An eLORETA Longitudinal Analysis of Resting State EEG Rhythms in Alzheimer’s Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. EEG Data
2.3. LORETA
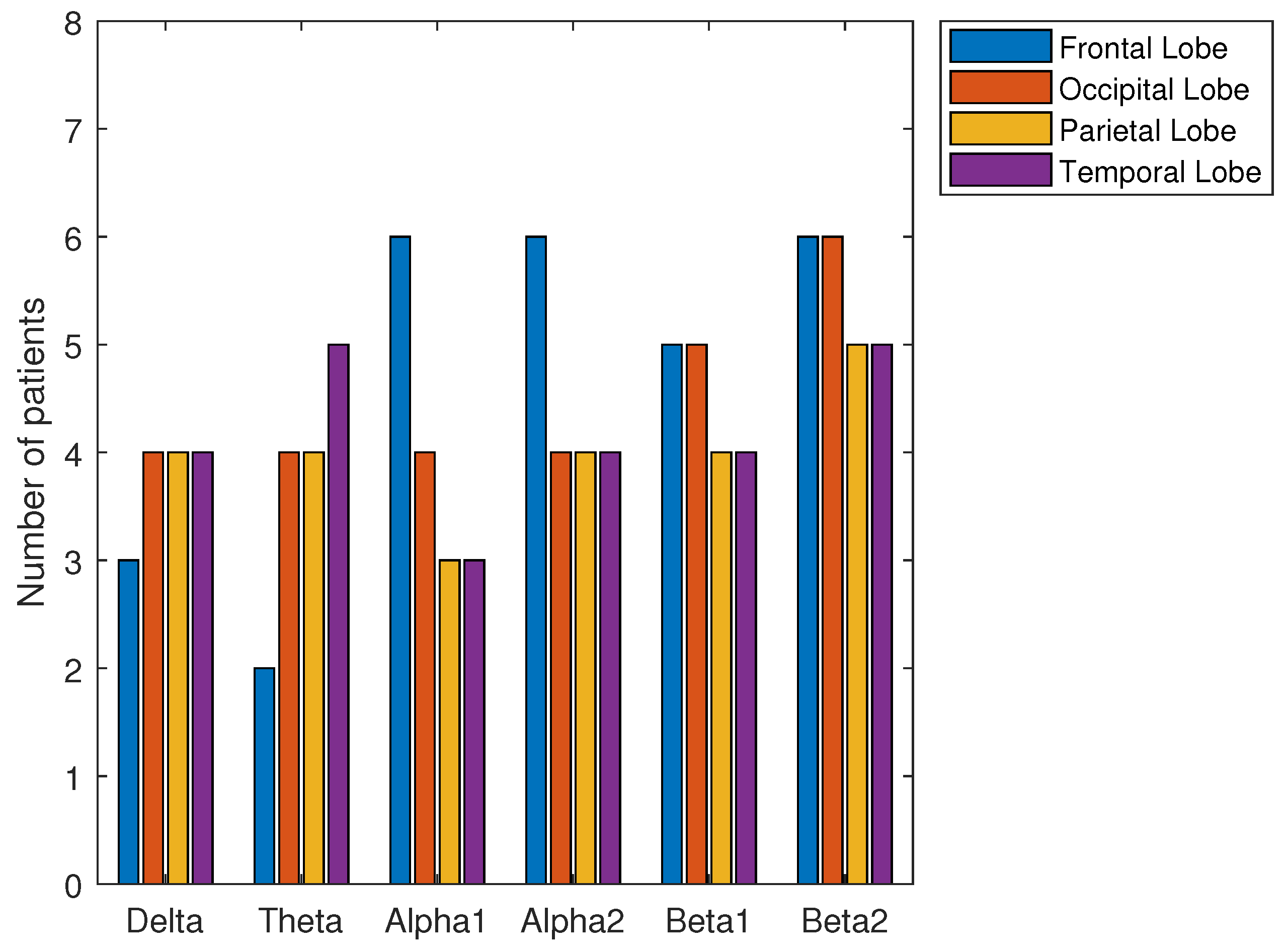
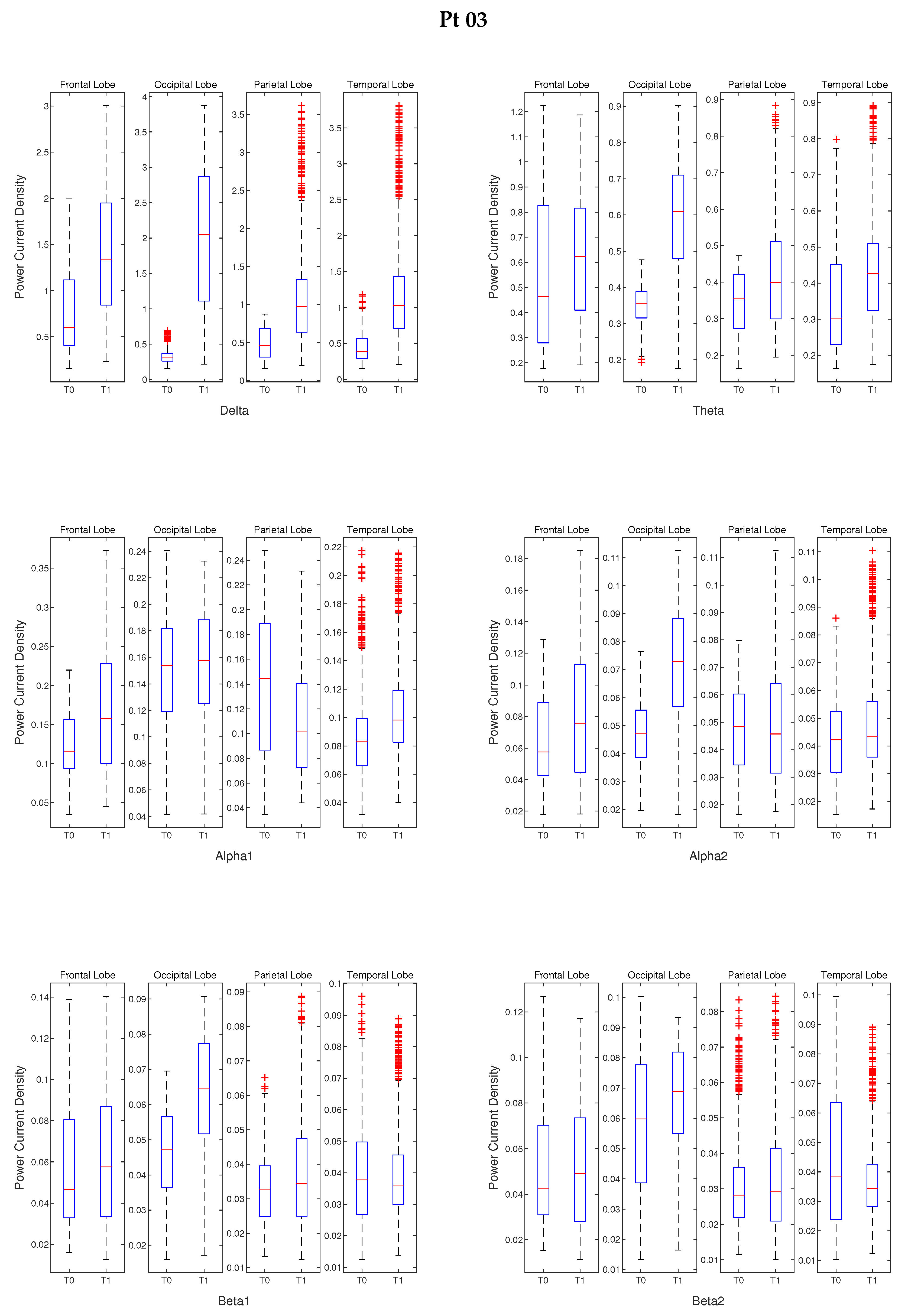
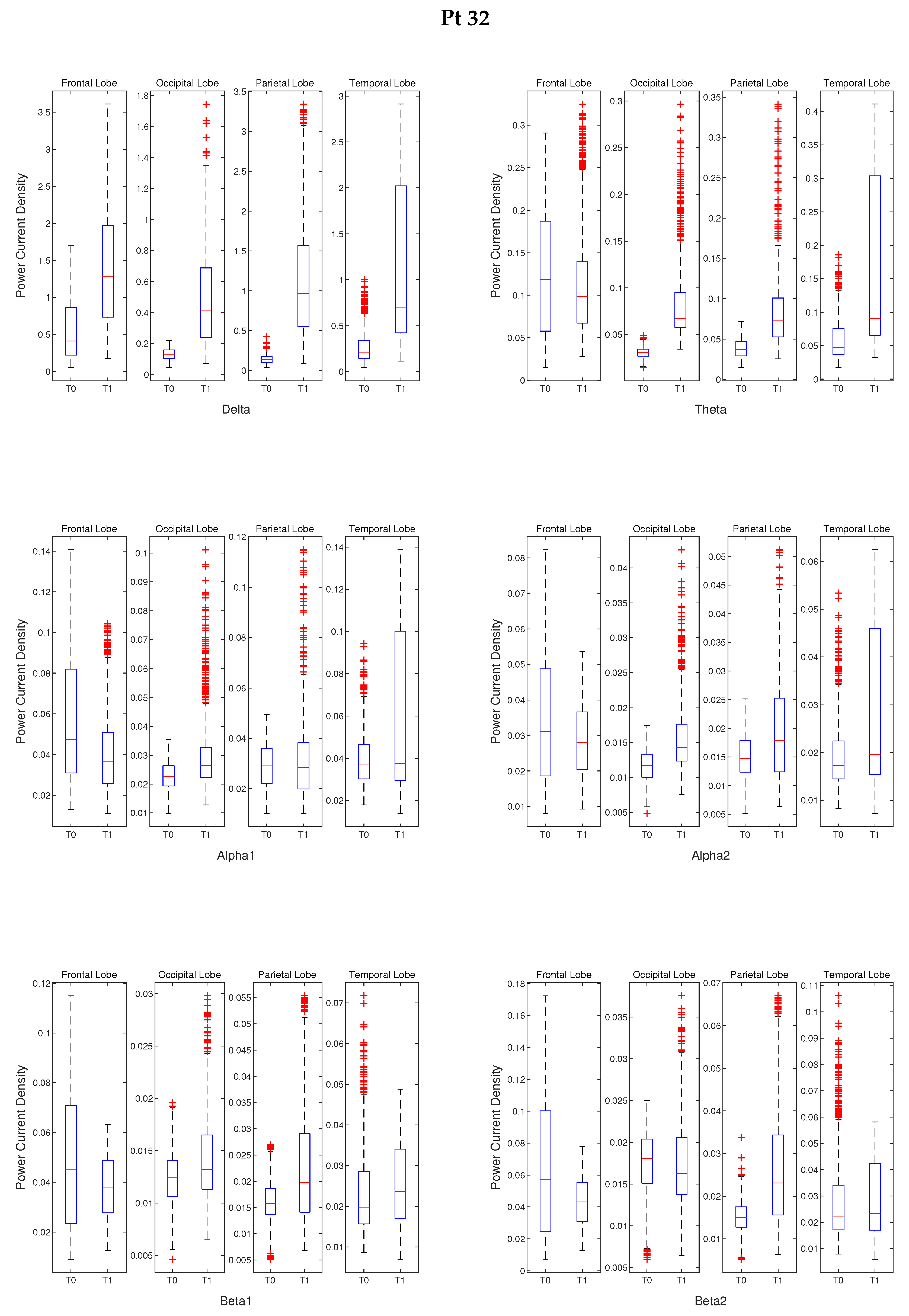
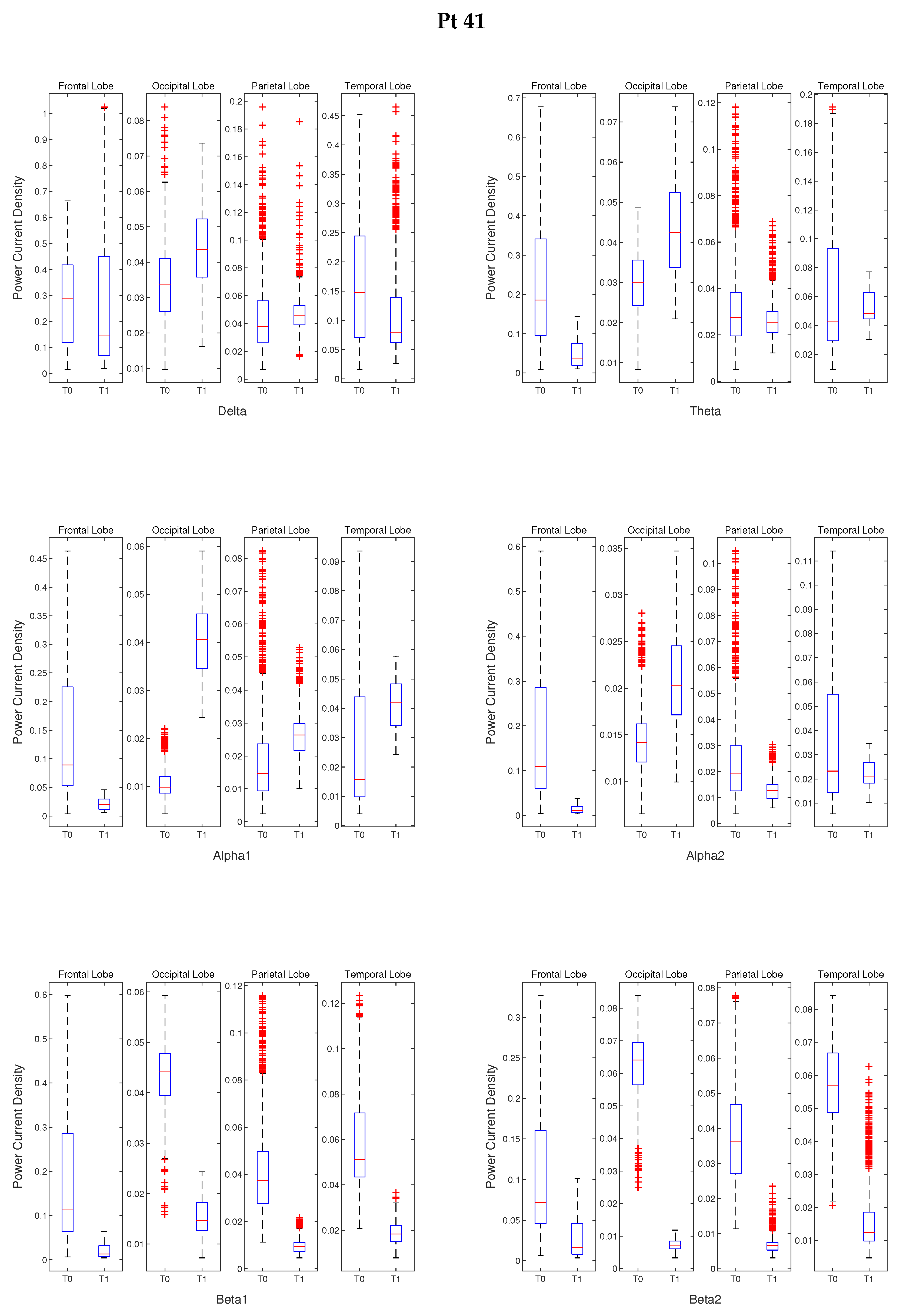
3. Results
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Patient ID | Delta | Theta | ||||||
|---|---|---|---|---|---|---|---|---|
| F. L. | O. L. | P. L. | T. L. | F. L. | O. L. | P. L. | T. L. | |
| Pt 03 | 8.75 × 10 | 1.12 × 10 | 2.82 × 10 | 7.55 × 10 | 1.54 × 10 | 1.49 × 10 | 5.13 × 10 | 4.16 × 10 |
| Pt 32 | 2.38 × 10 | 6.10 × 10 | 0 | 2.12 × 10 | 2.73 × 10 | 2.90 × 10 | 1.82 × 10 | 2.54 × 10 |
| Pt 41 | 3.22 × 10 | 2.78 × 10 | 2.37 × 10 | 3.382 × 10 | 0 | 6.27 × 10 | 8.97 × 10 | 5.55 × 10 |
| Pt 51 | 0 | 4.60 × 10 | 0 | 0 | 0 | 4.60 × 10 | 0 | 0 |
| Pt 71 | 8.15 × 10 | 2.31 × 10 | 4.56 × 10 | 1.37 × 10 | 7.94 × 10 | 5.59 × 10 | 6.23 × 10 | 1.13 × 10 |
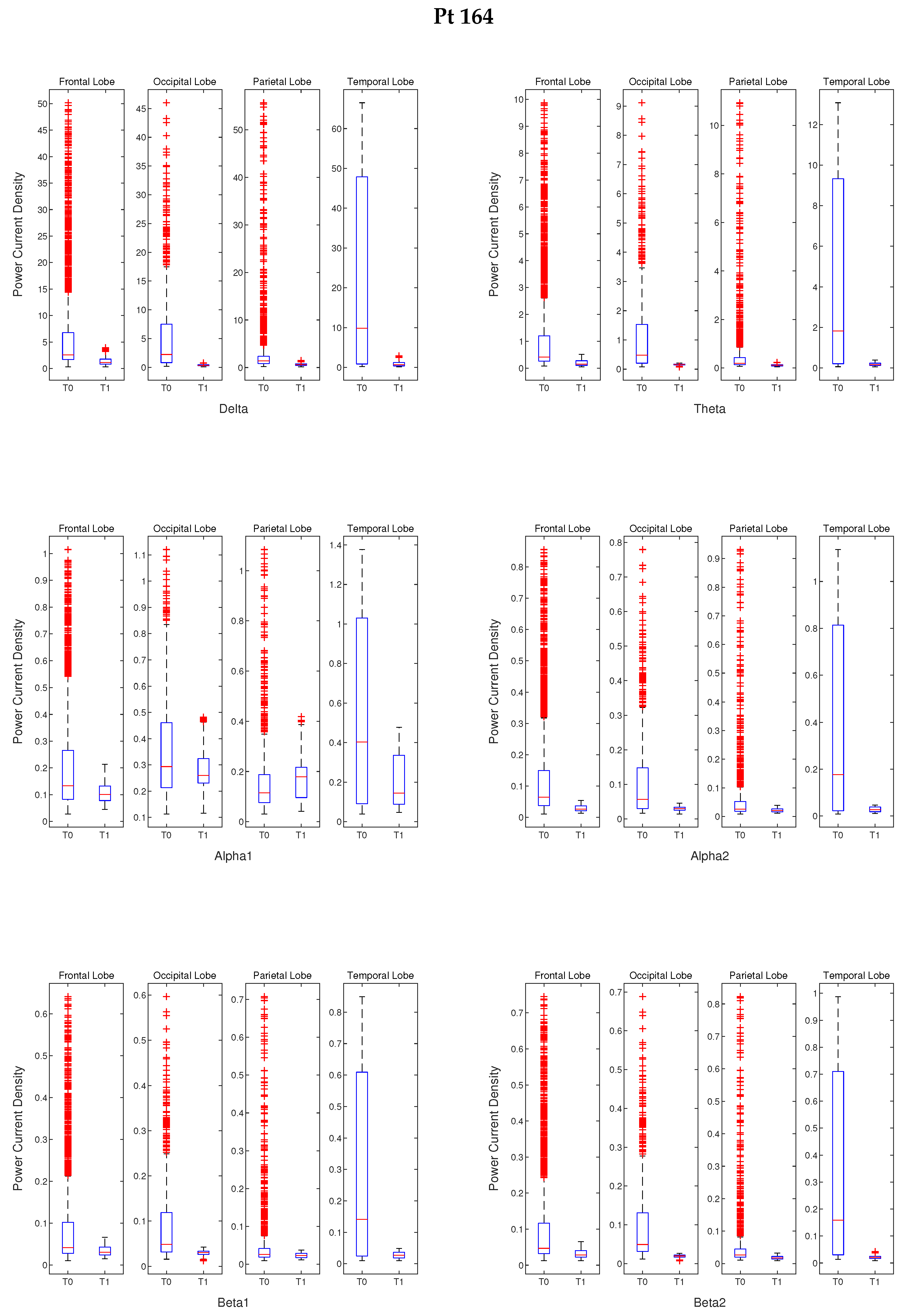
| Pt 164 | 3.87× 10 | 9.26 × 10 | 4.17 × 10 | 1.55 × 10 | 0 | 1.39 × 10 | 4.16 × 10 | 2.62 × 10 |
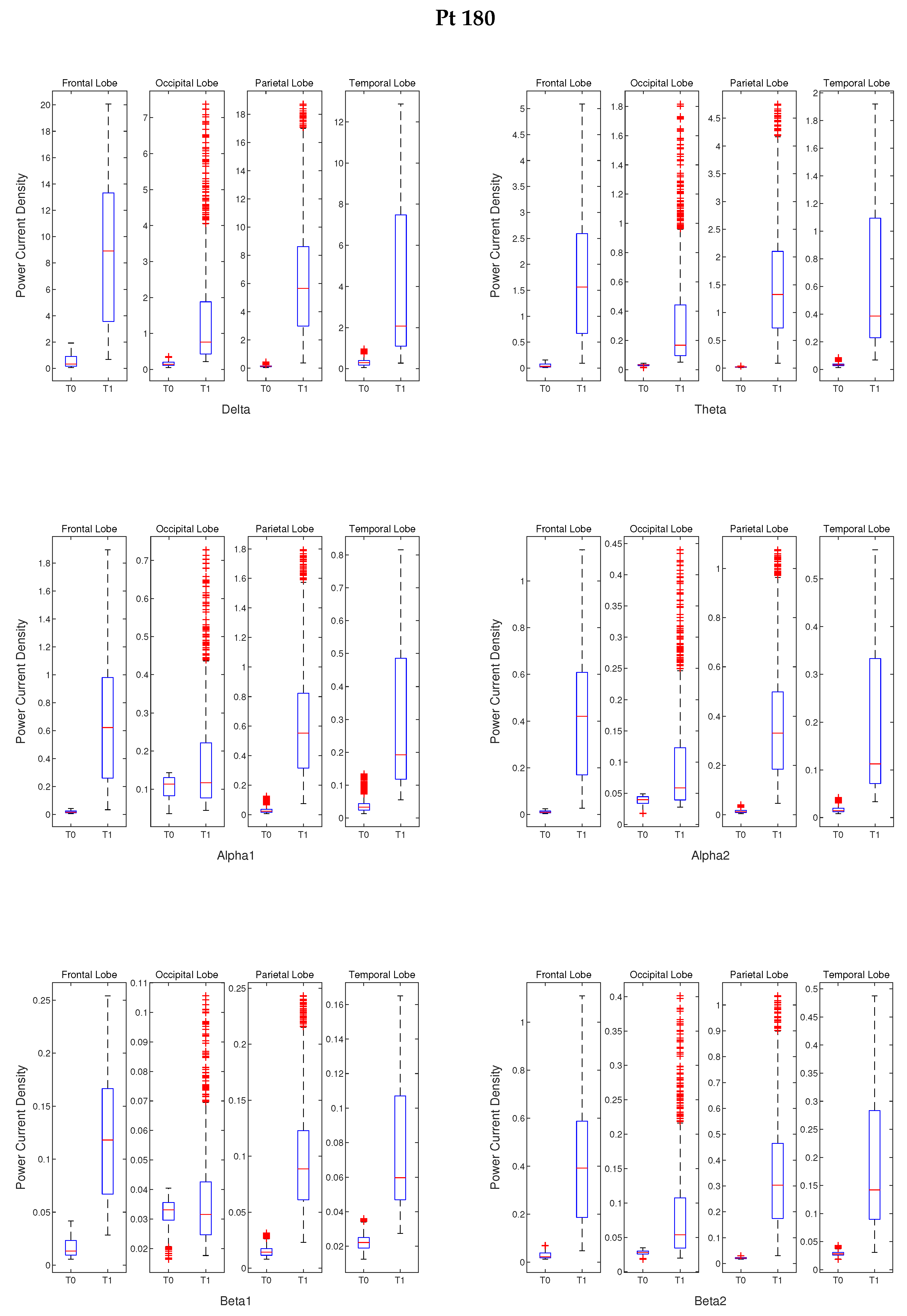
| Pt 180 | 0 | 2.66 × 10 | 0 | 0 | 0 | 4.60 × 10 | 0 | 0 |
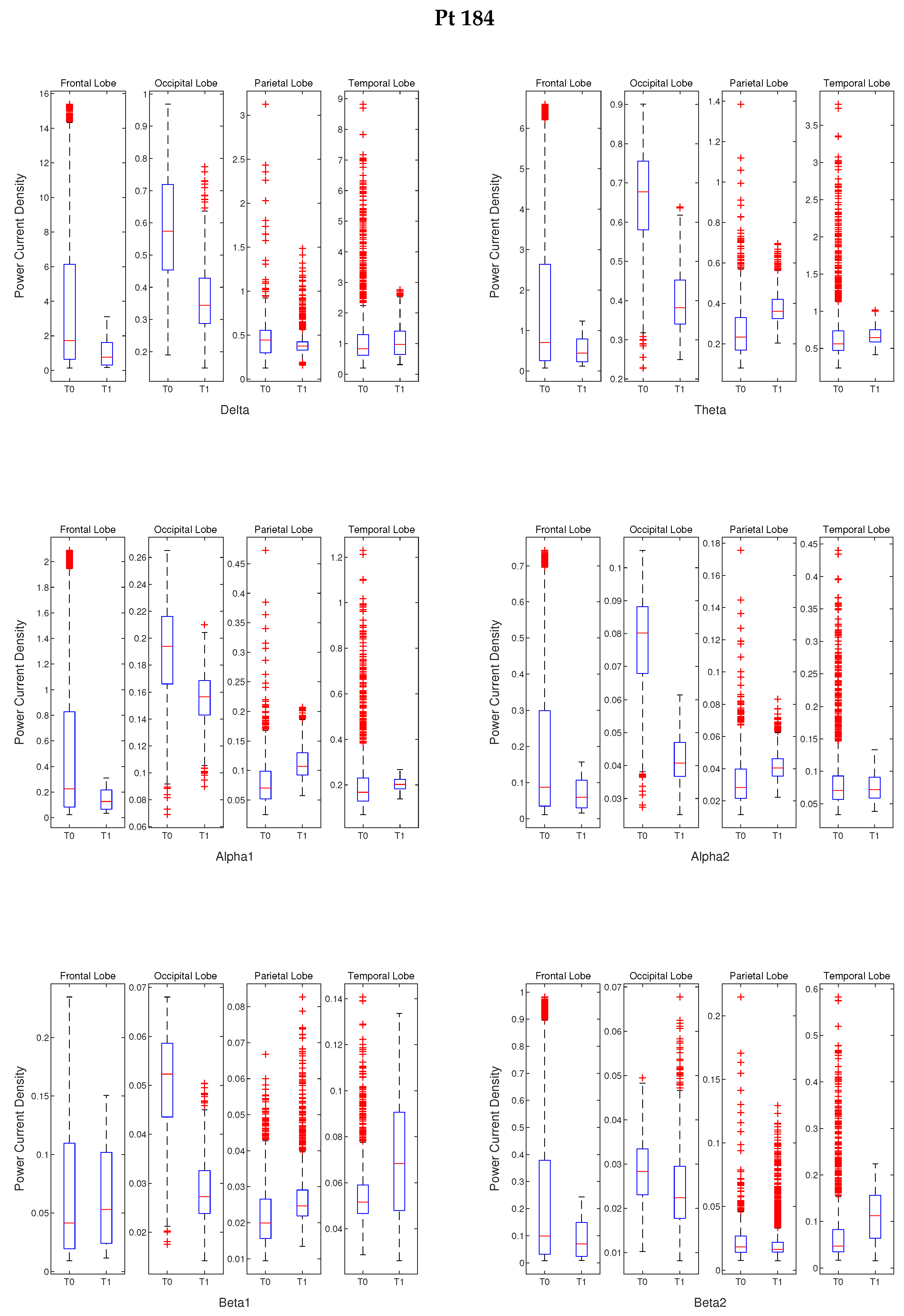
| Pt 184 | 1.05 × 10 | 7.47 × 10 | 7.11 × 10 | 3.80 × 10 | 1.15 × 10 | 3.22 × 10 | 4.31 × 10 | 6.08 × 10 |
| Patient ID | Alpha 1 | Alpha 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| F. L. | O. L. | P. L. | T. L. | F. L. | O. L. | P. L. | T. L. | |
| Pt 03 | 7.81 × 10 | 0.0511 | 3.42 × 10 | 1.23 × 10 | 4.07 × 10 | 4.38 × 10 | 0.4836 | 8.77 × 10 |
| Pt 32 | 2.30 × 10 | 7.24 × 10 | 0.6518 | 2.06 × 10 | 3.78 × 10 | 2.45 × 10 | 3.65 × 10 | 2.24 × 10 |
| Pt 41 | 0 | 4.60 × 10 | 1.37 × 10 | 5.93 × 10 | 0 | 2.07 × 10 | 8.614 × 10 | 5.95 × 10 |
| Pt 51 | 0 | 8.09 × 10 | 0 | 0 | 0 | 5.44 × 10 | 4.74 × 10 | 0 |
| Pt 71 | 1.69 × 10 | 4.72 × 10 | 5.86 × 10 | 1.25 × 10 | 0 | 2.97 × 10 | 1.63 × 10 | 1.55 × 10 |
| Pt 164 | 1.46 × 10 | 5.18 × 10 | 2.09 × 10 | 2.84 × 10 | 5.62 × 10 | 5.06 × 10 | 1.50 × 10 | 6.83 × 10 |
| Pt 180 | 0 | 1.81 × 10 | 0 | 0 | 0 | 1.32 × 10 | 0 | 0 |
| Pt 184 | 1.45 × 10 | 4.03 × 10 | 2.72 × 10 | 1.16 × 10 | 4.80 × 10 | 1.28 × 10 | 2.05 × 10 | 0.7671 |
| Patient ID | Beta 1 | Beta 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| F. L. | O. L. | P. L. | T. L. | F. L. | O. L. | P. L. | T. L. | |
| Pt 03 | 0.0015 | 5.75 × 10 | 8.44 × 10 | 0.8607 | 0.4786 | 1.66 × 10 | 0.0279 | 4.77 × 10 |
| Pt 32 | 1.02 × 10 | 8.53 × 10 | 7.93 × 10 | 5.12 × 10 | 1.17 × 10 | 0.0037 | 3.85 × 10 | 0.0128 |
| Pt 41 | 0 | 9.77 × 10 | 0 | 0 | 0 | 4.60 × 10 | 0 | 0 |
| Pt 51 | 7.31 × 10 | 3.02 × 10 | 6.65 × 10 | 0 | 1.83 × 10 | 6.56 × 10 | 9.64 × 10 | 1.41 × 10 |
| Pt 71 | 6.83 × 10 | 6.19 × 10 | 6.19 × 10 | 1.02 × 10 | 1.58 × 10 | 9.14 × 10 | 0 | 3.09 × 10 |
| Pt 164 | 2.77 × 10 | 4.62 × 10 | 3.14 × 10 | 1.23 × 10 | 3.13 × 10 | 8.86 × 10 | 1.23 × 10 | 2.67 × 10 |
| Pt 180 | 0 | 0.4370 | 0 | 0 | 0 | 1.84 × 10 | 0 | 0 |
| Pt 184 | 0.0016 | 5.54 × 10 | 2.60 × 10 | 6.59 × 10 | 1.45 × 10 | 1.05 × 10 | 2.67 × 10 | 1.47 × 10 |
References
- Weintraub, S.; Wicklund, A.H.; Salmon, D.P. The neuropsychological profile of Alzheimer disease. Cold Spring Harb. Perspect. Med. 2012, 2, a006171. [Google Scholar] [CrossRef]
- Sperling, R.A.; Aisen, P.S.; Beckett, L.A.; Bennett, D.A.; Craft, S.; Fagan, A.M.; Iwatsubo, T.; Jack, C.R., Jr.; Kaye, J.; Montine, T.J.; et al. Toward defining the preclinical stages of Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 280–292. [Google Scholar] [CrossRef]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef]
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R., Jr.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 263–269. [Google Scholar] [CrossRef]
- Rossini, P.; Di Iorio, R.; Vecchio, F.; Anfossi, M.; Babiloni, C.; Bozzali, M.; Bruni, A.; Cappa, S.; Escudero, J.; Fraga, F.; et al. Early diagnosis of alzheimer’s disease: The role of biomarkers including advanced EEG signals analysis. An IFCN-sponsored panel of Experts. Clin. Neurophysiol. 2020, 131, 1287–1310. [Google Scholar] [CrossRef]
- McGinnis, S.M. Neuroimaging in neurodegenerative dementias. In Seminars in Neurology; Thieme Medical Publishers: New York, NY, USA, 2012; Volume 32, pp. 347–360. [Google Scholar]
- Bozzali, M.; Serra, L.; Cercignani, M. Quantitative MRI to understand Alzheimer’s disease pathophysiology. Curr. Opin. Neurol. 2016, 29, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, L.; Chiotis, K.; Alongi, P.; Almkvist, O.; Wall, A.; Cerami, C.; Bettinardi, V.; Gianolli, L.; Nordberg, A.; Perani, D. A cross-validation of FDG-and amyloid-PET biomarkers in mild cognitive impairment for the risk prediction to dementia due to Alzheimer’s disease in a clinical setting. J. Alzheimers Dis. 2017, 59, 603–614. [Google Scholar] [CrossRef] [PubMed]
- Pillai, J.; Sperling, M.R. Interictal EEG and the diagnosis of epilepsy. Epilepsia 2006, 47, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Mammone, N.; De Salvo, S.; Ieracitano, C.; Marino, S.; Cartella, E.; Bramanti, A.; Giorgianni, R.; Morabito, F.C. Compressibility of High-Density EEG Signals in Stroke Patients. Sensors 2018, 18, 4107. [Google Scholar] [CrossRef] [PubMed]
- Wolters, C.H.; Anwander, A.; Tricoche, X.; Weinstein, D.; Koch, M.A.; Macleod, R.S. Influence of tissue conductivity anisotropy on EEG/MEG field and return current computation in a realistic head model: A simulation and visualization study using high-resolution finite element modeling. NeuroImage 2006, 30, 813–826. [Google Scholar] [CrossRef] [PubMed]
- Morabito, F.C.; Campolo, M.; Ieracitano, C.; Ebadi, J.M.; Bonanno, L.; Bramanti, A.; Desalvo, S.; Mammone, N.; Bramanti, P. Deep convolutional neural networks for classification of mild cognitive impaired and Alzheimer’s disease patients from scalp EEG recordings. In Proceedings of the 2016 IEEE 2nd International Forum on Research and Technologies for Society and Industry Leveraging a better tomorrow (RTSI), Bologna, Italy, 7–9 September 2016; pp. 1–6. [Google Scholar]
- Mammone, N.; Ieracitano, C.; Adeli, H.; Bramanti, A.; Morabito, F.C. Permutation Jaccard distance-based hierarchical clustering to estimate EEG network density modifications in MCI subjects. IEEE Trans. Neural Networks Learn. Syst. 2018, 29, 5122–5135. [Google Scholar] [CrossRef] [PubMed]
- Mammone, N.; De Salvo, S.; Bonanno, L.; Ieracitano, C.; Marino, S.; Marra, A.; Bramanti, A.; Morabito, F.C. Brain network analysis of compressive sensed high-density EEG signals in AD and MCI subjects. IEEE Trans. Ind. Inform. 2018, 15, 527–536. [Google Scholar] [CrossRef]
- La Foresta, F.; Morabito, F.C.; Marino, S.; Dattola, S. High-density EEG signal processing based on active-source reconstruction for brain network analysis in alzheimer’s disease. Electronics 2019, 8, 1031. [Google Scholar] [CrossRef]
- Ieracitano, C.; Mammone, N.; Hussain, A.; Morabito, F.C. A novel multi-modal machine learning based approach for automatic classification of EEG recordings in dementia. Neural Netw. 2020, 123, 176–190. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wahlund, L.O.; Dierks, T.; Julin, P.; Winblad, B.; Jelic, V. Discrimination of Alzheimer’s disease and mild cognitive impairment by equivalent EEG sources: A cross-sectional and longitudinal study. Clin. Neurophysiol. 2000, 111, 1961–1967. [Google Scholar] [CrossRef]
- Moretti, D.V.; Babiloni, C.; Binetti, G.; Cassetta, E.; Dal Forno, G.; Ferreric, F.; Ferri, R.; Lanuzza, B.; Miniussi, C.; Nobili, F.; et al. Individual analysis of EEG frequency and band power in mild Alzheimer’s disease. Clin. Neurophysiol. 2004, 115, 299–308. [Google Scholar] [CrossRef]
- Van der Hiele, K.; Vein, A.; Reijntjes, R.; Westendorp, R.; Bollen, E.; Van Buchem, M.; Van Dijk, J.; Middelkoop, H. EEG correlates in the spectrum of cognitive decline. Clin. Neurophysiol. 2007, 118, 1931–1939. [Google Scholar] [CrossRef]
- Czigler, B.; Csikós, D.; Hidasi, Z.; Gaál, Z.A.; Csibri, É.; Kiss, É.; Salacz, P.; Molnár, M. Quantitative EEG in early Alzheimer’s disease patients—power spectrum and complexity features. Int. J. Psychophysiol. 2008, 68, 75–80. [Google Scholar] [CrossRef]
- Gasser, U.S.; Rousson, V.; Hentschel, F.; Sattel, H.; Gasser, T. Alzheimer disease versus mixed dementias: An EEG perspective. Clin. Neurophysiol. 2008, 119, 2255–2259. [Google Scholar] [CrossRef]
- Hsiao, F.J.; Wang, Y.J.; Yan, S.H.; Chen, W.T.; Lin, Y.Y. Altered oscillation and synchronization of default-mode network activity in mild Alzheimer’s disease compared to mild cognitive impairment: An electrophysiological study. PLoS ONE 2013, 8, e68792. [Google Scholar] [CrossRef]
- Jeong, J. EEG dynamics in patients with Alzheimer’s disease. Clin. Neurophysiol. 2004, 115, 1490–1505. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Lizio, R.; Marzano, N.; Capotosto, P.; Soricelli, A.; Triggiani, A.I.; Cordone, S.; Gesualdo, L.; Del Percio, C. Brain neural synchronization and functional coupling in Alzheimer’s disease as revealed by resting state EEG rhythms. Int. J. Psychophysiol. 2016, 103, 88–102. [Google Scholar] [CrossRef] [PubMed]
- Marqui, R.P.; Michel, C.M.; Lehmann, D. Low-resolution electromagnetic tomography—A new method for localizing electrical activity in the brain. Int. J. Psychophysiol. 1994, 18, 49–65. [Google Scholar] [CrossRef]
- Babiloni, C.; Binetti, G.; Cassetta, E.; Cerboneschi, D.; Dal Forno, G.; Del Percio, C.; Ferreri, F.; Ferri, R.; Lanuzza, B.; Miniussi, C.; et al. Mapping distributed sources of cortical rhythms in mild Alzheimer’s disease. A multicentric EEG study. Neuroimage 2004, 22, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Binetti, G.; Cassetta, E.; Dal Forno, G.; Del Percio, C.; Ferreri, F.; Ferri, R.; Frisoni, G.; Hirata, K.; Lanuzza, B.; et al. Sources of cortical rhythms change as a function of cognitive impairment in pathological aging: A multicenter study. Clin. Neurophysiol. 2006, 117, 252–268. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Frisoni, G.B.; Pievani, M.; Vecchio, F.; Lizio, R.; Buttiglione, M.; Geroldi, C.; Fracassi, C.; Eusebi, F.; Ferri, R.; et al. Hippocampal volume and cortical sources of EEG alpha rhythms in mild cognitive impairment and Alzheimer disease. Neuroimage 2009, 44, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Lizio, R.; Carducci, F.; Vecchio, F.; Redolfi, A.; Marino, S.; Tedeschi, G.; Montella, P.; Guizzaro, A.; Esposito, F.; et al. Resting state cortical electroencephalographic rhythms and white matter vascular lesions in subjects with Alzheimer’s disease: An Italian multicenter study. J. Alzheimers Dis. 2011, 26, 331–346. [Google Scholar] [CrossRef]
- Babiloni, C.; Carducci, F.; Lizio, R.; Vecchio, F.; Baglieri, A.; Bernardini, S.; Cavedo, E.; Bozzao, A.; Buttinelli, C.; Esposito, F.; et al. Resting state cortical electroencephalographic rhythms are related to gray matter volume in subjects with mild cognitive impairment and Alzheimer’s disease. Hum. Brain Mapp. 2013, 34, 1427–1446. [Google Scholar] [CrossRef]
- Canuet, L.; Tellado, I.; Couceiro, V.; Fraile, C.; Fernandez-Novoa, L.; Ishii, R.; Takeda, M.; Cacabelos, R. Resting-state network disruption and APOE genotype in Alzheimer’s disease: A lagged functional connectivity study. PLoS ONE 2012, 7, e46289. [Google Scholar] [CrossRef]
- Gianotti, L.R.; Künig, G.; Lehmann, D.; Faber, P.L.; Pascual-Marqui, R.D.; Kochi, K.; Schreiter-Gasser, U. Correlation between disease severity and brain electric LORETA tomography in Alzheimer’s disease. Clin. Neurophysiol. 2007, 118, 186–196. [Google Scholar] [CrossRef]
- Nishida, K.; Yoshimura, M.; Isotani, T.; Yoshida, T.; Kitaura, Y.; Saito, A.; Mii, H.; Kato, M.; Takekita, Y.; Suwa, A.; et al. Differences in quantitative EEG between frontotemporal dementia and Alzheimer’s disease as revealed by LORETA. Clin. Neurophysiol. 2011, 122, 1718–1725. [Google Scholar] [CrossRef] [PubMed]
- Rossini, P.; Del Percio, C.; Pasqualetti, P.; Cassetta, E.; Binetti, G.; Dal Forno, G.; Ferreri, F.; Frisoni, G.; Chiovenda, P.; Miniussi, C.; et al. Conversion from mild cognitive impairment to Alzheimer’s disease is predicted by sources and coherence of brain electroencephalography rhythms. Neuroscience 2006, 143, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Frisoni, G.B.; Vecchio, F.; Lizio, R.; Pievani, M.; Cristina, G.; Fracassi, C.; Vernieri, F.; Rodriguez, G.; Nobili, F.; et al. Stability of clinical condition in mild cognitive impairment is related to cortical sources of alpha rhythms: An electroencephalographic study. Hum. Brain Mapp. 2011, 32, 1916–1931. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Lizio, R.; Del Percio, C.; Marzano, N.; Soricelli, A.; Salvatore, E.; Ferri, R.; Cosentino, F.I.; Tedeschi, G.; Montella, P.; et al. Cortical sources of resting state EEG rhythms are sensitive to the progression of early stage Alzheimer’s disease. J. Alzheimers Dis. 2013, 34, 1015–1035. [Google Scholar] [CrossRef] [PubMed]
- Hämäläinen, M.S.; Ilmoniemi, R.J. Interpreting magnetic fields of the brain: Minimum norm estimates. Med. Biol. Eng. Comput. 1994, 32, 35–42. [Google Scholar] [CrossRef]
- Talairach, J.; Tournoux, P. Co-Planar Stereotaxic Atlas of the Human Brain; Theime: New York, NY, USA, 1988. [Google Scholar]
- Collins, D.L.; Neelin, P.; Peters, T.M.; Evans, A.C. Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J. Comput. Assist. Tomogr. 1994, 18, 192–205. [Google Scholar] [CrossRef]
- Tong, S.; Thakor, N.V. Quantitative EEG Analysis Methods and Clinical Applications; Artech House: Norwood, MA, USA, 2009. [Google Scholar]
- Tikhonov, A.N.; Arsenin, V.Y. Solutions of Ill-Posed Problems; Wiley: New York, NY, USA, 1977; pp. 1–30. [Google Scholar]
- Pascual-Marqui, R.D. Standardized low-resolution brain electromagnetic tomography (sLORETA): Technical details. Methods Find. Exp. Clin. Pharmacol. 2002, 24, 5–12. [Google Scholar]
- Mazziotta, J.; Toga, A.; Evans, A.; Fox, P.; Lancaster, J.; Zilles, K.; Woods, R.; Paus, T.; Simpson, G.; Pike, B.; et al. A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM). Philos. Trans. R. Soc. Lond. Ser. Biol. Sci. 2001, 356, 1293–1322. [Google Scholar] [CrossRef]
- Fuchs, M.; Kastner, J.; Wagner, M.; Hawes, S.; Ebersole, J.S. A standardized boundary element method volume conductor model. Clin. Neurophysiol. 2002, 113, 702–712. [Google Scholar] [CrossRef]
- Dale, A.M.; Liu, A.K.; Fischl, B.R.; Buckner, R.L.; Belliveau, J.W.; Lewine, J.D.; Halgren, E. Dynamic statistical parametric mapping: Combining fMRI and MEG for high-resolution imaging of cortical activity. Neuron 2000, 26, 55–67. [Google Scholar] [CrossRef]
- Pascual-Marqui, R.D. Discrete, 3D distributed, linear imaging methods of electric neuronal activity. Part 1: Exact, zero error localization. arXiv 2007, arXiv:0710.3341. [Google Scholar]
- Jatoi, M.A.; Kamel, N.; Malik, A.S.; Faye, I. EEG based brain source localization comparison of sLORETA and eLORETA. Australas. Phys. Eng. Sci. Med. 2014, 37, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, J.; Chakraborti, S. Nonparametric Statistical Inference; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Dauwels, J.; Vialatte, F.; Cichocki, A. Diagnosis of Alzheimer’s disease from EEG signals: Where are we standing? Curr. Alzheimer Res. 2010, 7, 487–505. [Google Scholar] [CrossRef] [PubMed]
- Dattola, S.; Morabito, F.C.; Mammone, N.; La Foresta, F. Findings about LORETA Applied to High-Density EEG—A Review. Electronics 2020, 9, 660. [Google Scholar] [CrossRef]
- Jatoi, M.A.; Kamel, N.; Malik, A.S.; Faye, I.; Begum, T. A survey of methods used for source localization using EEG signals. Biomed. Signal Process. Control 2014, 11, 42–52. [Google Scholar] [CrossRef]


| Patient ID | Gender | Age |
|---|---|---|
| Pt 03 | M | 68 |
| Pt 32 | M | 78 |
| Pt 41 | M | 78 |
| Pt 51 | F | 72 |
| Pt 71 | F | 79 |
| Pt 164 | M | 76 |
| Pt 180 | F | 78 |
| Pt 184 | F | 69 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dattola, S.; La Foresta, F. An eLORETA Longitudinal Analysis of Resting State EEG Rhythms in Alzheimer’s Disease. Appl. Sci. 2020, 10, 5666. https://doi.org/10.3390/app10165666
Dattola S, La Foresta F. An eLORETA Longitudinal Analysis of Resting State EEG Rhythms in Alzheimer’s Disease. Applied Sciences. 2020; 10(16):5666. https://doi.org/10.3390/app10165666
Chicago/Turabian StyleDattola, Serena, and Fabio La Foresta. 2020. "An eLORETA Longitudinal Analysis of Resting State EEG Rhythms in Alzheimer’s Disease" Applied Sciences 10, no. 16: 5666. https://doi.org/10.3390/app10165666
APA StyleDattola, S., & La Foresta, F. (2020). An eLORETA Longitudinal Analysis of Resting State EEG Rhythms in Alzheimer’s Disease. Applied Sciences, 10(16), 5666. https://doi.org/10.3390/app10165666






