Adaptability Evaluation of Metal-Ceramic Crowns Obtained by Additive and Subtractive Technologies
Abstract
1. Introduction
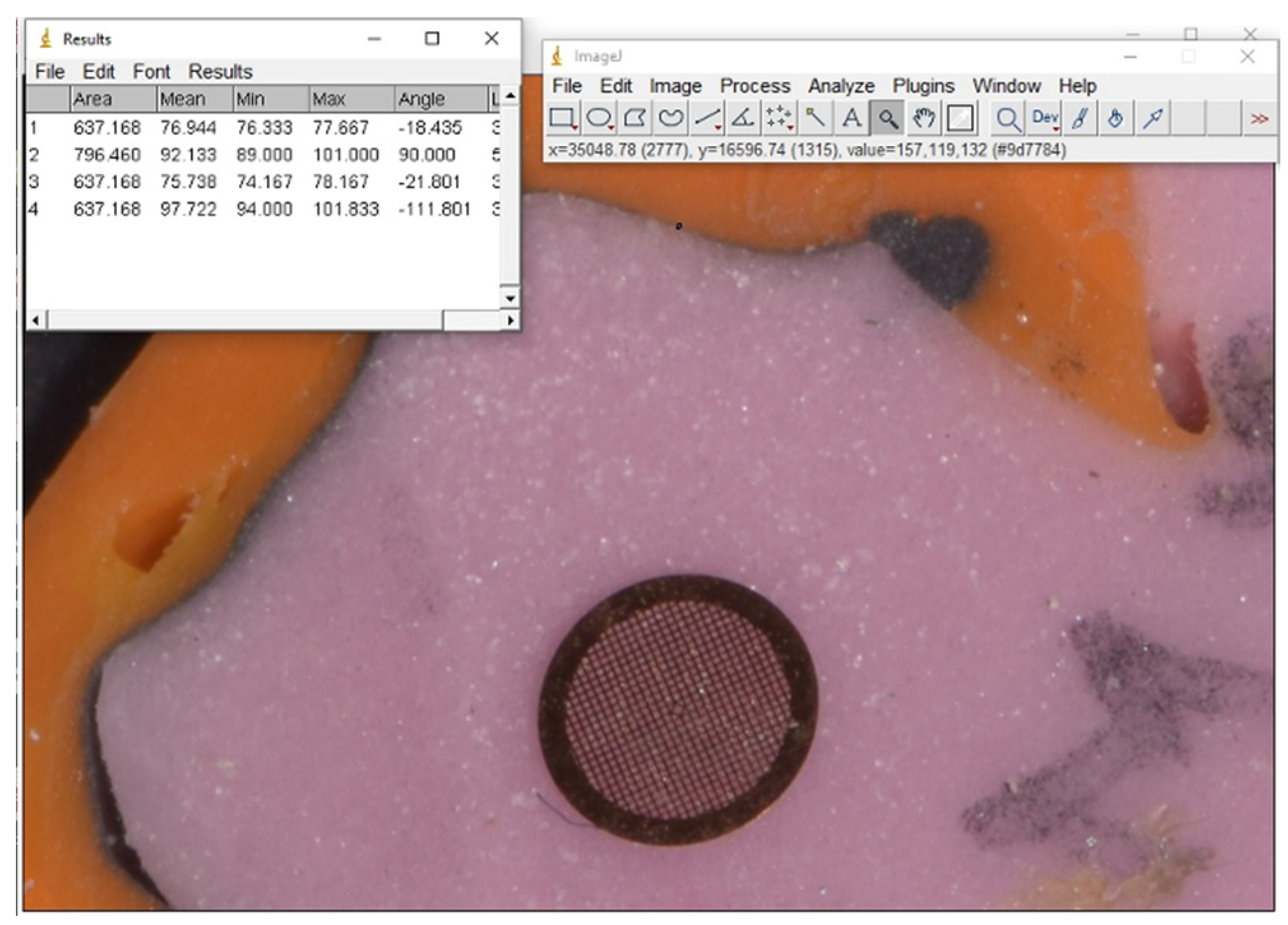
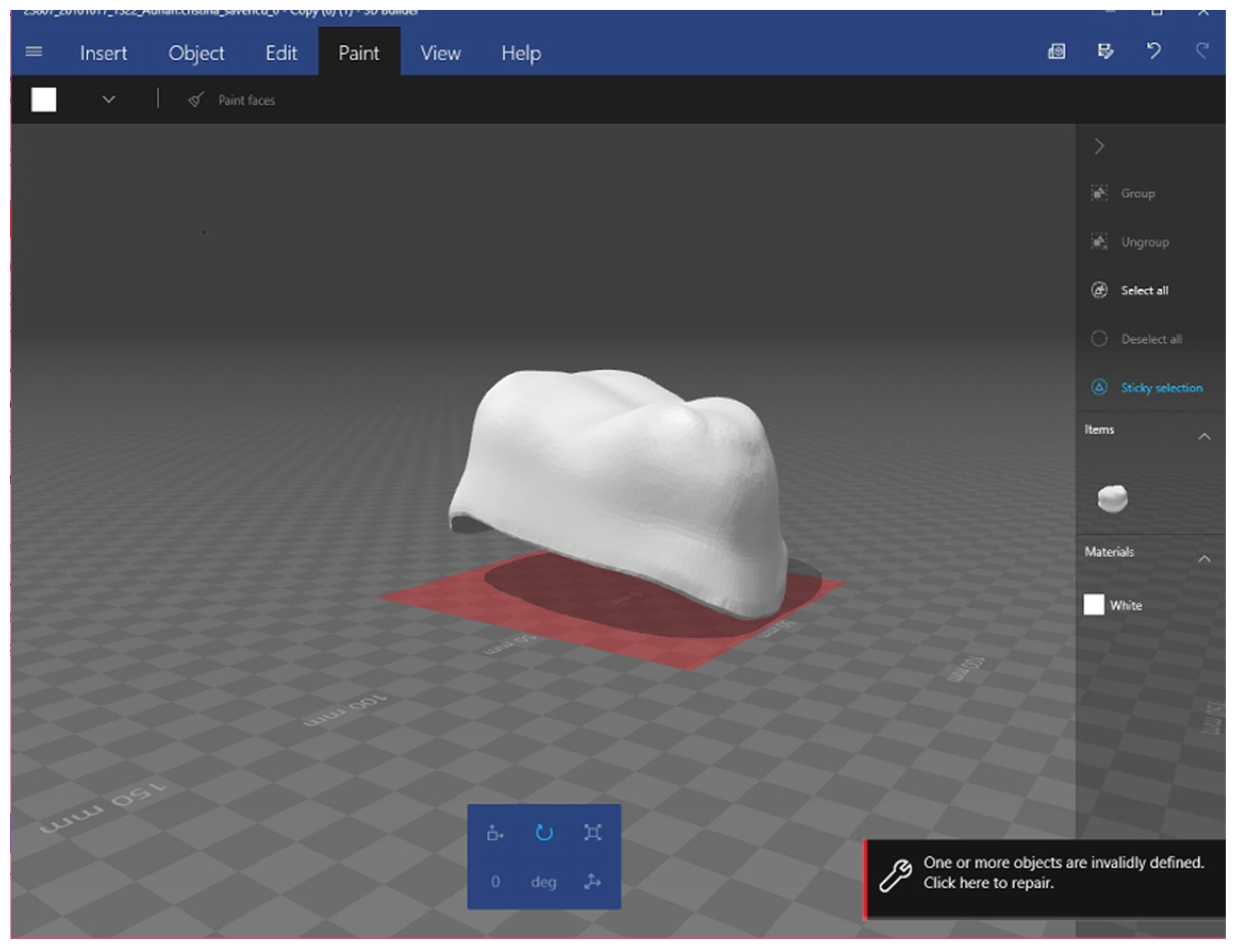
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kim, M.-J.; Choi, Y.-J.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Marginal Accuracy and Internal Fit of 3D Printing Laser-Sintered Co-Cr Alloy Copings. Materials 2017, 10, 93. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5344574/ (accessed on 6 May 2019). [CrossRef] [PubMed]
- Ishida, Y.; Miyasaka, T. Dimensional accuracy of dental casting patterns created by 3D printers. Dent. Mater. J. 2016, 35, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Vojdani, M.; Torabi, K.; Farjood, E.; Khaledi, A. Comparison the Marginal and Internal Fit of Metal Copings Cast from Wax Patterns Fabricated by CAD/CAM and Conventional Wax up Techniques. J. Dent. 2013, 14, 118–129. [Google Scholar]
- Porcelain-Fused-to-Metal Crowns Versus All-Ceramic Crowns: A Review of the Clinical and Cost-Effectiveness; CADTH Rapid Response Reports; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2015. Available online: http://www.ncbi.nlm.nih.gov/books/NBK304693/ (accessed on 1 July 2020).
- Kim, K.-B.; Kim, J.-H.; Kim, W.-C.; Kim, J.-H. Three-dimensional evaluation of gaps associated with fixed dental prostheses fabricated with new technologies. J. Prosthet. Dent. 2014, 112, 1432–1436. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Caradonna, G.; Biancardino, M.; De Lillo, A.; Troiano, G.; Guida, L. Digital versus conventional workflow for the fabrication of multiunit fixed prostheses: A systematic review and meta-analysis of vertical marginal fit in controlled in vitro studies. J. Prosthet. Dent. 2019, 122, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Benic, G.I.; Sailer, I.; Zeltner, M.; Gütermann, J.N.; Özcan, M.; Mühlemann, S. Randomized controlled clinical trial of digital and conventional workflows for the fabrication of zirconia-ceramic fixed partial dentures. Part III: Marginal and internal fit. J. Prosthet. Dent. 2019, 121, 426–431. [Google Scholar] [CrossRef]
- Bhaskaran, E.; Azhagarasan, N.S.; Miglani, S.; Ilango, T.; Krishna, G.P.; Gajapathi, B. Comparative Evaluation of Marginal and Internal Gap of Co-Cr Copings Fabricated from Conventional Wax Pattern, 3D Printed Resin Pattern and DMLS Tech: An In Vitro Study. J. Indian Prosthodont. Soc. 2013, 13, 189–195. [Google Scholar] [CrossRef]
- In Vitro Assessment of the Marginal and Internal Fits of Interim Implant Restorations Fabricated with Different Methods. J. Prosthet. Dent. Available online: https://www.thejpd.org/article/S0022-391330009-9/fulltext (accessed on 1 July 2020).
- Pompa, G.; Di Carlo, S.; De Angelis, F.; Cristalli, M.P.; Annibali, S. Comparison of Conventional Methods and Laser-Assisted Rapid Prototyping for Manufacturing Fixed Dental Prostheses: An In Vitro Study. BioMed. Res. Int. 2015, 2015, 318097. [Google Scholar] [CrossRef]
- Nesse, H.; Ulstein, D.M.Å.; Vaage, M.M.; Øilo, M. Internal and marginal fit of cobalt-chromium fixed dental prostheses fabricated with 3 different techniques. J. Prosthet. Dent. 2015, 114, 686–692. [Google Scholar] [CrossRef]
- Ng, J.; Ruse, D.; Wyatt, C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J. Prosthet. Dent. 2014, 112, 555–560. [Google Scholar] [CrossRef]
- Costea, C.M.; Badea, M.E.; Vasilache, S.; Mesaroş, M. Effects of CO-CR discrepancy in daily orthodontic treatment planning. Clujul Med. 2016, 89, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Douglas, R.D.; Hopp, C.D.; Augustin, M.A. Dental students’ preferences and performance in crown design: Conventional wax-added versus CAD. J. Dent. Educ. 2014, 78, 1663–1672. [Google Scholar] [CrossRef] [PubMed]
- Li, K.C.; Prior, D.J.; Waddell, J.N.; Swain, M.V. Comparison of the microstructure and phase stability of as-cast, CAD/CAM and powder metallurgy manufactured Co-Cr dental alloys. Dent. Mater. 2015, 31, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Porojan, L.; Topală, F.; Porojan, S.; Savencu, C. Effect of frame design and veneering material on biomechanical behavior of zirconia dental crowns veneered with overpressing ceramics. Dent. Mater. J. 2017, 36, 275–281. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xu, D.; Xiang, N.; Wei, B. The marginal fit of selective laser melting-fabricated metal crowns: An in vitro study. J. Prosthet. Dent. 2014, 112, 1437–1440. [Google Scholar] [CrossRef] [PubMed]
- Koç, E.; Öngül, D.; Şermet, B. A comparative study of marginal fit of copings prepared with various techniques on different implant abutments. Dent. Mater. J. 2016, 35, 447–453. [Google Scholar] [CrossRef]
- Digital Evaluation of Marginal and Internal Fit of Single-Crown Fixed Dental Prostheses. Eur. J. Oral Sci. 2018, 126, 517. [CrossRef]
- Güngör, M.B.; Doğan, A.; Bal, B.T.; Nemli, S.K. Evaluation of marginal and internal adaptations of posterior all-ceramic crowns fabricated with chair-side CAD/CAM system: An in vitro study. Acta Odontol. Turc. 2017, 35, 1–8. [Google Scholar]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and Reliability of Methods to Measure Marginal Adaptation of Crowns and FDPs: A Literature Review: Methods to Measure Marginal Adaptation of Crowns and FDPs. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef]
- Tamac, E.; Toksavul, S.; Toman, M. Clinical marginal and internal adaptation of CAD/CAM milling, laser sintering, and cast metal ceramic crowns. J. Prosthet. Dent. 2014, 112, 909–913. [Google Scholar] [CrossRef]
- Son, K.; Lee, S.; Kang, S.H.; Park, J.; Lee, K.-B.; Jeon, M.; Yun, B.J. A Comparison Study of Marginal and Internal Fit Assessment Methods for Fixed Dental Prostheses. J. Clin. Med. 2019, 8, 785. [Google Scholar] [CrossRef] [PubMed]
- Halawani, S.; Al-Harbi, S. Marginal adaptation of fixed prosthodontics. Int. J. Med. Dev. Ctries. 2017, 1, 78–84. [Google Scholar] [CrossRef]
- Riccitiello, F.; Amato, M.; Leone, R.; Spagnuolo, G.; Sorrentino, R. In vitro Evaluation of the Marginal Fit and Internal Adaptation of Zirconia and Lithium Disilicate Single Crowns: Micro-CT Comparison between Different Manufacturing Procedures. Open Dent. J. 2018, 12, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Evaluation of Marginal and Internal Gaps of Ni-Cr and Co-Cr Alloy Copings Manufactured by Microstereolithography. Abstract Europe PMC. Available online: https://europepmc.org/article/med/28680548 (accessed on 1 July 2020).
- Dauti, R.; Cvikl, B.; Lilaj, B.; Heimel, P.; Moritz, A.; Schedle, A. Micro-CT evaluation of marginal and internal fit of cemented polymer infiltrated ceramic network material crowns manufactured after conventional and digital impressions. J. Prosthodont. Res. 2019, 63, 40–46. [Google Scholar] [CrossRef]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef]
- Harish, V.; Mohamed Ali, S.A.; Jagadesan, N.; Mohamed Ifthikar, S.S.; Debasish Basak, F.H. Evaluation of Internal and Marginal Fit of Two Metal Ceramic System—In Vitro Study. J. Clin. Diagn. Res. 2014, 8, ZC53. Available online: http://jcdr.net/article_fulltext.asp?issn=0973-709x&year=2014&volume=8&issue=12&page=ZC53&issn=0973-709x&id=5300 (accessed on 1 July 2020).
- Shokry, T.E.; Attia, M.; Mosleh, I.; Elhosary, M.; Hamza, T.; Shen, C. Effect of metal selection and porcelain firing on the marginal accuracy of titanium-based metal ceramic restorations. J. Prosthet. Dent. 2010, 103, 45–52. [Google Scholar] [CrossRef]
- Yajvinder, G.V.; Agrawal, A.; Singh, B. Evaluation of Influence of Finish line Design on Marginal Discrepancy of All-ceramics Lithium disilicate Crown restorations using μ-CT. IOP Conf. Ser. Mater. Sci. Eng. 2020, 802, 012003. [Google Scholar] [CrossRef]
- George, E.; Liacouras, P.; Rybicki, F.J.; Mitsouras, D. Measuring and Establishing the Accuracy and Reproducibility of 3D Printed Medical Models. Radiographics 2017, 37, 1424–1450. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, L.; Zhu, J.; Zhang, X. Clinical marginal and internal fit of metal ceramic crowns fabricated with a selective laser melting technology. J. Prosthet. Dent. 2015, 113, 623–627. [Google Scholar] [CrossRef]
- Savencu, C.E.; Porojan, S.; Porojan, L. Analysis of Internal and Marginal fit of Metal-ceramic Crowns During Processing, Using Conventional and Digitized Technologies. Rev. Chim. 2018, 69, 1699–1701. [Google Scholar] [CrossRef]
- US4863538A-Method and Apparatus for Producing Parts by Selective Sintering-Google Patents. Available online: https://patents.google.com/patent/US4863538A/en (accessed on 2 July 2020).
- Akova, T.; Ucar, Y.; Tukay, A.; Balkaya, M.C.; Brantley, W.A. Comparison of the bond strength of laser-sintered and cast base metal dental alloys to porcelain. Dent. Mater. 2008, 24, 1400–1404. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-K.; Lee, W.-S.; Kim, H.-Y.; Kim, W.-C.; Kim, J.-H. Accuracy evaluation of metal copings fabricated by computer-aided milling and direct metal laser sintering systems. J. Adv. Prosthodont. 2015, 7, 122. [Google Scholar] [CrossRef] [PubMed]
- Alshalan, A.; Almutair, A.; Awad, D.; Alshmlani, M.; Abbas, S.B.; Asif, Z. Marginal and Internal Fit of CAD CAM System. Int. J. Dent. Oral Health 2019, 5, 9. [Google Scholar]
- Gouveia, D.N.M.; Razzoog, M.E.; Alfaro, M.F. A fully digital approach to fabricating a CAD-CAM ceramic crown to fit an existing removable partial denture. J. Prosthet. Dent. 2019, 121, 571–575. [Google Scholar] [CrossRef]
- Haider, Y.; Dimashkieh, M.; Rayyan, M. Survey of Dental Materials Used by Dentists for Indirect Restorations in Saudi Arabia. Int. J. Prosthodont. 2017, 30, 83–85. [Google Scholar] [CrossRef]
- Persson, A.S.K.; Andersson, M.; Odén, A.; Sandborgh-Englund, G. Computer aided analysis of digitized dental stone replicas by dental CAD/CAM technology. Dent. Mater. 2008, 24, 1123–1130. [Google Scholar] [CrossRef]
- Lopez-Suarez, C.; Gonzalo, E.; Pelaez, J.; Serrano, B.; Suarez, M. Marginal Vertical Discrepancies of Monolithic and Veneered Zirconia and Metal-Ceramic Three-Unit Posterior Fixed Dental Prostheses. Int. J. Prosthodont. 2016, 29, 256–258. [Google Scholar] [CrossRef]
- De França, D.G.B.; Morais, M.H.S.T.; das Neves, F.D.; Barbosa, G.A.S. Influence of CAD/CAM on the fit accuracy of implant-supported zirconia and cobalt-chromium fixed dental prostheses. J. Prosthet. Dent. 2015, 113, 22–28. [Google Scholar] [CrossRef]
- Moris, I.C.M.; Monteiro, S.B.; Martins, R.; Ribeiro, R.F.; Gomes, E.A. Influence of Manufacturing Methods of Implant-Supported Crowns on External and Internal Marginal Fit: A Micro-CT Analysis. BioMed. Res. Int. 2018, 2018, 1–6. [Google Scholar] [CrossRef]
- Mostafa, N.Z.; Ruse, N.D.; Ford, N.L.; Carvalho, R.M.; Wyatt, C.C.L. Marginal Fit of Lithium Disilicate Crowns Fabricated Using Conventional and Digital Methodology: A Three-Dimensional Analysis: Conventionally, Digitally Fabricated LD Crown Marginal Fit. J. Prosthodont. 2018, 27, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Bhering, C.L.B.; Marques, I.d.S.V.; Takahashi, J.M.F.K.; Barão, V.A.R.; Consani, R.L.X.; Mesquita, M.F. Fit and Stability of Screw-Retained Implant-Supported Frameworks Under Masticatory Simulation: Influence of Cylinder Type: Stability of Cast Multiunit Implant-Supported Frameworks. J. Prosthodont. 2016, 25, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, J.C.; Henriques, G.E.P.; Sobrinho, L.C.; de Góes, M.F. Stress-relieving and porcelain firing cycle influence on marginal fit of commercially pure titanium and titanium–aluminum–vanadium copings. Dent. Mater. 2003, 19, 686–691. [Google Scholar] [CrossRef]
- Hong, M.-H.; Min, B.K.; Lee, D.-H.; Kwon, T.-Y. Marginal fit of metal-ceramic crowns fabricated by using a casting and two selective laser melting processes before and after ceramic firing. J. Prosthet. Dent. 2019, 122, 475–481. [Google Scholar] [CrossRef]
- Moldovan, O.; Luthardt, R.G.; Corcodel, N.; Rudolph, H. Three-dimensional fit of CAD/CAM-made zirconia copings. Dent. Mater. 2011, 27, 1273–1278. [Google Scholar] [CrossRef]
- Tabata, L.F.; de Lima Silva, T.A.; de Paula Silveira, A.C.; Ribeiro, A.P.D. Marginal and internal fit of CAD-CAM composite resin and ceramic crowns before and after internal adjustment. J. Prosthet. Dent. 2020, 123, 500–505. [Google Scholar] [CrossRef]




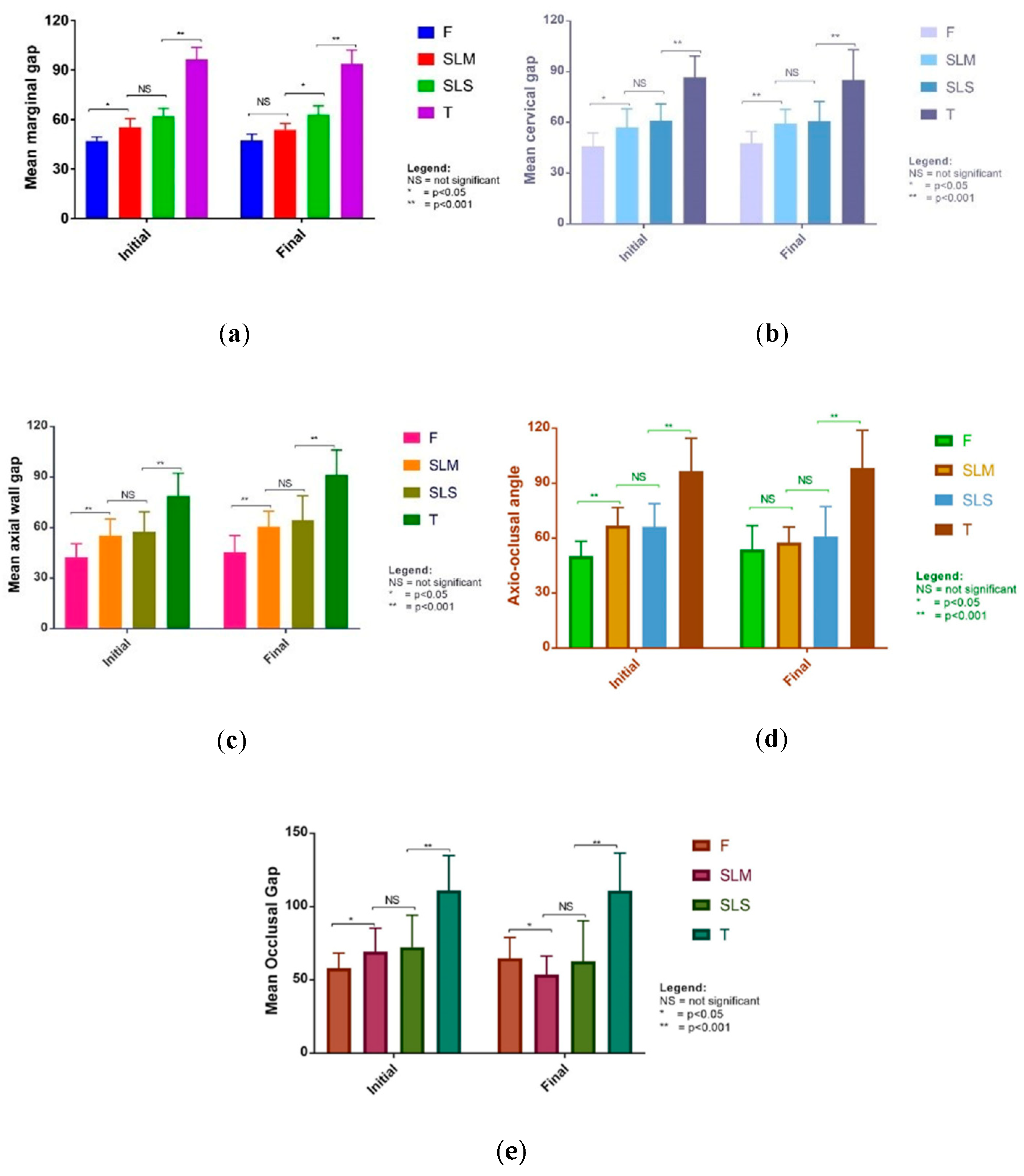
| Measurement Point | Time Point | Procedure | p-Value ** | |||
|---|---|---|---|---|---|---|
| SLS * | SLM * | F * | T * | |||
| Marginal gap | initial | 62.0 ± 11.27 | 55.3 ± 12.75 | 46.9 ± 6.20 | 96.4 ± 17.34 | <0.001 |
| final | 63.0 ± 12.64 | 53.8 ± 8.91 | 47.2 ± 9.36 | 93.8 ± 19.71 | <0.001 | |
| Cervical gap | initial | 61.3 ± 9.64 | 57.0 ± 11.12 | 45.8 ± 7.97 | 86.6 ± 12.67 | <0.001 |
| final | 60.9 ± 11.44 | 59.3 ± 8.40 | 47.6 ± 7.13 | 85.2 ± 17.76 | <0.001 | |
| Axial wall gap | initial | 57.5 ± 11.90 | 55.3 ± 9.83 | 42.5 ± 7.92 | 79.0 ± 13.36 | <0.001 |
| final | 64.4 ± 14.58 | 60.7 ± 9.11 | 45.5 ± 9.84 | 91.5 ± 14.64 | <0.001 | |
| Axio-occlusal angle | initial | 66.2 ± 12.64 | 67.0 ± 9.83 | 50.2 ± 8.10 | 96.6 ± 17.98 | <0.001 |
| final | 61.0 ± 16.15 | 57.6 ± 8.53 | 53.9 ± 13.01 | 98.4 ± 20.53 | <0.001 | |
| Occlusal gap | initial | 72.4 ± 21.75 | 69.3 ± 16.01 | 58.0 ± 10.24 | 111.1 ± 23.69 | <0.001 |
| final | 62.7 ± 27.53 | 53.8 ± 12.50 | 64.8 ± 14.09 | 110.9 ± 25.62 | <0.001 | |
| Difference between Initial and Final Measurement | SLS | SLM | F | T | Between Groups p-Value *** | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference ± SD * | p Value ** | Mean Difference ± SD * | p Value ** | Mean Difference ± SD * | p Value ** | Mean Difference ± SD * | p-Value ** | ||
| Marginal gap | −1.05 ± 19.6 | 0.795 | 1.53 ± 16.2 | 0.327 | −0.21 ± 9.9 | 0.920 | 2.52 ± 24.7 | 0.622 | 0.905 |
| Cervical gap | −4.22 ± 11.7 | 0.091 | −1.85 ± 1.6 | 0.443 | −0.61 ± 15.2 | 0.697 | −6.68 ± 17.0 | 0.067 | 0.810 |
| Axial wall gap | −6.98 ± 18.0 | 0.069 | −5.38 ± 2.6 | 0.048 | −2.96 ± 8.5 | 0.101 | −12.49 ± 17.6 | 0.002 | 0.149 |
| Axio-oclusal angle | 5.21 ± 20.2 | 0.218 | 9.45 ± 11.8 | 0.001 | −3.76 ± 14.1 | 0.203 | −1.79 ± 24.8 | 0.726 | 0.052 |
| Occlusal gap | 9.75 ± 34.7 | 0.182 | 15.55 ± 20.8 | 0.001 | −6.73 ± 17.8 | 0.077 | 0.19 ± 36.8 | 0.981 | 0.042 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savencu, C.E.; Șerban, C.; Porojan, L. Adaptability Evaluation of Metal-Ceramic Crowns Obtained by Additive and Subtractive Technologies. Appl. Sci. 2020, 10, 5563. https://doi.org/10.3390/app10165563
Savencu CE, Șerban C, Porojan L. Adaptability Evaluation of Metal-Ceramic Crowns Obtained by Additive and Subtractive Technologies. Applied Sciences. 2020; 10(16):5563. https://doi.org/10.3390/app10165563
Chicago/Turabian StyleSavencu, Cristina Elena, Costela Șerban, and Liliana Porojan. 2020. "Adaptability Evaluation of Metal-Ceramic Crowns Obtained by Additive and Subtractive Technologies" Applied Sciences 10, no. 16: 5563. https://doi.org/10.3390/app10165563
APA StyleSavencu, C. E., Șerban, C., & Porojan, L. (2020). Adaptability Evaluation of Metal-Ceramic Crowns Obtained by Additive and Subtractive Technologies. Applied Sciences, 10(16), 5563. https://doi.org/10.3390/app10165563





