Surface Morphology of Three-Dimensionally Printed Replicas of Upper Dental Arches
Abstract
1. Introduction
2. Materials and Methods
2.1. Three-Dimensional Prints
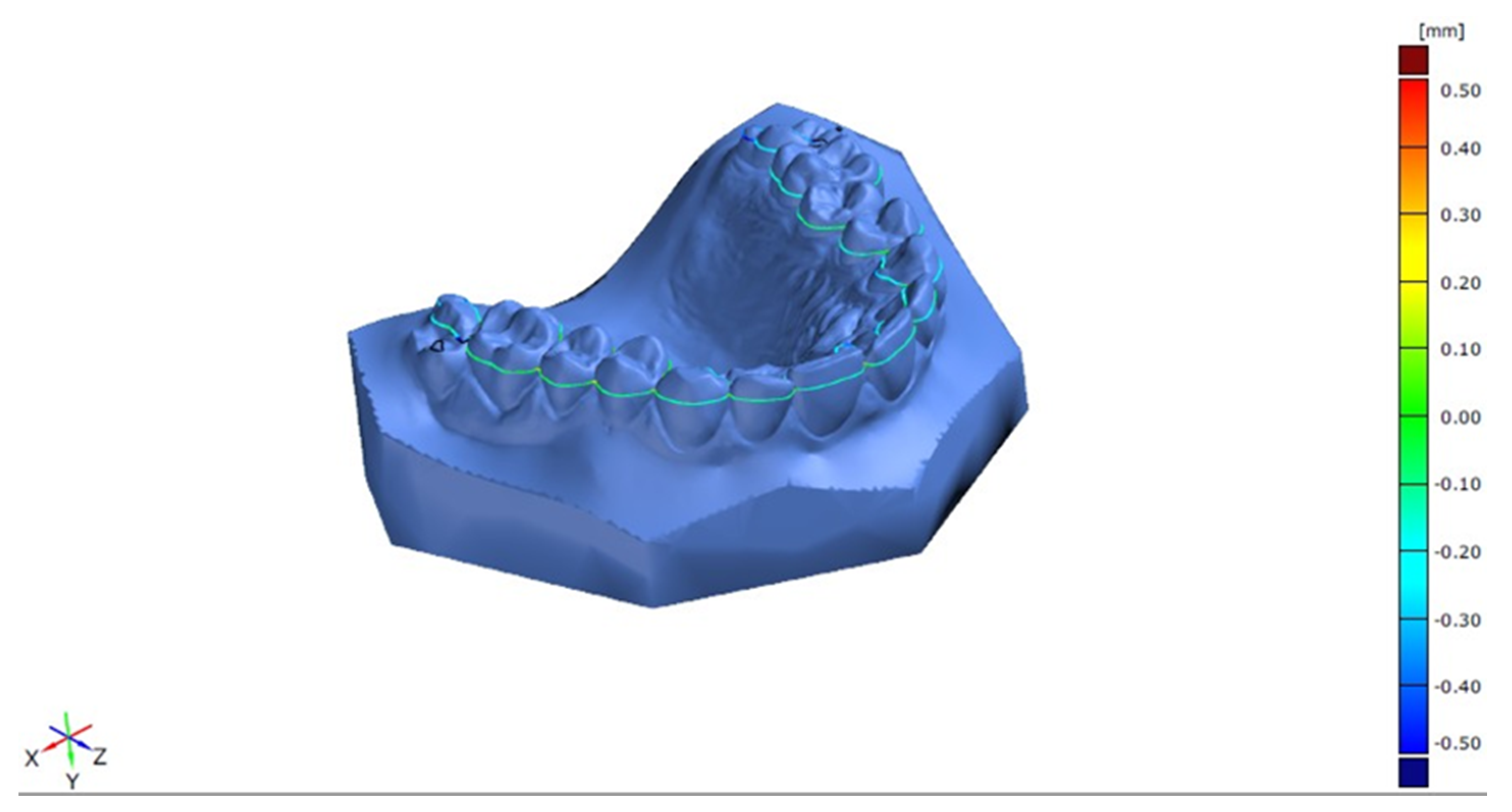
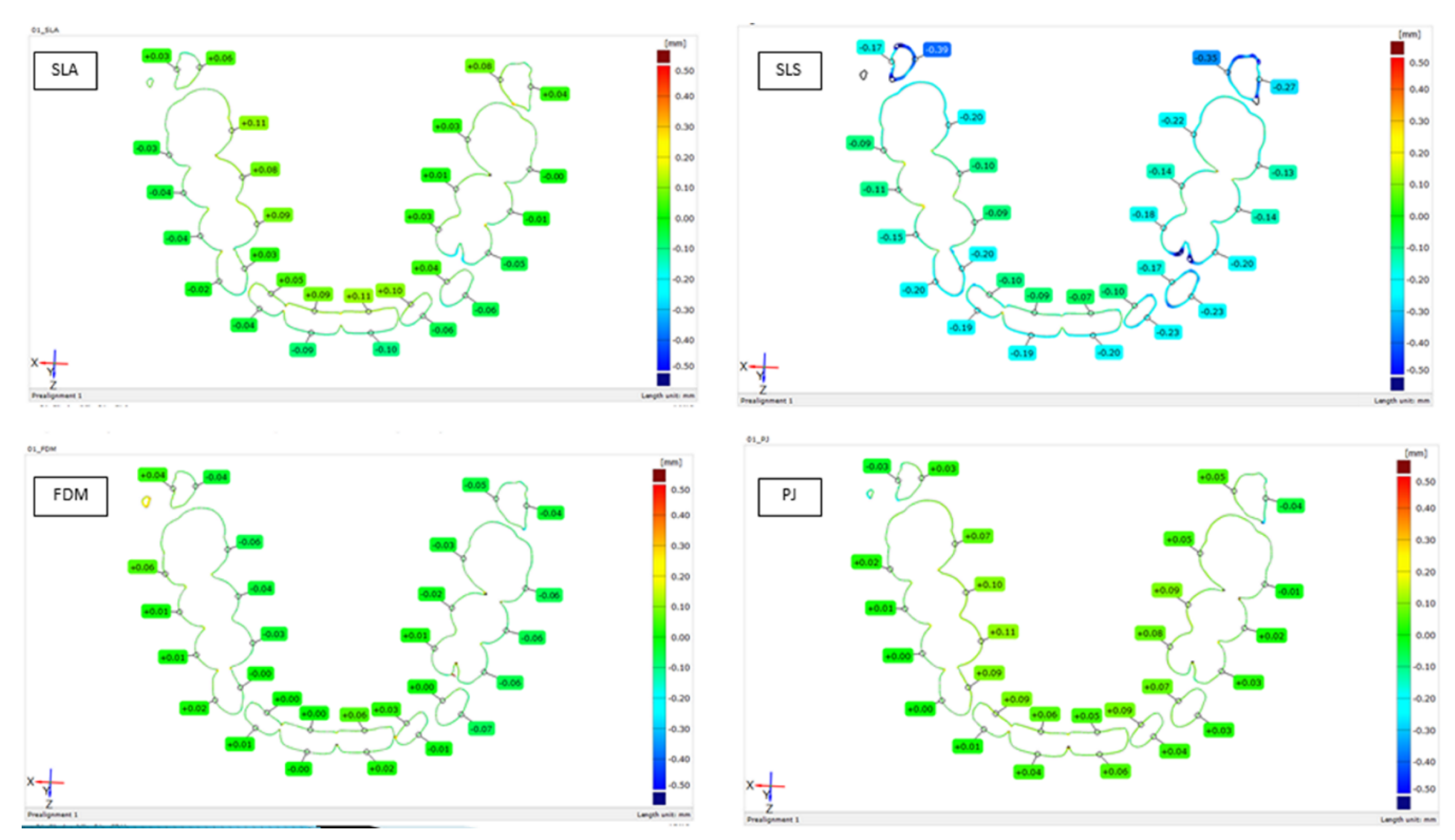
2.2. Cross-Section Model Analysis
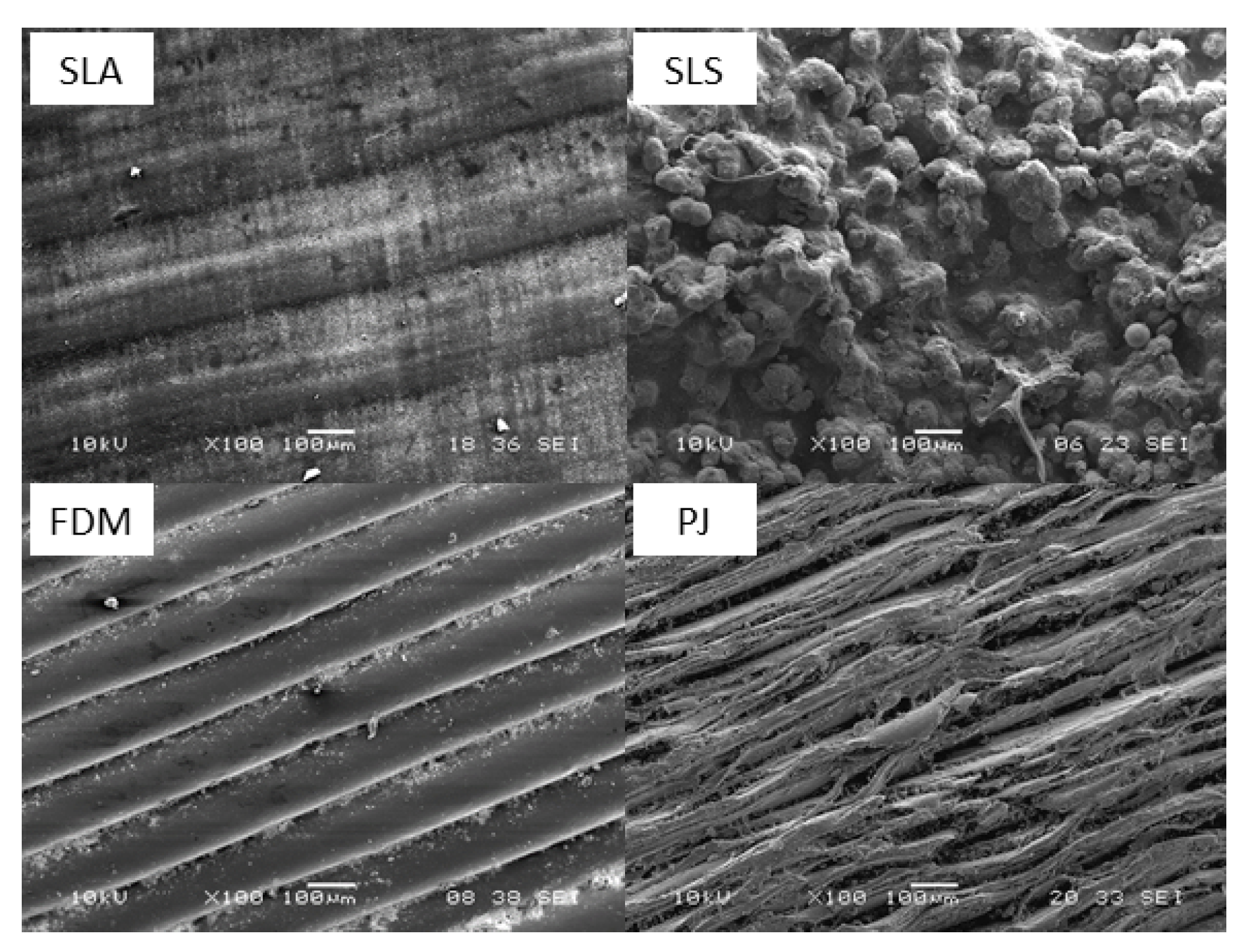
2.3. Surface and Morphology Analysis
3. Results
3.1. Cross-Section Model Analysis
3.2. Surface Structure Analysis
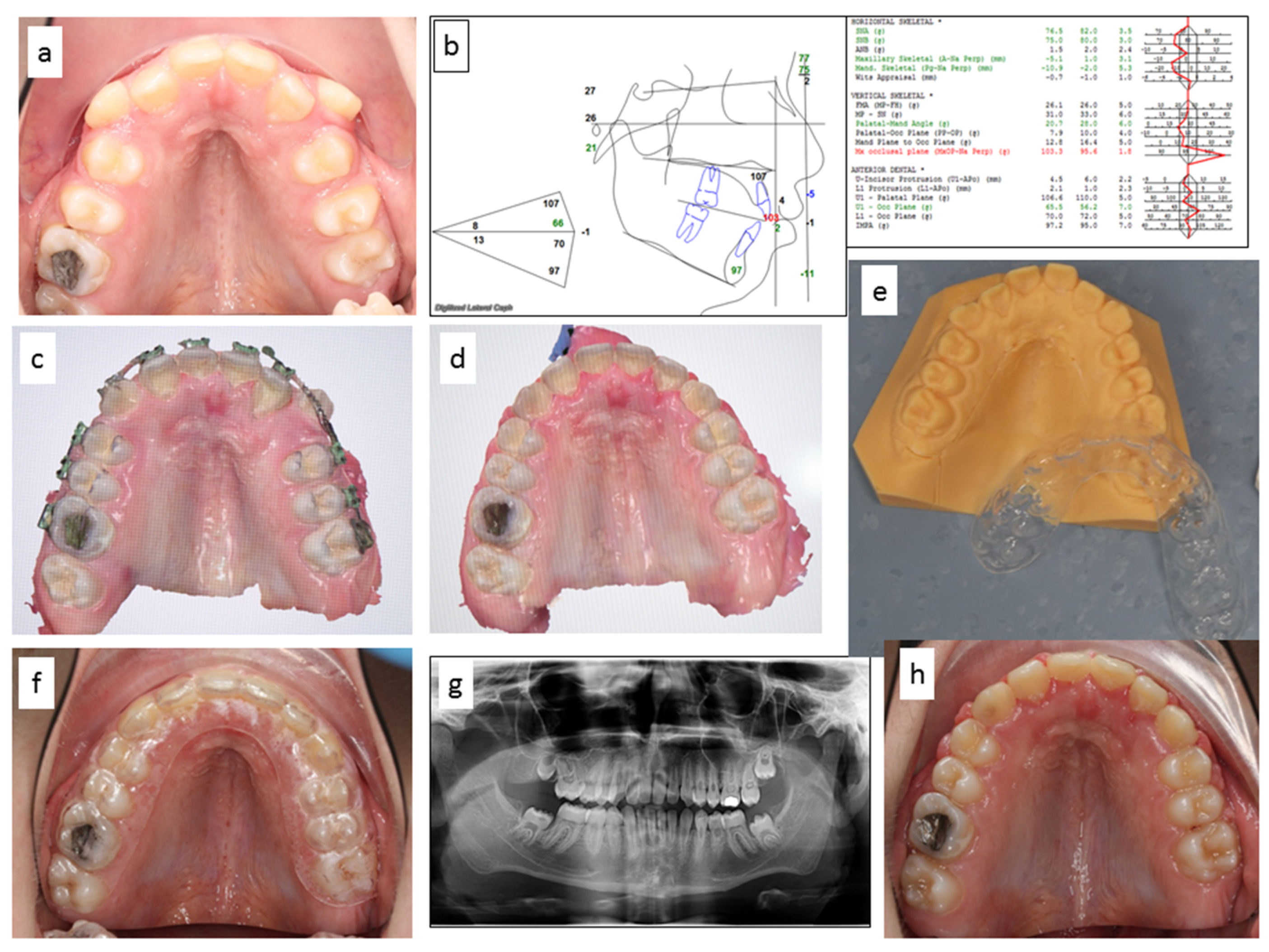
3.3. SLA Clinical Application—Case Report
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Duret, F.; Preston, J.D. CAD/CAM imaging in dentistry. Curr. Opin. Dent. 1991, 1, 150–154. [Google Scholar]
- Staderini, E.; Guglielmi, F.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional prediction of roots position through cone-beam computed tomography scans-digital model superimposition: A novel method. Orthod. Craniofac. Res. 2019, 22, 16–23. [Google Scholar] [CrossRef]
- Richert, R.; Goujat, A.; Venet, L.; Viguie, G.; Viennot, S.; Robinson, P.; Farges, J.C.; Fages, M.; Ducret, M. Intraoral scanner technologies: A review to make a successful impression. J. Healthc. Eng. 2017, 2017, 8427595. [Google Scholar] [CrossRef]
- Staderini, E.; Patini, R.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Three-Dimensional Assessment of Morphological Changes Following Nasoalveolar Molding Therapy in Cleft Lip and Palate Patients: A Case Report. Dent. J. 2019, 7, 27. [Google Scholar] [CrossRef]
- Bocklet, C.; Renne, W.; Mennito, A.; Bacro, T.; Latham, J.; Evans, Z.; Ludlow, M.; Kelly, A.; Nash, J. Effect of scan substrates on accuracy of 7 intraoral digital impression systems using human maxilla model. Orthod. Craniofac. Res. 2019, 22 (Suppl. 1), 168–174. [Google Scholar] [CrossRef]
- Kasparova, M.; Halamova, S.; Dostalova, T.; Prochazka, A. Intra-oral 3D scanning for the digital evaluation of dental arch parameters. Appl. Sci. 2018, 8, 1838. [Google Scholar] [CrossRef]
- Geffers, M.; Barralet, J.E.; Groll, J.; Gbureck, U. Dual-setting brushite-silica gel cements. Acta Biomater. 2015, 11, 467–476. [Google Scholar] [CrossRef] [PubMed]
- De Wild, M.; Meier, F.; Borman, T.; Howald, C.B.C.; Muller, B. Damping of Selective-Laser-Melted NiTi for Medical Implants. J. Mater. Eng. Perform. 2014, 23, 2614–2619. [Google Scholar] [CrossRef]
- Diloksumpan, P.; de Ruijter, M.; Castilho, M.; Gbureck, U.; Vermonden, T.; van Weeren, P.R.; Malda, J.; Levato, R. Combining multi-scale 3D printing technologies to engineer reinforced hydrogel-ceramic interfaces. Biofabrication 2020, 12, 025014. [Google Scholar] [CrossRef] [PubMed]
- Ngoa, T.D.; Kashania, A.; Imbalyanoa, G.; Nguzena, K.T.Q.; Huib, D. Additive manufacturing (3D printing): A review of materials, methods, applications and challenges. Compos. Part B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Stratasys Ltd. Available online: http://www.stratasys.com (accessed on 20 May 2020).
- Dostalova, T.; Kasparova, M.; Chleborad, K. Intraoral Scanner and Stereographic 3D Print in Orthodontics. In Proceedings of the SPIE Conference on Lasers in Dentistry XXV, San Francisco, CA, USA, 3 February 2019; Volume 10857. [Google Scholar]
- Kasparova, M.; Grafova, L.; Dvorak, P.; Dostalova, T.; Prochazka, A.; Eliasova, H.; Prusa, J.; Kakawand, S. Possibility of reconstruction of dental plaster cast from 3D digital study models. Biomed. Eng. Online 2013, 12, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.-C.; Li, P.-L.; Chu, F.-T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop. 2019, 80, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Dostalova, T.; Kasparova, M.; Kriz, P.; Halamova, S.; Jelinek, M.; Bradna, P.; Mendricky, J. Intraoral scanner and stereographic 3D print in dentistry-quality and accuracy of model-new laser application in clinical practice. Laser Phys. 2018, 28, 125602. [Google Scholar] [CrossRef]
- Stratasys. FDM Thermoplastics Material Overview. Available online: http://www.stratasys.com/materials/fdm (accessed on 6 June 2020).
- Stratasys. Dental Molding in Digital Dentistry. Available online: http://www.stratasys.com/materials/polyjet/dental-material (accessed on 10 June 2020).
- Formlabs. Professional 3D Printing Materials for Digital Dentistry. Available online: https://formlabs.com/materials/dentistry/ (accessed on 6 June 2020).
- Stratasys. Biocompatible Materials used in 3D Printing. Available online: http://www.stratasys.com/materials/polyjet/bio-compatible (accessed on 20 May 2020).
- Prochazka, A.; Dostalova, T.; Kasparova, M.; Vysata, O.; Charvatova, H.; Sanei, S.; Marik, V. Augmented Reality Implementations in Stomatology. Appl. Sci. 2019, 9, 2929. [Google Scholar] [CrossRef]
- Kerckhofs, G.; Pyka, G.; Moesen, M.; Van Bael, S.; Schrooten, J.; Wevers, M. High-Resolution Microfocus X-Ray Computed Tomography for 3D Surface Roughness Measurements of Additive Manufactured Porous Materials. Adv. Eng. Mater. 2013, 15, 153–158. [Google Scholar] [CrossRef]
- Cruz, N.; Martins, M.I.; Domingos Santos, J.; Gil Mur, J.; Tondela, J.P. Surface Comparison of Three Different Commercial Custom-Made Titanium Meshes Produced by SLM for Dental Applications. Materials 2020, 13, 2177. [Google Scholar] [CrossRef]
- Kuru, I.; Maier, H.; Müller, M.; Lenarz, T.; Lueth, T.C. A 3D-printed functioning anatomical human middle ear model. Hear. Res. 2016, 340, 204–213. [Google Scholar] [CrossRef]
- Kulczyk, T.; Rychlik, M.; Lorkiewicz-Muszyńska, D.; Abreu-Głowacka, M.; Czajka-Jakubowska, A.; Przystańska, A. Computed Tomography versus Optical Scanning: A Comparison of Different Methods of 3D Data Acquisition for Tooth Replication. BioMed Res. Int. 2019, 2019, 4985121. [Google Scholar] [CrossRef]
- Sommacal, B.; Savic, M.; Filippi, A.; Kühl, S.; Thieringer, F.M. Evaluation of Two 3D Printers for Guided Implant Surgery. Int. J. Oral Maxillofac. Implant. 2018, 33, 743–746. [Google Scholar] [CrossRef]
- Matta, R.E.; Adler, W.; Wichmann, M.; Heckmann, S.M. Accuracy of impression scanning compared with stone casts of implant impressions. J. Prosthet. Dent. 2017, 117, 507–512. [Google Scholar] [CrossRef]
- Jang, Y.; Sim, J.Y.; Park, J.K.; Kim, W.C.; Kim, H.Y.; Kim, J.H. Accuracy of 3-unit fixed dental prostheses fabricated on 3D-printed casts. J. Prosthet. Dent. 2020, 123, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Shulev, A.; Roussev, I.; Karpuzov, S.; Stoilov, G.; Ignatova, D. Roughness Measurement of Dental Materials. J. Theor. Appl. Mech. 2016, 46, 27–36. [Google Scholar] [CrossRef]
- Erpaçal, B.; Adıgüzel, Ö.; Cangül, S. The use of micro-computed tomography in dental applications. Int. Dent. Res. 2019, 9, 78–91. [Google Scholar] [CrossRef]
- Paderova, J.; Drabova, J.; Holubova, A.; Vlckova, M.; Havlovicova, M.; Gregorova, A.; Pourova, R.; Romankova, V.; Moslerova, V.; Geryk, J.; et al. Under the mask of Kabuki syndrome: Elucidation of genetic-and phenotypic heterogeneity in patients with Kabuki-like phenotype. Eur. J. Med. Genet. 2018, 61, 315–321. [Google Scholar] [CrossRef]
- Wesemann, C.; Muallah, J.; Mah, J.; Bumann, A. Accuracy and efficiency of full-arch digitalization and 3D printing: A comparison between desktop model scanners, an intraoral scanner, a CBCT model scan, and stereolithographic 3D printing. Quintessence Int. 2017, 48, 41–50. [Google Scholar]
- Staderini, E.; De Luca, M.; Candida, E. Lay People Esthetic Evaluation of Primary Surgical Repair on Three-Dimensional Images of Cleft Lip and Palate Patients. Medicina 2019, 55, 576. [Google Scholar] [CrossRef]
| SLS | SLA | FDM | PJ | |
|---|---|---|---|---|
| Section 1.dXYZ.1 | 0.000 | 0.039 | 0.226 | 0.000 |
| Section 1.dXYZ.2 | 0.000 | 0.185 | 0.024 | 0.000 |
| Section 1.dXYZ.3 | 0.000 | 0.260 | 0.000 | 0.000 |
| Section 1.dXYZ.4 | 0.000 | 0.845 | 0.000 | 0.008 |
| Section 1.dXYZ.5 | 0.000 | 0.396 | 0.000 | 0.001 |
| Section 1.dXYZ.6 | 0.000 | 0.587 | 0.001 | 0.069 |
| Section 1.dXYZ.7 | 0.000 | 0.329 | 0.039 | 0.758 |
| Section 1.dXYZ.9 | 0.002 | 0.006 | 0.240 | 0.002 |
| Section 1.dXYZ.10 | 0.002 | 0.008 | 0.004 | 0.000 |
| Section 1.dXYZ.11 | 0.001 | 0.267 | 0.307 | 0.018 |
| Section 1.dXYZ.12 | 0.001 | 0.073 | 0.001 | 0.000 |
| Section 1.dXYZ.13 | 0.000 | 0.041 | 0.002 | 0.000 |
| Section 1.dXYZ.14 | 0.001 | 0.162 | 0.000 | 0.000 |
| Section 1.dXYZ.15 | 0.000 | 0.083 | 0.000 | 0.000 |
| Section 1.dXYZ.17 | 0.000 | 0.011 | 0.001 | 0.145 |
| Section 1.dXYZ.18 | 0.000 | 0.659 | 0.081 | 0.630 |
| Section 1.dXYZ.19 | 0.000 | 0.654 | 0.226 | 0.206 |
| Section 1.dXYZ.20 | 0.000 | 0.294 | 0.063 | 0.093 |
| Section 1.dXYZ.21 | 0.000 | 0.154 | 0.005 | 0.790 |
| Section 1.dXYZ.22 | 0.001 | 0.345 | 0.295 | 0.193 |
| Section 1.dXYZ.23 | 0.011 | 0.837 | 0.171 | 0.034 |
| Section 1.dXYZ.25 | 0.003 | 0.001 | 0.929 | 0.000 |
| Section 1.dXYZ.26 | 0.000 | 0.029 | 1.000 | 0.000 |
| Section 1.dXYZ.27 | 0.001 | 0.120 | 0.557 | 0.010 |
| Section 1.dXYZ.28 | 0.000 | 0.004 | 0.000 | 0.000 |
| Section 1.dXYZ.29 | 0.000 | 0.013 | 0.000 | 0.000 |
| Section 1.dXYZ.30 | 0.001 | 0.309 | 0.000 | 0.004 |
| Section 1.dXYZ.31 | 0.000 | 0.049 | 0.000 | 0.012 |
| MEAN | 0.001 | 0.241 | 0.149 | 0.106 |
| STD | 0.002 | 0.254 | 0.263 | 0.223 |
| Cutoff | Ra (nm) in Direction of Printing | |||
|---|---|---|---|---|
| SLA | SLS | FDM | PJ | |
| 25 | 0.19 | 0.69 | 1.09 | 1.80 |
| 80 | 0.65 | 4.30 | 4.78 | 5.35 |
| 250 | 1.31 | 10.20 | 8.74 | 12.10 |
| 800 | 2.37 | 19.35 | 12.80 | 14.00 |
| Cutoff | Ra (nm) Perpendicular to the Direction of Printing | |||
|---|---|---|---|---|
| SLA | SLS | FDM | PJ | |
| 25 | 0.08 | 1.15 | 0.05 | 0.33 |
| 80 | 0.31 | 4.10 | 0.33 | 0.63 |
| 250 | 1.35 | 10.30 | 0.65 | 4.09 |
| 800 | 3.66 | 16.95 | 4.33 | 11.45 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eliasova, H.; Dostalova, T.; Jelinek, M.; Remsa, J.; Bradna, P.; Prochazka, A.; Kloubcova, M. Surface Morphology of Three-Dimensionally Printed Replicas of Upper Dental Arches. Appl. Sci. 2020, 10, 5708. https://doi.org/10.3390/app10165708
Eliasova H, Dostalova T, Jelinek M, Remsa J, Bradna P, Prochazka A, Kloubcova M. Surface Morphology of Three-Dimensionally Printed Replicas of Upper Dental Arches. Applied Sciences. 2020; 10(16):5708. https://doi.org/10.3390/app10165708
Chicago/Turabian StyleEliasova, Hana, Tatjana Dostalova, Miroslav Jelinek, Jan Remsa, Pavel Bradna, Ales Prochazka, and Magdalena Kloubcova. 2020. "Surface Morphology of Three-Dimensionally Printed Replicas of Upper Dental Arches" Applied Sciences 10, no. 16: 5708. https://doi.org/10.3390/app10165708
APA StyleEliasova, H., Dostalova, T., Jelinek, M., Remsa, J., Bradna, P., Prochazka, A., & Kloubcova, M. (2020). Surface Morphology of Three-Dimensionally Printed Replicas of Upper Dental Arches. Applied Sciences, 10(16), 5708. https://doi.org/10.3390/app10165708






