Wearable Sensors Technology as a Tool for Discriminating Frailty Levels During Instrumented Gait Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Assessment of Frailty Criteria
2.4. Physical Performance Tests
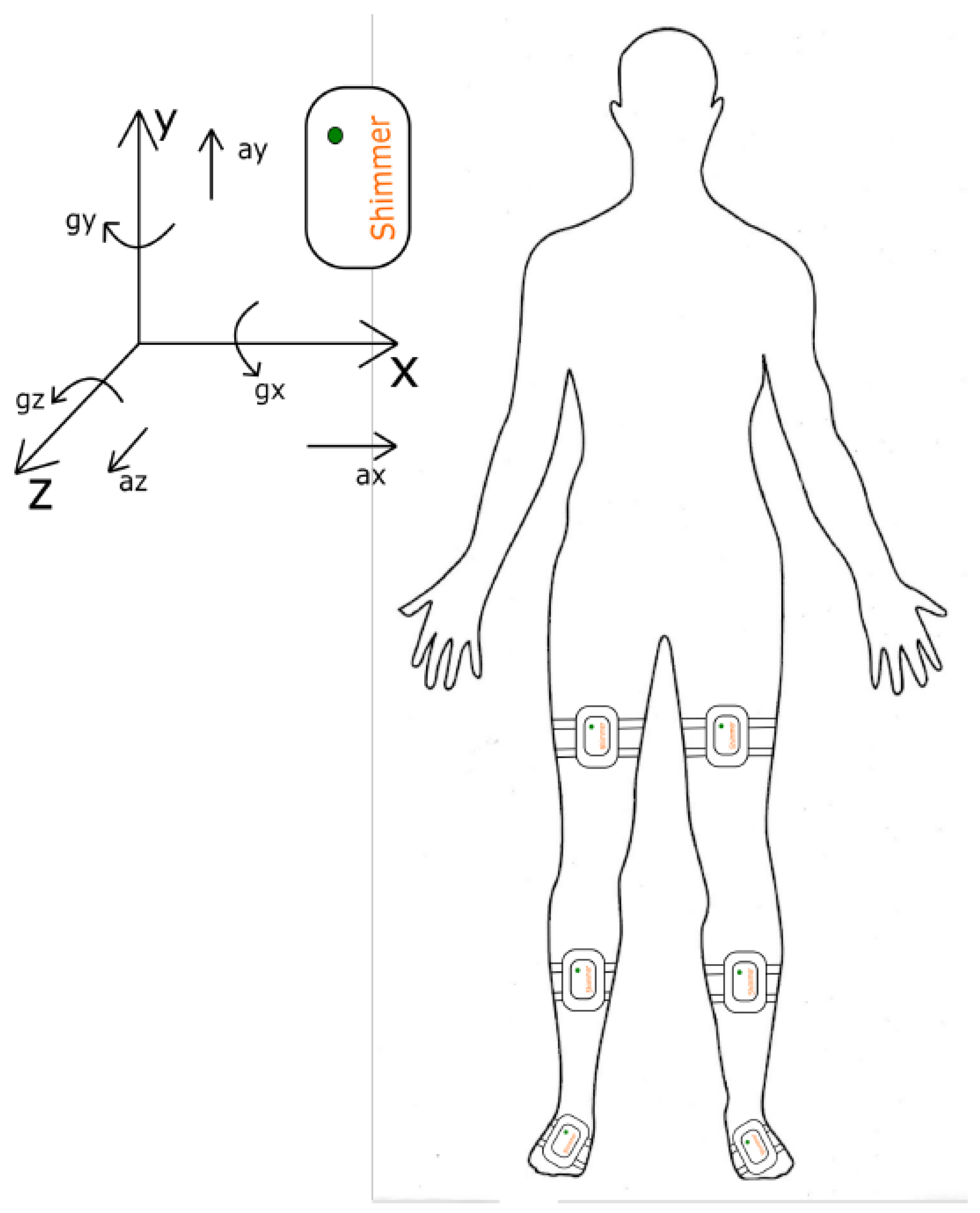
2.5. Sensor-Based Assessment of Gait
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- O’Caoimh, R.; Galluzzo, L.; Rodríguez-Laso, Á.; Van Der Heyden, J.; Ranhoff, A.H.; Lamprini-Koula, M.; Ciutan, M.; Samaniego, L.L.; Carcaillon-Bentata, L.; Kennelly, S.; et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: A systematic review and meta-analysis. Ann. Dell’Istituto Super. Sanita 2018. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2001, 56. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Mitnitski, A. Frailty in relation to the accumulation of deficits. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2007. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.M.; Gahbauer, E.A.; Allore, H.G.; Han, L. Transitions between frailty states among community-living older persons. Arch. Intern. Med. 2006. [Google Scholar] [CrossRef]
- Lang, P.O.; Michel, J.P.; Zekry, D. Frailty syndrome: A transitional state in a dynamic process. Gerontology 2009, 55, 539–549. [Google Scholar] [CrossRef]
- Woo, J. Designing fit for purpose health and social services for ageing populations. Int. J. Environ. Res. Public Health 2017, 14, 457. [Google Scholar] [CrossRef]
- Rodríguez Mañas, L.; García-Sánchez, I.; Hendry, A.; Bernabei, R.; Roller-Wirnsberger, R.; Gabrovec, B.; Liew, A.; Carriazo, A.M.; Redon, J.; Galluzzo, L.; et al. Key Messages for a Frailty Prevention and Management Policy in Europe from the Advantage Joint Action Consortium. J. Nutr. Health Aging 2018. [Google Scholar] [CrossRef]
- Dent, E.; Lien, C.; Lim, W.S.; Wong, W.C.; Wong, C.H.; Ng, T.P.; Woo, J.; Dong, B.; de la Vega, S.; Hua Poi, P.J.; et al. The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty. J. Am. Med. Dir. Assoc. 2017. [Google Scholar] [CrossRef]
- Da Câmara, S.M.A.; Alvarado, B.E.; Guralnik, J.M.; Guerra, R.O.; Maciel, Á.C.C. Using the Short Physical Performance Battery to screen for frailty in young-old adults with distinct socioeconomic conditions. Geriatr. Gerontol. Int. 2013. [Google Scholar] [CrossRef]
- Kiely, D.K.; Cupples, L.A.; Lipsitz, L.A. Validation and comparison of two frailty indexes: The MOBILIZE Boston study. J. Am. Geriatr. Soc. 2009. [Google Scholar] [CrossRef]
- Melzer, D.; Lan, T.Y.; Tom, B.D.; Deeg, D.J.; Guralnik, J.M. Variation in thresholds for reporting mobility disability between national population subgroups and studies. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2004. [Google Scholar] [CrossRef]
- Tudor-Locke, C.E.; Myers, A.M. Challenges and opportunities for measuring physical activity in sedentary adults. Sport. Med. 2001. [Google Scholar] [CrossRef] [PubMed]
- Rothman, M.D.; Leo-Summers, L.; Gill, T.M. Prognostic significance of potential frailty criteria. J. Am. Geriatr. Soc. 2008, 56, 2211–2216. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.; Patel, T.; Costa, A.; Bryce, E.; Hillier, L.M.; Slonim, K.; Hunter, S.W.; Heckman, G.; Molnar, F. Screening for frailty in primary care Accuracy of gait speed and hand-grip strength. Can. Fam. Physician 2017, 63, e51–e57. [Google Scholar] [PubMed]
- Schwenk, M.; Howe, C.; Saleh, A.; Mohler, J.; Grewal, G.; Armstrong, D.; Najafi, B. Frailty and technology: A systematic review of gait analysis in those with frailty. Gerontology 2013, 60, 79–89. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Muir, S.W.; Hall, M.; Doherty, T.J.; Kloseck, M.; Beauchet, O.; Speechley, M. Gait variability is associated with frailty in community-dwelling older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011. [Google Scholar] [CrossRef]
- Beauchet, O.; Dubost, V.; Herrmann, F.; Rabilloud, M.; Gonthier, R.; Kressig, R.W. Relationship between dual-task related gait changes and intrinsic risk factors for falls among transitional frail older adults. Aging Clin. Exp. Res. 2005. [Google Scholar] [CrossRef]
- Kressig, R.W.; Gregor, R.J.; Oliver, A.; Waddell, D.; Smith, W.; O’Grady, M.; Curns, A.T.; Kutner, M.; Wolf, S.L. Temporal and spatial features of gait in older adults transitioning to frailty. Gait Posture 2004. [Google Scholar] [CrossRef]
- Verghese, J.; Holtzer, R.; Lipton, R.B.; Wang, C. Mobility stress test approach to predicting frailty, disability, and mortality in high-functioning older adults. J. Am. Geriatr. Soc. 2012. [Google Scholar] [CrossRef]
- Schwenk, M.; Mohler, J.; Wendel, C.; D’Huyvetter, K.; Fain, M.; Taylor-Piliae, R.; Najafi, B. Wearable sensor-based in-home assessment of gait, balance, and physical activity for discrimination of frailty status: Baseline results of the Arizona frailty cohort study. Gerontology 2015. [Google Scholar] [CrossRef]
- Pradeep Kumar, D.; Toosizadeh, N.; Mohler, J.; Ehsani, H.; Mannier, C.; Laksari, K. Sensor-based characterization of daily walking: A new paradigm in pre-frailty/frailty assessment. BMC Geriatr. 2020. [Google Scholar] [CrossRef]
- Dasenbrock, L.; Heinks, A.; Schwenk, M.; Bauer, J.M. Technology-based measurements for screening, monitoring and preventing frailty. Z. Gerontol. Geriatr. 2016. [Google Scholar] [CrossRef]
- Thiede, R.; Toosizadeh, N.; Mills, J.L.; Zaky, M.; Mohler, J.; Najafi, B. Gait and balance assessments as early indicators of frailty in patients with known peripheral artery disease. Clin. Biomech. 2016, 32, 1–7. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- General Assembly of the World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 2014, 81, 14–18. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Kempen, G.I.; Yardley, L.; Van Haastregt, J.C.; Zijlstra, G.A.; Beyer, N.; Hauer, K.; Todd, C. The Short FES-I: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2008, 37, 45–50. [Google Scholar] [CrossRef]
- Orme, J.G.; Reis, J.; Herz, E.J. Factorial and discriminant validity of the center for epidemiological studies depression (CES-D) scale. J. Clin. Psychol. 1986, 42, 28–33. [Google Scholar] [CrossRef]
- Washburn, R.A.; Smith, K.W.; Jette, A.M.; Janney, C.A. The physical activity scale for the elderly (PASE): Development and evaluation. J. Clin. Epidemiol. 1993, 46, 153–162. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Savva, G.; Donoghue, O.; Horgan, F.; O’Regan, C.; Cronin, H.; Kenny, R.A. Timed-up-and-go and walking speed can identify frail members of the older population. J. Gerontol. A-Biol. 2013, 441–446. [Google Scholar] [CrossRef]
- Vander Linden, D.W. Shumway-Cook A, Wollacott MH. Motor Control: Theory and Practical Applications. Baltimore, Md; Neurology Report; Williams and Wilkins Inc.: Philadelphia, PA, USA, 1996. [Google Scholar] [CrossRef]
- Apóstolo, J.; Cooke, R.; Bobrowicz-Campos, E.; Santana, S.; Marcucci, M.; Cano, A.; Vollenbroek-Hutten, M.; Germini, F.; Holland, C. Predicting risk and outcomes for frail older adults: An umbrella review of frailty screening tools. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 1154. [Google Scholar] [CrossRef]
- Maggio, M.; Ceda, G.P.; Ticinesi, A.; De Vita, F.; Gelmini, G.; Costantino, C.; Meschi, T.; Kressig, R.W.; Cesari, M.; Fabi, M.; et al. Instrumental and non-instrumental evaluation of 4-m walking speed in older individuals. PLoS ONE 2016, 11. [Google Scholar] [CrossRef]
- Greene, B.R.; McGrath, D.; O’Neill, R.; O’Donovan, K.J.; Burns, A.; Caulfield, B. An adaptive gyroscope-based algorithm for temporal gait analysis. Med. Biol. Eng. Comput. 2010. [Google Scholar] [CrossRef]
- Aminian, K.; Najafi, B.; Büla, C.; Leyvraz, P.F.; Robert, P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J. Biomech. 2002. [Google Scholar] [CrossRef]
- Rueterbories, J.; Spaich, E.G.; Andersen, O.K. Gait event detection for use in FES rehabilitation by radial and tangential foot accelerations. Med. Eng. Phys. 2014. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 1988. [Google Scholar] [CrossRef]
- Böhning, D. Multinomial logistic regression algorithm. Ann. Inst. Stat. Math. 1992. [Google Scholar] [CrossRef]
| Characteristic * | Total Sample (n = 133) | Robust (n = 30) | Prefrail (n = 66) | Frail (n = 37) | p Value (F) Partial | p Value 95% CI [LL UL] | ||
|---|---|---|---|---|---|---|---|---|
| R vs. P | P vs. F | R vs. F | ||||||
| Age, mean (±SD) | 75.1 ± 8 [73.71 76.46] | 73 ± 6.3 [70.69 75.38] | 73.9 ± 8.5 [71.78 75.94] | 78.9 ± 7.3 [76.48 81.36] | 0.002 (6.467) 0.09 | 1.000 [−5.15 −3.93] | 0.006 [−8.97 −1.14] | 0.020 [−10.7 −0.68] |
| BMI, mean (±SD) | 27.6 ± 5.8 [26.6 28.6] | 28.9 ± 5.6 [26.8 30.9] | 27.7 ± 5.7 [26.3 29.1] | 26.5 ± 6.1 [24.4 28.5] | 0.244 (1.425) 0.021 | 1.000 [−2.07 4.71] | 0.900 [−1.67 4.18] | 0.289 [−1.16 6.30] |
| RCC, cm, mean (±SD) | 35.1 ± 69.2 [339 362] | 38.3 ± 38.4 [369 397] | 34.3 ± 84.5 [322 364] | 33.7 ± 47.4 [321 353] | 0.012 (4.596) 0.067 | 0.071 [−2.39 83.2] | 1.000 [−22.7 51.8] | 0.017 [7.64 102.3] |
| Number of comorbidities, mean (±SD) | 3.1 ± 1.7 [2.81 3.44] | 2.9 ± 2 [1.71 4.01] | 3 ± 1.6 [2.56 3.35] | 3.5 ± 1.8 [2.94 4.14] | 0.210 (1.580) 0.027 | 1.000 [−1.67 1.63] | 0.150 [−1.64 0.17] | 0.865 [−2.48 0.97] |
| Number of medications, mean (±SD) | 3.4 ± 2.4 [3 3.89] | 3.7 ± 2.1 [2.49 4.94] | 3 ± 2.2 [2.48 3.55] | 4.1 ± 2.8 [3.18 5.05] | 0.078 (2.604) 0.044 | 1.000 [−1.77 3.36] | 0.050 [−2.72 0.00] | 1.000 [−3.23 2.10] |
| MMSE score, mean (±SD) | 27.5 ± 2.2 [27.1 27.8] | 28.1 ± 1.9 [27.3 28.8] | 27.6 ± 1.8 [27.2 28.1] | 26.6 ± 2.6 [25.8 27.5] | 0.068 (2.752) 0.061 | 1.000 [−1.25 1.18] | 0.078 [−0.08 2.02] | 0.277 [−0.40 2.27] |
| PASE score, mean (±SD) | 97.9 ± 52.7 [88.8 107] | 109.9 ± 31.3 [98.2 122] | 106.6 ± 61 [91.5 122] | 72.9 ± 42.3 [58.8 87] | 0.002 (6.312 ) 0.061 | 1.000 [−29.10 30.97] | 0.006 [7.81 59.60] | 0.036 [1.68 67.59] |
| FES-I score, mean (±SD) | 22 ± 7.4 [20.7 23.36] | 17.6 ± 3.3 [16.4 18.9] | 23.3 ± 7.3 [21.4 25.1] | 23.5 ± 8.7 [20.5 26.4] | 0.001 (7.519) 0.106 | 0.002 [−10.50 −1.99] | 1.000 [−4.28 3.21] | 0.002 [−11.53 −2.03] |
| Gender and Falls History | Total Sample (n = 133) | Robust (n = 30) | Prefrail (n = 66) | Frail (n = 37) | p Value |
|---|---|---|---|---|---|
| Women, n (%) | 86 (67.7) | 20 (83.3) | 41 (62.1) | 25 (67.6) | 0.16 |
| History of falls in the last 12 months, n (%) | 60 (47.6) | 5 (20.8) | 33 (50.8) | 22 (59.5) | 0.01 |
| History of falls in the last 3 months, n (%) | 28 (22.2) | 3 (12.5) | 13 (20.0) | 12 (32.4) | 0.155 |
| Reported fear of falling, n (%) | 73 (56.2) | 9 (9.0) | 43 (66.2) | 21 (60.0) | 0.004 |
| Frailty criteria, n (%) Slow gait velocity Low physical activity Low hand grip Weight loss Exhaustion | 89 (70.1) | 0 | 54 (81.8) | 35 (94.6) | <0.001 |
| 39 (30.7) | 0 | 22 (33.3) | 17 (45.9) | 0.001 | |
| 26 (20.5) | 0 | 4 (6.1) | 22 (59.5) | <0.001 | |
| 25 (19.7) | 0 | 4 (6.1) | 21 (56.8) | <0.001 | |
| 52 (40.9) | 0 | 19 (28.8) | 33 (89.2) | <0.001 |
| Variable | Total Sample (n = 133) | Robust (n = 30) | Prefrail (n = 66) | Frail (n = 37) | p Value (F) | Partial | p Value 95% CI [LL UL] | ||
|---|---|---|---|---|---|---|---|---|---|
| R vs. P | P vs. F | R vs. F | |||||||
| TUG, s | 12.34 ± 5.03 | 7.68 ± 1.86 | 12.71 ± 4.56 | 15.56 ± 4.87 | <0.001 (29.195) | 0.238 | <0.001 [−7.23 −2.84] | 0.004 [2.84 7.23] | <0.001 [−10.3 −5.41] |
| DGI, score | 16.25 ± 4.04 | 18.90 ± 3.63 | 16.12 ± 3.52 | 14.32 ± 4.15 | <0.001 (12.547) | 0.139 | 0.003 [0.83 4.73] | 0.053 [−0.02 3.61] | <0.001 [2.4 6.75] |
| Gait speed, m/s | 0.68 ± 0.22 | 0.98 ± 0.17 | 0.63 ± 0.13 | 0.52 ± 0.13 | <0.001 (96.334) | 0.374 | <0.001 [0.275 0.42] | <0.001 [0.045 0.18] | <0.001 [0.38 0.54] |
| Stride time, s | 1.31 ± 0.24 | 1.06 ± 0.16 | 1.35 ± 0.16 | 1.46 ± 0.25 | <0.001 (39.415) | 0.274 | <0.001 [−0.38 −0.19] | 0.010 [−0.206 −0.023] | <0.001 [−0.51 −0.29] |
| Swing time, s | 0.49 ± 0.08 | 0.44 ± 0.06 | 0.51 ± 0.08 | 0.50 ± 0.09 | <0.001 (8.562) | 0.104 | <0.001 [−0.109 −0.028] | 0.92 [−0.033 0.043] | 0.003 [−0.108 −0.018] |
| Stance time, s | 0.83 ± 0.19 | 0.63 ± 0.11 | 0.84 ± 0.13 | 0.96 ± 0.21 | <0.001 (41.763) | 0.281 | <0.001 [−0.29 −0.14] | 0.001 [−0.19 −0.05] | <0.001 [−0.42 −0.25] |
| Swing phase,% | 37.58 ± 4.97 | 41.29 ± 3.35 | 37.59 ± 4.40 | 34.53 ± 5.05 | <0.001 (19.685) | 0.189 | 0.001 [1.41 5.99] | 0.003 [0.93 5.2] | <0.001 [4.21 9.32] |
| Stance phase,% | 62.42 ± 4.97 | 58.71 ± 3.35 | 62.40 ± 4.40 | 65.47 ± 5.05 | <0.001 (19.685) | 0.189 | 0.001 0.90 [−5.99 −1.41] | 0.003 0.66 [−5.2 −0.93] | <0.001 1.55 [−9.32 −4.21] |
| DS time, s | 0.15 ± 0.08 | 0.08 ± 0.04 | 0.15 ± 0.07 | 0.20 ± 0.09 | <0.001 (27.098) | 0.227 | <0.001 [−0.106 −0.033] | <0.001 [−0.09 −0.023] | <0.001 [−0.17 −0.085] |
| Cad., step/min | 95.38 ± 17.29 | 117.17 ± 13.18 | 91.35 ± 11.92 | 84.89 ± 12.71 | <0.001 (62.697) | 0.329 | <0.001 [19.32 32.3] | 0.033 [0.41 12.52] | <0.001 [25.04 39.52] |
| Variable * | Prefrail vs. Robust | Frail vs. Robust | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| TUG time, s | 2.36 | 1.68–3.31 | <0.001 | 2.67 | 1.89–3.78 | <0.001 |
| Dynamic gait index, score | 0.80 | 0.70–0.92 | 0.001 | 0.71 | 0.60–0.83 | <0.001 |
| Gait speed, cm/s | 0.93 | 0.90–0.95 | <0.001 | 0.92 | 0.89–0.95 | <0.001 |
| Stride time, ms | 1.006 | 1.003–1.009 | <0.001 | 1.006 | 1.003–1.009 | <0.001 |
| Swing phase time, ms | 1.007 | 1.001–1.013 | 0.028 | 1.008 | 1.001–1.015 | 0.024 |
| Stance phase time, ms | 1.009 | 1.005–1.013 | <0.001 | 1.008 | 1.004–1.012 | <0.001 |
| Swing phase,% | 0.80 | 0.71–0.91 | 0.001 | 0.69 | 0.60–0.90 | <0.001 |
| Stance phase,% | 1.24 | 1.10–1.41 | 0.001 | 1.44 | 1.25–1.67 | <0.001 |
| Double support time, ms | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 1.01–1.02 | 0.002 |
| Cadence, steps per min | 0.87 | 0.83–0.92 | <0.001 | 0.83 | 0.78–0.89 | <0.001 |
| Variables * | Frail vs. Prefrail or Robust | Prefrail or Frail vs. Robust | ||||||
|---|---|---|---|---|---|---|---|---|
| AUC | Cut-Off Value | Sens. (%) | Spec. (%) | AUC | Cut-Off Value | Sens. (%) | Spec. (%) | |
| TUG test time, s | 0.790 | 11.60 | 86.1 | 65.6 | 0.929 | 9.27 | 89.2 | 86.7 |
| DGI, score | 0.675 | 15.00 | 54.1 | 75.0 | 0.735 | 19.0 | 73.8 | 56.7 |
| Ch. gait speed, m/s | 0.801 | 0.59 | 83.8 | 68.8 | 0.969 | 0.74 | 91.3 | 90.0 |
| S. gait speed, m/s | 0.810 | 0.60 | 78.4 | 75.0 | 0.958 | 0.82 | 94.2 | 86.7 |
| Stride time, s | 0.740 | 1.27 | 91.9 | 51.0 | 0.915 | 1.19 | 90.3 | 86.7 |
| Stance time, s | 0.773 | 0.80 | 83.8 | 62.5 | 0.923 | 0.68 | 96.1 | 73.3 |
| Swing time, s | 0.569 | 0.48 | 59.5 | 57.3 | 0.759 | 0.48 | 58.3 | 86.7 |
| Stance phase,% | 0.749 | 63.15 | 75.7 | 68.8 | 0.788 | 63.27 | 53.4 | 96.7 |
| Swing phase,% | 0.749 | 36.85 | 75.7 | 68.8 | 0.790 | 36.73 | 53.4 | 96.7 |
| DS time, s | 0.778 | 0.16 | 70.3 | 76.0 | 0.858 | 0.14 | 62.1 | 96.7 |
| Cad., step/min | 0.724 | 99.54 | 94.6 | 44.8 | 0.930 | 101.22 | 84.4 | 90.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Apsega, A.; Petrauskas, L.; Alekna, V.; Daunoraviciene, K.; Sevcenko, V.; Mastaviciute, A.; Vitkus, D.; Tamulaitiene, M.; Griskevicius, J. Wearable Sensors Technology as a Tool for Discriminating Frailty Levels During Instrumented Gait Analysis. Appl. Sci. 2020, 10, 8451. https://doi.org/10.3390/app10238451
Apsega A, Petrauskas L, Alekna V, Daunoraviciene K, Sevcenko V, Mastaviciute A, Vitkus D, Tamulaitiene M, Griskevicius J. Wearable Sensors Technology as a Tool for Discriminating Frailty Levels During Instrumented Gait Analysis. Applied Sciences. 2020; 10(23):8451. https://doi.org/10.3390/app10238451
Chicago/Turabian StyleApsega, Andrius, Liudvikas Petrauskas, Vidmantas Alekna, Kristina Daunoraviciene, Viktorija Sevcenko, Asta Mastaviciute, Dovydas Vitkus, Marija Tamulaitiene, and Julius Griskevicius. 2020. "Wearable Sensors Technology as a Tool for Discriminating Frailty Levels During Instrumented Gait Analysis" Applied Sciences 10, no. 23: 8451. https://doi.org/10.3390/app10238451
APA StyleApsega, A., Petrauskas, L., Alekna, V., Daunoraviciene, K., Sevcenko, V., Mastaviciute, A., Vitkus, D., Tamulaitiene, M., & Griskevicius, J. (2020). Wearable Sensors Technology as a Tool for Discriminating Frailty Levels During Instrumented Gait Analysis. Applied Sciences, 10(23), 8451. https://doi.org/10.3390/app10238451






