Abstract
The ability to maintain postural stability is essential in our daily lives. Relatedly, hemiparetic stroke patients have a very high risk of falls. This study aimed to improve the traditional rehabilitation treatment for stroke patients with hemiparesis by providing a virtual reality (VR) feedback system with modular interactive tiles (MITs) to enhance their postural stability and thus prevent falls. The data collected included pre-test and post-test Berg Balance Scale (BBS) values, and complexity index (CI) values for center of pressure (COP) data based on multiscale entropy (MSE) and multivariate multiscale entropy (MMSE) at the 12-week exercise program. Higher BBS and CI values indicate better postural stability, and the results showed that the exercise program yielded significant improvements in postural stability. The mean pre-test BBS value of 51.67 ± 3.12 increased to 53.83 ± 2.17 (p < 0.05), and the mean CI of MMSE value increased by 14.8% (p < 0.01). We confirmed that this training program including MITs is beneficial to the rehabilitation of stroke patients. More specifically, the MITs training program positively affected the CI of MMSE values, and the affected result similar to the BBS values of the patients, indicating their improved balance and ability to avoid falls.
1. Introduction
Postural stability plays an important role in our daily lives, and the ability to maintain one’s balance relies upon complex physiological processes. Postural control involves a variety of sensory inputs, including proprioceptive, vestibular, visual, and tactile somatosensory inputs. The body state, or body schema, is represented by the integration of these multisensory inputs, and is then employed by the brain in the generation of motion [1]. More specifically, the combined activities and effects of the motor nervous system, sensory nervous system, cognitive ability, and visual feedback are typically needed to maintain postural balance. As such, if one of those contributing systems is defective, balance may be adversely affected, even to the extent that falls occur. Gallahue proposed that postural stability is an essential and indispensable physical capability in our daily lives [2]. Relatedly, physical fitness can be built up by regular and long-term exercise, and exercise can improve postural stability in a manner that may help prevent falls [3,4].
Falls are caused by many factors. Among the factors that are commonly responsible for falls are balance problems; gait problems; musculoskeletal problems; neurological problems; the utilization of medicines that affect balance; memory, thinking, and visual impairments; and environmental hazards (such as slippery floors, stairs, and poor lighting) [5]. Hemiparesis is the most frequent occurring neurological deficit after strokes [6]. Hemiparetic stroke patients often present with balance deficits, which in turn means that hemiparetic stroke patients have a very high risk of falls [7]. A study by Jørgensen et al. [8] reported that 73% of stroke patients had at least one fall within the first six months after a stroke, that 21% had at least one fall more than six months after, and that over half of all the reported falls occurred during walking activities due to problems such as loss of balance, misjudgments, and foot dragging. Fear of falling also leads to increased dependence of stroke patients on caregivers and reduced self-care skills in daily life [9]. In order to prevent and reduce the risk of falls, stroke rehabilitation provides a series of treatments aimed at helping stroke patients to relearn skills lost due to the effects of stroke on different parts of their brains. In the last few decades, rehabilitation has become an increasingly significant element in stroke care [10]. Various rehabilitation strategies are established or in development, targeting muscle activity, postural, and gait tasks. These include neuro-facilitation approaches, muscle strength training, treadmill training, multisensory training, and aerobic exercise training. Some strategies use technological equipment, such as functional electrical stimulation (FES) and electromechanical or robot-assisted gait training [11]. However, the physical rehabilitation and general fitness training regimens in rehabilitation centers were too routine and usually considered by patients to be tedious and monotonous, leading to reduced patient motivation, reduced compliance, and reduced effectiveness. In recent years, however, the use of virtual reality (VR) has been introduced in the field of stroke rehabilitation [12]. It has been shown that VR training can improve upper extremity motor function in adults with chronic hemiparesis resulting from a stroke [13]. For example, De Rooij et al. found that a positive and promising effect of VR training on balance and gait ability can be expected [14]. Meanwhile, Lund made another important contribution to rehabilitation efforts through the development of modular interactive tiles® (MITs) [15]. The MITs for rehabilitation are designed to motivate patients to perform specific physical actions by creating playful experiences for them. Nielsen and Lund explained how to use MITs with stroke patients, chronic obstructive pulmonary disease (COPD) patients, cardiac patients, and the elderly in general, both in hospitals and in the private homes of patients [16]. Moreover, the playful games enabled by the MITs motivate patients stay engaged in the games and forget about their surrounding environments, e.g., rehabilitation centers [17].
There are a variety of studies regarding the different measurements of physiological signals. Postural stability is most often characterized with measures based on displacements of the center of pressure (COP) measured with a force platform [18], with specific COP displacements, namely, anterior-posterior (AP) and medial-lateral (ML) displacement, mostly being used to characterize COP stabilograms. The linear method is usually used as the most typical analysis, but the physiological signals from the human body are dynamic, irregular, and non-linear. Therefore, some previous studies regarding gait and balance performance have used patients’ COP results as a factor to evaluate the complexity index (CI) of multiscale entropy (MSE). The area under the MSE curve defines CI as , where “sn” is the scale number. The COP signal shows the maximum difference when m = 2 and r = 0.15 [19].
However, data channels can only be considered separately when using the MSE method, and that is only appropriate in the event that the multivariate signals are not dependent on one another and are not statistically correlation with each other [20]. Relatedly, a published study regarding the MMSE (multivariate multiscale entropy) method provided validation of the method for illustrated benchmark signals, as well as for a simultaneous analysis of the ML and AP components of the postural sway dynamics of both elderly and young subjects [19]. Therefore, the aims of this study were to investigate the effects of a 12-week rehabilitation exercise training program on the postural stability of stroke patients, and to verify the sensitivity of the MMSE method for analyzing physiological signals of postural sway.
2. Materials and Methods
This study used the within-subject design in which the same group of subjects was subjected to more than one treatment. A within-subject design was chosen because it requires fewer participants, making the process much more streamlined and less resource-heavy, and because it can control for the individual differences in each participant that can affect the outcomes of treatments (that is, the changes in the independent variables).
The study activities were performed on a volunteer basis by 10 outpatients, including 5 men and 5 women, at the rehabilitation treatment center of a tertiary hospital in northern Taiwan. However, 1 male subject had to exit the training due to hospitalization. Therefore, the subjects in this study ultimately consisted of 9 stroke patients with a mean age of 56 ± 2.8 years. The subjects were recruited from the rehabilitation center of Far Eastern Hospital. All of the patients signed Institutional Review Board (IRB) approval agreements and informed consent before participating in the study, and the study was conducted in accordance with relevant guidelines and regulations. Ethical approval was received from the Research Ethics Review Committee of Far Eastern Memorial Hospital (New Taipei, Taiwan), and IRB approval was also received (no: FEMH-IRB-103034-F, v.05, Board Meeting/Approval Date: 30 June 2015), including approval of the recruitment posting, agreement text, and questionnaire. Furthermore, clinical trial registration (27 October 2019) and a PPS receipt (ClinicalTrials.gov ID: NCT04141384) were obtained. The following inclusion criteria were used: stroke with hemiparesis (with the stroke having occurred at least 12 months earlier); stable medical condition; ability to walk over five meters (able to use assistive devices); ability to tandem stand independently for more than ten seconds; and ability to understand and cooperate with the experimental procedures [7]. Our exclusion criteria included the inability to stand or walk as indicated by a modified Rankin Scale (mRS) score > 3. The exclusion criteria also included having Alzheimer’s, heart failure, eye disorders, and taking certain medications. Table 1 shows the subjects’ characteristics, as well as the specific inclusion criteria and exclusion criteria. The inclusion and exclusion criteria were rigorously reviewed by the IRB committee twice before finally being approved for this study.

Table 1.
Subjects’ characteristics and the inclusion criteria (n = 9).
2.1. Statistical Analysis
The Wilcoxon signed-rank test was used to test differences in the paired data in this study, with the Statistical Package for the Social Sciences, version 12.0 (SPSS; Chicago, IL, USA), being used for the statistical analyses.
Because the study was a pilot study that was subject to limitations imposed by the IRB requirements for patient safety and research funding, and because of the space limitations of the exercise program site itself, recruiting and including a large number of participants would have been difficult. So, the study size is limited to 10 patients. However, recent related studies of patients with chronic stroke with 10 participants have yielded clinically valuable results and contributions [21,22].
2.2. Group Exercise and MIT Program
The MITs (Entertainment Robotics, Odense, Denmark) are a distributed system of electronic tiles that, like building blocks, can be attached to one another to form the overall system. Each tile is self-sufficient in terms of processing power, and each one has a battery that lasts for approximately 30 h of use. When connected to one another to form a playing field, the modular tiles communicate with their neighbors through four infrared transceivers located on their sides [17].
The stroke patients in this study participated in a 12-week exercise program (with two 45-min sessions per week) in a therapeutic exercise room. The exercise program consisted of group exercises and MIT exercises. The group exercises can enhance the peer effect, and it started with warm-ups followed by strength training and balance training. The specific activities were decided on by the attending therapists based on each patient’s condition. Two therapists assisted six to eight patients, and the total duration of the group exercises was 30 min per session. In the last 15 min of each overall exercise session, four MIT games were played, including the (1) Color Race, (2) Island, (3) Final Countdown, and (4) Reach games. These four games are potentially challenging to patients in terms of mobility, balancing, endurance, and reaction. The protocol for the MIT exercises called for each patient to start by playing the Color Race game, with each round lasting from 1 min to 4 min at a time followed by a break of 0.5 min. Next, a 3 × 3 round of the Island game lasting from 1 min to 4 min was played, followed by a break of 0.5 min. Afterwards, a slow version of the Final Countdown game was played for safety. Again, the game lasted from 1 min to 4 min and was followed by a break of 0.5 min. The Reach game was then played as a final game, and the shape was set at 2 × 4; again, the game lasted from 1 min to 4 min.
Furthermore, in order to increase the intensity of the MIT exercises for the stroke patients, the therapists suggested increasing the duration and difficulty of each game gradually. As a result, the exercise schedule was divided into three stages as follows: (1) Holding with the sound side, (2) Holding with the affected side, and (3) Without holding. Meanwhile, the duration of each game was adjusted. For instance, in the first week, patients were asked to play only one minute of each game, and then the following week the exercising duration was increased to 2 min.
The primary measurements were static and dynamic balance function tests. The static balance, that is, the mediolateral weight distribution on the paretic and non-paretic extremities, was measured with the force platform test, which was used to assess the weight distribution and COP [9]. The dynamic balance was measured with the Berg Balance Scale (BBS). The BBS is an index that is used to assess overall balance ability in elderly people. The BBS has also been shown to be useful in assessing balance in patients with an acute stroke [23]. All the subjects were assessed at baseline (before training) and after the exercise program (that is, after finishing the 12-week training program).
2.3. Center of Pressure (COP) Measurement
The center of pressure (COP) is defined as “the position of the applied force vector that is influenced by the shear forces produced by body segment acceleration” [24]. The COP is often adapted to measure postural stability because it reflects the orientations of the body segments and the movements of the body (including joint angle velocities and accelerations) employed to keep the center-of-gravity over the base-of-support [18]. The COP has a bivariate distribution; it is jointly defined by ML (mediolateral, x-axis) and AP (anteroposterior, y-axis) coordinates, which can be measured with the AMTI force platform and AMTI amplifier devices: AMTI OR6-7-2000 [19]. The mean COP is defined by the arithmetic means of the AP0 and ML0.
Measurements of the area ellipse and mean velocity of sway for static posture show that those who have poor balance have larger COP displacements than those who have better balance [25].
Prieto et al. proposed several stabilogram metrics for estimating postural steadiness and the COP stabilogram, including the mean resultant distance (MDIST), total excursion (TOTEX), RMS distance (RDIST), mean displacement velocity (MVELO), sway area (AREA_SW), and 95% confidence cycle area (AREA_CC) [18], expressed as follows. A variety of metrics are used to characterize COP stabilograms. There are two related stabilogram metrics, AREA_CC and AREA_SW, which are used to estimate the area of a stabilogram. The computations of these stabilogram metrics are given below [26,27]:
2.4. Multivariate Multiscale Entropy (MMSE)
Entropy is particularly useful as a measure of the structure of time series, as it reflects the degree of regularity or irregularity of a sequence of data [28]. As mentioned previously, the physiological signals from the human body are dynamic, irregular, and non-linear. Therefore, to assess the structure dynamics across the different time series, Costa et al. introduced the multiscale entropy (MSE) to measure complexity by calculating sample entropy (SampEn) as the following function of scale, converting the original time series into coarse-grain data, computing the entropy for every scale, and mapping its dependence on the scale [29].
Although the MSE method only considers data channels separately, it can be effectively utilized for the evaluation of signal complexities over a variety of time scales, and previous studies effectively utilized it for analyses of biological, geoscientific, and physiological data [19]. Ahmed and Mandic proposed that the MMSE algorithm could rigorously incorporate multivariate sample entropy in order to take both cross-channel and within-channel dependencies in numerous data channels into account, and then be used to evaluate the effects of said entropy over numerous temporal scales. In comparison to standard MSE, the MMSE algorithm allows for more degrees of freedom to be applied in any analysis, and the algorithm has been demonstrated to yield reliable assessments of the dynamic richness underlying multichannel observations [20,28].
The MMSE method assesses the relative complexity of normalized multichannel temporal data by plotting multivariate sample entropy as a function of the scale factor [28]. Ahmed and Mandic analyzed the COP signals from quiet standing for both young and elderly subjects using the MMSE and MSE approaches. Both the MSE and MMSE analyses showed awareness differences [20,30]. Moreover, the MMSE approach provides complexity analyses of real world biological and physical systems, which are typically of multivariate, correlated, and noisy natures. Since Huang et al. first proposed empirical mode decomposition (EMD) method [31], it has been broadly applied for analyses of non-linear, non-stationary data based on the intrinsic characteristics of time series. Meanwhile, multivariate empirical mode decomposition (MEMD) solves the challenge of mode mixing through the addition of white noise to different channels and also overcomes the single input limitation of EMD. Wei et al. found MEMD-enhanced MMSE can distinguish the smaller differences between before and after the use of vibration shoes in both two directions, which is more powerful than the EMD-enhanced MSE in each individual direction [32]. Chen and Jiang applied the MSE and MMSE approaches to analyze the gait function of 24 elderly, chronically ill patients with cardiovascular disease, diabetes mellitus, or osteoporosis [33]. Chao and Jiang based on COP-Based MMSE measures, further analysis to make a comparison of postural stability during upright standing between normal and flatfooted Individuals of 54 healthy young adults [34]. Their results showed that the MSE algorithms used to identify the sense of balance in young adults and elderly individuals were inferior to the MMSE algorithms utilized for the calculation of the CI of COP data.
3. Results
3.1. Berg Balance Scale Test
The mean pre-test BBS score of the 9 subjects in this study was 51.67 (range: 46–56), while the mean post-test score was 53.83 (range: 49–56). These results showed a statistically significant difference (p = 0.031). However, the minimum pre-test BBS score of 46 was only a bit lower than the minimum post-test score of 49, with both scores being above 45. Moreover, the individual scores show that one subject achieved the full score (56) for the BBS in the pre-test and four subjects achieved the full score (56) in the post-test. Because the total number of subjects was less than 30, the Wilcoxon rank-sum test was adopted to show the difference between the scores before and after the training program for the measurements shown in Figure 1C.
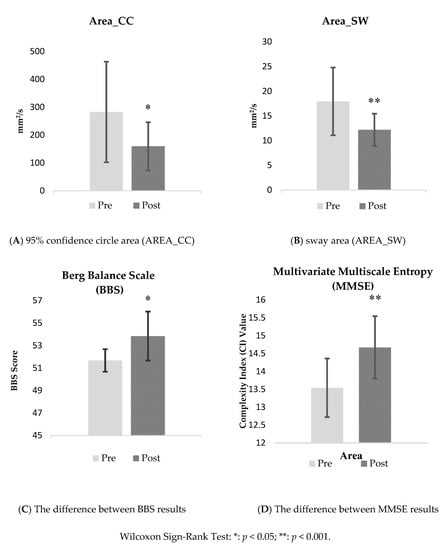
Figure 1.
The difference results between pre-test and post-test values with MIT training.
3.2. Center of Pressure (COP) Analysis
COP stabilograms often use the following values to evaluate measurement results: the mean resultant distance (MSIDT), total excursion (TOTEX), mean displacement velocity (MVELO), sway area (AREA_SW), and 95% confidence circle area (AREA_CC), among others [35]. In this study, the MSIDT, TOTEX, MVELO, and AREA_SW were used to analyze the results based on traditional COP (Table 2 shows the results of COP stabilometric parameter). As indicated in Table 2, both the AREA_CC and AREA_SW exhibited lower values after the 12-week training program (the mean AREA_CC value changed from 282.76 to 159.64, and the mean AREA_SW value changed from 17.93 to 12.17, for 36% and 32% decreases, respectively, for AREA_CC and AREA_SW). The analysis results showed significant decreases in AREA_SW and AREA_CC (p = 0.0391, p = 0.0078 for AREA_SW and AREA_CC, respectively), especially in AREA_CC. Figure 1A,B also present differences between the pre- and post-test values for AREA_CC and AREA_SW.

Table 2.
The results of the group exercise with modular interactive tiles (MITs) before and after the 12-week training program.
3.3. Multivariate Multiscale Entropy (MMSE)
The MMSE method showed similar results; Table 3 shows the significance of the results for the original signal. It is evident that the difference in complexity between the pre- and post-test results was statistically significant at the 0.05 significance level (p = 0.0039). The mean CI value changed from 13.33 to 15.30, for an increase of 14.8%. Figure 1D shows the difference between the pre- and post-test results.

Table 3.
The complexity index (CI) of multivariate multiscale entropy (MMSE) values.
4. Discussion
This study aimed to investigate the effect of group therapy and an MIT interactive system program to enhance gait function of chronic stroke patients, and to compare the clinical contribution of CI and BBS index in measuring postural stability. This is the first study of the direct application of MITs to stroke patients with hemiparesis. Based on the medical ethics and IRB requirements of clinical intervention experiments, it is not easy to collect a large number of research subjects for stroke-related intervention studies, and the first study for comparison of the CI of MMSE values and BBS score for the participating in clinical application.
Despite the small drawback of its ceiling effect, the BBS is one of the most commonly applied clinical measures of balance for individuals with stroke. Based on their previous clinical experiences, the developers of the BBS proposed that scores below 45 (out of 56) indicate an increased risk for falls [36,37]. In this study, after 12 weeks of training, the mean BBS score of the study participants was increased from 51.67 to 53.83, with an average improvement of 4.2%. Moreover, the results showed a statistically significant difference between pre- and post-test scores (p < 0.05). The study results thus showed that the 12-week exercise program including MIT training should improve the postural stability of these chronic stroke patients and provided value in rehabilitation therapy. However, due to the sampling method and lack of a control group, further research is required. The results were similar to those reported in the study [17] focused on healthy elderly in the community. Using MITs for gameplay and interactive training activities can improve the balance, mobility, agility, etc. of those using the MITS and reduce the incidence of falls.
Traditional (conventional) group exercises for chronic stroke patients in the hospital rehabilitation treatment center only include strength training and balance exercise training, and such exercises are unable to achieve effective two-way feedback. These single approach and low-variability training activities also result in reduced patient participation. MIT training, in contrast, provides VR feedback in the form of games that effectively improves patient motivation. The purpose of this study was to increase motivation and achieve two-way feedback on the MIT exercise program. This aimed to increase patient interest and compliance, prolong movement time, reduce the difficulty of upper limb support to increase the difficulty of the movement, and promote muscle strength, movement coordination, and postural stability. These are very important for chronic stroke patients and even healthy elderly people. In this study, the difference in the mean BBS pre- and post-test scores was small but statistically significant (p = 0.0313). However, the degree of improvement was only 4.2%, lower than the improvement in the CI results (14.8%) based on the COP measurement MMSE method. Among all 9 subjects, four subjects achieved the full BBS score (56). This finding could be explained by a ceiling effect of the BBS, with a ceiling effect occurring when a significant proportion of a tested population achieves the highest possible score on a test [38,39].
On the other hand, according to the results of a study by Straube et al. [40], there was misfit for two of the 14 BBS items of the BBS (specifically, the tandem standing and standing on a single foot items). According to the original instructions for the BBS, the individual taking the test can decide which limb to utilize for the tandem stance and the single-limb stance items. However, administering these items in a standardized manner could potentially enhance the effectiveness of the BBS in terms of accurately measuring an initial balance impairment, as well as changes to a person’s balance caused by spontaneous recovery and rehabilitation interventions. All of the subjects in this study were chronic stroke patients with hemiparesis, and this was probably a factor that affected the results of this study. However, the BBS has also been shown to be useful in assessing balance in patients with an acute stroke [23].
Wii Fit balance training (WBT) and progressive balance training (PBT) are both approaches that have been found to be effective in improving balance functions, balance confidence, and activities of daily living [9].
The Wii Fit and MITs both provide VR feedback in the form of games. In a comparison of these two interesting training modules, Lund and Jessen explained a noteworthy difference in subjects’ performance on standard tests [17]. They showed that community-dwelling elderly subjects (age range: 63–95 years; mean: 83.2 years) using the MITs for 9 sessions showed statistically significant performance improvements on the 6-min walk test (6MWT), timed up go test (TUG), and chair-stand test (CS). Meanwhile, Franco et al. showed in their study based of community-dwelling elderly subjects (average age: 78.3 years) that the participants obtained no significant effects on their standardized BBS test scores with a Nintendo Wii Fit exercise program [41]. Relatedly, Nitz et al. reported that adult subjects (age range: 30–58 years) using the Nintendo Wii Fit for 20 sessions had no significant improvements on the 6MWT and TUG [42]. That said, the Wii Fit should be more suitable for in-house use and is maybe not suitable for use in a rehabilitation center in a hospital or medical clinic. There is sufficient evidence showing that the use of commercial video games (VGs) could be added as an adjunct treatment in rehabilitation in order to stimulate patient motivation, and that such games could also be used at home to maintain the benefits of rehabilitation for a patient [43,44].
With regard to COP measurements, Prieto and Myklebust reported that shorter trajectories and smaller distances and areas represent better balance [18]. As shown in Table 2, the results in this study showed significant decrease in AREA_SW and AREA_CC (p = 0.0391, p = 0.0078 for AREA_SW and AREA_CC, respectively). The definition of AREA_SW is the area that is enclosed by the COP path per unit of time, and said area can be thought of as being proportional to the product of the mean velocity and mean distance [18]. The value of AREA_SW can be determined by adding the mean COP to the areas of the triangles formed to consecutive points on the COP path [27]. Meanwhile, AREA_CC is the area of a circle with a radius equal to the one-sided 95% confidence limit of the RD time series [18]. Figure 1 clearly shows the changes in AREA_SW and AREA_CC, with both values becoming smaller in the post-test, which means in turn that these two stabilometric parameters are able to detect improvements in balance stability.
An MMSE value can be utilized for the assessment of the structural complexity of multivariate systems, and such a value can be determined through the measurement of the relative complexity of the multichannel signals in a plot of the multivariate sample entropy [28]. According to past research, better adaptability in an external environment is indicated by higher complexity, such that the greater the CI value, the greater the postural stability [45]. Table 3 shows the significance of the MMSE results. It is evident that the difference in complexity between the pre-test and post-test was statistically significant at a 0.05 significance level (p = 0.0039). In addition, the findings in terms of the application value were similar to those of Chen and Jiang [33]. This study again validates the significance of CI of the MMSE in postural stability and its application to chronically ill patients for effective balance assessment.
Limitations
This pilot study provided an interactive and interesting exercise program for stroke patients aimed at improving their posture and balance. However, there were some limitations to the study. First, the primary limitations were the small sample size and the lack of a control group. The compliance of the subjects may also have affected our recruitment efforts. Second, the study did not use any assessment tools more accurate that the mRS to evaluate the risk of falls. Third, the study did not follow-up on the effects, if any, of the exercise program after the completion of the 12-week training program itself.
This was a pilot study, and the small number of subjects was a major limitation. In order to ensure patient safety, and because of limitations related to research funding and scheduling, the study had to be implemented in a manner approved by the IRB, such that we could not recruit a larger number of participants.
In addition, as indicated in the criteria listed in Table 1, we excluded patients at a high risk of falling as indicated by the BBS and mRS scores, as well as patients with certain diseases, such that none of the participating patients was at increased risk for falls. As such, the results of this study cannot be generalized to patients with poorer balance or patients with more severe strokes and certain other diseases.
Therefore, in future studies, researchers may want to consider recruiting stroke patients who take part in the original rehabilitation protocol without adopting the MITs in order to detect the differences, if any, between the training programs with and without the MITs. For randomized controlled studies, control subjects with the same conditions can be recruited to make sure that the participants who participate in the 12-week exercise program achieve a better ability to control their postural stability. We also recommend study designs including a follow-up period to look into the sustained effects of the investigated exercise program.
In addition, considering the ceiling effect in BBS, we suggest adding more challenge scales (e.g., the Four Step Square Test) for future studies, so as to ensure the validity and reliability of the results. We also recommend that future studies use the Fall Risk Assessment Score (FRAS) to evaluate the risk of falls before and after the intervention period, look into the sustained effects of the investigated exercise program, and recruit a control group to more effectively investigate the effects of the exercise program.
5. Conclusions
This study examined an exercise program consisting of group and individual exercises. The study results showed that the investigated training program, which includes the use of MITs, benefits the rehabilitation of stroke patients in a rehabilitation therapy center or hospital. Furthermore, the study results also yielded the following conclusions. First, the postural stability of middle-aged and old-aged stroke patients can be improved through the exercise program. The playful program with MITs is highly motivating and interesting and thus encourages participants to continue taking part in the exercise program in order to improve their postural and balance control. The effects on the exercise program are proved by the improvement in terms of the decreased body sway area.
Although this pilot study did not look into the effects of this exercise program after the completion of the 12-week intervention itself, a previous meta-analysis investigating the effects of exercise therapy on balance capacity in chronic stroke patients showed significant effects during follow-up periods for studies reporting BBS scores [46]. Rehabilitation or exercise interventions are used to improve physical function-related indicators. After the regular application of an intervention for a period of time, indicators may be significantly improved. However, when an intervention is stopped, the effects of said intervention may gradually be reduced or even disappear. Nonetheless, the playful exercise program with MITs investigated in this study can yield acute effects that can be generalized to community-dwelling chronic stroke patients. Therefore, it is highly motivating and interesting exercise program for stroke patients to take part in, and one that can be used to maintain the resulting training effects, which consist of postural and balance control benefits.
In the hospital setting, traditional clinical trials are used to evaluate the effectiveness of training exercise program interventions aimed at enhancing gait functions and postural stability and balance. The most discriminating clinical indicator is BBS, typically used along with indicators of knee flexion strength, sit-to-stand movement, TUB or CS test, single-leg stance with eyes-open/ eyes-close, 6MWT in a straight line, and so on to support the accuracy of results [47,48,49]. All of these measurement methods and tools are time- and effort-intensive in terms of data collection, and the collected data may also show high levels of variation, besides BBS.
Only a few previous studies have sought to compare the differences between traditional clinical indicators and MSE or MMSE with regard to postural stability and balance function while also using COP data for the analysis of related indicators [33,34]. This study is the first to compare patients with BBS and MMSE on gait balance in chronic stroke.
Moreover, in addition to the traditional tests used to evaluate balance or postural stability, such as the BBS, CS, TUG, 6MWT, etc., the CI values based on MSE and MMSE of entropy algorithms of COP data were found to provide similar and statistically significant results. These results were highly correlated with BBS, but the costs and benefits of measurement are more highly and avoid the ceiling effect in BBS.
Using these entropy-based methods and traditional clinical indicators of postural stability such as the BBS, the group exercise and MIT training program were found to affect the CI of MMSE values for the participating chronically ill stroke patients with the same result, indicating MITs should improve balance and ability to avoid falls.
Author Contributions
C.-C.L. and B.C.J. conceived and designed the experiments; I.-L.C. and C.-C.L. performed the experiments; C.-C.L. and M.-S.C. analyzed the data; B.C.J. and M.-S.C. were supervision; I.-L.C. and C.-C.L. did the project administration; I.-L.C. and T.-C.L. contributed investigation material; I.-L.C., C.-C.L., and M.-S.C. wrote the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Ministry of Science and Technology (MOST) for supporting this research with ID MOST PB10001-0879, MOST 108-2221-E-161-003-MY2 and this research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors are grateful for the participation and assistance of Dr. Cheng-Ming Chiu (Director of the Rehabilitation Dept.) and to the medical rehabilitation therapists of the FEMH for their support and help in this study. This work was supported by [Ministry of Science and Technology] grant number [MOST PB10001-0879]; [MOST 108-2221-E-161-003-MY2], and this research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
There is no conflict of interests from any author.
Patient Consent for Publication
Not required.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Research Ethics Review Committee at the Far Eastern Memorial Hospital (New Taipei, Taiwan) and the Institutional Review Boards (IRB) approval no: FEMH-IRB-103034-F, v.05, Board Meeting/Approval Date: 20150630, including recruitment post; agreement; questionnaire.
Consent for Publication
This manuscript contains no person’s details, images, or videos.
References
- Chiba, R.; Takakusaki, K.; Ota, J.; Yozu, A.; Haga, N. Human upright posture control models based on multisensory inputs; in fast and slow dynamics. Neurosci. Res. 2016, 104, 96–104. [Google Scholar] [CrossRef]
- Gallahue, D.L.; Ozmun, J.C.; Goodway, J. Understanding Motor Development: Infants, Children, Adolescents, Adults; McGraw-Hill: New York, NY, USA, 1998. [Google Scholar]
- Gillespie, L.; Gillespie, W.; Robertson, M.; Lamb, S.; Cumming, R.; Rowe, B. Interventions for preventing falls in elderly people. Review. Cochrane Database Syst. Rev. 2004, 4, CD000340. [Google Scholar]
- Sherrington, C.; Whitney, J.C.; Lord, S.R.; Herbert, R.D.; Cumming, R.G.; Close, J.C. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2008, 56, 2234–2243. [Google Scholar] [CrossRef]
- Chang, H.J.; Lynm, C.; Glass, R.M. Falls and older adults. JAMA 2010, 303, 288. [Google Scholar] [CrossRef]
- Gresham, G.E.; Duncan, P.W.; Stason, W.B. Post-Stroke Rehabilitation; DIANE Publishing: Darby, PA, USA, 1997; Volume 95. [Google Scholar]
- Oliveira, C.B.; Medeiros, Í.R.; Greters, M.G.; Frota, N.A.; Lucato, L.T.; Scaff, M.; Conforto, A.B.J.C. Abnormal sensory integration affects balance control in hemiparetic patients within the first year after stroke. Clinics 2011, 66, 2043–2048. [Google Scholar] [CrossRef]
- Jørgensen, L.; Engstad, T.; Jacobsen, B.K.J.S. Higher incidence of falls in long-term stroke survivors than in population controls: Depressive symptoms predict falls after stroke. Stroke 2002, 33, 542–547. [Google Scholar] [CrossRef]
- Yatar, G.I.; Yildirim, S.A.J.J. Wii Fit balance training or progressive balance training in patients with chronic stroke: A randomised controlled trial. J. Phys. Ther. Sci. 2015, 27, 1145–1151. [Google Scholar] [CrossRef]
- Nyberg, L.; Gustafson, Y. Patient falls in stroke rehabilitation a challenge to rehabilitation strategies. Stroke 1995, 26, 838–842. [Google Scholar] [CrossRef]
- Beyaert, C.; Vasa, R.; Frykberg, G.E. Gait post-stroke: Pathophysiology and rehabilitation strategies. Neurophysiol. Clin./Clin. Neurophysiol. 2015, 45, 335–355. [Google Scholar] [CrossRef]
- Kim, J.H.; Jang, S.H.; Kim, C.S.; Jung, J.H.; You, J.H. Use of virtual reality to enhance balance and ambulation in chronic stroke: A double-blind, randomized controlled study. Am. J. Phys. Med. Rehabil. 2009, 88, 693–701. [Google Scholar] [CrossRef]
- Saposnik, G.; Levin, M.; Stroke, S.O.R.C.W.G.J. Virtual reality in stroke rehabilitation: A meta-analysis and implications for clinicians. Stroke 2011, 42, 1380–1386. [Google Scholar]
- De Rooij, I.J.; van de Port, I.G.; Meijer, J.-W. Effect of virtual reality training on balance and gait ability in patients with stroke: Systematic review and meta-analysis. Phys. Ther. 2016, 96, 1905–1918. [Google Scholar] [CrossRef]
- Lund, H.H. Modular robotics for playful physiotherapy. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; pp. 571–575. [Google Scholar]
- Nielsen, C.B.; Lund, H.H. Adapting playware to rehabilitation practices. Int. J. Comput. Sci. Sport 2011, 11, 29–41. [Google Scholar]
- Lund, H.H.; Jessen, J.D. Effects of short-term training of community-dwelling elderly with modular interactive tiles. Games Health: Res. Dev. Clin. Appl. 2014, 3, 277–283. [Google Scholar] [CrossRef]
- Prieto, T.E.; Myklebust, J.B.; Hoffmann, R.G.; Lovett, E.G.; Myklebust, B.M. Measures of postural steadiness: Differences between healthy young and elderly adults. Biomed. Eng. IEEE Trans. 1996, 43, 956–966. [Google Scholar] [CrossRef]
- Jiang, B.C.; Yang, W.H.; Shieh, J.S.; Fan, J.Z.; Peng, C.K. Entropy-based method for COP data analysis. Theor. Issues Ergon. Sci. 2013, 14, 227–246. [Google Scholar] [CrossRef]
- Ahmed, M.U.; Mandic, D.P. Multivariate multiscale entropy analysis. Signal Process. Lett. IEEE 2012, 19, 91–94. [Google Scholar] [CrossRef]
- Liao, W.W.; McCombe Waller, S.; Whitall, J. Kinect-based individualized upper extremity rehabilitation is effective and feasible for individuals with stroke using a transition from clinic to home protocol. Cogent Med. 2018, 5, 1428038. [Google Scholar] [CrossRef]
- Boone, A.E.; Wolf, T.J.; Engsberg, J.R. Combining Virtual Reality Motor Rehabilitation With Cognitive Strategy Use in Chronic Stroke. Am. J. Occup. Ther. 2019, 73, 7304345020p1–7304345020p9. [Google Scholar] [CrossRef]
- Suzuki, M.; Fujisawa, H.; Machida, Y.; Minakata, S.J.J. Relationship between the Berg balance scale and static balance test in hemiplegic patients with stroke. J. Phys. Ther. Sci. 2013, 25, 1043–1049. [Google Scholar] [CrossRef]
- Hasan, S.S.; Robin, D.W.; Szurkus, D.C.; Ashmead, D.H.; Peterson, S.W.; Shiavi, R.G.J.G. Simultaneous measurement of body center of pressure and center of gravity during upright stance. Part II: Amplitude and frequency data. Gait Posture 1996, 4, 11–20. [Google Scholar] [CrossRef]
- Thapa, P.B.; Gideon, P.; Brockman, K.G.; Fought, R.L.; Ray, W.A. Clinical and biomechanical measures of balance fall predictors in ambulatory nursing home residents. J. Gerontol. Ser. A Biol. Sci. Med Sci. 1996, 51, M239–M246. [Google Scholar] [CrossRef] [PubMed]
- Hasselkus, B.R.; Shambes, G.M.J.J. Aging and postural sway in women. J. Gerontol. 1975, 30, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Hufschmidt, A.; Dichgans, J.; Mauritz, K.-H.; Hufschmidt, M. Some methods and parameters of body sway quantification and their neurological applications. Arch. Für Psychiatr. Nervenkrankh. 1980, 228, 135–150. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.U.; Mandic, D.P. Multivariate multiscale entropy: A tool for complexity analysis of multichannel data. Phys. Rev. E 2011, 84, 061918. [Google Scholar] [CrossRef]
- Costa, M.; Goldberger, A.L.; Peng, C.K. Multiscale entropy analysis of complex physiologic time series. Phys. Rev. Lett. 2002, 89, 068102. [Google Scholar] [CrossRef]
- Ahmed, M.; Rehman, N.; Looney, D.; Rutkowski, T.; Mandic, D.J.B. Dynamical complexity of human responses: A multivariate data-adaptive framework. Bull. Pol. Acad. Sci. Tech. Sci. 2012, 60, 433–445. [Google Scholar] [CrossRef]
- Huang, N.E.; Shen, Z.; Long, S.R.; Wu, M.C.; Shih, H.H.; Zheng, Q.; Yen, N.C.; Tung, C.C.; Liu, H.H. The empirical mode decomposition and Hilbert spectrum for nonlinear and nonstationary time series analysis. Proc. R. Soc. Lond. A 1998, 454, 903–995. [Google Scholar] [CrossRef]
- Wei, Q.; Liu, D.-H.; Wang, K.-H.; Liu, Q.; Abbod, M.; Jiang, B.; Chen, K.-P.; Wu, C.; Shieh, J.-S. Multivariate multiscale entropy applied to center of pressure signals analysis: An effect of vibration stimulation of shoes. Entropy 2012, 14, 2157–2172. [Google Scholar] [CrossRef]
- Chen, M.-S.; Jiang, B.C. Resistance training exercise program for intervention to enhance gait function in elderly chronically ill patients: Multivariate multiscale entropy for center of pressure signal analysis. Comput. Math. Methods Med. 2014, 2014, 1–10. [Google Scholar] [CrossRef]
- Chao, T.-C.; Jiang, B.C. A Comparison of Postural Stability during Upright Standing between Normal and Flatfooted Individuals, Based on COP-Based Measures. Entropy 2017, 19, 76. [Google Scholar] [CrossRef]
- Nurwulan, N.; Iridiastadi, H.; Jiang, B.C. A Review of the Effect on Postural Stability While Using Mobile Phone. In Bridging Research and Good Practices towards Patients Welfare. In Proceedings of the 4th International Conference on Healthcare Ergonomics and Patient Safety (HEPS), Taipei, Taiwan, 23–26 June 2014; CRC Press: Boca Raton, FL, USA, 2014; p. 101. [Google Scholar]
- Andersson, A.G.; Kamwendo, K.; Seiger, A.; Appelros, P. How to identify potential fallers in a stroke unit: Validity indexes of 4 test methods. J. Rehabil. Med. 2006, 38, 186–191. [Google Scholar] [CrossRef]
- Stevenson, T.J. Detecting change in patients with stroke using the Berg Balance Scale. Aust. J. Physiother. 2001, 47, 29–38. [Google Scholar] [CrossRef]
- Everitt, B. The Cambridge Dictionary of Statistics; Cambridge University Press: Cambridge, UK, 1998. [Google Scholar]
- Ban, B.; Sevšek, F.; Rugelj, D.J.P.Q. A comparison of the ceiling effect between Berg Balance Scale and Mini-BESTest in a group of balance trained community-dwelling older adults. Physiother. Q. 2017, 25, 3–9. [Google Scholar] [CrossRef]
- Straube, D.; Moore, J.; Leech, K.; George Hornby, T.J.T. Item analysis of the berg balance scale in individuals with subacute and chronic stroke. Top. Stroke Rehabil. 2013, 20, 241–249. [Google Scholar] [CrossRef]
- Franco, J.R.; Jacobs, K.; Inzerillo, C.; Kluzik, J.J.T. The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol. Health Care 2012, 20, 95–115. [Google Scholar] [CrossRef]
- Nitz, J.; Kuys, S.; Isles, R.; Fu, S.J.C. Is the Wii Fit™ a new-generation tool for improving balance, health and well-being? A pilot study. Climacteric 2010, 13, 487–491. [Google Scholar] [CrossRef]
- Bonnechère, B.; Jansen, B.; Omelina, L.; Van Sint, J. The use of commercial video games in rehabilitation: A systematic review. Int. J. Rehabil. Res. 2016, 39, 277–290. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Pinto, R.Z.; Saraiva, B.T.; Tebar, W.R.; Delfino, L.D.; Franco, M.R.; Silva, C.C.M.; Christofaro, D.G.D. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 4–12. [Google Scholar] [CrossRef]
- Yang, W. Data Mining on Physiological Single-Integrate Dissimilarity Approach and Signal Reconstruction for Complexity Analysis. Ph.D. Dissertation, Industrial Engineering and Management Department, Yuan Ze University, Chung-Li, Taiwan, 2010. [Google Scholar]
- van Duijnhoven, H.J.; Heeren, A.; Peters, M.A.; Veerbeek, J.M.; Kwakkel, G.; Geurts, A.C.; Weerdesteyn, V. Effects of exercise therapy on balance capacity in chronic stroke: Systematic review and meta-analysis. Stroke 2016, 47, 2603–2610. [Google Scholar] [CrossRef]
- Martínez-Amat, A.; Hita-Contreras, F.; Lomas-Vega, R.; Caballero-Martínez, I.; Alvarez, P.J.; Martínez-López, E. Effects of 12-week proprioception training program on postural stability, gait, and balance in older adults: A controlled clinical trial. J. Strength Cond. Res. 2013, 27, 2180–2188. [Google Scholar]
- Sparrow, D.; Gottlieb, D.J.; DeMolles, D.; Fielding, R.A. Increases in muscle strength and balance using a resistance training program administered via a telecommunications system in older adults. J. Gerontol. Ser. A Biomed. Sci. Med Sci. 2011, 66, 1251–1257. [Google Scholar]
- Muir, S.W.; Berg, K.; Chesworth, B.; Speechley, M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: A prospective study. Phys. Ther. 2008, 88, 449–459. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).