Development of a Mobile Personal Health Record Application Designed for Emergency Care in Korea; Integrated Information from Multicenter Electronic Medical Records
Abstract
1. Introduction
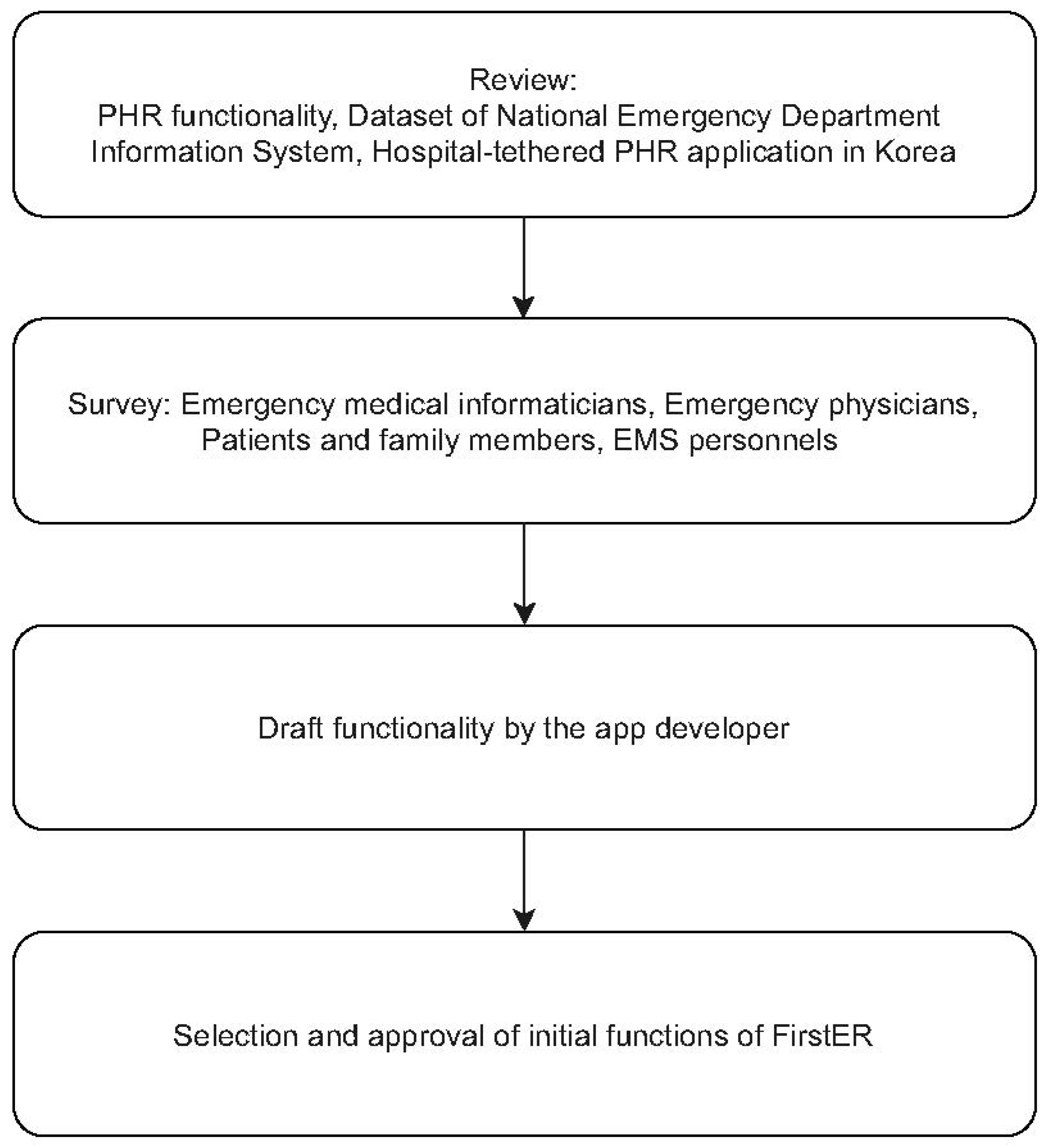
2. Methods
2.1. Design of the mPHR Service for Emergency Situations
2.1.1. Functions and Input Data That Were Considered Necessary
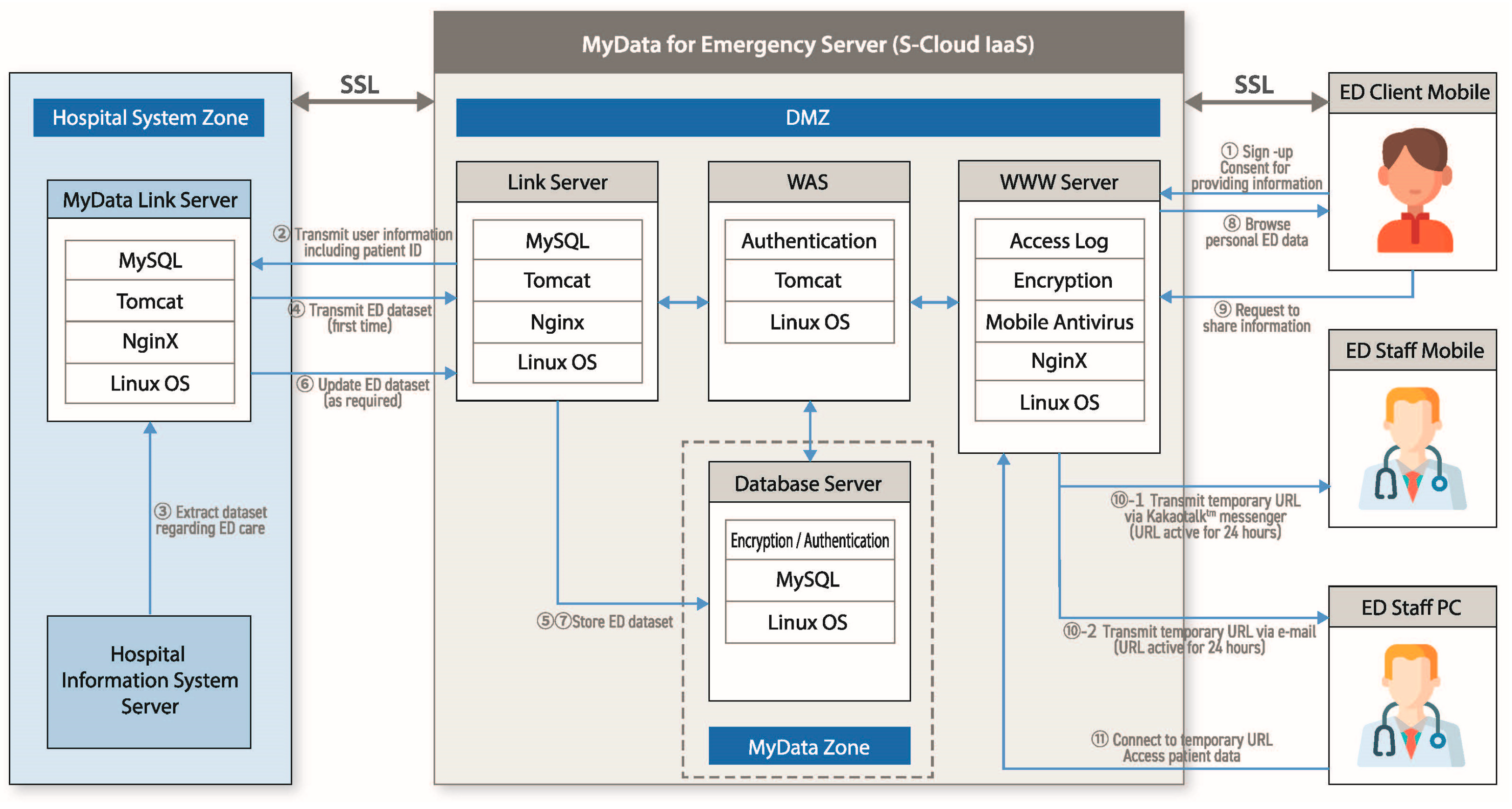
2.1.2. Development of the System and Server
2.2. Development of the Prototype
2.3. Development of the mPHR Application
2.4. Testing the New mPHR Application
3. Results
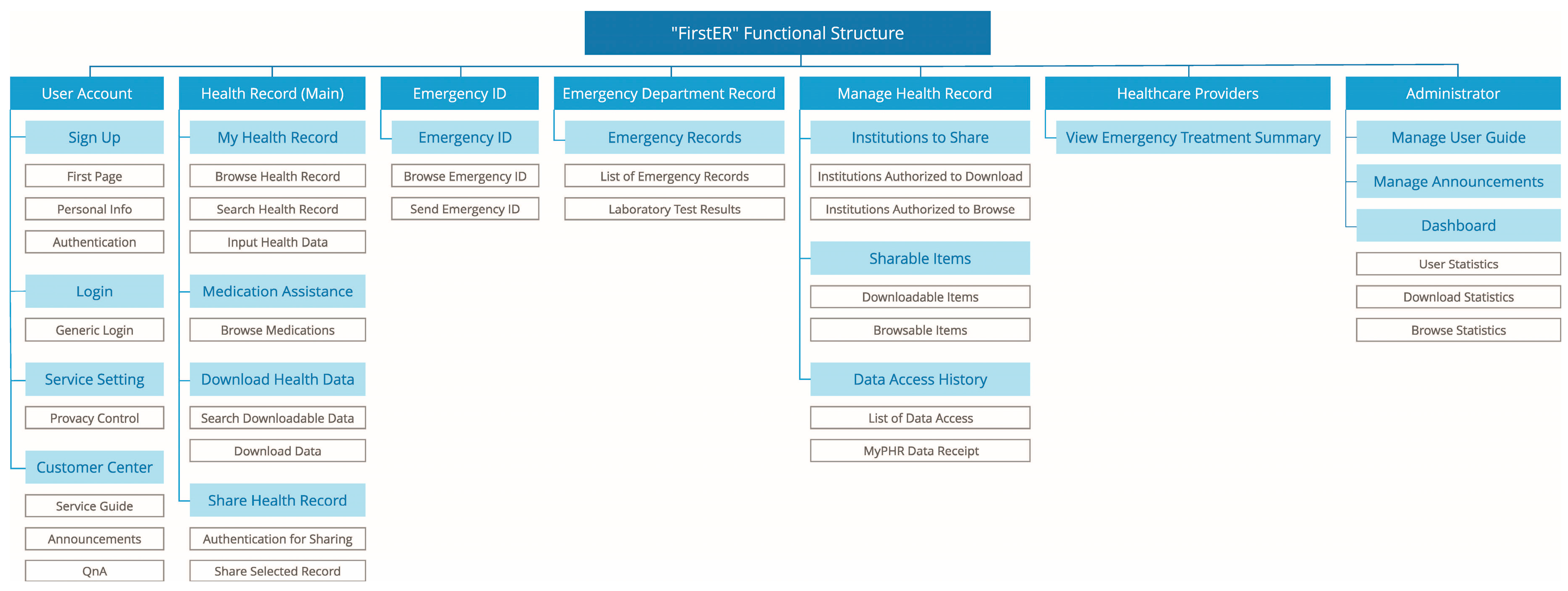
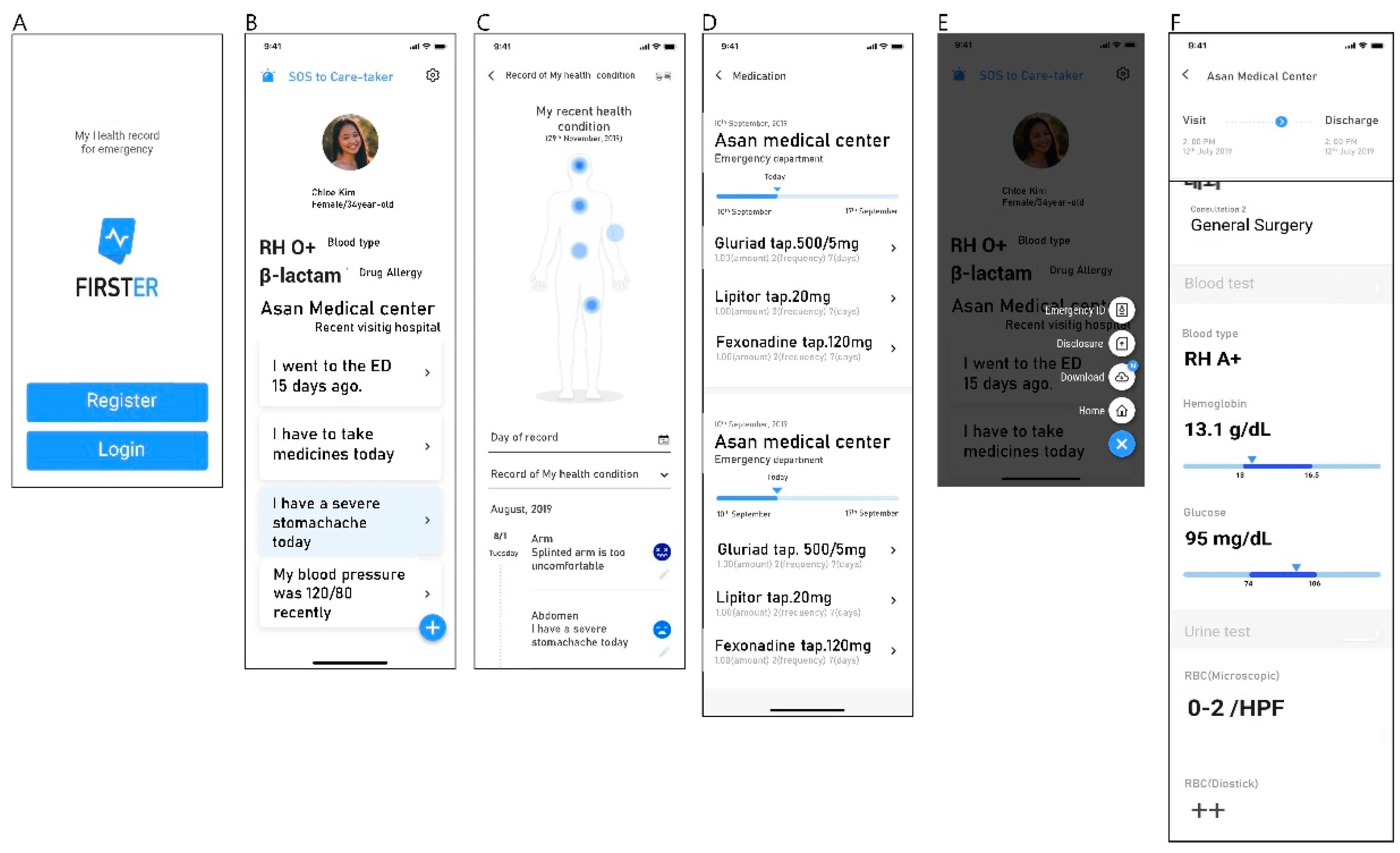
3.1. Services Provided by the Novel PHR Application for Emergency Situations: FirstER
3.1.1. Main Function
3.1.2. Data Provided by FirstER
3.1.3. Developed System and Server of FirstER
3.2. Pre-Operation Testing
3.3. Flow of Services
3.4. Frequency of System Access and Utilization
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hudson, P.; Ekholm, J.; Johnson, M.; Langdon, R. Early identification and management of the unstable adult patient in the emergency department. J. Clin. Nurs. 2015, 24, 3138–3146. [Google Scholar] [CrossRef]
- Abel, G.A.; Mendonca, S.C.; McPhail, S.; Zhou, Y.; Elliss-Brookes, L.; Lyratzopoulos, G. Emergency diagnosis of cancer and previous general practice consultations: Insights from linked patient survey data. Br. J. Gen. Pract. 2017, 67, e377–e387. [Google Scholar] [CrossRef] [PubMed]
- Alimenti, D.; Buydos, S.; Cunliffe, L.; Hunt, A. Improving perceptions of patient safety through standardizing handoffs from the emergency department to the inpatient setting. J. Am. Assoc. Nurse Pract. 2019, 31, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, J.S.; Kannry, J.; Lipton, M.; Goldberg, E.; Conocenti, P.; Stuard, S.; Wyatt, B.M.; Kuperman, G. Approaches to patient health information exchange and their impact on emergency medicine. Ann. Emerg. Med. 2006, 48, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Bouayad, L.; Ialynytchev, A.; Padmanabhan, B. Patient health record systems scope and functionalities: Literature review and future directions. J. Med. Internet Res. 2017, 19, e388. [Google Scholar] [CrossRef]
- Bouri, N.; Ravi, S. Going mobile: How mobile personal health records can improve health care during emergencies. JMIR Mhealth Uhealth 2014, 2, e8. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.Y.; Song, B.; Anand, E.; Schwartz, D.; Panesar, M.; Jackson, G.P.; Elkin, P.L. Barriers, facilitators, and solutions to optimal patient portal and personal health record use: A systematic review of the literature. AMIA Annu. Symp. Proc. 2018, 2017, 1913–1922. [Google Scholar]
- Ro, H.J.; Jung, S.Y.; Lee, K.; Hwang, H.; Yoo, S.; Baek, H.; Lee, K.; Bae, W.K.; Han, J.-S.; Kim, S.; et al. Establishing a personal health record system in an academic hospital: One year’s experience. Korean J. Fam. Med. 2015, 36, 121–127. [Google Scholar] [CrossRef]
- Andrikopoulou, E.; Scott, P.J.; Herrera, H. Important design features of personal health records to improve medication adherence for patients with long-term conditions: Protocol for a systematic literature review. JMIR Res. Protoc. 2018, 7, e159. [Google Scholar] [CrossRef]
- Koivumäki, T.; Pekkarinen, S.; Lappi, M.; Väisänen, J.; Juntunen, J.; Pikkarainen, M. Consumer adoption of future MyData-based Preventive eHealth Services: An acceptance model and survey study. J. Med. Internet Res. 2017, 19, e429. [Google Scholar] [CrossRef]
- Park, J.-Y.; Lee, G.; Shin, S.-Y.; Kim, J.H.; Han, H.-W.; Kwon, T.-W.; Kim, W.S.; Lee, J.H. Lessons learned from the development of health applications in a tertiary hospital. Telemed. J. E Health 2014, 20, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.-H.; Min, M.-K.; Lee, D.-S.; Yeom, S.-R.; Lee, S.-H.; Wang, I.-J.; Cho, S.-J.; Hwang, S.-Y.; Lee, J.-H.; Kim, Y.H. Changes in relative importance of the 5-level triage system, Korean Triage and Acuity Scale, for the disposition of emergency patients induced by forced reduction in its level number: A multi-center registry-based retrospective cohort study. J. Korean Med. Sci. 2019, 34, 1–12. [Google Scholar] [CrossRef]
- Ham, S.; Min, Y.-G.; Chae, M.K.; Kim, H.-H. Epidemiology and regional differences of acute poisonings of eight cities in Gyeonggi-do province in Korea using data from the National Emergency Department Information System of Korea. Clin. Exp. Emerg. Med. 2020, 7, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.-Y.; Kim, J.; Chung, K.-Y.; Park, D.K. Mobile healthcare application with EMR interoperability for diabetes patients. Cluster Comput. 2013, 17, 871–880. [Google Scholar] [CrossRef]
- Wagner, P.J.; Dias, J.; Howard, S.; Kintziger, K.W.; Hudson, M.F.; Seol, Y.H.; Sodomka, P. Personal health records and hypertension control: A randomized trial. J. Am. Med. Inform. Assoc. 2012, 19, 626–634. [Google Scholar] [CrossRef]
- Bellini, P.; Boncinelli, S.; Grossi, F.; Mangini, M.; Nesi, P.; Sequi, L. Mobile emergency, an emergency support system for hospitals in mobile devices: Pilot study. JMIR Res. Protoc. 2013, 2, e19. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; DeAlmeida, D.; Parmanto, B. Applying a user-centered approach to building a mobile personal health record app: Development and usability study. JMIR Mhealth Uhealth 2019, 7, e13194. [Google Scholar] [CrossRef] [PubMed]
- Nittas, V.; Mütsch, M.; Ehrler, F.; Puhan, M.A. Electronic patient-generated health data to facilitate prevention and health promotion: A scoping review protocol. BMJ Open 2018, 8, e021245. [Google Scholar] [CrossRef] [PubMed]
- Abdolkhani, R.; Gray, K.; Borda, A.; DeSouza, R. Patient-generated health data management and quality challenges in remote patient monitoring. JAMIA Open 2019, 2, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.Y.; Kim, J.-W.; Hwang, H.; Lee, K.; Baek, R.-M.; Lee, H.-Y.; Yoo, S.; Song, W.; Han, J.-S. Development of comprehensive personal health records integrating patient-generated health data directly from Samsung S-health and Apple health apps: Retrospective cross-sectional observational study. JMIR Mhealth Uhealth 2019, 7, e12691. [Google Scholar] [CrossRef]
- Perotte, R.; Lewin, G.O.; Tambe, U.; Galorenzo, J.B.; Vawdrey, D.K.; Akala, O.O.; Makkar, J.S.; Lin, D.J.; Mainieri, L.; Chang, B.C. Improving emergency department flow- reducing turnaround time for emergent CT scans. AMIA Annu. Symp. Proc. 2018, 2018, 897–906. [Google Scholar] [PubMed]
- Kaushik, N.; Khangulov, V.S.; O’Hara, M.; Arnaout, R. Reduction in laboratory turnaround time decreases emergency room length of stay. Open Access Emerg. Med. 2018, 10, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Stang, A.S.; Crotts, J.; Johnson, D.W.; Hartling, L.; Guttmann, A. Crowding measures associated with the quality of emergency department care: A systematic review. Acad. Emerg. Med. 2015, 22, 643–656. [Google Scholar] [CrossRef] [PubMed]
| Targeted User Groups | Functionalities Required | |
|---|---|---|
| Patient | Registration | |
| Log-in | ||
| Personal information management | ||
| Customer service center | ||
| Health records (Home) | ||
| Medication alarm | ||
| Download of medical record | ||
| “Disclosure” of medical record | ||
| Record of health condition | ||
| Record of self-checked blood pressure | ||
| Emergency ID | ||
| Inquiry of ED records | ||
| Inquiry of laboratory test results | ||
| Inquiry of urinalysis test result | ||
| Inquiry of list of ED visits | ||
| Set-up of data-shareable institution | ||
| Set-up of shareable details | ||
| List of data utilization and withdrawal of sharing SOS to care-taker | ||
| ED staff | Receiving temporary URL of “ED record summary” via e-mail or SNS | |
| Authentication | ||
| Inquiry of “ED record summary” | ||
| Inquiry of details of ED records | ||
| Manager | Management of service usage | |
| Management of notice | ||
| Dashboard | ||
| Others | Easy-to-read terms | |
| Selective sharing method | ||
| Safe data collection and utilization process | ||
| Explicit consent before downloading | ||
| Receipt of utilized data | ||
| Sample | Name of Laboratory Test |
|---|---|
| Blood | White blood cell count |
| Blood | Hemoglobin |
| Blood | Platelet count |
| Blood | Absolute neutrophil count |
| Blood | Prothrombin time |
| Blood | Activated prothrombin time |
| Blood | Blood urea nitrogen |
| Blood | Creatinine |
| Blood | Total bilirubin |
| Blood | Gamma glutamyl transpeptidase |
| Blood | Alkaline phosphatase |
| Blood | Alanine transaminase |
| Blood | Aspartate transaminase |
| Blood | Amylase |
| Blood | Lipase |
| Blood | Sodium |
| Blood | Potassium |
| Blood | Uric acid |
| Blood | Hemoglobin A1c |
| Blood | Creatine kinase |
| Blood | Creatine kinase-myocardial band fraction |
| Blood | Troponin I |
| Blood | C-reactive protein |
| Blood | N-terminal pro-B-type natriuretic peptide |
| Blood | Brain natriuretic peptide |
| Urine | pH |
| Urine | Occult hematuria |
| Blood | ABO blood typing |
| Others | Influenza antigen immunoassay |
| Category of EMR-Tethered Data Provided | Samsung Medical Center | Asan Medical Center | Dong-A University Hospital | Total (%) |
|---|---|---|---|---|
| Visit | 4523 | 1694 | 2398 | 8615 (54.0) |
| Consultation history | 16 | 0 | 0 | 16 (0.0) |
| Laboratory test | 2699 | 886 | 1636 | 5221 (32.7) |
| Operation history | 10 | 0 | 2 | 12 (0.0) |
| Prescription data | 1285 | 241 | 561 | 2087 (13.1) |
| Total | 8533 | 2821 | 4597 | 15,951 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.; Kim, J.-s.; Kwon, I.H.; Kim, T.; Kim, S.M.; Cha, W.; Jeong, J.; Lee, J.-H. Development of a Mobile Personal Health Record Application Designed for Emergency Care in Korea; Integrated Information from Multicenter Electronic Medical Records. Appl. Sci. 2020, 10, 6711. https://doi.org/10.3390/app10196711
Choi Y, Kim J-s, Kwon IH, Kim T, Kim SM, Cha W, Jeong J, Lee J-H. Development of a Mobile Personal Health Record Application Designed for Emergency Care in Korea; Integrated Information from Multicenter Electronic Medical Records. Applied Sciences. 2020; 10(19):6711. https://doi.org/10.3390/app10196711
Chicago/Turabian StyleChoi, Yuri, June-sung Kim, In Ho Kwon, Taerim Kim, Su Min Kim, Wonchul Cha, Jinwoo Jeong, and Jae-Ho Lee. 2020. "Development of a Mobile Personal Health Record Application Designed for Emergency Care in Korea; Integrated Information from Multicenter Electronic Medical Records" Applied Sciences 10, no. 19: 6711. https://doi.org/10.3390/app10196711
APA StyleChoi, Y., Kim, J.-s., Kwon, I. H., Kim, T., Kim, S. M., Cha, W., Jeong, J., & Lee, J.-H. (2020). Development of a Mobile Personal Health Record Application Designed for Emergency Care in Korea; Integrated Information from Multicenter Electronic Medical Records. Applied Sciences, 10(19), 6711. https://doi.org/10.3390/app10196711





