W-Band Millimeter Waves Targeted Mortality of H1299 Human Lung Cancer Cells without Affecting Non-Tumorigenic MCF-10A Human Epithelial Cells In Vitro
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Media and Cell Cultures
2.2. Irradiation Conditions
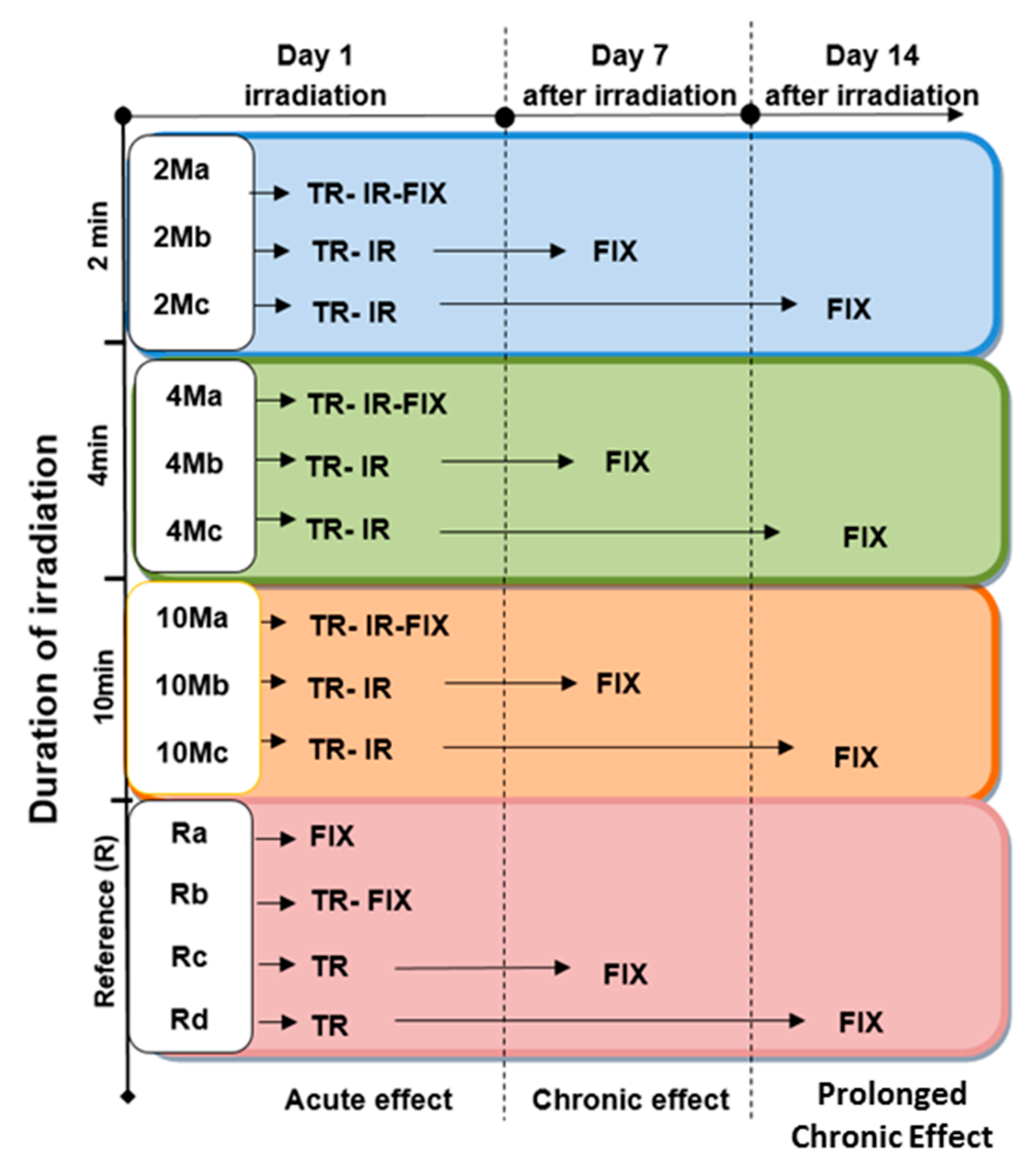
2.3. Time-Schedule and Experimental Conditions
2.4. Evaluation of cell Mortality by DAPI Staining
2.5. Evaluation of Cell Senescence by β-Galactosidase (β-Gal) Assay
2.6. Microscopy Observations and Image processing
2.7. Statistical Analysis
3. Results
3.1. Exposure Duration-Dependent Effects of Low Power W-Band (75–105 GHZ) MMW Irradiation
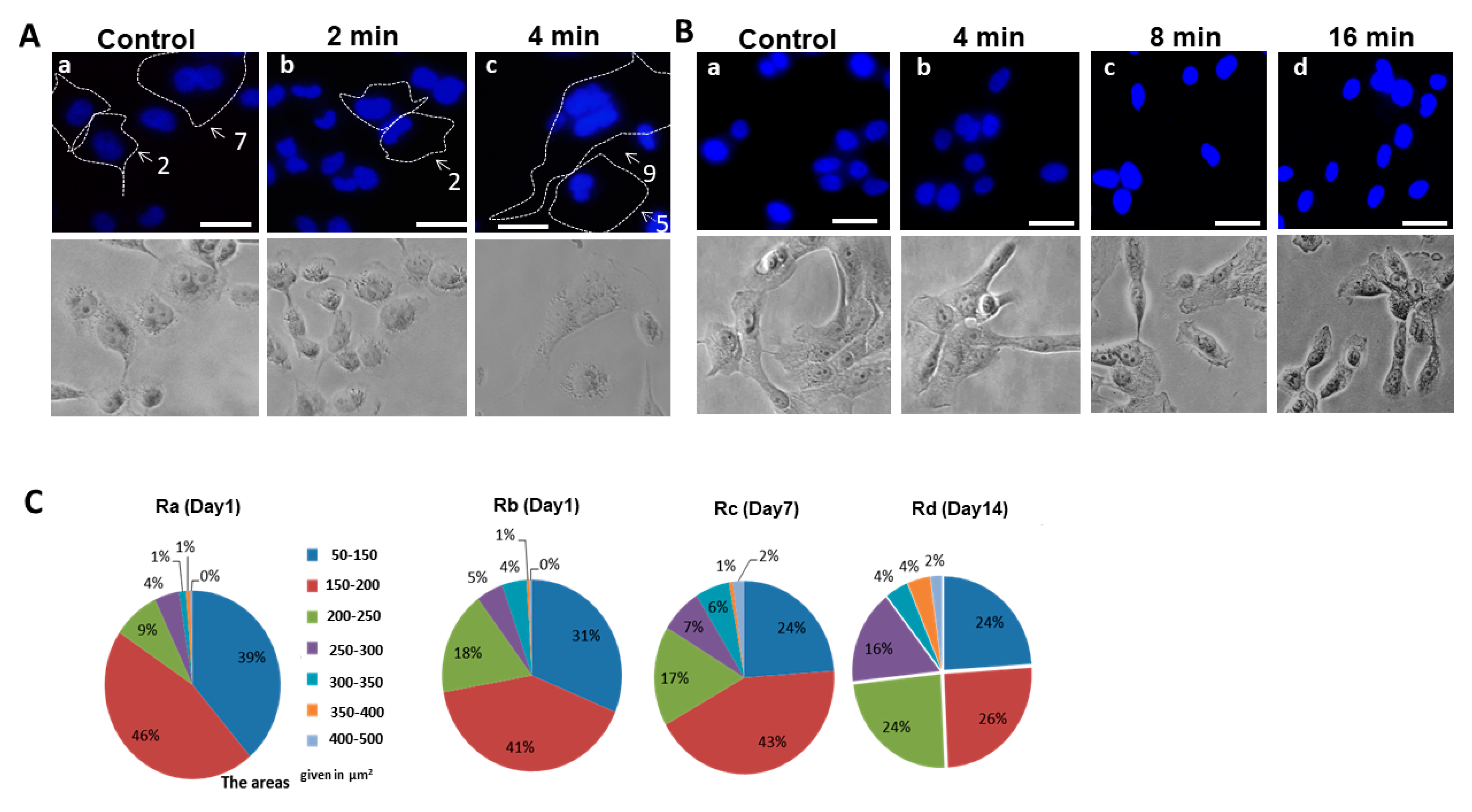
3.2. Nuclear Morphology of Non-Irradiated (Control) and Irradiated H1299 and MCF-10A Cells
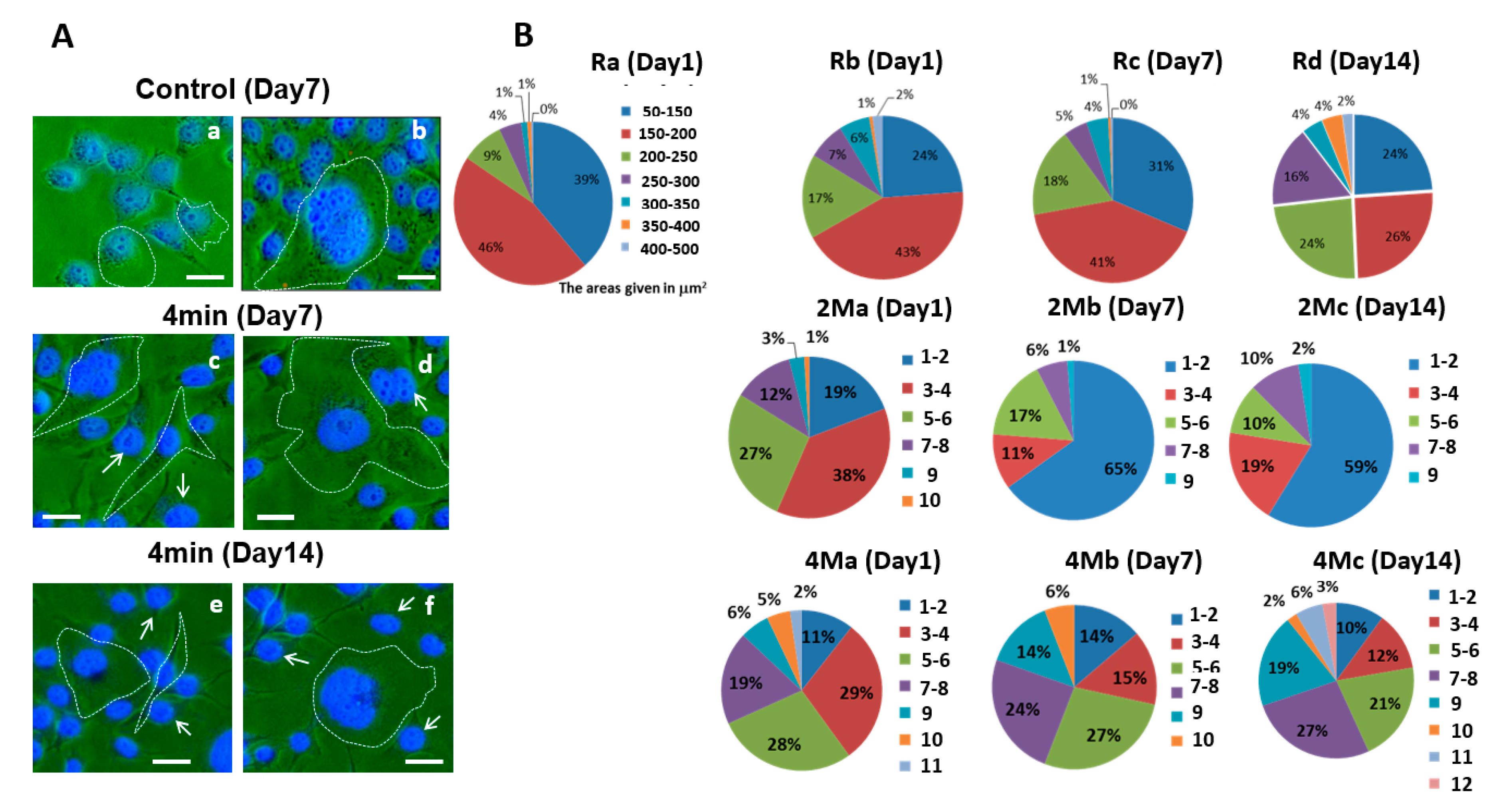
3.3. H1299 Cell Nucleus Shapes and Sizes Change in Response to MMW Irradiation
3.4. Analysis of Correlation between H1299 Cells and Nuclei Distributions in Response to MMW Irradiation
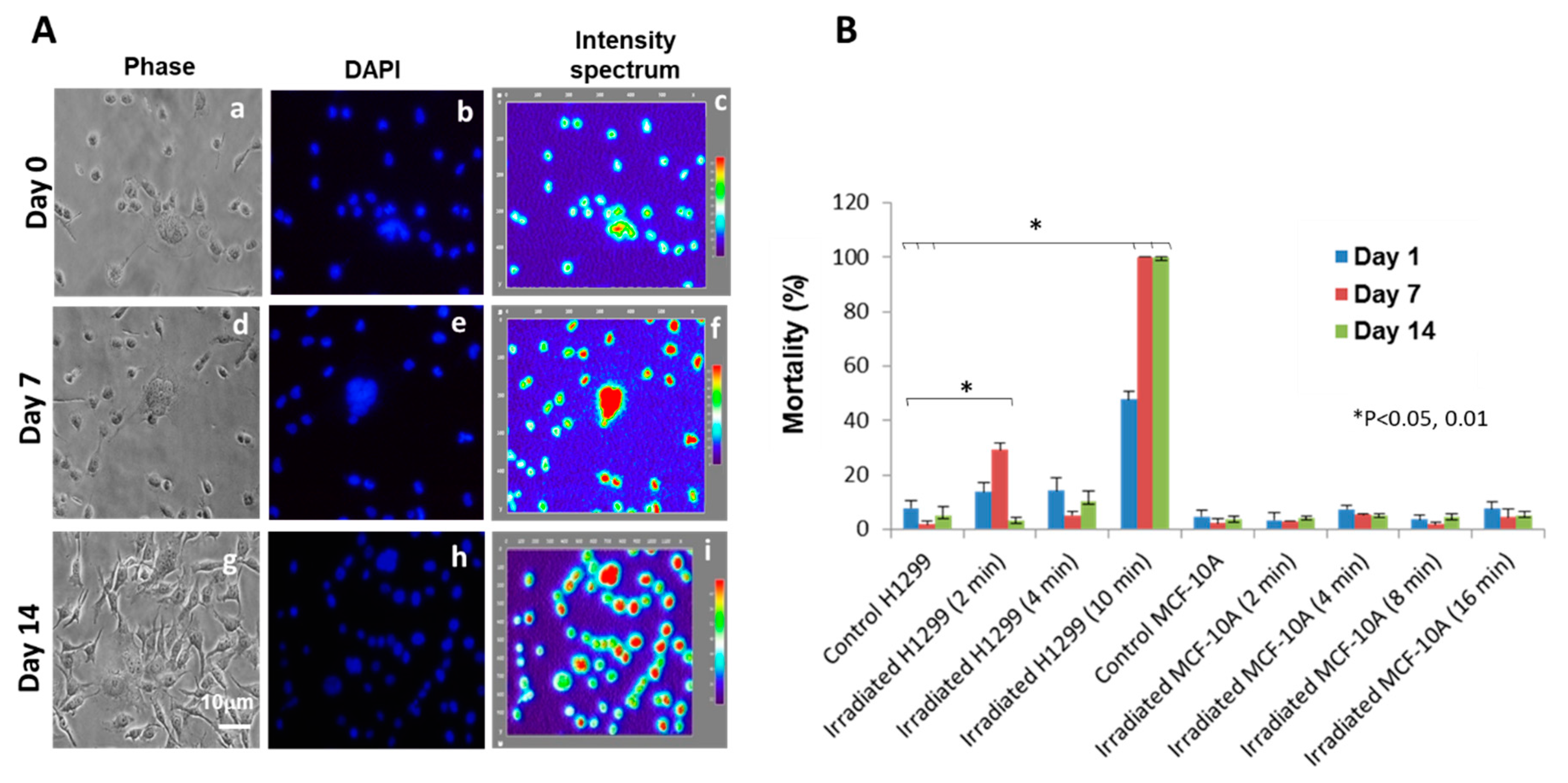
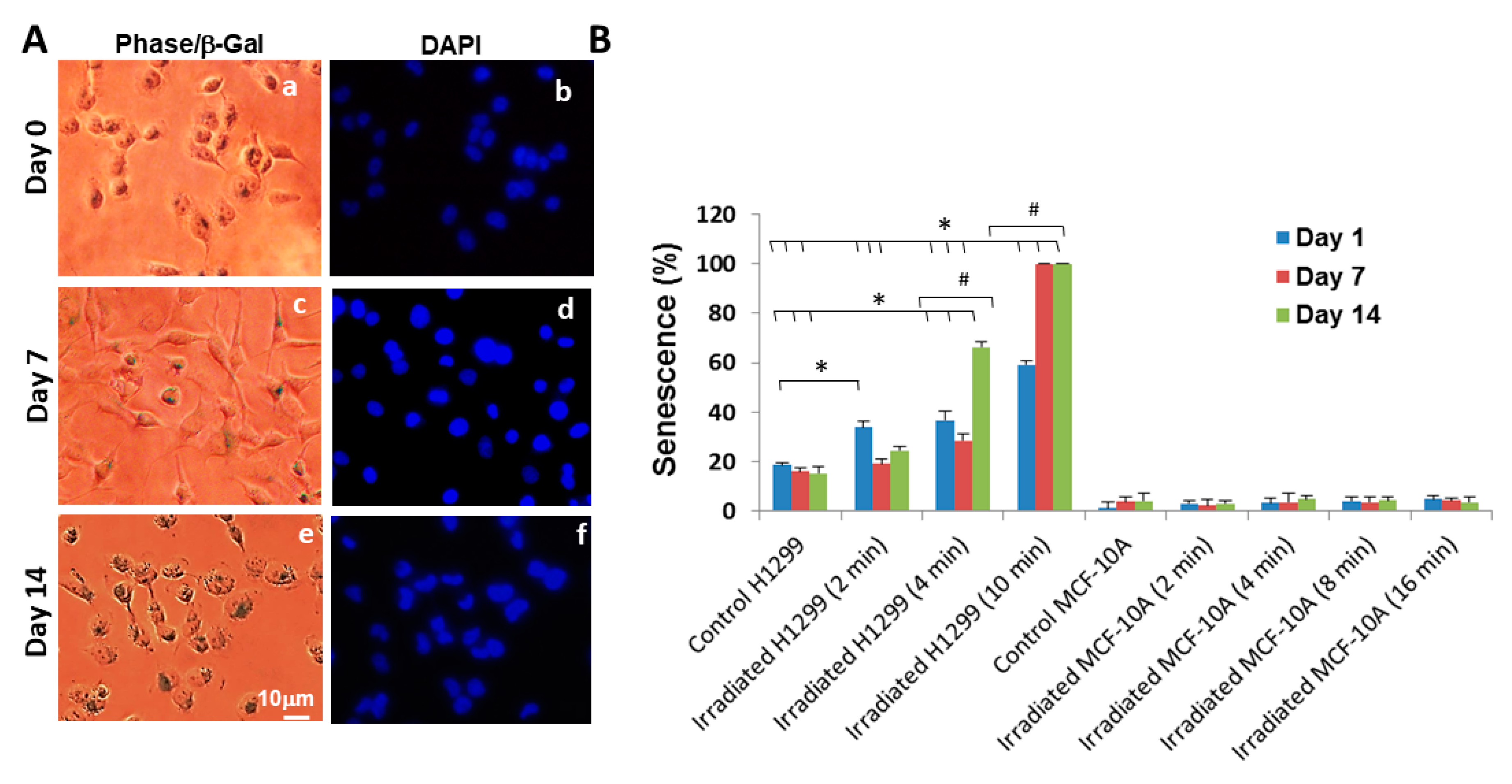
3.5. Short-Term and Long-Term Mortality and Senescence Effects of MMW Irradiation on H1299 Cancer Cells
3.6. Mortality and Senescence Effects of MMW Irradiation Observed in H1299 Cancer Cells does not Affect MCF-10A Non-Tumorigenic Cells
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jemal, A.; Siegel, R.; Ward, E.; Hao, Y.; Xu, J.; Thun, M.J. Cancer Statistics, 2009. CA A Cancer J. Clin. 2009, 59, 225–249. [Google Scholar] [CrossRef]
- Jemal, A.; Siegel, R.; Xu, J.; Ward, E. Cancer Statistics, 2010. CA A Cancer J. Clin. 2010, 60, 277–300. [Google Scholar] [CrossRef]
- Faraonio, R.; Moffatt, P.; LaRochelle, O.; Schipper, H.M.; S-Arnaud, R.; Séguin, C. Characterization of cis-acting elements in the promoter of the mouse. Eur. J. Biochem. 2000, 267, 1743–1753. [Google Scholar] [CrossRef]
- Greulich, H. The Genomics of Lung Adenocarcinoma: Opportunities for Targeted Therapies. Genes Cancer 2010, 1, 1200–1210. [Google Scholar] [CrossRef]
- Wao, H.; Mhaskar, R.; Kumar, A.; Miladinovic, B.; Djulbegovic, B. Survival of patients with non-small cell lung cancer without treatment: A systematic review and meta-analysis. Syst. Rev. 2013, 2, 10. [Google Scholar] [CrossRef]
- Apollonio, F.; Liberti, M.; Paffi, A.; Merla, C.; Marracino, P.; Denzi, A.; Marino, C.; D’Inzeo, G. Feasibility for microwaves energy to affect biological systems via nonthermal mechanisms: A systematic approach. IEEE Trans. Microw. Theory Tech. 2013, 61, 2031–2045. [Google Scholar] [CrossRef]
- Paffi, A.; Apollonio, F.; Lovisolo, G.A.; Marino, C.; Pinto, R.; Repacholi, M.; Liberti, M. Considerations for Developing an RF Exposure System: A Review for in vitro Biological Experiments. IEEE Trans. Microw. Theory Tech. 2010, 58, 2702–2714. [Google Scholar] [CrossRef]
- Pakhomov, A.; Prol, H.; Mathur, S.; Akyel, Y.; Campbell, C. Search for frequency-specific effects of millimeter-wave radiation on isolated nerve function. Bioelectromagnetics 1997, 18, 324–334. [Google Scholar] [CrossRef]
- Alekseev, S.I.; Ziskin, M.C. Effects of millimeter waves on ionic currents of Lymnaea neurons. Bioelectromagnetics 1999, 20, 24–33. [Google Scholar] [CrossRef]
- Alekseev, S.I.; Ziskin, M.C. Local heating of human skin by millimeter waves: A kinetics study. Bioelectromagnetics 2003, 24, 571–581. [Google Scholar] [CrossRef]
- Krajnik, M.; Schäfer, M.; Sobański, P.; Kowalewski, J.; Bloch-Bogusławska, E.; Zylicz, Z.; Mousa, S.A. Local pulmonary opioid network in patients with lung cancer: A putative modulator of respiratory function. Pharmacol. Rep. 2010, 62, 139–149. [Google Scholar] [CrossRef]
- Maneckjee, R.; Minna, J.D. Opioids induce while nicotine suppresses apoptosis in human lung cancer cells. Cell Growth Differ. 1994, 5, 1033–1040. [Google Scholar]
- Radzievsky, A.; Gordiienko, O.; Szabó, I.; Alekseev, S.; Ziskin, M. Millimeter wave-induced suppression of B16 F10 melanoma growth in mice: Involvement of endogenous opioids. Bioelectromagnetics 2004, 25, 466–473. [Google Scholar] [CrossRef]
- Beneduci, A.; Chidichimo, G.; Tripepi, S.; Perrotta, E. Transmission electron microscopy study of the effects produced by wide-band low-power millimeter waves on MCF-7 human breast cancer cells in culture. Anticancer Res. 2005, 25, 1009–1013. [Google Scholar]
- Beneduci, A.; Chidichimo, G.; Tripepi, S.; Perrotta, E.; Cufone, F. Antiproliferative effect of millimeter radiation on human erythromyeloid leukemia cell line K562 in culture: Ultrastructural- and metabolic-induced changes. Bioelectrochemistry 2007, 70, 214–220. [Google Scholar] [CrossRef]
- Beneduci, A.; Cosentino, K.; Chidichimo, G. Millimeter Wave Radiations Affect Membrane Hydration in Phosphatidylcholine Vesicles. Materials 2013, 6, 2701–2712. [Google Scholar] [CrossRef] [PubMed]
- Zhadobov, M.; Nicolaz, C.; Sauleau, R.; Desmots, F.; Thouroude, D.; Michel, D.; Le Drean, Y. Evaluation of the potential biological effects of the 60-GHz millimeter waves upon human cells. IEEE Trans. Antennas Propag. 2009, 57, 2949–2956. [Google Scholar] [CrossRef]
- Logani, M.K.; Szabó, I.; Makar, V.; Bhanushali, A.; Alekseev, S.; Ziskin, M.C. Effect of millimeter wave irradiation on tumor metastasis. Bioelectromagnetics 2006, 27, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Komoshvili, K.; Becker, T.; Levitan, J.; Yahalom, A.; Barbora, A.; Liberman-Aronov, S. Morphological Changes in H1299 Human Lung Cancer Cells Following W-Band Millimeter-Wave Irradiation. Appl. Sci. 2020, 10, 3187. [Google Scholar] [CrossRef]
- Webster, M.; Witkin, K.L.; Cohen-Fix, O. Sizing up the nucleus: Nuclear shape, size and nuclear-envelope assembly. J. Cell Sci. 2009, 122, 1477–1486. [Google Scholar] [CrossRef]
- Krajcovic, M.; Overholtzer, M. Mechanisms of Ploidy Increase in Human Cancers: A New Role for Cell Cannibalism. Cancer Res. 2012, 72, 1596–1601. [Google Scholar] [CrossRef] [PubMed]
- Filippi-Chiela, E.; Oliveira, M.M.; Jurkovski, B.; Jacques, S.M.C.; Da Silva, V.D.; Lenz, G. Nuclear morphometric analysis (NMA): Screening of senescence, apoptosis and nuclear irregularities. PLoS ONE 2012, 7, e42522. [Google Scholar] [CrossRef] [PubMed]
- Debnath, J.; Muthuswamy, S.K.; Brugge, J.S. Morphogenesis and oncogenesis of MCF-10A mammary epithelial acini grown in three-dimensional basement membrane cultures. Methods 2003, 30, 256–268. [Google Scholar] [CrossRef]
- Yaswen, P.; Stampfer, M.R. Molecular changes accompanying senescence and immortalization of cultured human mammary epithelial cells. Int. J. Biochem. Cell Biol. 2002, 34, 1382–1394. [Google Scholar] [CrossRef]
- Heppner, G.H.; Wolman, S.R. MCF-10AT: A Model for Human Breast Cancer Development. Breast J. 1999, 5, 122–129. [Google Scholar] [CrossRef]
- Campisi, J. Aging, Cellular Senescence, and Cancer. Annu. Rev. Physiol. 2013, 75, 685–705. [Google Scholar] [CrossRef]
- Junk, D.; Bryson, B.L.; Jackson, M.W. HiJAK’d Signaling; the STAT3 Paradox in Senescence and Cancer Progression. Cancers 2014, 6, 741–755. [Google Scholar] [CrossRef]
- Lee, H.O.; Davidson, J.M.; Duronio, R.J. Endoreplication: Polyploidy with purpose. Genes Dev. 2009, 23, 2461–2477. [Google Scholar] [CrossRef]
- Weihua, Z.; Lin, Q.; Ramoth, A.J.; Fan, D.; Fidler, I.J. Formation of solid tumors by a single multinucleated cancer cell. Cancer 2011, 117, 4092–4099. [Google Scholar] [CrossRef]
- Shiroff, V.M. DNA and Chromosome Damage: A Crucial Non-Thermal Biological Effect of Microwave Radiation. An Overview of Studies and Models on the Effect Mechanism. In How Susceptible Are Genes to Mobile Phone Radiation? Kompetenzinitiative: Stuttgart, Germany, 1998; pp. 29–43. [Google Scholar]
- Zhadobov, M.; Sauleau, R.; Vie, V.; Himdi, M.; Le Coq, L.; Thouroude, D. Interactions between 60-GHz millimeter waves and artificial biological membranes: Dependence on radiation parameters. IEEE Trans. Microw. Theory Tech. 2006, 54, 2534–2542. [Google Scholar] [CrossRef]
- Titushkin, I.A.; Rao, V.S.; Pickard, W.F.; Moros, E.; Shafirstein, G.; Cho, M.R. Altered Calcium Dynamics Mediates P19-Derived Neuron-Like Cell Responses to Millimeter-Wave Radiation. Radiat. Res. 2009, 172, 725–736. [Google Scholar] [CrossRef]
- Brosig, M.; Ferralli, J.; Gelman, L.; Chiquet, M.; Chiquet-Ehrismann, R. Interfering with the connection between the nucleus and the cytoskeleton affects nuclear rotation, mechanotransduction and myogenesis. Int. J. Biochem. Cell Biol. 2010, 42, 1717–1728. [Google Scholar] [CrossRef] [PubMed]
- Ramundo-Orlando, A. Effects of Millimeter Waves Radiation on Cell Membrane—A Brief Review. J. Infrared Millim. Terahertz Waves 2010, 31, 1400–1411. [Google Scholar] [CrossRef]
- Beneduci, A.; Filippelli, L.; Cosentino, K.; Calabrese, M.L.; Massa, R.; Chidichimo, G. Microwave induced shift of the main phase transition in phosphatidylcholine membranes. Bioelectrochemistry 2012, 84, 18–24. [Google Scholar] [CrossRef]
- Siegel, P.H.; Pikov, V. Impact of low intensity millimetre waves on cell functions. Electron. Lett. 2010, 46, S70. [Google Scholar] [CrossRef]
- Szabó, I.; Kappelmayer, J.; Alekseev, S.; Ziskin, M.C. Millimeter wave induced reversible externalization of phosphatidylserine molecules in cells exposed in vitro. Bioelectromagnetics 2006, 27, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Burrell, R.A.; Swanton, C. Tumour heterogeneity and the evolution of polyclonal drug resistance. Mol. Oncol. 2014, 8, 1095–1111. [Google Scholar] [CrossRef]
- Hong, J.-L.; Lan, K.-C.; Jang, L.-S. Electrical characteristics analysis of various cancer cells using a microfluidic device based on single-cell impedance measurement. Sens. Actuators B Chem. 2012, 173, 927–934. [Google Scholar] [CrossRef]
- Garg, A.; Jones, T.; Moss, S.M.; Mishra, S.; Kaul, K.; Ahirwar, D.K.; Ferree, J.; Kumar, P.; Subramaniam, D.; Ganju, R.K.; et al. Electromagnetic fields alter the motility of metastatic breast cancer cells. Commun. Biol. 2019, 2, 303–316. [Google Scholar] [CrossRef]
- Karinen, A.; Heinävaara, S.; Nylund, R.; Leszczynski, D. Mobile phone radiation might alter protein expression in human skin. BMC Genom. 2008, 9, 77. [Google Scholar] [CrossRef]
- Xu, S.; Zhou, Z.; Zhang, L.; Yu, Z.; Zhang, W.; Wang, Y.; Wang, X.; Li, M.; Chen, Y.; Chen, C.; et al. Exposure to 1800 MHz radiofrequency radiation induces oxidative damage to mitochondrial DNA in primary cultured neurons. Brain Res. 2010, 1311, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Olson, W.K.; Srinivasan, A.R.; Colasanti, A.V.; Zheng, G.; Swigon, D. DNA Biomechanics. In Handbook of Molecular Biophysics: Methods and Applications; Bohr, H.G., Ed.; Wiley: Hoboken, NJ, USA, 2009; p. 1074. [Google Scholar]
- Belyaev, I.Y.; Alipov, Y.D.; Polunin, V.A.; Shcheglov, V.S. Evidence for Dependence of Resonant Frequency of Millimeter Wave Interaction with Escherichia coli K12 Cells on Haploid Genome Length. Electro-and Magnetobiol. 1993, 12, 39–49. [Google Scholar] [CrossRef]
- Furman, O.; Komoshvili, K.; Levitan, J.; Yahalom, A.; Marks, H.; Borodin, D.; Liberman-Aronov, S. The Lack of Toxic Effect of High-Power Short-Pulse 101 GHz Millimeter Waves on Healthy Mice. Bioelectromagnetics 2020, 41, 188–199. [Google Scholar] [CrossRef] [PubMed]
| Number of Subgroup | Nucleus Area (μm2) | Content of Interval | Form of the Nucleus | % of Total Number in Population |
|---|---|---|---|---|
| 1–2 | 50–150 | Interphase-G0-G1 | round or oval | 30 ± 3.7% |
| 3–4 | 150–200 | Interphase-G1-S | round or oval | 46 ± 5.1% |
| 5–6 | 200–250 | Interpase-S-G2 | round or oval | 20 ± 2.9% |
| 6–7 | 200–300 | Mitosis’s | dividing nuclei | 9 ± 1.9% |
| 8–9 | 300–400 | “Monsters”/huge | multi-lobed | 4 ± 1.3% |
| 10 | 500–600 | Polyploid | poly-nuclear | 1 ± 0.67% |
| Subintervals | 2Ma (Day1) | 2Mb (Day7) | 2Mc (Day14) | 4Ma (Day1) | 4Mb (Day7) | 4Mc (Day14) | 10Ma (Day1) |
|---|---|---|---|---|---|---|---|
| 1–2 | −30 | +150 | +125 | −200 | −30 | −150 | −170 |
| 3–4 | ≈ | −300 | −25 | −25 | −200 | −100 | −120 |
| 4–5 | +30 | ≈ | −150 | +30 | +30 | ≈ | −5 |
| 6–7 | +100 | ≈ | −30 | +300 | +300 | +30 | +100 |
| 8–10 | <5 | <5 | <5 | +120 | +20 | +200 | +250 |
| Group | Cell Size | Nuclear Size | Nuclei/Cells (%) |
|---|---|---|---|
| Ra (Day 1, not trans) | NC | NC | 32 ± 5.4 |
| Rb (Day 1, trans) | NC | NC | 36 ± 6.3 |
| Rc (Day7) | NC | NC | 34 ± 8.1 |
| Rd (Day14) | NC | NC | 33 ± 5.7 |
| 2Ma (Day1) | ↓ | ↑ | 42 ± 3.9 |
| 2Mb (Day7) | ↑ | ↓ | 28 ± 5.0 |
| 2Mc (Day14) | ↑ | ↓ | 29 ± 2.6 |
| 4Ma (Day1) | ↓ | ↑ | 52 ± 3.3 |
| 4Mb (Day7) | ↓ | ↑ | 57 ± 6.5 |
| 4Mc (Day14) | ↓ | ↑ | 66 ± 7.6 |
| 10Ma (Day 1) | ↓ | ↑ | 78 ± 5.4 |
| Group | Day 1 | Day 7 | Day 14 |
|---|---|---|---|
| Control | 0.85 | 0.91 | 0.90 |
| 2 min | 0.35 | 0.04 | 0.17 |
| 4 min | −0.11 | −0.2 | −0.41 |
| 10 min | −0.35 | - | - |
| Cell Type | Exposure Time (min) | Mortality (%) in observed days | |||
|---|---|---|---|---|---|
| Day 1 | Day 7 | Day 14 | |||
| H1299 | Control | 0 | 3.9 ± 2.7 | 1.9 ± 3.3 | 3.1 ± 0.88 |
| Irradiated | 2 | 13.9 ± 1.2 | 29.3 ± 2.6 | 3.4 ± 1.4 | |
| 4 | 14.3 ± 2.9 | 8.3 ± 2.0 | 10.3 ± 3.3 | ||
| 10 | 46.8 ± 4.3 | Cell died | Cell died | ||
| MCF-10A | Control | 0 | 4.9 ± 1.7 | 2.5 ± 1.8 | 3.7 ± 1.6 |
| Irradiated | 2 | 3.6 ± 2.0 | 3.0 ± 1.3 | 4.4 ± 1.9 | |
| 4 | 7.5 ± 3.1 | 5.5 ± 2.1 | 5.3 ± 2.5 | ||
| 10 | 5.3 ± 1.4 | 3.5 ± 1.8 | 5.7 ± 2.0 | ||
| 16 | 7.6 ± 2.6 | 4.6 ± 1.4 | 5.3 ± 2.2 | ||
| Cell Type | Exposure Time (min) | Senescence (%) in Observed Days | |||
|---|---|---|---|---|---|
| Day 1 | Day 7 | Day 14 | |||
| H1299 | Control | 0 | 18.6 ± 2.8 | 16.2 ± 1.6 | 15.4 ± 15 |
| Irradiated | 2 | 34.0 ± 3.0 | 19.3 ± 2.5 | 24.6 ± 1.3 | |
| 4 | 36.9 ± 4.1 | 28.6 ± 3.3 | 66.3 ± 2.7 | ||
| 10 | 60.1 ± 3.7 | Cell died | Cell died | ||
| MCF-10A | Control | 0 | 1.4 ± 0.9 | 4 ± 1.2 | 4.3 ± 1.8 |
| Irradiated | 2 | 3.1 ± 1.4 | 2.5 ± 0.7 | 3.1 ± 1.1 | |
| 4 | 3.4 ± 2.2 | 3.8 ± 0.6 | 5.0 ± 2.1 | ||
| 8 | 4.2 ± 1.9 | 3.7 ± 1.1 | 4.4 ± 1.9 | ||
| 10 | 3.9 ± 1.5 | 4.2 ± 1.4 | 3.7 ± 1.7 | ||
| 16 | 5.0 ± 2.3 | 4.4 ± 1.5 | 3.7 ± 0.8 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Komoshvili, K.; Israel, K.; Levitan, J.; Yahalom, A.; Barbora, A.; Liberman-Aronov, S. W-Band Millimeter Waves Targeted Mortality of H1299 Human Lung Cancer Cells without Affecting Non-Tumorigenic MCF-10A Human Epithelial Cells In Vitro. Appl. Sci. 2020, 10, 4813. https://doi.org/10.3390/app10144813
Komoshvili K, Israel K, Levitan J, Yahalom A, Barbora A, Liberman-Aronov S. W-Band Millimeter Waves Targeted Mortality of H1299 Human Lung Cancer Cells without Affecting Non-Tumorigenic MCF-10A Human Epithelial Cells In Vitro. Applied Sciences. 2020; 10(14):4813. https://doi.org/10.3390/app10144813
Chicago/Turabian StyleKomoshvili, Konstantin, Katya Israel, Jacob Levitan, Asher Yahalom, Ayan Barbora, and Stella Liberman-Aronov. 2020. "W-Band Millimeter Waves Targeted Mortality of H1299 Human Lung Cancer Cells without Affecting Non-Tumorigenic MCF-10A Human Epithelial Cells In Vitro" Applied Sciences 10, no. 14: 4813. https://doi.org/10.3390/app10144813
APA StyleKomoshvili, K., Israel, K., Levitan, J., Yahalom, A., Barbora, A., & Liberman-Aronov, S. (2020). W-Band Millimeter Waves Targeted Mortality of H1299 Human Lung Cancer Cells without Affecting Non-Tumorigenic MCF-10A Human Epithelial Cells In Vitro. Applied Sciences, 10(14), 4813. https://doi.org/10.3390/app10144813







