Comparison of Pain Perception between Clear Aligners and Fixed Appliances: A Systematic Review and Meta-Analysis
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Subsection
2.2. Eligibility Criteria
- Clear aligners treatment comparing with fixed appliances and determined pain discomfort through pain visual analog scale (VAS) at multiple time points;
- Randomized and non-randomized studies;
- Studies in humans.
- Studies reporting results emerging from questionnaires;
- Studies lacking control;
- Retrospective studies;
- In vitro and animal studies;
- Case reports/case series;
- Editorials, opinions, narrative reviews and technique description articles, without reported sample.
2.3. Search Strategy
2.4. Assessment of Validity
2.5. Data Extraction
2.6. Risk of Bias of Included Studies
2.7. Summary Measures & Synthesis of Results
2.8. Strength of Recommendation
3. Results
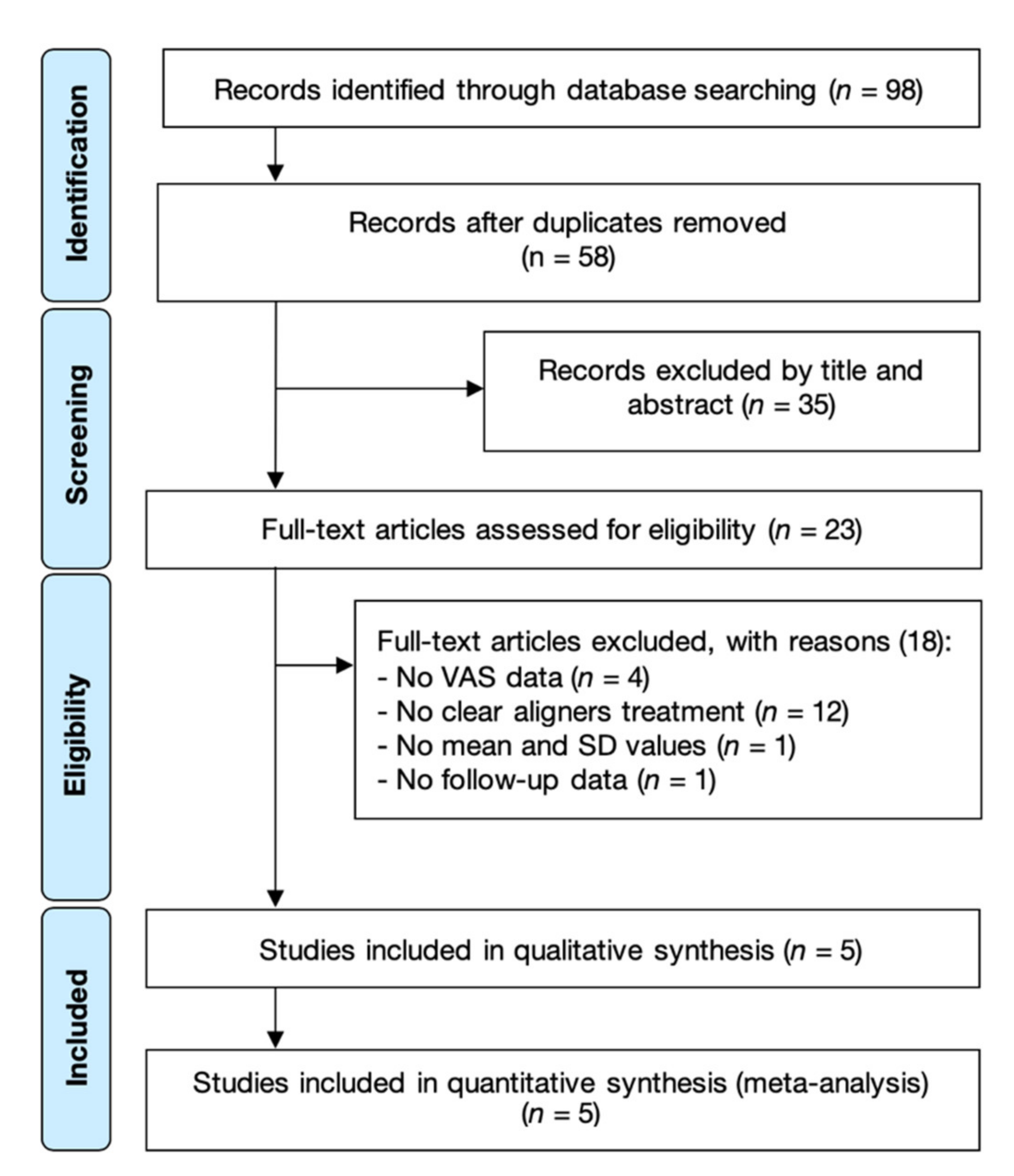
3.1. Study Selection
3.2. Study Characteristics
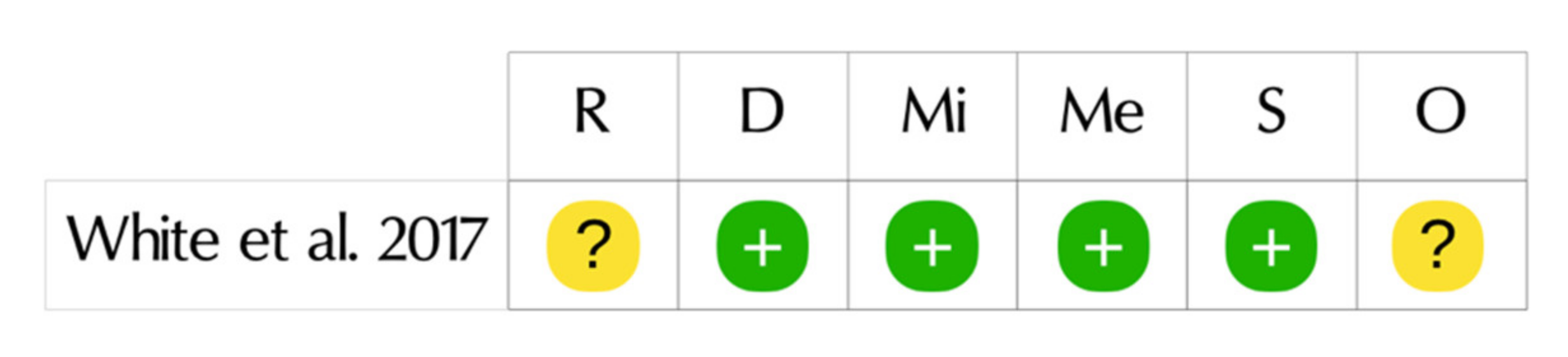
3.3. Risk of Bias within Studies
3.4. Synthesis of Results
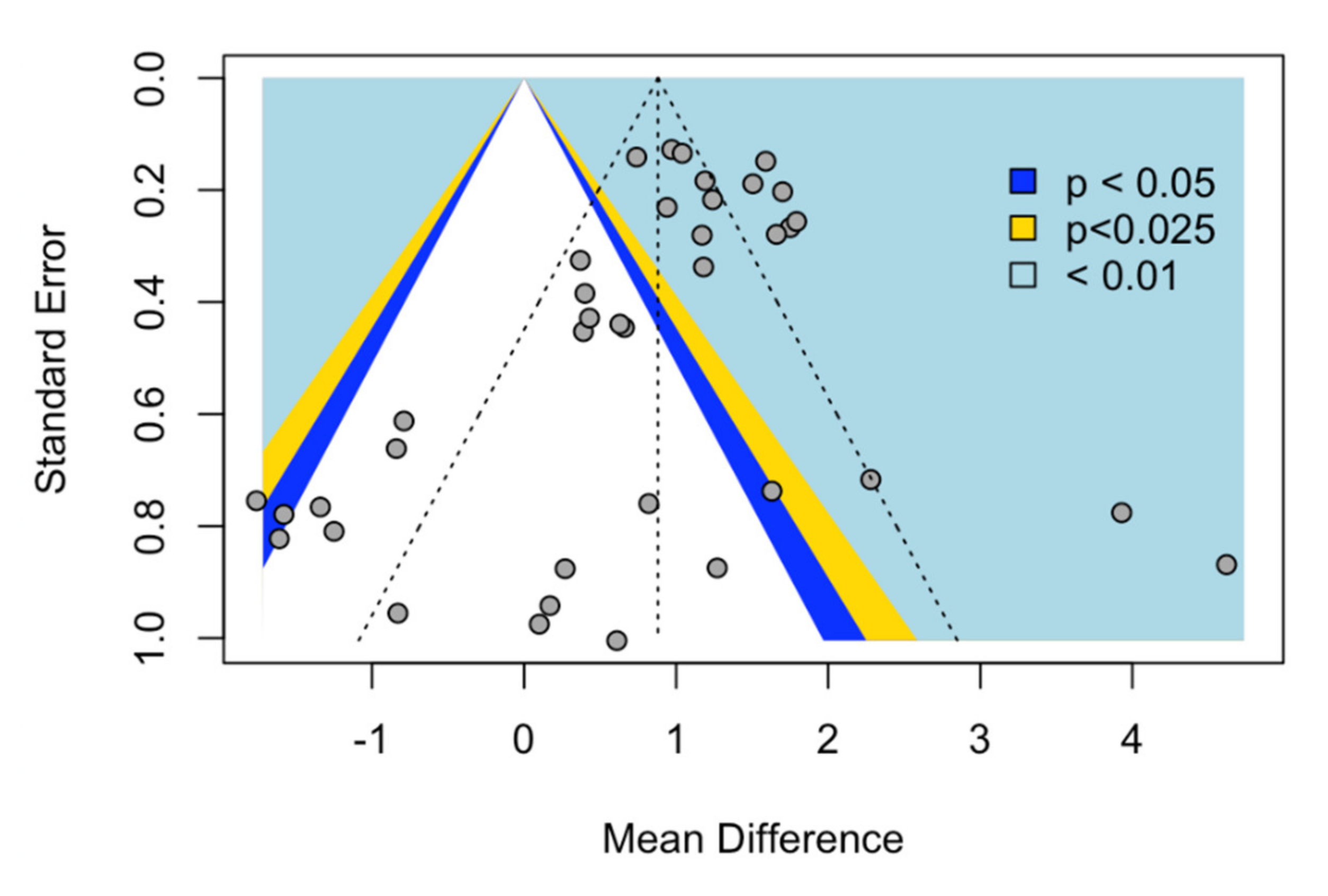
3.5. Synthesis of Results
4. Discussion
4.1. Summary of Main Findings
4.2. Quality of the Evidence, Limitations and Potential Biases in the Review Process
5. Conclusions
Implications for Clinical Practice and Research
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ziuchkovski, J.P.; Fields, H.W.; Johnston, W.M.; Lindsey, D.T. Assessment of perceived orthodontic appliance attractiveness. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Sarver, D.M. Interactions of hard tissues, soft tissues, and growth over time, and their impact on orthodontic diagnosis and treatment planning. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 380–386. [Google Scholar] [CrossRef]
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, e1–e276. [Google Scholar] [CrossRef]
- Kesling, H.D. The philosophy of the tooth positioning appliance. Am. J. Orthod. Oral Surg. 1945, 31, 297–304. [Google Scholar] [CrossRef]
- Wong, B.H.; Scholz, R.P.; Turpin, D.L. Invisalign A to Z. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 540–541. [Google Scholar] [CrossRef]
- White, D.W.; Julien, K.C.; Jacob, H.; Campbell, P.M.; Buschang, P.H. Discomfort associated with Invisalign and traditional brackets: A randomized, prospective trial. Angle Orthod. 2017, 87, 801–808. [Google Scholar] [CrossRef]
- Giddon, D.B.; Anderson, N.K.; Will, L.A. Cognitive, Affective, and Behavioral Responses Associated with Mechanical Tooth Movement. Semin. Orthod. 2007, 13, 212–219. [Google Scholar] [CrossRef]
- Piancino, M.G.; Isola, G.; Cannavale, R.; Cutroneo, G.; Vermiglio, G.; Bracco, P.; Anastasi, G.P. From periodontal mechanoreceptors to chewing motor control: A systematic review. Arch. Oral Biol. 2017, 78, 109–121. [Google Scholar] [CrossRef]
- Isola, G.; Anastasi, G.P.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and molecular outcomes of the human masticatory muscles. Oral Dis. 2018, 24, 1428–1441. [Google Scholar] [CrossRef]
- Abbate, G.M.; Caria, M.P.; Montanari, P.; Mannu, C.; Orrù, G.; Caprioglio, A.; Levrini, L. Parodontale Gesundheit von Teenagern mit herausnehmbaren Alignern und festsitzenden kieferorthopädischen Apparaturen. J. Orofac. Orthop. 2015, 76, 240–250. [Google Scholar] [CrossRef]
- Azaripour, A.; Weusmann, J.; Mahmoodi, B.; Peppas, D.; Gerhold-Ay, A.; Van Noorden, C.J.F.; Willershausen, B. Braces versus Invisalign®: Gingival parameters and patients’ satisfaction during treatment: A cross-sectional study. BMC Oral Health 2015, 15, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Tang, H.; Zhou, T.; Kang, N. Assessment of the periodontal health status in patients undergoing orthodontic treatment with fixed appliances and Invisalign system. Medicine 2018, 97, e0248. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, C.; Jian, F.; Mcintyre, G.T.; Millett, D.T.; Hickman, J.; Lai, W. Initial arch wires used in orthodontic treatment with fixed appliances. Cochrane Database Syst. Rev. 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.; Ngan, P.; Kess, B. Time course of the discomfort in young patients undergoing orthodontic treatment. Pediatr. Dent. 1989, 11, 107–110. [Google Scholar] [PubMed]
- Jones, M.; Chan, C. The pain and discomfort experienced during orthodntic treatment: A randomized controlled clinical trial of two intial aligning arch wires. Am. J. Orthod. Dentofac. Orthop. 1992, 102, 373–381. [Google Scholar] [CrossRef]
- Ngan, P.; Kess, B.; Wilson, S. Perception of discomfort by patients undergoing orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 47–53. [Google Scholar] [CrossRef]
- Scheurer, P.A.; Firestone, A.R.; Bürgin, W.B. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur. J. Orthod. 1996, 18, 349–357. [Google Scholar] [CrossRef]
- Stewart, F.N.; Kerr, W.J.S.; Taylor, P.J.S. Appliance wear: The patient’s point of view. Eur. J. Orthod. 1997, 19, 377–382. [Google Scholar] [CrossRef]
- Krishnan, V.; Davidovitch, Z. Cellular, molecular, and tissue-level reactions to orthodontic force. Am. J. Orthod. Dentofac. Orthop. 2006, 129, e1–e469. [Google Scholar] [CrossRef]
- Grieve, W.G.; Johnson, G.K.; Moore, R.N.; Reinhardt, R.A.; DuBois, L.M. Prostaglandin E (PGE) and interleukin-1β (IL-1β) levels in gingival crevicular fluid during human orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 1994, 105, 369–374. [Google Scholar] [CrossRef]
- Cardoso, P.C.; Espinosa, D.G.; Mecenas, P.; Flores-Mir, C.; Normando, D. Pain level between clear aligners and fixed appliances: A systematic review. Prog. Orthod. 2020, 21, 3. [Google Scholar] [CrossRef]
- Flores-Mir, C.; Brandelli, J.; Pacheco-Pereira, C. Patient satisfaction and quality of life status after 2 treatment modalities: Invisalign and conventional fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Beller, E.M.; Glasziou, P.P.; Altman, D.G.; Hopewell, S.; Bastian, H.; Chalmers, I.; Gøtzsche, P.C.; Lasserson, T.; Tovey, D. PRISMA for Abstracts: Reporting Systematic Reviews in Journal and Conference Abstracts. PLoS Med. 2013, 10, e1001419. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 1–10. [Google Scholar] [CrossRef]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Meta-Analysis with R; Springer: Berlin/Heidelberg, Germany, 2015; ISBN 9783319214153. [Google Scholar]
- Schwarzer, G. Meta: An R Package for Meta-Analysis. R News 2007, 7, 40–45. [Google Scholar]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; 5.1.0 (updated March 2011); The Cochrane Collaboration: 2011. Available online: https://www.cochrane-handbook.org (accessed on 15 April 2020).
- Newman, M.G.; Weyant, R.; Hujoel, P. JEBDP Improves Grading System and Adopts Strength of Recommendation Taxonomy Grading (SORT) for Guidelines and Systematic Reviews. J. Evid. Based. Dent. Pract. 2007, 7, 147–150. [Google Scholar] [CrossRef]
- Miller, K.B.; McGorray, S.P.; Womack, R.; Quintero, J.C.; Perelmuter, M.; Gibson, J.; Dolan, T.A.; Wheeler, T.T. A comparison of treatment impacts between Invisalign aligner and fixed appliance therapy during the first week of treatment. Am. J. Orthod. Dentofac. Orthop. 2007, 131, e1–e302. [Google Scholar] [CrossRef]
- Shalish, M.; Cooper-Kazaz, R.; Ivgi, I.; Canetti, L.; Tsur, B.; Bachar, E.; Chaushu, S. Adult patients’ adjustability to orthodontic appliances. Part I: A comparison between Labial, Lingual, and InvisalignTM. Eur. J. Orthod. 2012, 34, 724–730. [Google Scholar] [CrossRef]
- Almasoud, N.N. Pain perception among patients treated with passive self-ligating fixed appliances and invisalign® aligners during the first week of orthodontic treatment. Korean J. Orthod. 2018, 48, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Piergentili, M.; Bucci, R.; Madariaga, A.C.P.; Martina, S.; Rongo, R.; D’Antò, V. Pain and discomfort associated with labial multibracket appliances vs clear aligners. J. Aligner Orthod. 2019, 3, 205–212. [Google Scholar]
- Wright, N.; Modarai, F.; Cobourne, M.T.; DiBiase, A.T. Do you do Damon ®? What is the current evidence base underlying the philosophy of this appliance system? J. Orthod. 2011, 38, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.S.; DiBiase, A.T.; Sarri, G.; Lee, R.T. Pain experience during initial alignment with a self-ligating and a conventional fixed orthodontic appliance system. Angle Orthod. 2009, 79, 46–50. [Google Scholar] [CrossRef]
- Fleming, P.S.; Johal, A. Self-ligating brackets in orthodontics a systematic review. Angle Orthod. 2010, 80, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Miles, P.G.; Weyant, R.J.; Rustveld, L. A clinical trial of damon 2TM Vs conventional twin brackets during initial alignment. Angle Orthod. 2006, 76, 480–485. [Google Scholar]
- Rahman, S.; Spencer, R.J.; Littlewood, S.J.; O’Dywer, L.; Barber, S.K.; Russell, J.S. A multicenter randomized controlled trial to compare a self-ligating bracket with a conventional bracket in a UK population: Part 2: Pain perception. Angle Orthod. 2016, 86, 149–156. [Google Scholar] [CrossRef]
- Scott, P.; Sherriff, M.; DiBiase, A.T.; Cobourne, M.T. Perception of discomfort during initial orthodontic tooth alignment using a self-ligating or conventional bracket system: A randomized clinical trial. Eur. J. Orthod. 2008, 30, 227–232. [Google Scholar] [CrossRef]
- Bergius, M.; Kiliaridis, S.; Berggren, U. Pain in orthodontics. A review and discussion of the literature. J. Orofac. Orthop. 2000, 61, 125–137. [Google Scholar] [CrossRef]
- Firestone, A.R.; Scheurer, P.A.; Bürgin, W.B. Patients’ anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur. J. Orthod. 1999, 21, 387–396. [Google Scholar] [CrossRef]
- Brown, D.F.; Moerenhout, R.G. The pain experience and psychological adjustment to orthodontic treatment of preadolescents, adolescents, and adults. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 349–356. [Google Scholar] [CrossRef]
- Chow, J.; Cioffi, I. Pain and orthodontic patient compliance: A clinical perspective. Semin. Orthod. 2018, 24, 242–247. [Google Scholar] [CrossRef]
- Erdinç, A.; Dinçer, B. Perception of pain during orthodontic treatment with fixed appliances. Eur. J. Orthod. 2004, 26, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, S.S.; Sandhu, J. Orthodontic pain: An interaction between age and sex in early and middle adolescence. Angle Orthod. 2013, 83, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Alhaija, E.S.A.; AlDaikki, A.; Al-Omairi, M.K.; Al-Khateeb, S.N. The relationship between personality traits, pain perception and attitude toward orthodontic treatment. Angle Orthod. 2010, 80, 1141–1149. [Google Scholar] [CrossRef]
| Study | Country | N (F/M) | Participants | Outcome | Funding | |
|---|---|---|---|---|---|---|
| CA | FA | |||||
| Miller (2007) [31] | USA | 60 (43/17) | 33 | 27 | Adults treated with Invisalign aligners experienced less pain and fewer negative impacts on their lives during the first week of orthodontic treatment than did those treated with fixed appliances | NR |
| Shalish (2012) [32] | USA | 68 (45/23) | 21 | 47 | The Invisalign patients complained of relatively high levels of pain in the first days after insertion; however this group was characterized by the lowest level of oral symptoms and by a similar level of general activity disturbances and oral dysfunction compared to the Buccal appliance. | NR |
| White (2017) [6] | USA | 41 (24/17) | 23 | 18 | Patients treated with traditional fixed appliances reported greater discomfort and consumed more analgesics than patients treated with aligners. | Partially funded by the Robert E. Gaylord Endowed Chair in Orthodontics and by Align Technology |
| Almasoud (2018) [33] | Saudi Arabia | 64 (42/22) | 32 | 32 | During the first week of orthodontic treatment, patients treated with Invisalign aligners reported lower pain than did those treated with passive self-ligating fixed appliances. | NR |
| Piergentili (2019) [34] | Italy | 40 (23/17) | 20 | 20 | Therapy with traditional fixed orthodontics appliances caused more discomfort to the patients, than clear aligner therapy | NR |
| Selection | Comparability | Outcome | TOTAL | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Score | ||
| Miller (2007) [31] | a | a | a | a | a | a | a | a | 8 | Low |
| Shalish (2012) [32] | a | a | a | a | a | a | a | a | 8 | Low |
| Almasoud (2018) [33] | c | a | a | a | a | a | a | a | 7 | Low |
| Piergentili (2019) [34] | a | a | a | a | a | a | a | a | 8 | Low |
| Subgroup Meta-Analysis | n | MD | 95% CI | p-Value | I2 (%) | Tau | p-Value |
|---|---|---|---|---|---|---|---|
| Day 1 | 6 | 1.07 | (0.00; 2.13) | <0.001 | 84.9 | 1.16 | <0.001 |
| Day 2 | 5 | 0.60 | (−0.20; 1.41) | >0.05 | 80.7 | 0.77 | <0.001 |
| Day 3 | 6 | 1.25 | (0.32; 2.17) | <0.001 | 83.0 | 0.99 | <0.001 |
| Day 4 | 5 | 0.79 | (−0.07; 1.65) | >0.05 | 83.8 | 0.84 | <0.001 |
| Day 5 | 5 | 0.62 | (−0.13; 1.37) | >0.05 | 83.7 | 0.71 | <0.001 |
| Day 6 | 5 | 0.76 | (0.31; 1.21) | <0.001 | 67.6 | 0.38 | <0.001 |
| Day 7 | 6 | 0.79 | (0.37; 1.22) | <0.001 | 64.2 | 0.36 | <0.001 |
| Overall | 6 | 0.33 | (0.45; 1.57) | <0.001 | 80.5 | 0.58 | <0.001 |
| Subgroup Meta-Analysis | n | OR | 95% CI | p-Value | I2 (%) | Tau | p-Value |
|---|---|---|---|---|---|---|---|
| Day 1 | 3 | 0.15 | (0.04; 0.50) | <0.001 | 84.9 | 49.3 | 0.14 |
| Day 3 | 3 | 0.75 | (0.11; 5.10) | <0.001 | 83.0 | 81.0 | <0.001 |
| Day 7 | 3 | 0.23 | (0.52; 0.99) | <0.001 | 64.2 | 0.0 | 0.79 |
| Overall | 3 | 0.30 | (0.12; 0.72) | <0.001 | 80.5 | 58.8 | 0.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira, D.; Machado, V.; Botelho, J.; Proença, L.; Mendes, J.J.; Delgado, A.S. Comparison of Pain Perception between Clear Aligners and Fixed Appliances: A Systematic Review and Meta-Analysis. Appl. Sci. 2020, 10, 4276. https://doi.org/10.3390/app10124276
Pereira D, Machado V, Botelho J, Proença L, Mendes JJ, Delgado AS. Comparison of Pain Perception between Clear Aligners and Fixed Appliances: A Systematic Review and Meta-Analysis. Applied Sciences. 2020; 10(12):4276. https://doi.org/10.3390/app10124276
Chicago/Turabian StylePereira, Dinis, Vanessa Machado, João Botelho, Luís Proença, José João Mendes, and Ana Sintra Delgado. 2020. "Comparison of Pain Perception between Clear Aligners and Fixed Appliances: A Systematic Review and Meta-Analysis" Applied Sciences 10, no. 12: 4276. https://doi.org/10.3390/app10124276
APA StylePereira, D., Machado, V., Botelho, J., Proença, L., Mendes, J. J., & Delgado, A. S. (2020). Comparison of Pain Perception between Clear Aligners and Fixed Appliances: A Systematic Review and Meta-Analysis. Applied Sciences, 10(12), 4276. https://doi.org/10.3390/app10124276









