Development of a Mortality Risk Model in Elderly Hip Fracture Patients by Different Analytical Approaches
Abstract
1. Introduction
2. Subjects and Methods
2.1. Database
2.2. Study Population
2.3. Covariates
2.4. Statistical Analysis
2.5. Data Mining Learning Algorithms
2.6. Measures for Performance Evaluation
3. Empirical Results
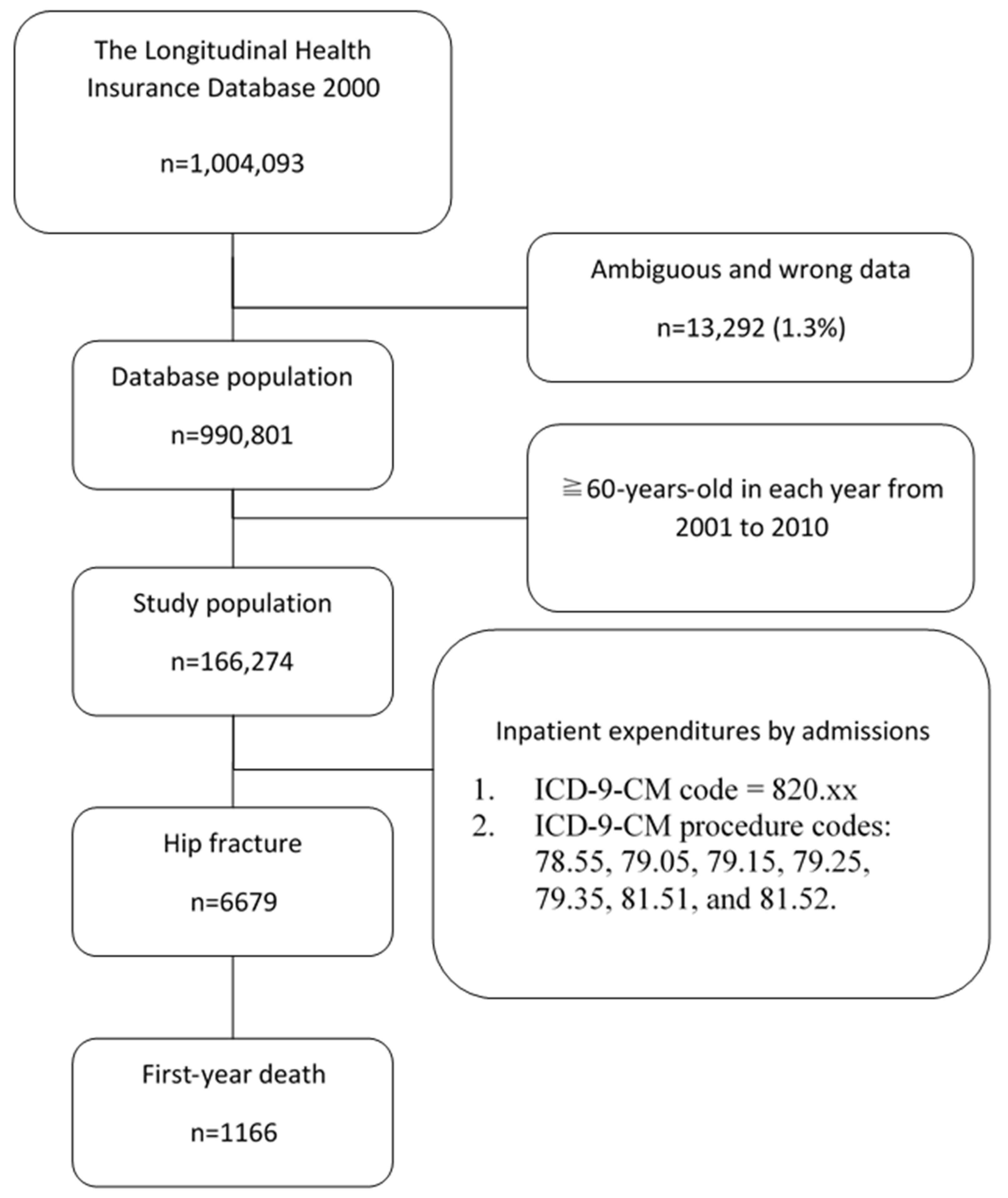
3.1. Patient Selection
3.2. Model Construction and Evaluation
4. Discussion
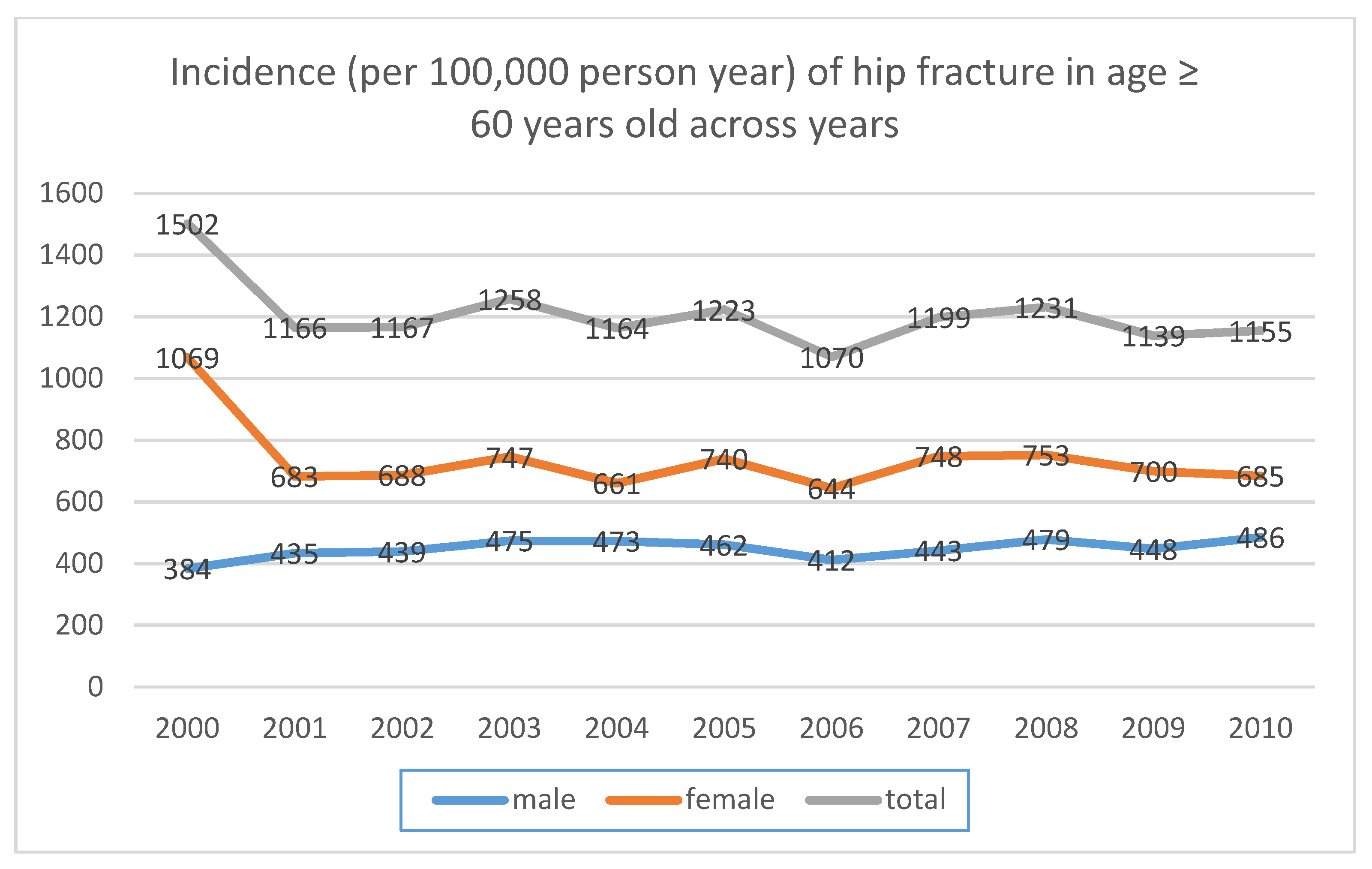
4.1. Incidence of Hip Fracture
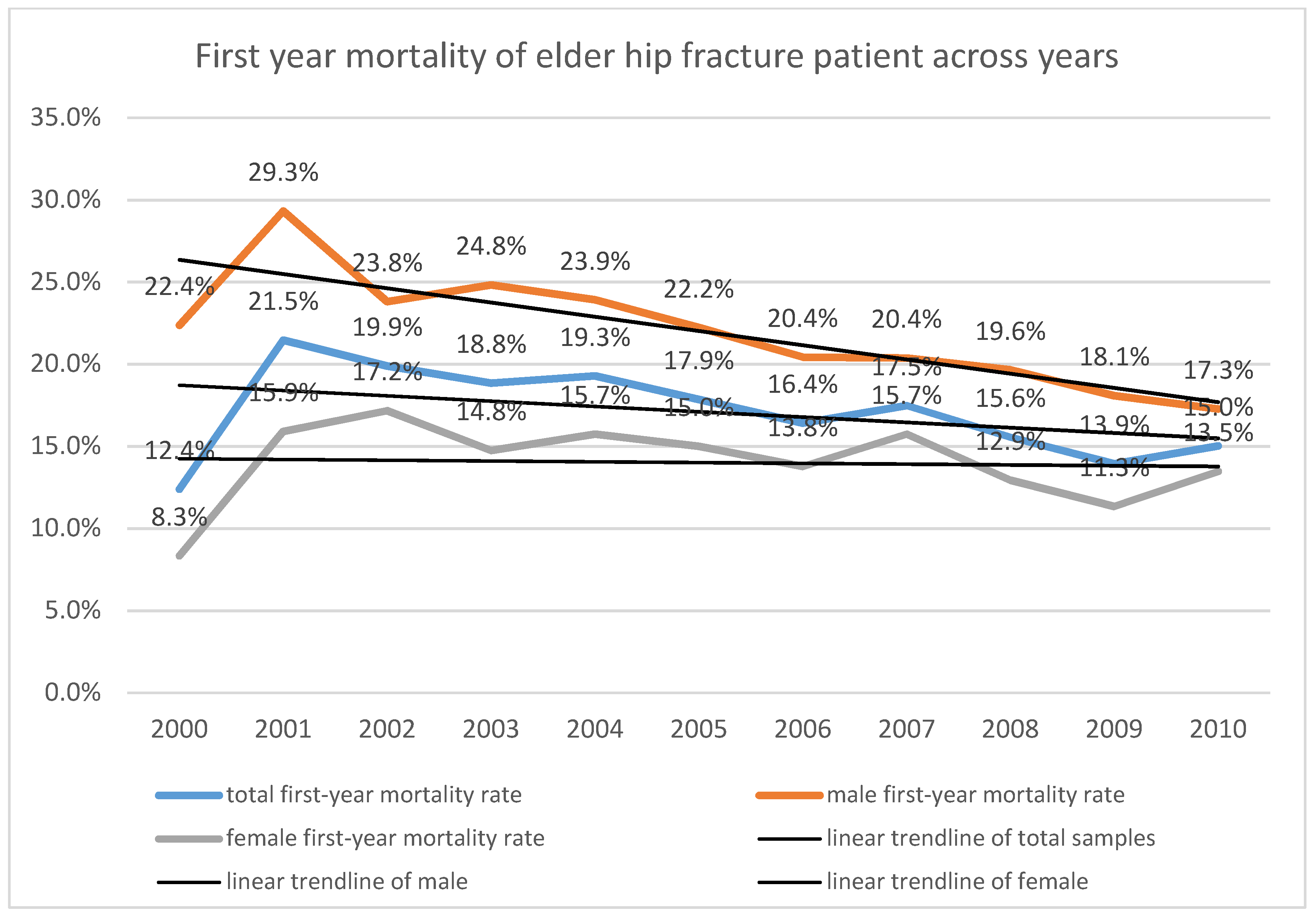
4.2. First-Year Mortality
4.3. Risk Factor of First-Year Mortality after Hip Fracture
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hasegawa, Y.; Suzuki, S.; Wingstrand, H. Risk of mortality following hip fracture in Japan. J. Orthop. Sci. 2007, 12, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Campion, G.; Melton, L., III. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Man, L.P.; Ho, A.W.; Wong, S.H. Excess mortality for operated geriatric hip fracture in Hong Kong. Hong Kong Med. J. 2016, 22, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Boufous, S.; Finch, C.F.; Lord, S.R. Incidence of hip fracture in New South Wales: Are our efforts having an effect? Med. J. Aust. 2004, 180, 623–626. [Google Scholar] [CrossRef]
- White, S.M.; Griffiths, R. Projected incidence of proximal femoral fracture in England: A report from the NHS Hip Fracture Anaesthesia Network (HIPFAN). Injury 2011, 42, 1230–1233. [Google Scholar] [CrossRef]
- Smith, T.; Pelpola, K.; Ball, M.; Ong, A.; Myint, P.K. Pre-operative indicators for mortality following hip fracture surgery: A systematic review and meta-analysis. Age Ageing 2014, 43, 464–471. [Google Scholar] [CrossRef]
- Castronuovo, E.; Pezzotti, P.; Franzo, A.; Di Lallo, D.; Guasticchi, G. Early and late mortality in elderly patients after hip fracture: A cohort study using administrative health databases in the Lazio region, Italy. BMC Geriatr. 2011, 11, 37. [Google Scholar] [CrossRef]
- Dhanwal, D.K.; Dennison, E.M.; Harvey, N.C.; Cooper, C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J. Orthop. 2011, 45, 15–22. [Google Scholar] [CrossRef]
- Hall, S.E.; Williams, J.A.; Senior, J.A.; Goldswain, P.R.T.; Criddle, R.A. Hip fracture outcomes: Quality of life and functional status in older adults living in the community. Aust. N. Z. J. Med. 2000, 30, 327–332. [Google Scholar] [CrossRef]
- Randell, A.G.; Nguyen, T.V.; Bhalerao, N.; Silverman, S.L.; Sambrook, P.N.; Eisman, J.A. Deterioration in quality of life following hip fracture: A prospective study. Osteoporos. Int. 2000, 11, 460–466. [Google Scholar] [CrossRef]
- Omsland, T.K.; Emaus, N.; Tell, G.S.; Magnus, J.H.; Ahmed, L.A.; Holvik, K.; Vestergaard, P. Mortality following the first hip fracture in Norwegian women and men (1999–2008). A NOREPOS study. Bone 2014, 63, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Schnell, S.; Friedman, S.M.; Mendelson, D.A.; Bingham, K.W.; Kates, S.L. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop. Surg. Rehabil. 2010, 1, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Brauer, C.A.; Coca-Perraillon, M.; Cutler, D.M.; Rosen, A.B. Incidence and mortality of hip fractures in the United States. JAMA 2009, 302, 1573–1579. [Google Scholar] [CrossRef] [PubMed]
- Haleem, S.; Lutchman, L.; Mayahi, R.; Grice, J.E.; Parker, M.J. Mortality following hip fracture: Trends and geographical variations over the last 40 years. Injury 2008, 39, 1157–1163. [Google Scholar] [CrossRef]
- Giversen, I.M. Time trends of mortality after first hip fractures. Osteoporos. Int. 2007, 18, 721–732. [Google Scholar] [CrossRef]
- Roberts, S.E.; Goldacre, M.J. Time trends and demography of mortality after fractured neck of femur in an English population, 1968–1998: Database study. BMJ 2003, 327, 771–775. [Google Scholar] [CrossRef]
- Wang, C.B.; Lin, C.F.; Liang, W.M.; Cheng, C.F.; Chang, Y.J.; Wu, H.C.; Leu, T.H. Excess mortality after hip fracture among the elderly in Taiwan: A nationwide population-based cohort study. Bone 2013, 56, 147–153. [Google Scholar] [CrossRef]
- Fisher, L.D.; Lin, D.Y. Time-dependent covariates in the Cox proportional hazards regression model. Annu. Rev. Public Health 1999, 20, 145–157. [Google Scholar] [CrossRef]
- Ohno, M.L. A comparison of Cox proportional hazards and artificial neural network models for medical prognosis. Comput. Biol. Med. 1997, 27, 55–65. [Google Scholar] [CrossRef]
- Bakker, B.; Heskes, T.; Neijt, J.; Kappen, B. Improving Cox survival analysis with a neural-Bayesian approach. Stat. Med. 2004, 23, 2989–3012. [Google Scholar] [CrossRef]
- Bakker, S.J. Crippling of inflammatory markers as predictors of death by dichotomization and multicollinearity. Nephrol. Dial. Transplant. 2006, 21, 2990–2991. [Google Scholar] [CrossRef] [PubMed]
- Fayyad, U.; Piatetsky, S.G.; Smyth, P. From Data Mining to Knowledge Discovery in Databases (a survey). AI Mag. 1996, 17, 37–54. [Google Scholar]
- Beretta, L.; Santaniello, A.; Cappiello, F.; Chawla, N.V.; Vonk, M.C.; Carreira, P.E.; Allanore, Y.; Popa-Diaconu, D.A.; Cossu, M.; Bertolotti, F.; et al. Development of a five-year mortality model in systemic sclerosis patients by different analytical approaches. Clin. Exp. Rheumatol. 2010, 28 (Suppl. 58), 18–27. [Google Scholar]
- Hsing, A.W.; Ioannidis, J.P. Nationwide Population Science: Lessons From the Taiwan National Health Insurance Research Database. JAMA Intern. Med. 2015, 175, 1527–1529. [Google Scholar] [CrossRef] [PubMed]
- The National Health Research Institutes. Data Subsets. Available online: Nhird.nhri.org.tw/en/Data_Subsets.html#S3 (accessed on 1 August 2020).
- Quinlan, J.R. C4. 5: Programs for Machine Learning; Morgan Kaufmann: San Francisco, CA, USA, 1993. [Google Scholar]
- Vapnik, V. The Nature of Statistical Learning Theory; Springer: New York, NY, USA, 1995. [Google Scholar]
- Rumelhart, D.E.; Hinton, G.E.; Williams, R.J. Learning representations by backpropagating errors. Nature 1986, 323, 533–536. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression; John Wiley & Sons: New York, NY, USA, 1989. [Google Scholar]
- Vuk, M.; Curk, T. ROC curve, Lift Chart and Calibration Plot. Metodološki Zvezki 2006, 3, 89–108. [Google Scholar]
- Tan, P.N.; Steinbach, M.; Kumar, V. Introduction to Data Mining; Addison Wesley: Boston, MA, USA, 2006; p. 769. [Google Scholar]
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide projections for hip fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef]
- Grigorie, D.; Sucaliuc, A.; Vladescu, C. Hip fracture epidemiology in Romania: Nationwide study 2005–2009. Osteoporos. Int. 2011, 22, S323. [Google Scholar]
- Williams, N.; Hardy, B.M.; Tarrant, S.; Enninghorst, N.; Attia, J.; Oldmeadow, C.; Balogh, Z.J. Changes in hip fracture incidence, mortality and length of stay over the last decade in an Australian major trauma centre. Arch. Osteoporos. 2013, 8, 150. [Google Scholar] [CrossRef]
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef]
- Lönnroos, E.; Kautiainen, H.; Karppi, P.; Huusko, T.; Hartikainen, S.; Kiviranta, I.; Sulkava, R. Increased incidence of hip fractures: A population based-study in Finland. Bone 2006, 39, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Melton, L.J., 3rd; Kearns, A.E.; Atkinson, E.J.; Bolander, M.E.; Achenbach, S.J.; Huddleston, J.M.; Leibson, C.L. Secular trends in hip fracture incidence and recurrence. Osteoporos. Int. 2009, 20, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Odén, A.; McCloskey, E.V.; Johansson, H.; Wahl, D.A.; Cooper, C. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos. Int. 2012, 2, 2239–2256. [Google Scholar] [CrossRef] [PubMed]
- Black, D.M.; Cooper, C. Epidemiology of fractures and assessment of fracture risk. Clin. Lab. Med. 2000, 20, 439–453. [Google Scholar] [CrossRef]
- Grigorie, D.; Sucaliuc, A.; Johansson, H.; Kanis, J.A.; McCloskey, E. Incidence of hip fracture in Romania and the development of a Romanian FRAX model. Calcif. Tissue Int. 2013, 92, 429–436. [Google Scholar] [CrossRef]
- Formiga, F.; Lopez-Soto, A.; Duaso, E.; Ruiz, D.; Chivite, D.; Perez-Castejon, J.M.; Pujol, R. Differences in the characteristics of elderly patients suffering from hip fracture due to falls according to place of residence. J. Am. Med. Dir. Assoc. 2007, 8, 533–537. [Google Scholar] [CrossRef]
- Jaller-Raad, J.J.; Jaller-Char, J.J.; Lechuga-Ortiz, J.A.; Navarro-Lechuga, E.; Johansson, H.; Kanis, J.A. Incidence of hip fracture in Barranquilla, Colombia, and the development of a Colombian FRAX model. Calcif. Tissue Int. 2013, 93, 15–22. [Google Scholar] [CrossRef]
- Doshi, H.K.; Ramason, R.; Azellarasi, J.; Naidu, G.; Chan, W.L.W. Orthogeriatric model for hip fracture patients in Singapore: Our early experience and initial outcomes. Arch. Orthop. Trauma Surg. 2014, 134, 351–357. [Google Scholar] [CrossRef]
- Ariza-Vega, P.; Kristensen, M.T.; Martín-Martín, L.; Jiménez-Moleón, J.J. Predictors of long-term mortality in older people with hip fracture. Arch. Phys. Med. Rehabil. 2015, 96, 1215–1221. [Google Scholar] [CrossRef]
- Endo, Y.; Aharonoff, G.B.; Zuckerman, J.D.; Egol, K.A.; Koval, K.J. Gender differences in patients with hip fracture: A greater risk of morbidity and mortality in men. J. Orthop. Trauma 2005, 19, 29–35. [Google Scholar] [CrossRef]
- Kannegaard, P.N.; van der Mark, S.; Eiken, P.; Abrahamsen, B.O. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 2010, 39, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Koh, G.C.; Tai, B.C.; Ang, L.W.; Heng, D.; Yuan, J.M.; Koh, W.P. All-cause and cause-specific mortality after hip fracture among Chinese women and men: The Singapore Chinese Health Study. Osteoporos. Int. 2013, 24, 1981–1989. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, S.J.; Goldberg, J.; Miles, T.P.; Brody, J.A.; Stiers, W.; Rimm, A.A. Race and sex differences in mortality following fracture of the hip. Am. J. Public Health 1992, 82, 1147–1150. [Google Scholar] [CrossRef] [PubMed]
- Alegre-López, J.; Cordero-Guevara, J.; Alonso-Valdivielso, J.L.; Fernández-Melón, J. Factors associated with mortality and functional disability after hip fracture: An inception cohort study. Osteoporos. Int. 2005, 16, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Keaveny, T.M.; Kopperdahl, D.L.; Melton, L.J., 3rd. Age-dependence of femoral strength in white women and men. J. Bone Miner. Res. 2010, 25, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Hedlund, R.; Lindgren, U. Trauma type, age, and gender as determinants of hip fracture. J. Orthop. Res. 1987, 5, 242–246. [Google Scholar]
- Lin, W.P.; Wen, C.J.; Jiang, C.C.; Hou, S.M.; Chen, C.Y.; Lin, J. Risk factors for hip fracture sites and mortality in older adults. J. Trauma Acute Care Surg. 2011, 71, 191–197. [Google Scholar] [CrossRef]
- Gerdhem, P.; Ringsberg, K.; Akesson, K.; Obrant, K.J. Just one look, and fractures and death can be predicted in elderly ambulatory women. Gerontology 2004, 50, 309–314. [Google Scholar] [CrossRef]
- Valizadeh, M.; Mazloomzadeh, S.; Golmohammadi, S.; Larijani, B. Mortality after low trauma hip fracture: A prospective cohort study. BMC Musculoskelet. Disord. 2012, 13, 143. [Google Scholar] [CrossRef]
- Pugely, A.J.; Martin, C.T.; Gao, Y.; Klocke, N.F.; Callaghan, J.J.; Marsh, J.L. A risk calculator for short-term morbidity and mortality after hip fracture surgery. J. Orthop. Trauma 2014, 28, 63–69. [Google Scholar] [CrossRef]
- Lin, J.C.; Wu, C.C.; Lo, C.; Liang, W.M.; Cheng, C.F.; Wang, C.B.; Leu, T.H. Mortality and complications of hip fracture in young adults: A nationwide population-based cohort study. BMC Musculoskelet. Disord. 2014, 15, 362. [Google Scholar] [CrossRef]
- Ireland, A.W.; Kelly, P.J.; Cumming, R.G. Risk factor profiles for early and delayed mortality after hip fracture: Analyses of linked Australian Department of Veterans’ Affairs databases. Injury 2015, 46, 1028–1035. [Google Scholar] [CrossRef] [PubMed]
- Poor, G.; Atkinson, E.J.; O’fallon, W.M.; Melton, L.J., 3rd. Determinants of reduced survival following hip fractures in men. Clin. Orthop. Relat. Res. 1995, 260–265. [Google Scholar]
- Jou, H.J.; Siao, R.Y.; Tsai, Y.S.; Chen, Y.T.; Li, C.Y.; Chen, C.C. Postdischarge rehospitalization and in-hospital mortality among Taiwanese women with hip fracture. Taiwan J. Obstet. Gynecol. 2014, 53, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.J.; Handoll, H.H.; Bhargara, A. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst. Rev. 2000, Cd000337. [Google Scholar] [CrossRef]
- Jain, R.; Basinski, A.; Kreder, H.J. Nonoperative treatment of hip fractures. Int. Orthop. 2003, 27, 11–17. [Google Scholar] [CrossRef]
- Neuman, M.D.; Fleisher, L.A.; Even-Shoshan, O.; Mi, L.; Silber, J.H. Nonoperative care for hip fracture in the elderly: The influence of race, income, and comorbidities. Med. Care 2010, 48, 314–320. [Google Scholar] [CrossRef]

| Method | Parameters | Value Setting |
|---|---|---|
| C4.5 | Confidence factor | 0.25 |
| Minimum number of instances per leaf | 20 | |
| Random Forest | Number of trees | 10 |
| Number of attributes to be used in random selection | 4 | |
| Support Vector Machines | Kernel | PolyKernel |
| Multilayer Perceptron | Number of hidden nodes | 7 |
| Learning rate | 0.3 | |
| Momentum factor | 0.2 | |
| Maximum number of epochs | 500 |
| No. | % | |||||
|---|---|---|---|---|---|---|
| Gender | male | 509081 | 51.4 | |||
| female | 481720 | 48.6 | ||||
| total | 990801 | 100 | ||||
| mean | std. err | 95% C.I. | p value | |||
| Age | male | 34.20 | 0.03 | 34.14 | 34.25 | 0.5093 |
| female | 34.17 | 0.03 | 34.11 | 34.23 | ||
| total | 34.18 | 0.02 | 34.14 | 34.22 ioii | ||
| Year | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | Total | Trend p (* t-Test **) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All hip fractures | 759 | 601 | 613 | 674 | 638 | 683 | 603 | 692 | 733 | 703 | 739 | 7438 | |
| survival | 665 | 472 | 491 | 547 | 515 | 561 | 504 | 571 | 619 | 605 | 628 | 6178 | |
| death | 94 | 129 | 122 | 127 | 123 | 122 | 99 | 121 | 114 | 98 | 111 | 1260 | |
| First year mortality rate | 12.38% | 21.46% | 19.90% | 18.84% | 19.28% | 17.86% | 16.42% | 17.49% | 15.55% | 13.94% | 15.02% | 16.94% | 0.042 |
| Male hip fractures | 219 | 249 | 252 | 274 | 276 | 270 | 240 | 260 | 285 | 271 | 301 | 2678 | |
| survival | 170 | 176 | 192 | 206 | 210 | 210 | 191 | 207 | 229 | 222 | 249 | 2092 | |
| death | 49 | 73 | 60 | 68 | 66 | 60 | 49 | 53 | 56 | 49 | 52 | 586 | |
| First year mortality rate | 22.37% | 29.32% | 23.81% | 24.82% | 23.91% | 22.22% | 20.42% | 20.83% | 19.65% | 18.08% | 17.28% | 21.88% | 0.000 |
| Female hip fractures | 540 | 352 | 361 | 400 | 362 | 413 | 363 | 432 | 448 | 432 | 438 | 4541 | |
| survival | 495 | 296 | 299 | 341 | 305 | 351 | 313 | 364 | 390 | 383 | 379 | 3916 | |
| death | 45 | 56 | 62 | 59 | 57 | 62 | 50 | 68 | 58 | 49 | 59 | 580 | |
| First year mortality rate | 8.33% | 15.91% | 17.71% | 14.75% | 15.75% | 15.01% | 13.77% | 15.74% | 12.95% | 11.34% | 13.47%% | 12.77% | 0.769 |
| Ratio | Std. Err. | t | p Value | [95% Conf. | Interval] | |
|---|---|---|---|---|---|---|
| Entire study group | ||||||
| age | 0.005 | 0.000 | 19.46 | 0.000 | 0.004 | 0.005 |
| gender (male vs. female) | 0.075 | 0.008 | 9.61 | 0.000 | 0.060 | 0.090 |
| number of comorbidity | 0.004 | 0.006 | 0.69 | 0.488 | −0.008 | 0.016 |
| the year of fracture | −0.006 | 0.001 | −4.56 | 0.000 | −0.008 | −0.003 |
| surgical intervention (yes vs. no) | −1.554 | 0.122 | −12.74 | 0.000 | −0.179 | −0.132 |
| Male group | ||||||
| age | 0.005 | 0.000 | 15.75 | 0.000 | 0.005 | 0.006 |
| number of comorbidity | 0.007 | 0.010 | 0.68 | 0.497 | −0.013 | −0.027 |
| the year of fracture | −0.009 | 0.002 | −4.59 | 0.000 | −0.125 | −0.005 |
| surgical intervention | −0.141 | −0.019 | −7.34 | 0.000 | −0.178 | −0.103 |
| Female group | ||||||
| age | 0.004 | 0.000 | 10.66 | 0.000 | 0.003 | 0.005 |
| number of comorbidity | 0.002 | 0.007 | 0.23 | 0.822 | −0.012 | 0.016 |
| The year of fracture | −0.003 | 0.002 | −1.82 | 0.069 | −0.006 | 0.000 |
| surgical intervention | −0.170 | 0.016 | −10.83 | 0.000 | −0.201 | −0.139 |
| Logistic Regression Analysis | Cox PH Regression Analysis | ||||||
|---|---|---|---|---|---|---|---|
| Features | OR | 95% CI | p | Features | HR | 95% CI | p |
| Gender | 0.59 | 0.536–0.649 | Gender | 1.455 | 1.375–1.539 | ||
| Age | 0.932 | 0.926–0.937 | Age | 1.047 | 1.044–1.051 | ||
| Surgical intervention | 1.763 | 1.523–2.040 | Surgical intervention | 0.682 | 0.631–0.736 | ||
| Comorbidity | Comorbidity | ||||||
| DM | 0.678 | 0.603–0.762 | DM | 1.237 | 1.154–1.327 | ||
| CV | 1.339 | 1.214–1.476 | CV | 0.876 | 0.825–0.930 | ||
| CVA | 1.047 | 0.487–2.252 | 0.905 | CVA | 0.985 | 0.640–1.514 | 0.944 |
| RENAL | 0.159 | 0.071–0.355 | RENAL | 2.911 | 2.267–3.738 | ||
| Model | Sensitivity | Specificity | Accuracy | AUC |
|---|---|---|---|---|
| C4.5 | 0.674 | 0.672 | 0.674 | 0.723 |
| Random Forest | 0.725 | 0.731 | 0.724 | 0.790 |
| SVM | 0.637 | 0.636 | 0.636 | 0.637 |
| MLP | 0.626 | 0.639 | 0.620 | 0.674 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo, C.-L.; Yang, Y.-H.; Hsu, C.-J.; Chen, C.-Y.; Huang, W.-C.; Tang, P.-L.; Renn, J.-H. Development of a Mortality Risk Model in Elderly Hip Fracture Patients by Different Analytical Approaches. Appl. Sci. 2020, 10, 6787. https://doi.org/10.3390/app10196787
Lo C-L, Yang Y-H, Hsu C-J, Chen C-Y, Huang W-C, Tang P-L, Renn J-H. Development of a Mortality Risk Model in Elderly Hip Fracture Patients by Different Analytical Approaches. Applied Sciences. 2020; 10(19):6787. https://doi.org/10.3390/app10196787
Chicago/Turabian StyleLo, Chia-Lun, Ya-Hui Yang, Chien-Jen Hsu, Chun-Yu Chen, Wei-Chun Huang, Pei-Ling Tang, and Jenn-Huei Renn. 2020. "Development of a Mortality Risk Model in Elderly Hip Fracture Patients by Different Analytical Approaches" Applied Sciences 10, no. 19: 6787. https://doi.org/10.3390/app10196787
APA StyleLo, C.-L., Yang, Y.-H., Hsu, C.-J., Chen, C.-Y., Huang, W.-C., Tang, P.-L., & Renn, J.-H. (2020). Development of a Mortality Risk Model in Elderly Hip Fracture Patients by Different Analytical Approaches. Applied Sciences, 10(19), 6787. https://doi.org/10.3390/app10196787







