2. Materials and Methods
2.1. The Numerical Simulation of the Uniplane Opening Tibial Osteotomy
- Young’s modulus (E)—12 to 19 GPa for the cortical bone, 0.5 to 1.5 GPa for the spongy bone, and 0.01 to 0.015 GPa for the articular cartilage.
- Poisson’s ratio—0.3 to 0.35 for the cortical bone, 0.16 to 0.2 for the spongy bone, and 0.2 to 0.25 for the cartilage.
- Transverse modulus of elasticity (G)—4 to 7 GPa for the cortical bone.
- Fracture resistance (Rm)—115 to 125 MPa for the cortical bone.
- Elongation (A)—1.4 to 2.8% for the cortical bone.
- Porosity—5 to 10% for the cortical bone, 50 to 90% for the trabecular bone.
- Density—1.6 to 1.9 g/cm3 for the cortical bone, 0.2 to 1 g/cm3 for the trabecular bone.
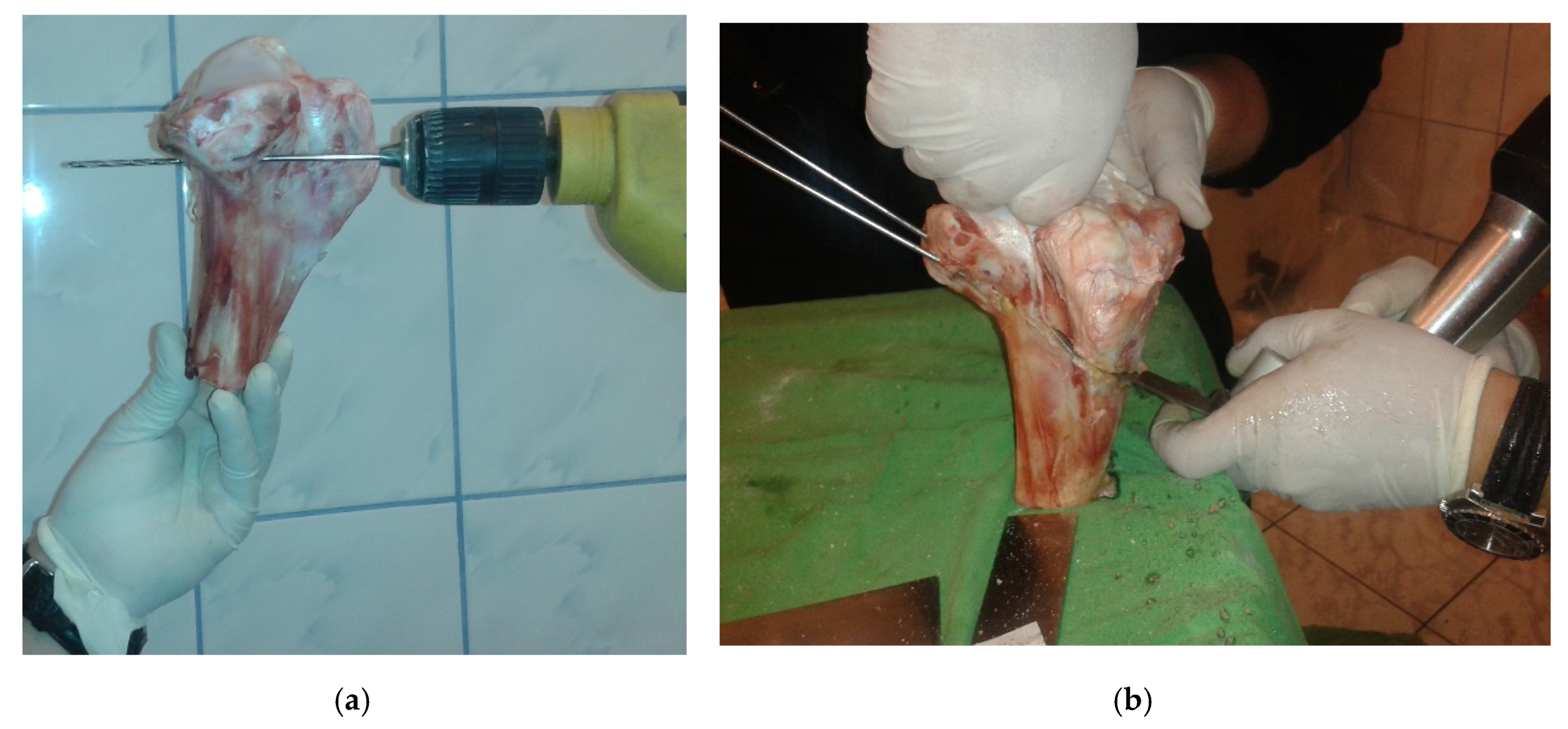
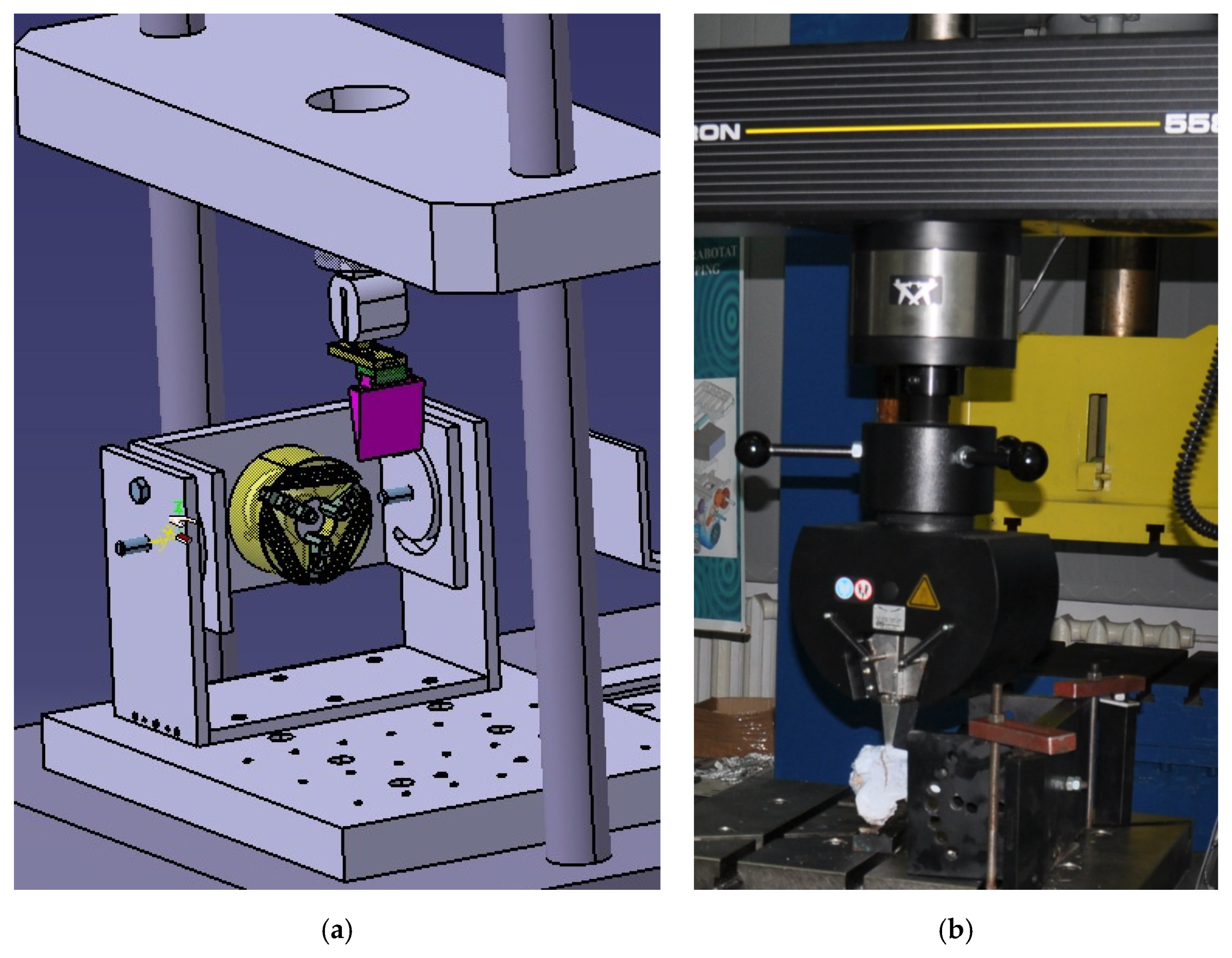
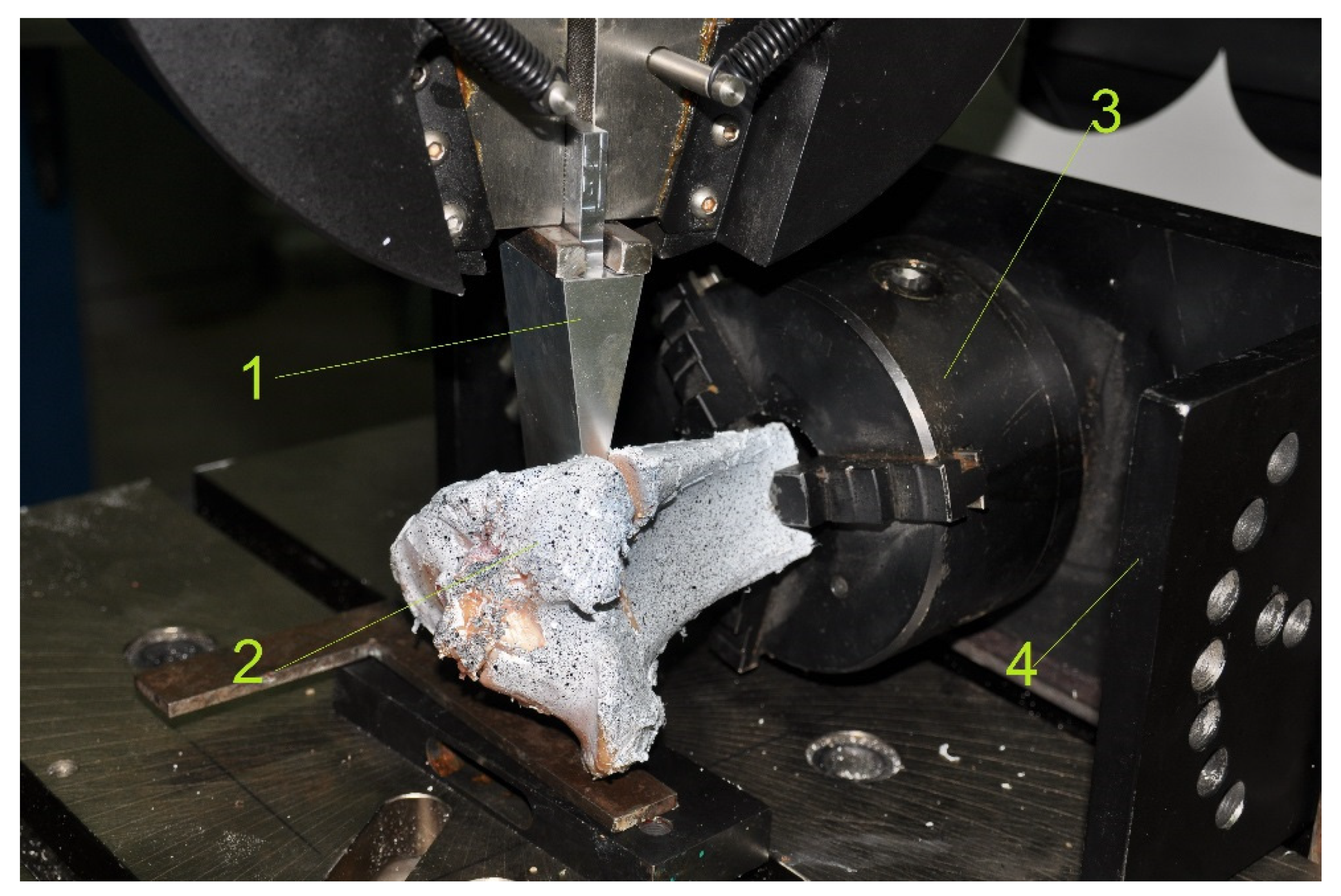
2.2. Experimental Research on the Study of the Intraoperative Behavior of the Bone Structure in the Case of the Opening Tibial Osteotomies
3. Results
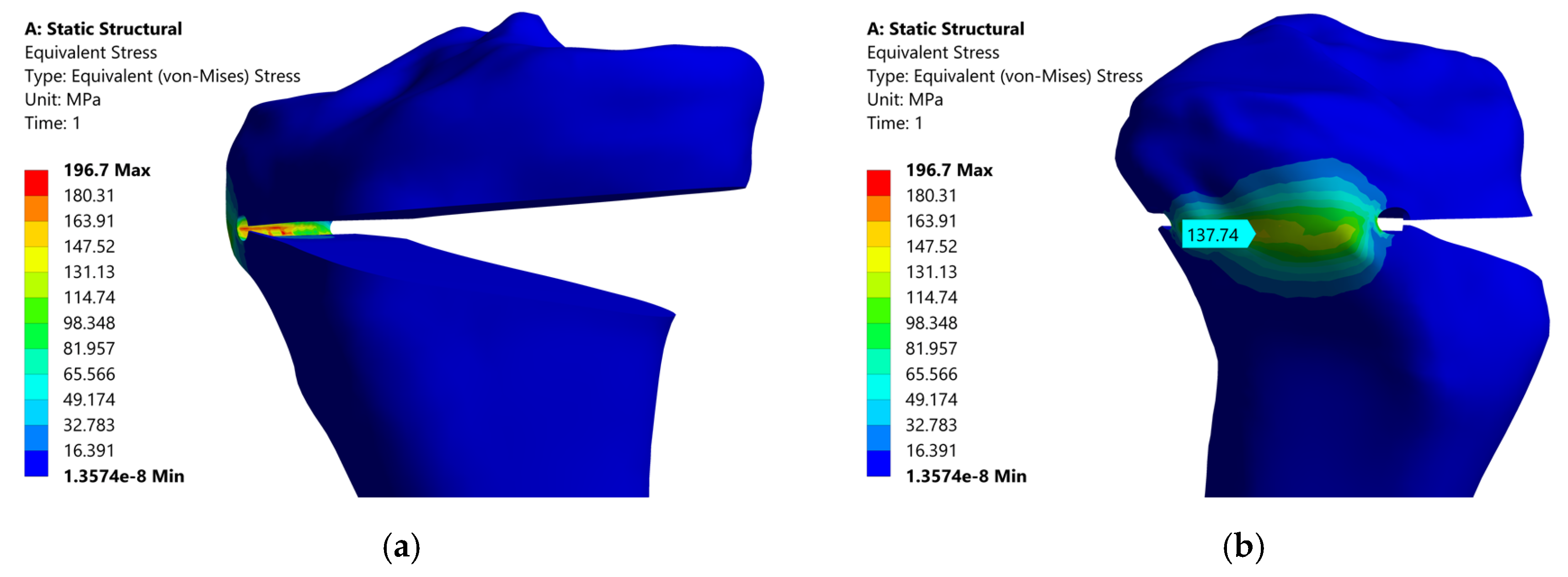
3.1. The Results of the Numerical Simulation of the Uniplane Opening Tibial Osteotomy
3.2. Experimental Results Regarding the Study of the Intraoperative Behavior of the Bone Structure in the Case of Opening Tibial Osteotomies
4. Discussion
- -
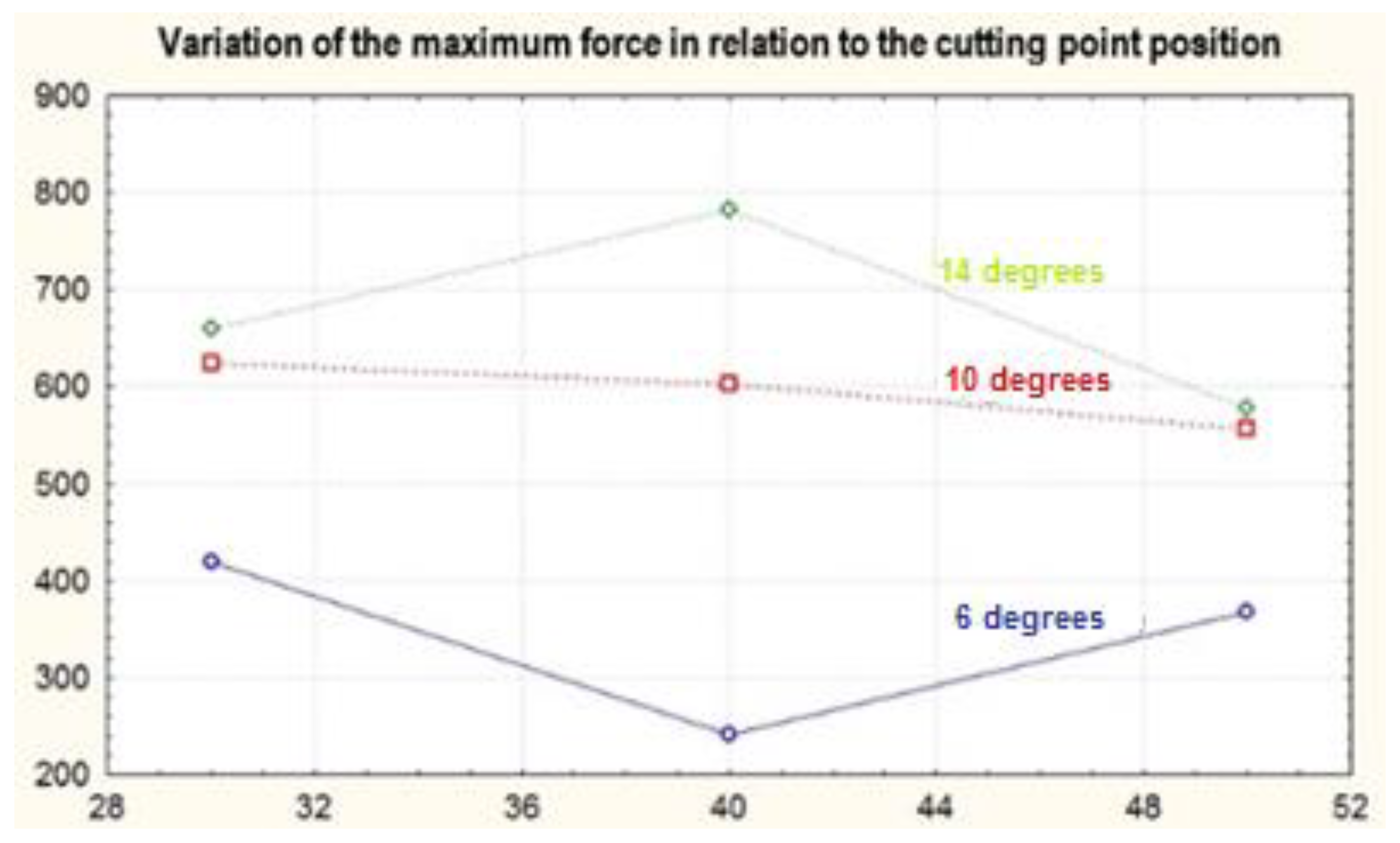
- For the 14 degree angle (for high correction values), it was clearly favorable to position the cutting point at 40 mm;
- -
- For the 10 degree angle (for medium correction values), it was favorable to position the cutting point at 30 mm;
- -
- Positioning the cutting point at 50 mm appearred as the least favorable solution for almost all of the used combinations of parameters.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fleaca, R.S. Transplantul Osteocondral Autolog înTratamentul Leziunilor Cartilajului Articular. Ph.D. Thesis, Lucian Blaga University of Sibiu, Sibiu, Romania, December 2009. [Google Scholar]
- Eckstein, F.; Adam, C.; Sittek, H.; Becker, C.; Milz, S.; Schulte, E.; Reiser, M.; Putz, R. Non-invasive determination of cartilage thickness throughout joint surfaces using magnetic resonance imaging. J. Biomech. 1997, 30, 285–289. [Google Scholar] [CrossRef]
- Eckstein, F.; Winzheimer, M.; Westhoff, J.; Schnier, M.; Haubner, M.; Englmeier, K.H.; Reiser, M.; Putz, R. Quantitative relationships of normal cartilage volumes of the human knee joint—Assessment by magnetic resonance imaging. Anat. Embryol. 1998, 197, 383–390. [Google Scholar] [CrossRef]
- Potter, H.G.; Foo, L.F. Magnetic Resonance Imaging of Articular Cartilage: Trauma, Degeneration, and Repair. Am. J. Sports Med. 2006, 34, 661–677. [Google Scholar] [CrossRef] [PubMed]
- Helminen, H.J.; Kiviranta, I.; Säämänen, A.M.; Jurvelin, J.; Arokoski, J.; Oettmeier, R.; Abendroth, K.; Roth, A.J.; Tammi, M. Effect of motion and load on articular cartilage in animal models. In Articular Cartilage and Osteoarthritis; Keuttner, K.E., Schleyerbach, R., Peyron, J.G., Eds.; Raven Press: New York, NY, USA, 1992; pp. 501–510. [Google Scholar]
- Abramson, S.B. The role of COX-2 produced by cartilage in arthritis. Osteoarthr. Cartil. 1999, 7, 380–381. [Google Scholar] [CrossRef]
- Antonescu, D.M.; Pop, D.M. Elemente de Patologie Osteoarticulara; Teora Publisher: Bucharest, Romania, 2000; pp. 7–9. [Google Scholar]
- Brockmeier, P. Effects of Articular Cartilage Defect Size and Shape on Subchondral Bone Contact: Implications for Surgical Cartilage Restoration. Ph.D. Thesis, The Ohio State University, Athens, OH, USA, June 2008. [Google Scholar]
- Derek, T.; Cooke, V.; Allan Scudamore, R.A.; Bryant, T. Mechanical Factors in the Pathogenesis of Osteoarthritis. In Trends in Research and Treatment of Joint Diseases; Springer Science and Business Media LLC: Tokyo, Japan, 1992; pp. 29–34. [Google Scholar]
- Guilak, F. Biomechanical factors in osteoarthritis. Best Pr. Res. Clin. Rheumatol. 2011, 25, 815–823. [Google Scholar] [CrossRef]
- Mansur, H.; Rocha, F.A.; Texeira de Dousa Filho, P.G.; De Castro Junior, I.M. Relationship between the knee and hindfoot axes in patients with severe knee osteoarthritis. Acta Ortop. Bras. 2020, 28, 229–232. [Google Scholar] [CrossRef]
- Amis, A.A. Biomechanics of high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 197–205. [Google Scholar] [CrossRef]
- Floerkemeier, S.; Staubli, A.E.; Schroeter, S.; Goldhahn, S.; Lobenhoffer, P. Outcome after high tibial open-wedge osteotomy: A retrospective evaluation of 533 patients. Knee Surg. Sports. Traumatol. Arthrosc. 2013, 21, 170–180. [Google Scholar] [CrossRef]
- Ryohei, T.; Hiroyuki, I.; Masato, A.; Haruhiko, B.; Izumi, S.; Ken, K. Medial opening wedge high tibial osteotomy with early full weight bearing. J. Arthrosc. Relat. Surg. 2009, 25, 46–53. [Google Scholar] [CrossRef]
- Spahn, G. Complications in high tibial (medial opening wedge) osteotomy. Arch. Orthop. Trauma Surg. 2003, 124, 649–653. [Google Scholar] [CrossRef]
- Sprenger, T.R.; Doerzbacher, J.F. Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J. Bone Jt. Surg. Am. 2003, 85, 469–474. [Google Scholar] [CrossRef]
- Amendola, A.; Bonasia, D.E. Results of high tibial osteotomy: Review of the literature. Int. Orthop. 2010, 34, 155–160. [Google Scholar] [CrossRef]
- Song, E.K.; Seon, J.K.; Park, S.J.; Jeong, M.S. The complications of high tibial osteotomy: Closing- versus opening-wedge methods. J. Bone Jt. Surg. Br. 2010, 92, 1245–1252. [Google Scholar] [CrossRef]
- Tomofix Medial High Tibial Plate for Medial Tibial Osteotomy. Available online: http://synthes.vo.llnwd.net/o16/LLNWMB8/INT%20Mobile/Synthes%20International/Product%20Support%20Material/legacy_Synthes_PDF/DSEM-TRM-0115-0288-1_LR.pdf (accessed on 15 August 2020).
- Elson, D.W.; Petheram, T.G.; Dawson, M.J. High reliability in digital planning of medial opening wedge high tibial osteotomy, using Miniaci’s method. Knee. Surg. Sports Traumatol. Arthrosc. 2015, 23, 2041–2048. [Google Scholar] [CrossRef]
- Modern High Tibial Osteotimy. Available online: http:/www.ilizarov.org/HTO1.pdf (accessed on 15 August 2020).
- Yin, Y.; Li, S.; Zhang, R.; Guo, J.; Hou, Z.; Zhang, Y. What is the relationship between the “Fujisawa point” andpostoperative knee valgus angle? A theoretical, computer-based study. Knee 2020, 27, 183–191. [Google Scholar] [CrossRef]
- Somtua, C.; Aroonjarattham, P.; Aroonjarattham, K. The correction of Thai varus knee by high tibial osteotomy with Fujisawa’s point using finite element analysis. J. Res. Appl. Mech. Eng. 2019, 7, 45–59. [Google Scholar]
- Yang, J.C.; Chen, C.F.; Luo, C.A.; Chang, M.C.; Lee, O.K.; Huang, Y.; Lin, S.C. Clinical Experience Using a 3D-Printed Patient-Specific Instrument for Medial Opening Wedge High Tibial Osteotomy. BioMed Res. Int. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Rudzki, J.R. Medial Opening Wedge High Tibial Osteotomy, Arthrex Knee Meeting, Los Angeles, CA, USA, 12 May 2012. Published on 23 January 2015. Available online: https://www.slideshare.net/washingtonortho/arthrex-hto-talk-51212 (accessed on 20 November 2020).
- Kader, D. High Tibial Osteotomy and UniKnee, Health & Medicine. 2015. Available online: https://www.slideshare.net/ProfDeiaryFKader/high-tibial-osteotomy-and-uniknee-for-post-grad-orth-frcs-course (accessed on 20 November 2020).
- Lee, Y.S.; Moon, G.H. Comparative analysis of osteotomy accuracy between the conventional and devised technique using a protective cutting system in medial open-wedge high tibial osteotomy. J. Orthop. Sci. 2015, 20, 129–136. [Google Scholar] [CrossRef]
- Kwun, J.D.; Kim, H.J.; Park, J.; Park, I.H.; Kyung, H.S. Open wedge high tibial osteotomy using three-dimensional printed models: Experimental analysis using porcine bone. Knee 2017, 24, 16–22. [Google Scholar] [CrossRef]
- Ogawa, H.; Matsumoto, K.; Akiyama, H. The prevention of a lateral hinge fracture as a complication of a medial opening wedge high tibial osteotomy-a case control study. Bone Jt. J. 2017, 99. [Google Scholar] [CrossRef]
- Ionescu, I.; Conway, T.; Schonning, A.; Almutairi, M.; Nicholson, D.W. Solid Modeling and Static Finite Element Analysis of the Human Tibia. In Proceedings of the Summer Bioengineering Conference 2003, Sonesta Beach Resort, Key Biscayne, FL, USA, 25–29 June 2003. [Google Scholar]
- Isaksson, H.E. Mechanical and Mechanobiological Influences on Bone Fracture Repair: Identifying Important Cellular Characteristics. Ph.D. Thesis, Eindhoven University of Technology, Eindhoven, The Netherlands, November 2007. [Google Scholar] [CrossRef]
- Cilingira, A.C.; Ucara, V.; Kazana, R. Three-Dimensional Anatomic Finite Element Modelling of Hemi-Arthroplasty of Human Hip Joint. Trends Biomater. Artif. Organs 2007, 21, 63–72. [Google Scholar]
- Petersen, W.; Zantop, T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin. Orthop. Relat. 2007, 454, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Müller-Karger, C.; Larrazabal, C.A. Finite Element Bone Model Incorporating Heterogeneity and Anisotropy from CT. In Proceedings of the ISB XXth Congress of the International Society of Biomechanis and ASB 29th Annual Meeting of the American Society of Biomechanics, Cleveland, OH, USA, 31 July–5 August 2004. [Google Scholar]
- Galik, K. The Effect of Design Variations on Stresses in Total Ankle Arthroplasty. Ph.D. Thesis, University of Pittsburgh, Pittsburgh, PA, USA, April 2002. [Google Scholar]
- Bayraktara, H.H.; Morgana, E.F.; Nieburb, G.L.; Morrisa, G.E.; Wonga, E.K.; Keaveny, T.M. Comparison of the elastic and yield properties of human femoral trabecular and cortical bone tissue. J. Biomech. 2004, 37, 27–35. [Google Scholar] [CrossRef]
- Kelly, D.J.; Predengast, P.J. Prediction of the Optimal Mechanical Properties for a Scaffold Used in Osteochondral Defect Repair. Tissue Eng. 2006, 12, 2509–2519. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.; Salo, A.D.; Barbu-Mcinnis, M.; Lerner, A.L. Finite Element Modeling of Knee Joint Contact Pressures and Comparison to Magnetic Resonance Imaging of the Loaded Knee. In Proceedings of the IMECE’032003 ASME International Mechanical Engineering Congress & Exposition, Washington, DC, USA, 16–21 November 2003. [Google Scholar]
- Boruah, S.; Subit, D.L.; Paskoff, G.R.; Shender, B.S.; Crandall, J.R.; Salzar, R.S. Influence of bone microstructure on the mechanical properties of skull cortical bone—A combined experimental and computational approach. J. Mech. Behav. Biomed. Mater. 2017, 65, 688–704. [Google Scholar] [CrossRef]
- Leordean, D.; Dudescu, C.; Marcu, T.; Berce, P.; Balc, N. Customized implants with specific properties, made by selective laser melting. Rapid Prototyp. J. 2015, 21, 98–104. [Google Scholar] [CrossRef]
- Cofaru, I.I. Research on the Biomechanics of Axial Deviations of the Human Lower Limb and the Development of Related Surgical Equipment. Ph.D. Thesis, Lucian Blaga University of Sibiu, Sibiu, Romania, November 2013. [Google Scholar]
- Morgan, F.; Bayraktar, H.H.; Keaveny, T.M. Trabecular bone modulus–density relationships depend on anatomic site. J. Biomech. 2003, 36, 897–904. [Google Scholar] [CrossRef]
- Koh, Y.G.; Lee, J.A.; Lee, H.Y.; Chun, H.J.; Kim, H.J.; Kang, K.T. Design optimization of high tibial osteotomy plates using finite element analysis for improved biomechanical effect. J. Orthop. Surg. Res. 2019, 14, 1–10. [Google Scholar] [CrossRef]
- Fletcher, J.W.A.; Williams, S.; Whitehouse, M.R.; Gill, H.S.; Preatoni, E. Juvenile bovine bone is an appropriate surrogate for normal and reduced density human bone in biomechanical testing: A validation study. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef]
- Sisljacic, V.; Jovanovic, S.; Mrcela, T.; Nikolic, V.; Radic, R.; Wertheimerc, V.; Tanja Kovac, T.; Mrcela, M. Applicability of bovine tibia as a model in research on various osteosynthesis techniques. Period. Biol. UDC 2010, 112, 59–62. [Google Scholar]
- Bowland, P.; Cowie, R.M.; Ingham, E.; Fisher, J.; Jennings, M. Biomechanical assessment of the stability of osteochondral grafts implanted in porcine and bovine femoral condyles. Proc. Inst. Mech. Eng. Part H. J. Eng. Med. 2019, 234, 163–170. [Google Scholar] [CrossRef]
- Akhbar, M.F.A.; Yuosoff, A.R. Comparison of bone temperature elevation in drilling of human, bovine and porcine bone. Sci. Direct 2019, 82, 411–414. [Google Scholar] [CrossRef]
- Hillerya, M.T.; Shuaibb, I. Temperature effects in the drilling of human and bovine bone. J. Mater. Process. Technol. 1999, 302–308. [Google Scholar] [CrossRef]
- Brown, C.P.; Nguyen, T.C.; Moody, H.R.; Crawford, R.W.; Oloyede, A. Assessment of common hyperelastic constitutive equations for describing normal and osteoarthritic articular cartilage. Proc. Inst. Mech. Eng. Part H-J. Eng. Med. 2009, 223, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Demarteau, O.; Pillet, L.; Inaebnit, A.; Borens, O.; Quinn, T.M. Biomechanical characterization and in vitro mechanical injury of elderly human femoral head cartilage: Comparison to adult bovine humeral head cartilage. Osteoarthr. Cartil. 2006, 14, 589–596. [Google Scholar] [CrossRef][Green Version]
- Koh, Y.G.; Son, J.; Kim, H.J.; Kwon, S.K.; Kwon, O.R.; Kim, H.J.; Kang, K.T. Multi-objective design optimization of high tibial osteotomy for improvement of biomechanical effect by using finite element analysis. J. Orthop. Res. 2018, 36, 2956–2965. [Google Scholar] [CrossRef]
- Russu, O.M.; Strnad, G.; Farkas, L.J.; Cazacu, R.; Feier, A.; Gergely, I.; Trambitas, C.; Petrovan, C. Electrochemical Synthesis of Nanostructured Oxide Layers on Threaded Surfaces of Medical Implants. Rev. Chim. 2018, 69, 1636–1639. [Google Scholar] [CrossRef]
- Andor, B.; Patrascu, J.M.; Florescu, S.; Cojocaru, D.; Sandesc, M.; Borcan, F.; Boruga, O.; Bolintineanu, S. Comparison of Different Knee Implants Used on Patients with Osteoarthritis Control Study. Mater. Plast. 2016, 53, 119–125. [Google Scholar]
- Todor, A.; Vermesan, D.; Haragus, H., Jr.; Patrascu, J.M.; Timar, B.; Cosma, D.I. Cross-cultural adaptation and validation of the Romanian International Knee Documentation Committee—Subjective knee form. PeerJ. 2020, 8, e8448. [Google Scholar] [CrossRef]
- Csernátony, Z.; Kiss, L.; Manó, S. A new technique of wedge osteotomy to diminish undesirable fractures. Eur. J. Orthop. Surg. Traumatol. 2008, 18, 485–488. [Google Scholar] [CrossRef]
- Chernchujit, B.; Tharakulphan, S.; Prasetia, R.; Chantarapanich, N.; Jirawison, C.; Sitthiseripratip, K. Preoperative planning of medial opening wedge high tibial osteotomy using 3D computer-aided design weight-bearing simulated guidance: Technique and preliminary result. J. Orthop. Surg. 2019, 27. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, E.A. Opening wedge high tibial osteotomy in varus osteoarthritis of the knee without bone graft©. Egypt. Orthop. J. 2018, 53, 38–43. [Google Scholar] [CrossRef]


| No. | X1 (mm) | X2 (degree) |
|---|---|---|
| 1 | 30 | 6 |
| 2 | 30 | 10 |
| 3 | 30 | 14 |
| 4 | 40 | 6 |
| 5 | 40 | 10 |
| 6 | 40 | 14 |
| 7 | 50 | 6 |
| 8 | 50 | 10 |
| 9 | 50 | 14 |
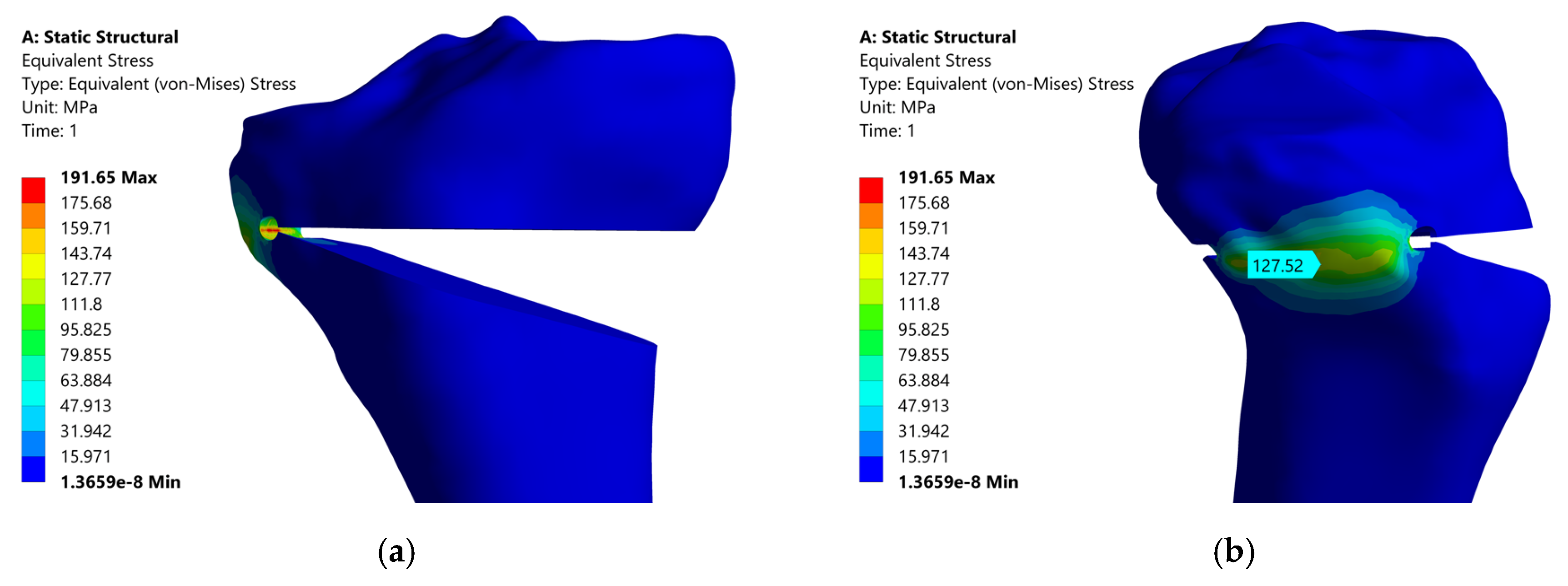
| No. | X1 (mm) | X2 (Degree) | Von Mises Stress (MPa) | Max. Principal Stress (MPa) |
|---|---|---|---|---|
| 1 | 30 | 6 | 67.195 | 76.905 |
| 2 | 30 | 10 | 119.25 | 136.775 |
| 3 | 30 | 14 | 196.61 | 225.49 |
| 4 | 40 | 6 | 65.23 | 74.615 |
| 5 | 40 | 10 | 120.67 | 137.465 |
| 6 | 40 | 14 | 191.65 | 223.865 |
| 7 | 50 | 6 | 69.085 | 78.125 |
| 8 | 50 | 10 | 127.73 | 145.755 |
| 9 | 50 | 14 | 198.16 | 230.905 |
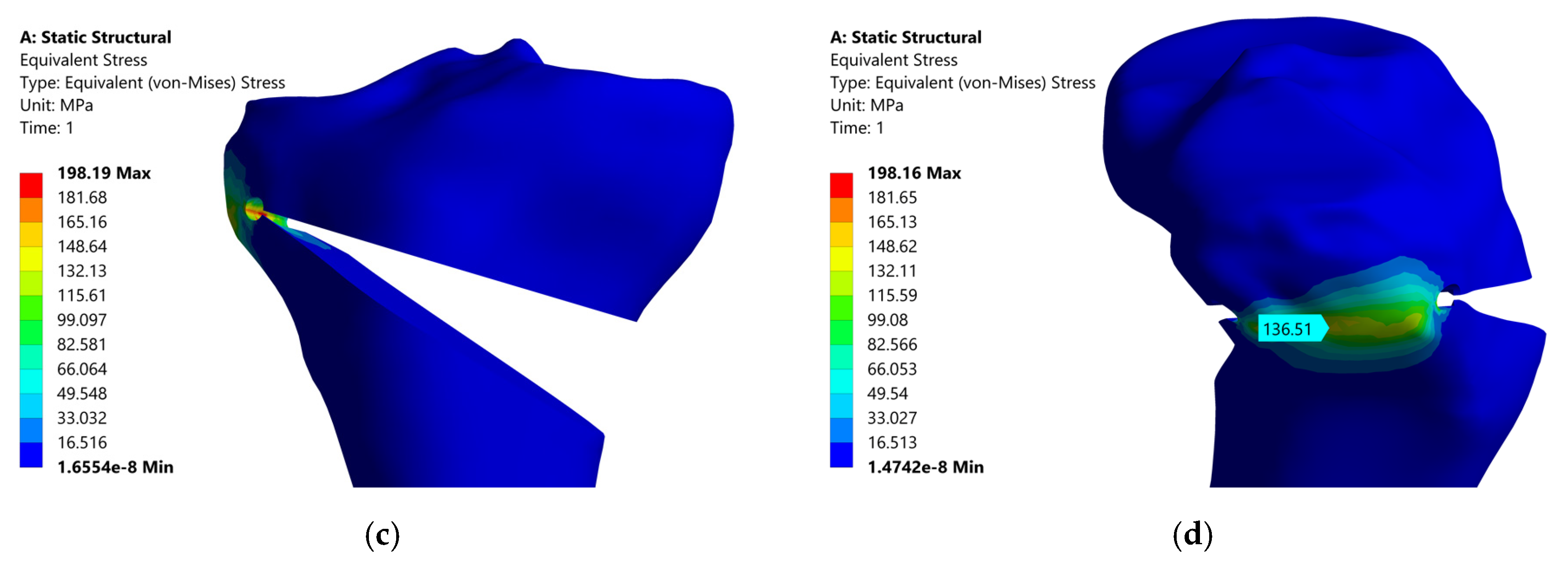
| No. | X1 (mm) | X2 (Degrees) | Fmax (N) |
|---|---|---|---|
| 1 | 30 | 6 | 419.774 |
| 2 | 30 | 10 | 624.373 |
| 3 | 30 | 14 | 660.231 |
| 4 | 40 | 6 | 241.172 |
| 5 | 40 | 10 | 602.558 |
| 6 | 40 | 14 | 782.012 |
| 7 | 50 | 6 | 367.227 |
| 8 | 50 | 10 | 555.678 |
| 9 | 50 | 14 | 577.410 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cofaru, N.F.; Roman, M.D.; Cofaru, I.I.; Oleksik, V.S.; Fleaca, S.R. Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach. Appl. Sci. 2020, 10, 8972. https://doi.org/10.3390/app10248972
Cofaru NF, Roman MD, Cofaru II, Oleksik VS, Fleaca SR. Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach. Applied Sciences. 2020; 10(24):8972. https://doi.org/10.3390/app10248972
Chicago/Turabian StyleCofaru, Nicolae Florin, Mihai Dan Roman, Ileana Ioana Cofaru, Valentin Stefan Oleksik, and Sorin Radu Fleaca. 2020. "Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach" Applied Sciences 10, no. 24: 8972. https://doi.org/10.3390/app10248972
APA StyleCofaru, N. F., Roman, M. D., Cofaru, I. I., Oleksik, V. S., & Fleaca, S. R. (2020). Medial Opening Wedge High Tibial Osteotomy in Knee Osteoarthritis—A Biomechanical Approach. Applied Sciences, 10(24), 8972. https://doi.org/10.3390/app10248972






