Intravoxel Incoherent Motion Model of Diffusion Weighted Imaging and Diffusion Kurtosis Imaging in Differentiating of Local Colorectal Cancer Recurrence from Scar/Fibrosis Tissue by Multivariate Logistic Regression Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Dataset Characteristics
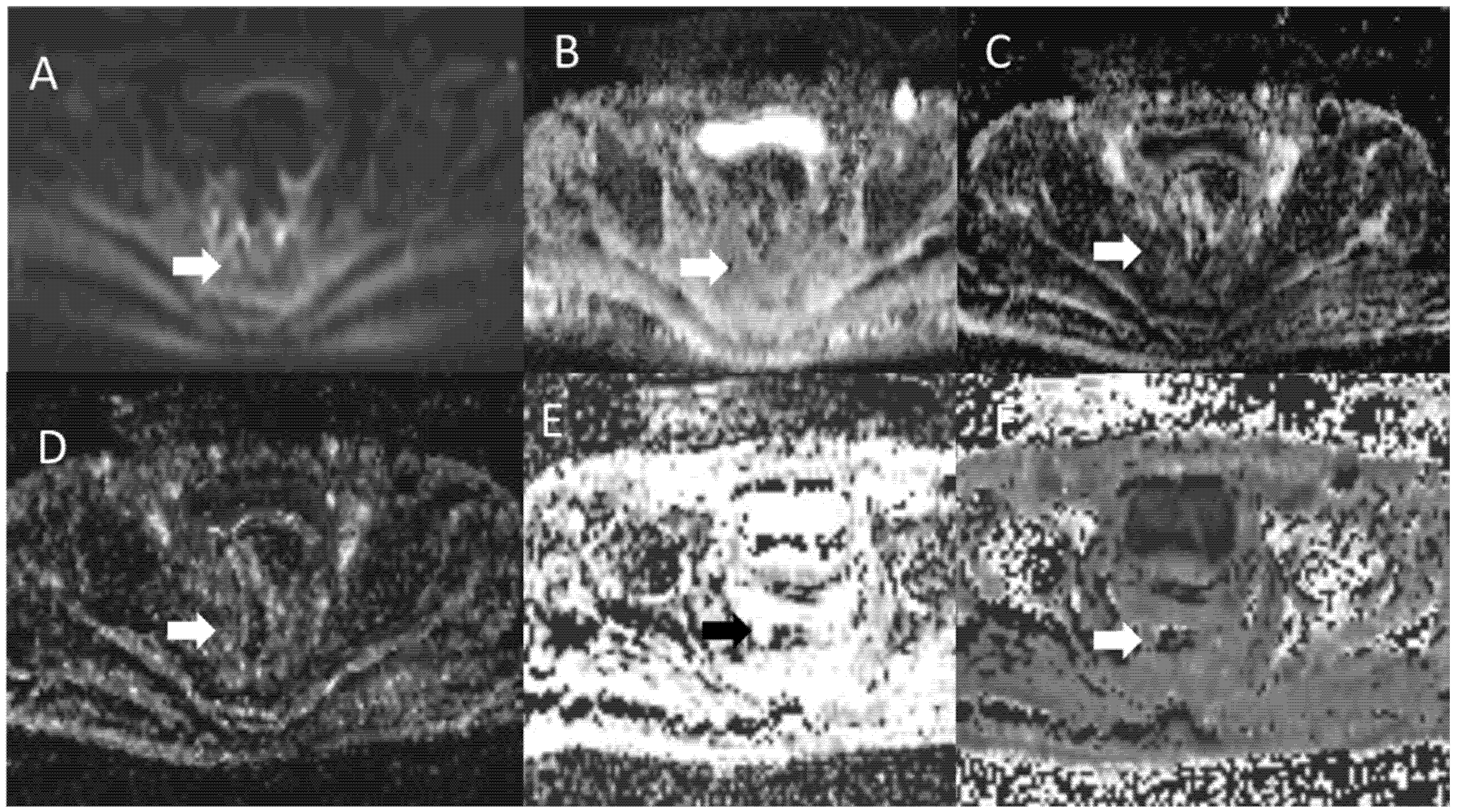
2.2. MR Imaging Protocol
2.3. Data Analysis
DWI Features
2.4. Statistical Analysis
2.4.1. Univariate Analysis
2.4.2. Multivariate Analysis
3. Results
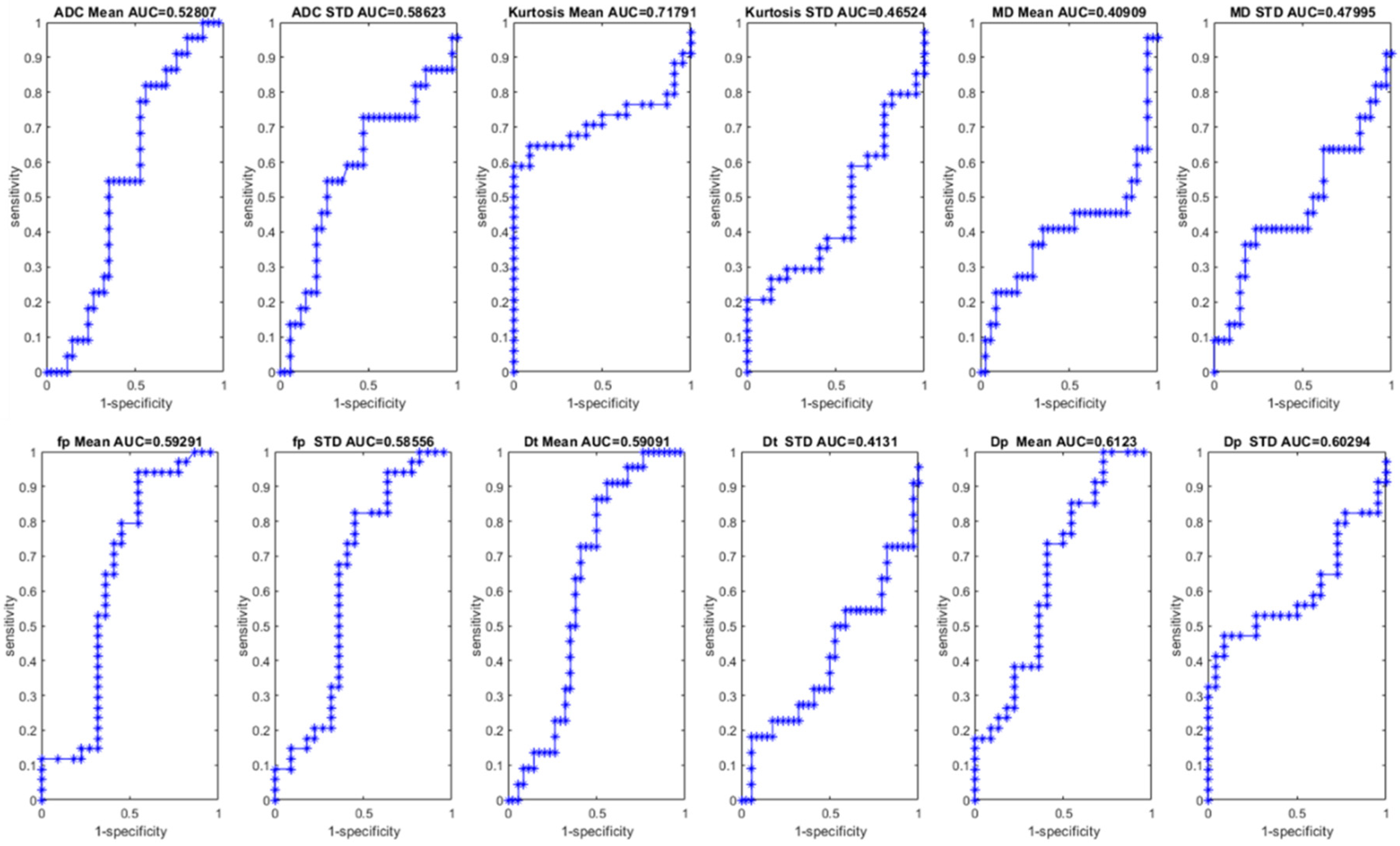
3.1. Univariate Analysis Results
3.2. Multivariate Analysis Results
4. Discussions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer ststistics. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Malvezzi, M.; Bertuccio, P.; Levi, F.; La Vecchia, C.; Negri, E. European cancer mortality predictions for the year 2014. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. ESMO 2014, 25, 1650–1656. [Google Scholar] [CrossRef] [PubMed]
- Sauer, R.; Becker, H.; Hohenberger, W.; Rödel, C.; Wittekind, C.; Fietkau, R.; Martus, P.; Tschmelitsch, J.; Hager, E.; Hess, C.F.; et al. German Rectal Cancer Study Group. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N. Engl. J. Med. 2004, 351, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Sugarbaker, P.H. Update on the prevention of local recurrence and peritoneal metastases in patients with colorectal cancer. World J. Gastroenterol. 2014, 20, 9286–9291. [Google Scholar] [CrossRef] [PubMed]
- Abulafi, A.M.; Williams, N.S. Local recurrence of colorectal cancer: The problem, mechanisms, management and adjuvant therapy. Br. J. Surg. 1994, 81, 7–19. [Google Scholar] [CrossRef]
- Cai, Y.; Li, Z.; Gu, X.; Fang, Y.; Xiang, J.; Chen, Z. Prognostic factors associated with locally recurrent rectal cancer following primary surgery (Review). Oncol. Lett. 2014, 7, 10–16. [Google Scholar] [CrossRef]
- Lambregts, D.M.J.; Cappendijk, V.C.; Maas, M.; Beets, G.L.; Beets-Tan, R.G.H. Value of MRI and diffusion-weighted MRI for the diagnosis of locally recurrent rectal cancer. Eur. Radiol. 2011, 21, 1250–1258. [Google Scholar] [CrossRef]
- Beets-Tan, R.G.H.; Beets, G.L. Rectal Cancer: Review with Emphasis on MR Imaging. Radiology 2004, 232, 335–346. [Google Scholar] [CrossRef]
- Curvo-Semedo, L.; Lambregts, D.M.J.; Maas, M.; Thywissen, T.; Mehsen, R.T.; Lammering, G.; Beets, G.L.; Caseiro-Alves, F.; Beets-Tan, R.G.H. Rectal Cancer: Assessment of Complete Response to Preoperative Combined Radiation Therapy with Chemotherapy—Conventional MR Volumetry versus Diffusion-weighted MR Imaging. Radiology 2011, 260, 734–743. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Catalano, O.; Filice, S.; Amato, D.M.; Nasti, G.; Avallone, A.; Izzo, F.; Petrillo, A. Early Assessment of Colorectal Cancer Patients with Liver Metastases Treated with Antiangiogenic Drugs: The Role of Intravoxel Incoherent Motion in Diffusion-Weighted Imaging. PLoS ONE 2015, 10, e0142876. [Google Scholar] [CrossRef]
- Petrillo, A.; Fusco, R.; Granata, V.; Filice, S.; Sansone, M.; Rega, D.; DelRio, P.; Bianco, F.; Romano, G.M.; Tatangelo, F.; et al. Assessing response to neo-adjuvant therapy in locally advanced rectal cancer using Intra-voxel Incoherent Motion modelling by DWI data and Standardized Index of Shape from DCE-MRI. Ther. Adv. Med. Oncol. 2018, 10, 1758835918809875. [Google Scholar] [CrossRef] [PubMed]
- Fusco, R.; Sansone, M.; Granata, V.; Grimm, R.; Pace, U.; DelRio, P.; Tatangelo, F.; Botti, G.; Avallone, A.; Pecori, B.; et al. Diffusion and perfusion MR parameters to assess preoperative short-course radiotherapy response in locally advanced rectal cancer: A comparative explorative study among Standardized Index of Shape by DCE-MRI, intravoxel incoherent motion- and diffusion kurtosis imaging-derived parameters. Abdom. Radiol. 2019, 44, 3683–3700. [Google Scholar]
- Nishie, A.; Stolpen, A.; Obuchi, M.; Kuehn, D.M.; Dagit, A.; Andresen, K. Evaluation of locally recurrent pelvic malignancy: Performance of T2- and diffusion-weighted MRI with image fusion. J. Magn. Reson. Imaging 2008, 28, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Le Bihan, D.; Breton, E.; Lallemand, D.; Aubin, M.L.; Vignaud, J.; Laval-Jeantet, M. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 1988, 168, 497–505. [Google Scholar] [CrossRef]
- Le Bihan, D.; Breton, E.; Lallemand, D.; Grenier, P.; Cabanis, E.; Laval-Jeantet, M. MR imaging of intravoxel incoherent motions: Application to diffusion and perfusion in neurologic disorders. Radiology 1986, 161, 401–407. [Google Scholar] [CrossRef]
- Koh, D.-M.; Collins, D.J.; Orton, M.R. Intravoxel Incoherent Motion in Body Diffusion-Weighted MRI: Reality and Challenges. Am. J. Roentgenol. 2011, 196, 1351–1361. [Google Scholar] [CrossRef]
- Meng, N.; Bs, X.W.; Sun, J.; Huang, L.; Wang, Z.; Wang, K.; Wang, J.; Ms, D.H.; Wang, M. Comparative Study of Amide Proton Transfer-Weighted Imaging and Intravoxel Incoherent Motion Imaging in Breast Cancer Diagnosis and Evaluation. J. Magn. Reson. Imaging 2020, 52, 1175–1186. [Google Scholar] [CrossRef]
- Jensen, J.H.; Helpern, J.A. MRI quantification of non-Gaussian water diffusion by kurtosis analysis. NMR Biomed. 2010, 23, 698–710. [Google Scholar] [CrossRef]
- Elmi, A.; Hedgire, S.; Covarrubias, D.; Abtahi, S.; Hahn, P.; Harisinghani, M. Apparent diffusion coefficient as a non-invasive predictor of treatment response and recurrence in locally advanced rectal cancer. Clin. Radiol. 2013, 68, e524–e531. [Google Scholar] [CrossRef]
- Cai, G.; Xu, Y.; Zhu, J.; Gu, W.-L.; Zhang, S.; Ma, X.-J.; Cai, S.-J.; Zhang, Z. Diffusion-weighted magnetic resonance imaging for predicting the response of rectal cancer to neoadjuvant concurrent chemoradiation. World J. Gastroenterol. 2013, 19, 5520–5527. [Google Scholar] [CrossRef]
- Jung, S.H.; Heo, S.H.; Kim, J.W.; Jeong, Y.Y.; Shin, S.S.; Soung, M.-G.; Kim, H.R.; Kang, H.K. Predicting response to neoadjuvant chemoradiation therapy in locally advanced rectal cancer: Diffusion-weighted 3 tesla MR imaging. J. Magn. Reson. Imaging 2012, 35, 110–116. [Google Scholar] [CrossRef]
- Petrillo, A.; Fusco, R.; Petrillo, M.; Granata, V.; Sansone, M.; Avallone, A.; DelRio, P.; Pecori, B.; Tatangelo, F.; Ciliberto, G. Standardized Index of Shape (SIS): A quantitative DCE-MRI parameter to discriminate responders by non-responders after neoadjuvant therapy in LARC. Eur. Radiol. 2015, 25, 1935–1945. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, M.; Fusco, R.; Catalano, O.; Sansone, M.; Avallone, A.; DelRio, P.; Pecori, B.; Tatangelo, F.; Petrillo, A. MRI for Assessing Response to Neoadjuvant Therapy in Locally Advanced Rectal Cancer Using DCE-MR and DW-MR Data Sets: A Preliminary Report. BioMed Res. Int. 2015, 2015, 514740. [Google Scholar] [CrossRef] [PubMed]
- Grosu, S.; Schäfer, A.-O.; Baumann, T.; Manegold, P.; Langer, M.; Gerstmair, A. Differentiating locally recurrent rectal cancer from scar tissue: Value of diffusion-weighted MRI. Eur. J. Radiol. 2016, 85, 1265–1270. [Google Scholar] [CrossRef] [PubMed]
- Efroymson, M.A. Multiple regression analysis. In Mathematical Methods for Digital Computers; Ralston, A., Wilf, H.S., Eds.; Wiley: New York, NY, USA, 1960. [Google Scholar]
- Dulk, M.D.; Marijnen, C.A.M.; Putter, H.; Rutten, H.J.T.; Beets, G.L.; Wiggers, T.; Nagtegaal, I.D.; Van De Velde, C.J.H. Risk Factors for Adverse Outcome in Patients with Rectal Cancer Treated with an Abdominoperineal Resection in the Total Mesorectal Excision Trial. Ann. Surg. 2007, 246, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; De Anda, E.H.; Finne, C.O.; Madoff, R.D.; Garcia-Aguilar, J. The Effect of Circumferential Tumor Location in Clinical Outcomes of Rectal Cancer Patients Treated with Total Mesorectal Excision. Dis. Colon Rectum 2005, 48, 2249–2257. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.L.; Bokey, E.L.; Chapuis, P.H.; Renwick, A.A.; Dent, O.F. Local recurrence after curative resection for rectal cancer is associated with anterior position of the tumour. Br. J. Surg. 2006, 93, 105–112. [Google Scholar] [CrossRef]
- Gunderson, L.L.; Sargent, D.J.; Tepper, J.E.; Wolmark, N.; O’Connell, M.J.; Begovic, M.; Allmer, C.; Colangelo, L.; Smalley, S.R.; Haller, D.G.; et al. Impact of T and N stage and treatment on survival and relapse in adjuvant rectal cancer: A pooled analysis. J. Clin. Oncol. 2004, 22, 1785–1796. [Google Scholar] [CrossRef]
- Kitz, J.; Fokas, E.; Beissbarth, T.; Ströbel, P.; Wittekind, C.; Hartmann, A.; Rüschoff, J.; Papadopoulos, T.; Rösler, E.; Ortloff-Kittredge, P.; et al. German Rectal Cancer Study Group. Association of Plane of Total Mesorectal Excision with Prognosis of Rectal Cancer: Secondary Analysis of the CAO/ARO/AIO-04 Phase 3 Randomized Clinical Trial. JAMA Surg. 2018, 153, e181607. [Google Scholar] [CrossRef]
- Boras, Z.; Kondza, G.; Sisljagić, V.; Busić, Z.; Gmajnić, R.; Istvanić, T. Prognostic factors of local recurrence and survival after curative rectal cancer surgery: A single institution experience. Coll. Antropol. 2012, 36, 1355–1361. [Google Scholar]
- Dulk, M.D.; Putter, H.; Collette, L.; Marijnen, C.A.; Folkesson, J.; Bosset, J.-F.; Rödel, C.; Bujko, K.; Påhlman, L.; Van De Velde, C. The abdominoperineal resection itself is associated with an adverse outcome: The European experience based on a pooled analysis of five European randomised clinical trials on rectal cancer. Eur. J. Cancer 2009, 45, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Hupkens, B.J.P.; Maas, M.; Martens, M.H.; Deserno, W.M.L.L.G.; Leijtens, J.W.A.; Nelemans, P.J.; Bakers, F.C.H.; Lambregts, D.M.J.; Beets, G.L.; Beets-Tan, R.G.H. MRI surveillance for the detection of local recurrence in rectal cancer after transanal endoscopic microsurgery. Eur. Radiol. 2017, 27, 4960–4969. [Google Scholar] [CrossRef]
- Colosio, A.; Soyer, P.; Rousset, P.; Barbe, C.; Nguyen, F.; Bouché, O.; Hoeffel, C. Value of diffusion-weighted and gadolinium-enhanced MRI for the diagnosis of pelvic recurrence from colorectal cancer. J. Magn. Reson. Imaging 2014, 40, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.; Foudi, F.; Charton, J.; Jung, M.; Lang, H.; Saussine, C.; Jacqmin, D. Comparative Sensitivities of Functional MRI Sequences in Detection of Local Recurrence of Prostate Carcinoma After Radical Prostatectomy or External-Beam Radiotherapy. AJR Am. J. Roentgenol. 2013, 200, W361–W368. [Google Scholar] [CrossRef]
- Molinelli, V.; Angeretti, M.G.; Duka, E.; Tarallo, N.; Bracchi, E.; Novario, R.; Fugazzola, C. Role of MRI and added value of diffusion-weighted and gadolinium-enhanced MRI for the diagnosis of local recurrence from rectal cancer. Abdom. Radiol. 2018, 43, 2903–2912. [Google Scholar] [CrossRef]
- Filli, L.; Wurnig, M.; Nanz, D.; Luechinger, R.; Kenkel, D.; Boss, A. Whole-body diffusion kurtosis imaging: Initial experience on non-Gaussian diffusion in various organs. Investig. Radiol. 2014, 49, 773–778. [Google Scholar] [CrossRef]
- Pentang, G.; Lanzman, R.S.; Heusch, P.; Müller-Lutz, A.; Blondin, D.; Antoch, G.; Wittsack, H.-J. Diffusion kurtosis imaging of the human kidney: A feasibility study. Magn. Reson. Imaging 2014, 32, 413–420. [Google Scholar] [CrossRef]
- Wittsack, H.-J.; Lanzman, R.S.; Mathys, C.; Janssen, H.; Mödder, U.; Blondin, D. Statistical evaluation of diffusion-weighted imaging of the human kidney. Magn. Reson. Med. 2010, 64, 616–622. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Sansone, M.; Grassi, R.; Maio, F.; Palaia, R.; Tatangelo, F.; Botti, G.; Grimm, R.; Curley, S.; et al. Magnetic resonance imaging in the assessment of pancreatic cancer with quantitative parameter extraction by means of dynamic contrast-enhanced magnetic resonance imaging, diffusion kurtosis imaging and intravoxel incoherent motion diffusion-weighted imaging. Ther. Adv. Gastroenterol. 2020, 13, 1756284819885052. [Google Scholar]
- Granata, V.; Fusco, R.; Setola, S.V.; Palaia, R.; Albino, V.; Piccirillo, M.; Grimm, R.; Petrillo, A.; Izzo, F. Diffusion kurtosis imaging and conventional diffusion weighted imaging to assess electrochemotherapy response in locally advanced pancreatic cancer. Radiol. Oncol. 2019, 53, 15–24. [Google Scholar] [CrossRef]


| Patients Description | Numbers (%)/Range |
|---|---|
| Gender | Men 37 (66.1%) |
| Women 19 (33.9%) | |
| Age | 62.5 y; range: 35–82 y |
| Local recurrence Description | |
| Presacral site | 14 (41.2%) |
| Anastomotic site | 7 (20.6%) |
| Rectal lumen | 10 (29.4%) |
| Precoccygeal site | 3 (8.8%) |
| ADC Mean [mm2/s × 10−6] | ADC STD [mm2/s × 10−6] | Kurtosis Mean [×10−3] * | Kurtosis STD [×10−3] * | MD Mean [mm2/s × 10−6] | MD STD [mm2/s × 10−6] | fp Mean [%] | fp STD [%] | Dt Mean [mm2/s × 10−6] | Dt STD [mm2/s × 10−6] | Dp Mean [mm2/s × 10−5] | Dp STD [mm2/s × 10−5] | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scar/Fibrosis | Median value | 1424.0 | 260.4 | 988.5 | 414.0 | 2305.8 | 499.1 | 13.0 | 70.8 | 1262.6 | 256.4 | 104.0 | 76.4 |
| STD | 374.7 | 86.3 | 209.9 | 92.6 | 688.7 | 242.6 | 6.9 | 34.9 | 384.4 | 107.8 | 29.3 | 20.1 | |
| Recurrence | Median value | 1122.9 | 202.2 | 1335.1 | 397.5 | 1893.9 | 515.1 | 16.4 | 94.2 | 983.3 | 240.2 | 107.9 | 79.5 |
| STD | 446.1 | 100.8 | 485.7 | 196.0 | 615.3 | 226.8 | 6.0 | 31.5 | 439.5 | 97.0 | 33.5 | 31.7 | |
| Total | Median value | 1146.6 | 214.0 | 1188.7 | 397.5 | 1941.8 | 515.0 | 16.1 | 93.0 | 1024.3 | 242.7 | 107.8 | 77.3 |
| STD | 438.8 | 99.0 | 470.2 | 183.3 | 626.6 | 229.1 | 6.2 | 32.1 | 437.1 | 98.7 | 32.8 | 30.2 | |
| p value at Wilcoxon-Mann-Whitney U test | 0.47 | 0.28 | 0.01 | 0.67 | 0.25 | 0.80 | 0.08 | 0.10 | 0.13 | >0.28 | 0.05 | 0.20 | |
| AUC | Sensitivity [%] | Specificity [%] | PPV [%] | NPV [%] | Accuracy [%] | Cut-off Value | |
|---|---|---|---|---|---|---|---|
| ADC Mean [mm2/s × 10−6] | 0.53 | 81.8 | 44.1 | 48.7 | 79.0 | 58.9 | 1054.3 |
| ADC STD [mm2/s × 10−6] | 0.59 | 54.6 | 73.5 | 57.1 | 71.4 | 66.1 | 246.6 |
| Kurtosis Mean [×10−3] * | 0.72 | 58.8 | 100.0 | 100.0 | 61.1 | 75.0 | 1184.1 |
| Kurtosis STD [×10−3] * | 0.47 | 20.6 | 100.0 | 100.0 | 44.9 | 51.8 | 561.1 |
| MD Mean [mm2/s × 10−6] | 0.41 | 22.7 | 91.2 | 62.5 | 64.6 | 64.3 | 2738.0 |
| MD STD [mm2/s × 10−6] | 0.48 | 36.4 | 82.4 | 57.1 | 66.7 | 64.3 | 699.7 |
| fp Mean [%] | 0.59 | 94.1 | 45.5 | 72.7 | 83.3 | 75.0 | 9.5 |
| fp STD [%] | 0.59 | 82.4 | 54.6 | 73.7 | 66.7 | 71.4 | 7.0 |
| Dt Mean [mm2/s × 10−6] | 0.59 | 86.4 | 50.0 | 52.8 | 85.0 | 64.3 | 981.7 |
| Dt STD [mm2/s × 10−6] | 0.41 | 18.2 | 94.1 | 66.7 | 64.0 | 64.3 | 344.2 |
| Dp Mean [mm2/s × 10−5] | 0.61 | 73.5 | 59.1 | 73.5 | 59.1 | 67.9 | 93.1 |
| Dp STD [mm2/s × 10−5] | 0.60 | 47.1 | 90.9 | 88.9 | 52.6 | 64.3 | 82.4 |
| Univariate Regression Analysis | Coefficients ×10−3 | Odds Ratio | p Value | |
|---|---|---|---|---|
| PARAMETER | ADC Mean | −0.1 | −1.9 | 0.05 |
| ADC STD | −0.4 | −1.6 | 0.12 | |
| Kurtosis Mean | 0.2 | 3.8 | <<0.01 | |
| Kurtosis STD | 0.1 | 0.9 | 0.37 | |
| MD Mean | −0.0 | −0.7 | 0.51 | |
| MD STD | −0.1 | −0.8 | 0.44 | |
| fp Mean | 0.8 | 1.7 | 0.09 | |
| fp STD | 1.3 | 1.5 | 0.13 | |
| Dt Mean | 0.9 | 1.0 | 0.32 | |
| Dt STD | −0.2 | −0.7 | 0.47 | |
| Dp Mean | −0.2 | −2.4 | 0.02 | |
| Dp STD | 1.0 | 1.0 | 0.30 | |
| Multivariate Regression Analysis | Coefficients ×10−3 | Odds Ratio | p Value | |
| PARAMETER | ADC Mean | 0.3 | 2.2 | 0.02 |
| Kurtosis Mean | 0.5 | 3.6 | <<0.01 | |
| fp Mean | 0.04 | 0.1 | 0.94 | |
| Dp Mean | −0.4 | −0.5 | 0.63 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fusco, R.; Granata, V.; Sansone, M.; Grimm, R.; Delrio, P.; Rega, D.; Tatangelo, F.; Avallone, A.; Raiano, N.; Totaro, G.; et al. Intravoxel Incoherent Motion Model of Diffusion Weighted Imaging and Diffusion Kurtosis Imaging in Differentiating of Local Colorectal Cancer Recurrence from Scar/Fibrosis Tissue by Multivariate Logistic Regression Analysis. Appl. Sci. 2020, 10, 8609. https://doi.org/10.3390/app10238609
Fusco R, Granata V, Sansone M, Grimm R, Delrio P, Rega D, Tatangelo F, Avallone A, Raiano N, Totaro G, et al. Intravoxel Incoherent Motion Model of Diffusion Weighted Imaging and Diffusion Kurtosis Imaging in Differentiating of Local Colorectal Cancer Recurrence from Scar/Fibrosis Tissue by Multivariate Logistic Regression Analysis. Applied Sciences. 2020; 10(23):8609. https://doi.org/10.3390/app10238609
Chicago/Turabian StyleFusco, Roberta, Vincenza Granata, Mario Sansone, Robert Grimm, Paolo Delrio, Daniela Rega, Fabiana Tatangelo, Antonio Avallone, Nicola Raiano, Giuseppe Totaro, and et al. 2020. "Intravoxel Incoherent Motion Model of Diffusion Weighted Imaging and Diffusion Kurtosis Imaging in Differentiating of Local Colorectal Cancer Recurrence from Scar/Fibrosis Tissue by Multivariate Logistic Regression Analysis" Applied Sciences 10, no. 23: 8609. https://doi.org/10.3390/app10238609
APA StyleFusco, R., Granata, V., Sansone, M., Grimm, R., Delrio, P., Rega, D., Tatangelo, F., Avallone, A., Raiano, N., Totaro, G., Cerciello, V., Pecori, B., & Petrillo, A. (2020). Intravoxel Incoherent Motion Model of Diffusion Weighted Imaging and Diffusion Kurtosis Imaging in Differentiating of Local Colorectal Cancer Recurrence from Scar/Fibrosis Tissue by Multivariate Logistic Regression Analysis. Applied Sciences, 10(23), 8609. https://doi.org/10.3390/app10238609






