Comparison of Cone Beam Computed Tomography and Digital Radiography in Detecting Separated Endodontic Files and Strip Perforation
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
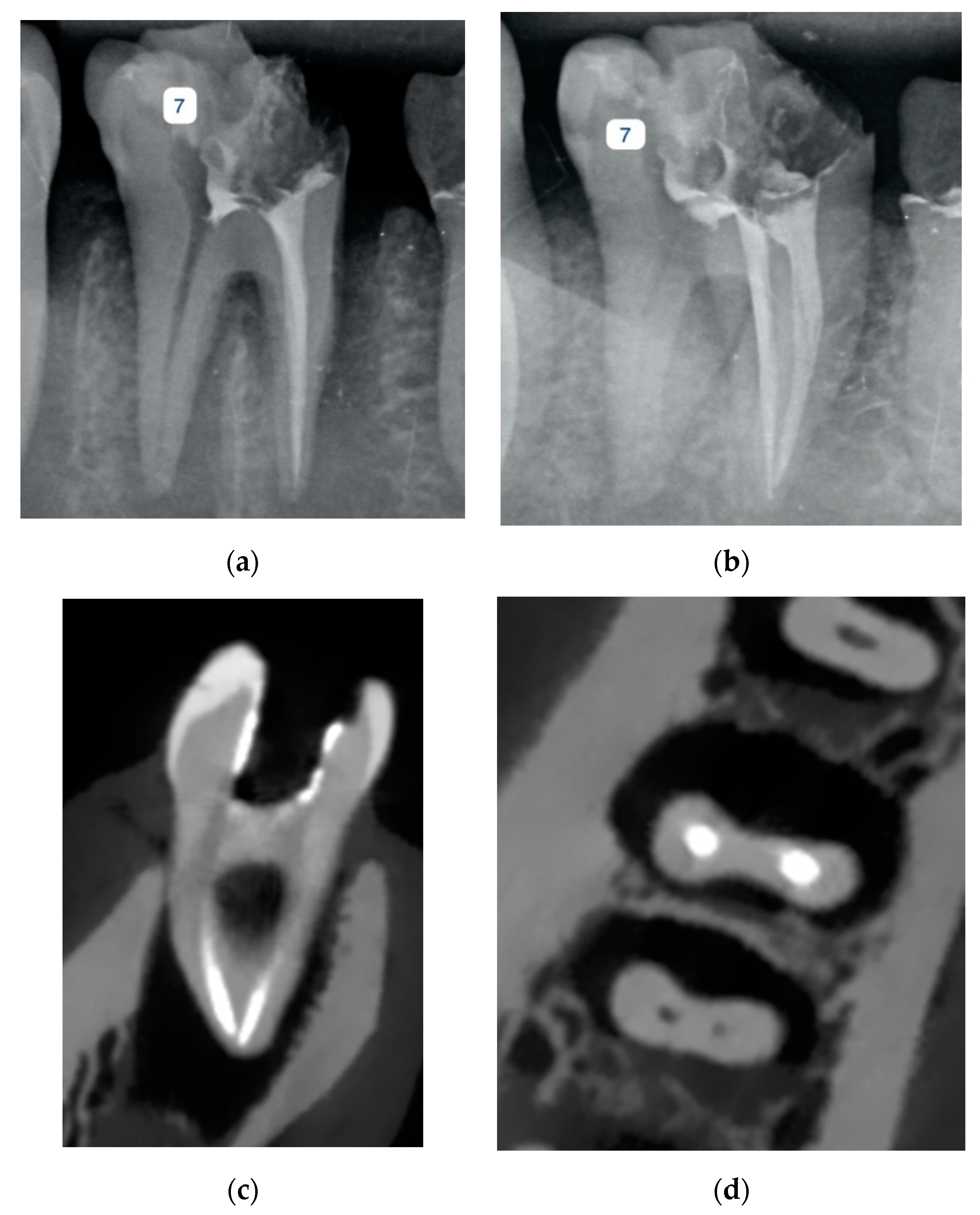
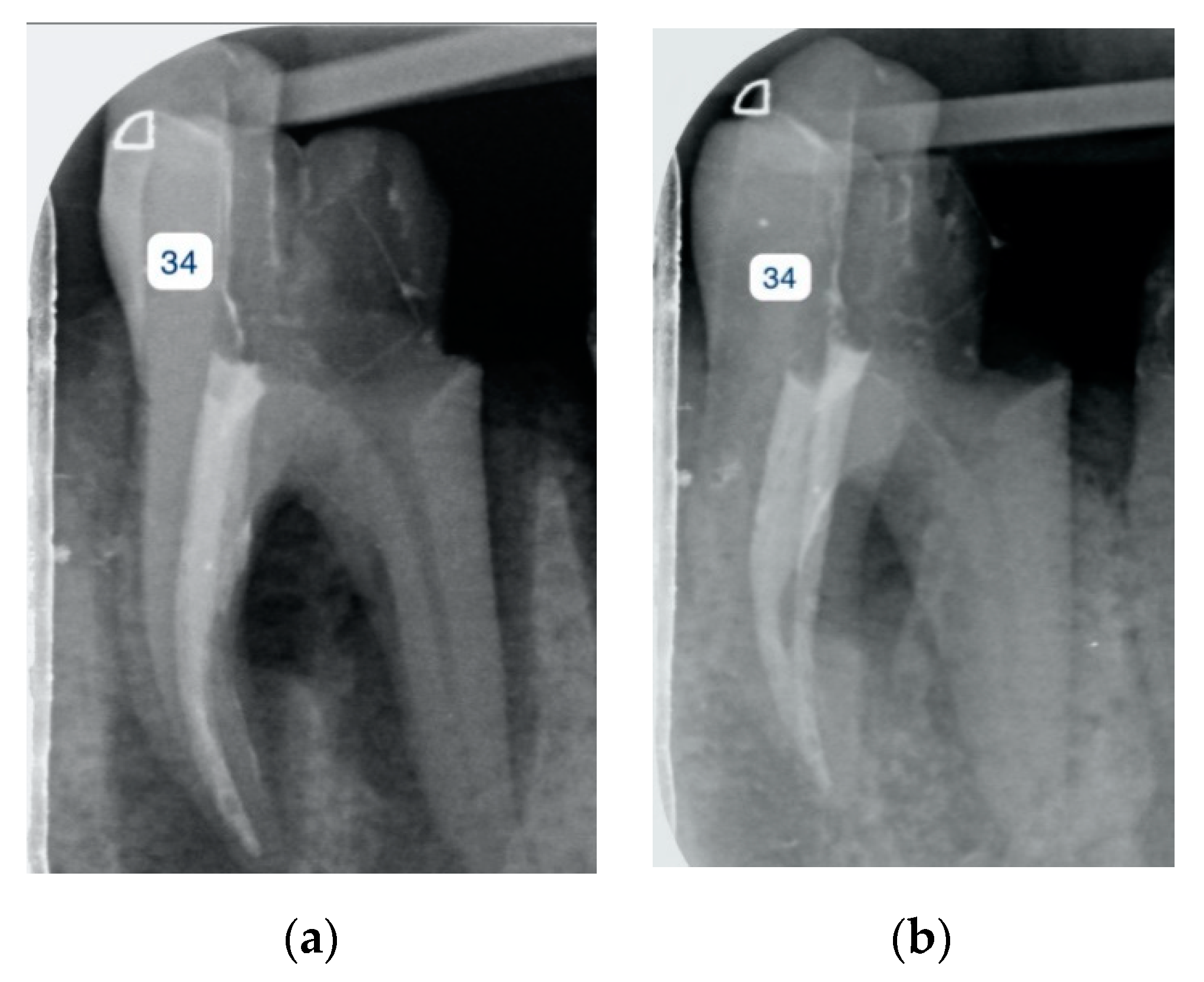
2.1. Sample Preparation
2.2. Imaging Procedure
2.3. Image Evaluation
2.4. Statistical Analysis
3. Results
3.1. Intraobserver and Interobserver Agreement
3.2. Accuracy, Specificity, Sensitivity, NPV, and PPV
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Spagnuolo, G.; Codispoti, B.; Marrelli, M.; Rengo, C.; Rengo, S.; Tatullo, M. Commitment of oral-derived stem cells in dental and maxillofacial applications. Dent. J. 2018, 6, 72. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, F.E.D.; Lima, L.F.; Oliveira, L.S.; Ribeiro, M.A.; Correa, M.B.; Brito-Junior, M.; Faria-e-Silva, A.L. Effectiveness of a reciprocating single file, single cone endodontic treatment approach: A randomized controlled pragmatic clinical trial. Clin. Oral. Investig. 2019, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nosrat, A.; Kolahdouzan, A.; Khatibi, A.H.; Verma, P.; Jamshidi, D.; Nevins, A.J.; Torabinejad, M. Clinical, radiographic, and histologic outcome of regenerative endodontic treatment in human teeth using a novel collagen-hydroxyapatite scaffold. J. Endod. 2019, 45, 136–143. [Google Scholar] [CrossRef]
- Iqbal, A. The factors responsible for endodontic treatment failure in the permanent dentitions of the patients reported to the college of dentistry, the University of Aljouf, Kingdom of Saudi Arabia. J. Clin. Diagn. Res. 2016, 10, 146. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Noiri, Y.; Itoh, Y.; Komichi, S.; Yagi, K.; Uemura, R.; Naruse, H.; Matsui, S.; Kuriki, N.; Hayashi, M.; et al. Factors that cause endodontic failures in general practices in Japan. BMC Oral. Health 2018, 18, 70. [Google Scholar] [CrossRef]
- Akbar, I. Radiographic study of the problems and failures of endodontic treatment. Int. J. Health Sci. 2015, 9, 111. [Google Scholar] [CrossRef]
- Tabassum, S.; Khan, F.R. Failure of endodontic treatment: The usual suspects. Eur. J. Dent. 2016, 10, 144. [Google Scholar] [CrossRef]
- Saber, S.E.-D.M. Factors influencing the fracture of rotary nickel titanium instruments. Endod. Pract. Today 2008, 2, 273–283. [Google Scholar]
- Ametrano, G.; D’Antò, V.; Di Caprio, M.; Simeone, M.; Rengo, S.; Spagnuolo, G. Effects of sodium hypochlorite and ethylenediaminetetraacetic acid on rotary nickel–titanium instruments evaluated using atomic force microscopy. Int. Endod. J. 2011, 44, 203–209. [Google Scholar] [CrossRef]
- Madarati, A.; Watts, D.; Qualtrough, A. Factors contributing to the separation of endodontic files. Br. Dent. J. 2008, 204, 241–245. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Ametrano, G.; D’Antò, V.; Rengo, C.; Simeone, M.; Riccitiello, F.; Amato, M. Effect of autoclaving on the surfaces of TiN-coated and conventional nickel–titanium rotary instruments. Int. Endod. J. 2012, 45, 1148–1155. [Google Scholar] [CrossRef] [PubMed]
- Eghbal, M.J.; Fazlyab, M.; Asgary, S. Repair of a strip perforation with calcium-enriched mixture cement: A case report. Iran Endod. J. 2014, 9, 225–228. [Google Scholar] [PubMed]
- Çalışkan, M.K.; Kaval, M.E.; Tekin, U.; Ünal, T. Radiographic and histological evaluation of persistent periapical lesions associated with endodontic failures after apical microsurgery. Int. Endod. J. 2016, 49, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Nicoloso, G.F.; Pötter, I.G.; Rocha, R.d.O.; Montagner, F.; Casagrande, L. A comparative evaluation of endodontic treatments for immature necrotic permanent teeth based on clinical and radiographic outcomes: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2017, 27, 217–227. [Google Scholar] [CrossRef]
- Mehdizadeh, M.; Booshehri, S.G.; Kazemzadeh, F.; Soltani, P.; Motamedi, M.R. Level of knowledge of dental practitioners in Isfahan, Iran about cone-beam computed tomography and digital radiography. Imaging Sci. Dent. 2015, 45, 133–135. [Google Scholar] [CrossRef]
- Hasheminia, S.M.; Farhad, A.; Sheikhi, M.; Soltani, P.; Hendi, S.S.; Ahmadi, M. Cone-beam computed tomographic analysis of canal transportation and centering ability of single-file systems. J. Endod. 2018, 44, 1788–1791. [Google Scholar] [CrossRef]
- Alemam, S.; Abuelsadat, S.; Saber, S.; Elsewify, T. Accuracy, sensitivity and specificity of three imaging modalities in detection of separated intracanal instruments. G. Ital. Endod. 2020, 34. [Google Scholar] [CrossRef]
- Patel, S.; Brown, J.; Semper, M.; Abella, F.; Mannocci, F. European society of endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int. Endod. J. 2019, 52, 1675–1678. [Google Scholar] [CrossRef]
- Krug, R.; Connert, T.; Beinicke, A.; Soliman, S.; Schubert, A.; Kiefner, P.; Sonntag, D.; Weiger, R.; Krastl, G. When and how do endodontic specialists use cone-beam computed tomography? Aust. Endod. J. 2019, 45, 365–372. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Ayatollahi, F.; Tabrizizadeh, M.; Razavi, H.; Mowji, M. Diagnostic value of cone-beam computed tomography and digital periapical radiography in detection of separated instruments. Iran Endod. J. 2019, 14, 14–17. [Google Scholar]
- D’Addazio, P.; Campos, C.; Özcan, M.; Teixeira, H.; Passoni, R.; Carvalho, A. A comparative study between cone-beam computed tomography and periapical radiographs in the diagnosis of simulated endodontic complications. Int. Endod. J. 2011, 44, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Rosen, E.; Venezia, N.B.; Azizi, H.; Kamburoglu, K.; Meirowitz, A.; Ziv-Baran, T.; Tsesis, I. A comparison of cone-beam computed tomography with periapical radiography in the detection of separated instruments retained in the apical third of root canal-filled teeth. J. Endod. 2016, 42, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Brito, A.C.R.; Verner, F.S.; Junqueira, R.B.; Yamasaki, M.C.; Queiroz, P.M.; Freitas, D.Q.; de Oliveira-Santos, C. Detection of fractured endodontic instruments in root canals: Comparison between different digital radiography systems and cone-beam computed tomography. J. Endod. 2017, 43, 544–549. [Google Scholar] [CrossRef]
- Koç, C.; Sönmez, G.; Yılmaz, F.; Karahan, S.; Kamburoğlu, K. Comparison of the accuracy of periapical radiography with CBCT taken at 3 different voxel sizes in detecting simulated endodontic complications: An ex vivo study. Dentomaxillofac. Radiol. 2018, 47, 20170399. [Google Scholar] [CrossRef] [PubMed]
- Haghanifar, S.; Moudi, E.; Mesgarani, A.; Bijani, A.; Abbaszadeh, N. A comparative study of cone-beam computed tomography and digital periapical radiography in detecting mandibular molars root perforations. Imaging Sci. Dent. 2014, 44, 115–119. [Google Scholar] [CrossRef][Green Version]
- Shemesh, H.; Cristescu, R.C.; Wesselink, P.R.; Wu, M.-K. The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J. Endod. 2011, 37, 513–516. [Google Scholar] [CrossRef]
- Nikeghbal, K.; Zamanian, Z.; Shahidi, S.; Spagnuolo, G.; Soltani, P. Designing and fabricating nano-structured and micro-structured radiation shields for protection against CBCT exposure. Materials 2020, 13, 4371. [Google Scholar] [CrossRef]
- Mallya, S.; Lam, E. White and Pharoah’s Oral Radiology E-Book: Principles and Interpretation; Elsevier: Gurgaon, India, 2019. [Google Scholar]
- Kohli, M.R.; Schloss, T. The use of Cone Beam Computer Tomography (CBCT) in endodontics. Curr. Oral Health Rep. 2019, 6, 377–384. [Google Scholar] [CrossRef]
- Codari, M.; Vasconcelos, K.d.F.; Nicolielo, L.F.P.; Neto, F.H.; Jacobs, R. Quantitative evaluation of metal artifacts using different CBCT devices, high-density materials and field of views. Clin. Oral Implants Res. 2017, 28, 1509–1514. [Google Scholar] [CrossRef]
- Lupi, S.M.; Galinetto, P.; Cislaghi, M.; Baena, A.R.Y.; Scribante, A.; Baena, R.R.Y. Geometric distortion of panoramic reconstruction in third molar tilting assessments: A comprehensive evaluation. Dentomaxillofac. Radiol. 2018, 47, 20170467. [Google Scholar] [CrossRef] [PubMed]
- Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in endodontics 2015 update. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Schulze, R.; Heil, U.; Groβ, D.; Bruellmann, D.; Dranischnikow, E.; Schwanecke, U.; Schoemer, E. Artefacts in CBCT: A review. Dentomaxillofac. Radiol. 2011, 40, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, R.; Stamatakis, H.; Bosmans, H.; Bogaerts, R.; Jacobs, R.; Horner, K.; Tsiklakis, K. Quantification of metal artifacts on cone beam computed tomography images. Clin. Oral Implants Res. 2013, 24, 94–99. [Google Scholar] [CrossRef]
- Iikubo, M.; Nishioka, T.; Okura, S.; Kobayashi, K.; Sano, T.; Katsumata, A.; Ariji, E.; Kojima, I.; Sakamoto, M.; Sasano, T. Influence of voxel size and scan field of view on fracture-like artifacts from gutta-percha obturated endodontically treated teeth on cone-beam computed tomography images. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 631–637. [Google Scholar] [CrossRef]
- Helvacioglu-Yigit, D.; Kocasarac, H.D.; Bechara, B.; Noujeim, M. Evaluation and reduction of artifacts generated by 4 different root-end filling materials by using multiple cone-beam computed tomography imaging settings. J. Endod. 2016, 42, 307–314. [Google Scholar] [CrossRef]
- Celikten, B.; Jacobs, R.; Vasconcelos, K.d.F.; Huang, Y.; Nicolielo, L.F.P.; Orhan, K. Assessment of volumetric distortion artifact in filled root canals using different cone-beam computed tomographic devices. J. Endod. 2017, 43, 1517–1521. [Google Scholar] [CrossRef]
- Katsumata, A.; Hirukawa, A.; Noujeim, M.; Okumura, S.; Naitoh, M.; Fujishita, M.; Ariji, E.; Langlais, R.P. Image artifact in dental cone-beam CT. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, 652–657. [Google Scholar] [CrossRef]
- Suetens, P. Fundamentals of Medical Imaging; Cambridge University Press: Cambridge, UK, 2017. [Google Scholar]
- Vanderstuyft, T.; Tarce, M.; Sanaan, B.; Jacobs, R.; Vasconcelos, K.d.F.; Quirynen, M. Inaccuracy of buccal bone thickness estimation on cone-beam CT due to implant blooming: An ex-vivo study. J. Clin. Periodontol. 2019, 46, 1134–1143. [Google Scholar] [CrossRef]
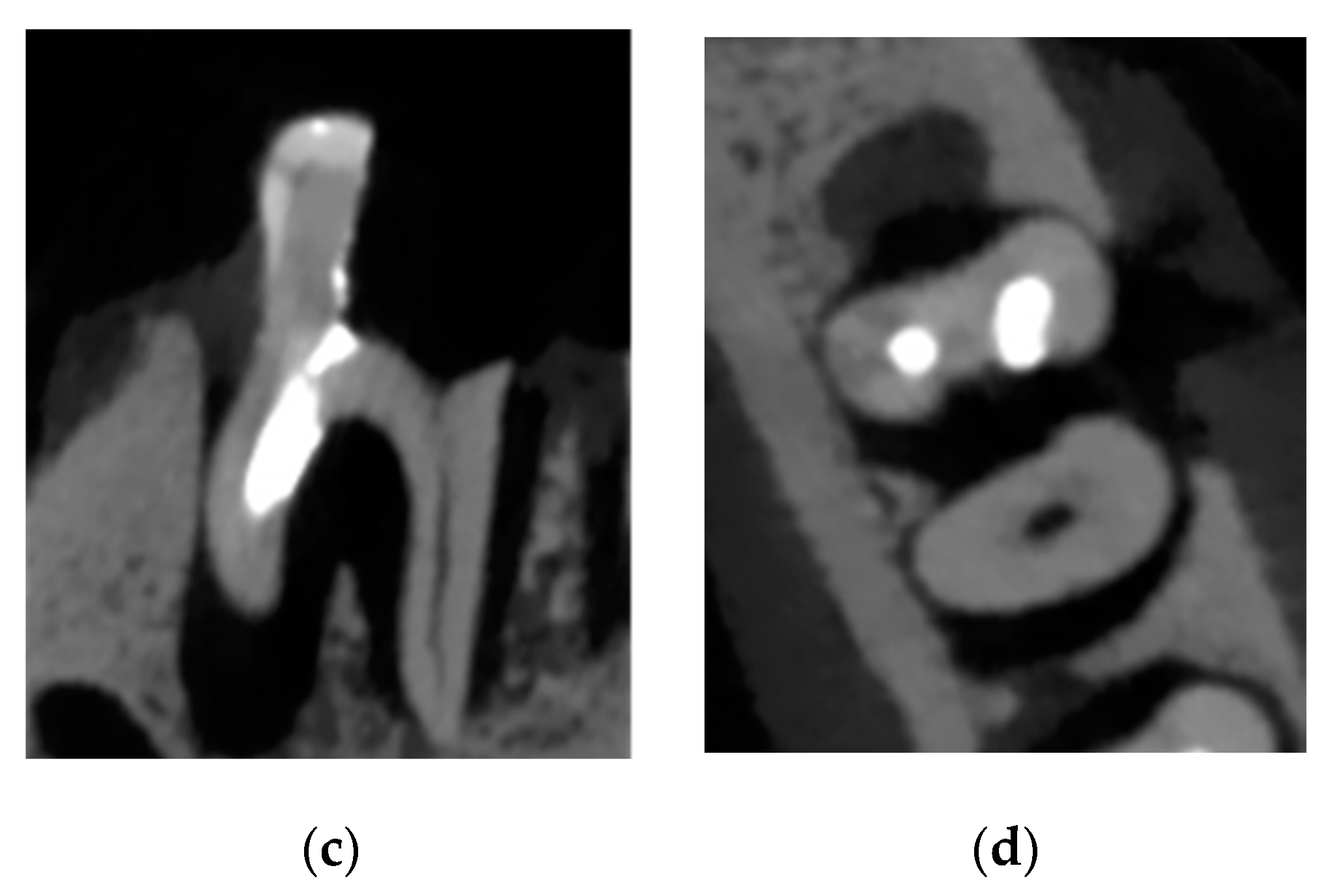
| Accuracy | p | 95% Confidence Interval | Sensitivity | Specificity | PPV | NPV | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||||
| Observer 1 | Periapical radiograph | 0.750 | 0.003 | 0.607 | 0.893 | 0.560 | 0.920 | 0.875 | 0.677 |
| CBCT | 0.576 | 0.369 | 0.412 | 0.739 | 0.440 | 0.760 | 0.647 | 0.576 | |
| Observer 2 | Periapical radiograph | 0.875 | 0.000 | 0.766 | 0.984 | 0.840 | 0.920 | 0.913 | 0.852 |
| CBCT | 0.773 | 0.001 | 0.635 | 0.911 | 0.826 | 0.720 | 0.731 | 0.818 | |
| Observer 3 | Periapical radiograph | 0.896 | 0.000 | 0.795 | 0.997 | 0.958 | 0.833 | 0.852 | 0.952 |
| CBCT | 0.659 | 0.059 | 0.502 | 0.817 | 0.440 | 0.840 | 0.733 | 0.600 | |
| Observers’ average | Periapical radiograph | 0.950 | 0.000 | 0.839 | 1.000 | 0.813 | 0.957 | 0.929 | 0.880 |
| CBCT | 0.747 | 0.031 | 0.541 | 0.954 | 0.667 | 0.900 | 0.833 | 0.783 | |
| Accuracy | p | 95% Confidence Interval | Sensitivity | Specificity | PPV | NPV | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||||
| Observer 1 | Periapical radiograph | 0.795 | 0.001 | 0.656 | 0.935 | 0.640 | 0.920 | 0.889 | 0.719 |
| CBCT | 0.920 | 0.000 | 0.832 | 1.000 | 1.000 | 0.840 | 0.862 | 1.000 | |
| Observer 2 | Periapical radiograph | 0.932 | 0.000 | 0.845 | 1.000 | 0.957 | 0.913 | 0.917 | 0.955 |
| CBCT | 0.900 | 0.000 | 0.803 | 0.997 | 0.960 | 0.840 | 0.857 | 0.955 | |
| Observer 3 | Periapical radiograph | 0.727 | 0.010 | 0.574 | 0.881 | 0.750 | 0.625 | 0.667 | 0.714 |
| CBCT | 0.960 | 0.000 | 0.897 | 1.000 | 1.000 | 0.920 | 0.926 | 1.000 | |
| Observers’ average | Periapical radiograph | 0.855 | 0.000 | 0.729 | 0.980 | 0.800 | 0.909 | 0.889 | 0.833 |
| CBCT | 0.955 | 0.000 | 0.883 | 1.000 | 1.000 | 0.920 | 0.926 | 1.000 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdinian, M.; Moshkforoush, S.; Hemati, H.; Soltani, P.; Moshkforoushan, M.; Spagnuolo, G. Comparison of Cone Beam Computed Tomography and Digital Radiography in Detecting Separated Endodontic Files and Strip Perforation. Appl. Sci. 2020, 10, 8726. https://doi.org/10.3390/app10238726
Abdinian M, Moshkforoush S, Hemati H, Soltani P, Moshkforoushan M, Spagnuolo G. Comparison of Cone Beam Computed Tomography and Digital Radiography in Detecting Separated Endodontic Files and Strip Perforation. Applied Sciences. 2020; 10(23):8726. https://doi.org/10.3390/app10238726
Chicago/Turabian StyleAbdinian, Mehrdad, Saba Moshkforoush, Hamidreza Hemati, Parisa Soltani, Mansoure Moshkforoushan, and Gianrico Spagnuolo. 2020. "Comparison of Cone Beam Computed Tomography and Digital Radiography in Detecting Separated Endodontic Files and Strip Perforation" Applied Sciences 10, no. 23: 8726. https://doi.org/10.3390/app10238726
APA StyleAbdinian, M., Moshkforoush, S., Hemati, H., Soltani, P., Moshkforoushan, M., & Spagnuolo, G. (2020). Comparison of Cone Beam Computed Tomography and Digital Radiography in Detecting Separated Endodontic Files and Strip Perforation. Applied Sciences, 10(23), 8726. https://doi.org/10.3390/app10238726






