A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options
Abstract
1. Introduction
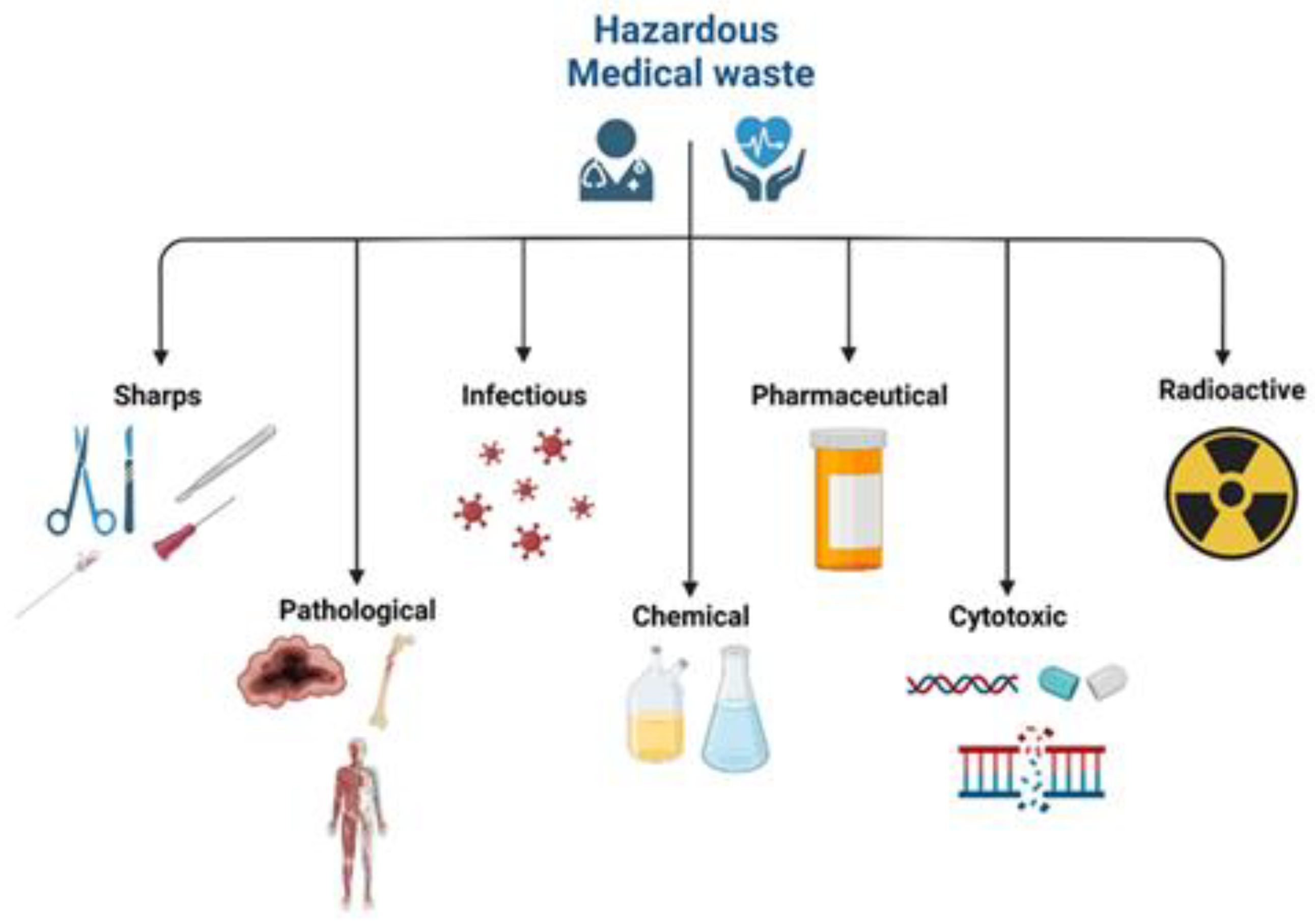
2. Classification of Medical Waste
3. Medical Waste Management Process
3.1. Waste Generation
3.2. Waste Segregation
3.3. Waste Collection and Transportation
3.4. Waste Treatment
- Poisoning from toxic elements,
- Bacterial and fungal infections,
- Release of toxins into the atmosphere,
- Leaching to the soil and underlying aquifers,
- Bioaccumulation,
- Leaving a footprint on the environment,
- Destruction of habitats.
3.4.1. Incineration
- Mixing of waste,
- Moisture content,
- Amount of waste in the furnace,
- Temperature,
- Residence time,
- Maintenance and repair.
3.4.2. Autoclave Disinfection
- Temperature (121–134 °C),
- Steam penetration,
- Waste load,
- Length of the treatment cycle,
- Chamber air removal.
3.4.3. Microwave Disinfection
- Waste characteristics,
- Moisture content,
- Microwave source strength,
- Exposure time,
- Degree of waste mixing.
3.4.4. Chemical Disinfection
- pH,
- Contact time,
- Waste and chemical mixing,
- Recirculation versus flow.
3.5. Waste Recycling
3.6. Waste Disposal
- Rapid cover of waste,
- Burying it under the old municipal waste of minimum burial of three months,
- Waterproof bottom,
- Minimum 2 m above the water table,
- No disposal of chemicals.
4. Case Studies
4.1. Germany
Policies
- “The Directory on Hazardous Waste (94/904/EC), 1994”,
- “European Waste Catalogue (EWC)” and “European Commission Decision 2000/532/EC-2000”,
- “Closed Subsistence Cycle Waste Management Act”—Principle law of waste management,
- “Infection Control and Safety Regulations”,
- “The Dangerous Goods Regulations”—for the transport of hazardous waste,
- “Federal Control of Pollution Act”—for the incineration of waste.
- Sharp waste: is immediately collected in resistant leak-proof and closable containers at the point of the waste generation source. This type of MW is disposed of together with general waste;
- Anatomical waste: is also collected in resistant leak-proof and closable containers from the point of waste generation origin and refrigerated and transported for incineration by authorised plants;
- Infectious waste: is also collected from the source of origin in protected containers, flagged with a biohazard symbol. Authorised companies transport waste to approved standard incineration plants;
- Other waste: waste produced during care or treatment without considering specific requirements for disposal is also collected and finally disposed of with domestic waste following municipal regulations;
- Amalgam waste: this is waste collected from dentistry and is collected separately and recycled by the producer or distributor;
- Chemical waste: is collected in a leak-proof container, flagged by hazardous properties of chemical content, which a specialised waste management company manages;
- Cytostatic drug wastes: are also collected at the point of waste generation origin in leak-proof containers flagged with a danger symbol. These wastes are transported to the authorised incineration facilities by companies specialising in MW transportation.
4.2. China
Policies
- “Medical waste control act 380”—Mandatory obligation and requirements of a disposal facility for the MW generator;
- “Regulation 287”—related to the MW category issued by the Ministry of Health and State Environment Protection Administration;
- “Administrative Penalty Regulation 21”—deals with the behaviour and the improper management of MW by the generator;
- “Standard HJ 421-2008”—concerned about the standards regarding containers, packaging bags, and warning labels and symbols of different types of MW;
- “Technical Standard for Medical Waste Incinerator, 2003”;
- “Technical Specifications for Centralised Incineration Facility for Hazardous Waste, 2005”;
- “Measures on Permit for Operation of Hazardous Wastes, 2004”;
- “Regulations on the Administration of Medical Wastes, 2003”;
- “Standard for Pollution Control on Hazardous Waste Storage, 2001”;
- “Pollution Control Standard for Hazardous Wastes Incineration, 2001”;
- “Standard for Pollution Control on the Security Landfill Site for Hazardous Wastes, 2001”;
- “Measure for the Administration of Registration of Hazardous Chemical, 2002”.
4.3. United States of America
Policies
- Incineration: three types of incineration are used for MW disposal. These are controlled air, multiple chamber air, and rotary kiln models. The Environmental Protection Agency (EPA) estimates that more than 70% of the total MW generated in the USA is incinerated [32];
- Steam sterilisation or autoclaving: it is necessary to follow sterilisation or autoclaving before landfill disposal of MW. Autoclaving includes keeping the temperature between 120 and 135 °C, bags of infectious MW are placed in a chamber and steamed for 30–50 min. After that, the sterile waste can be safely disposed of in a landfill [37].
4.4. Egypt
Policies
4.5. Management of MW in Other Countries
4.5.1. India
4.5.2. Canada
4.5.3. Europe
4.5.4. Australia
- The “Clinical and Related Waste Management Policy of 2016” in Western Australia addresses both the hazardous and non-hazardous types of MW,
- The “Environment Protection (Waste Management) Policy 1994” addresses and regulates all types of waste in southern Australia.
5. COVID-19 and Medical Waste
6. Conclusions and Recommendations
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yoon, C.-W.; Kim, M.-J.; Park, Y.-S.; Jeon, T.-W.; Lee, M.-Y. A review of medical waste management systems in the Republic of Korea for hospital and medical waste generated from the COVID-19 pandemic. Sustainability 2022, 14, 3678. [Google Scholar] [CrossRef]
- Prem Ananth, A.; Prashanthini, V.; Visvanathan, C. Healthcare waste management in Asia. Waste Manag. 2010, 30, 154–161. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Health-Care Waste. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 15 May 2022).
- Ordway, A.; Pitonyak, J.S.; Johnson, K.L. Durable medical equipment reuse and recycling: Uncovering hidden opportunities for reducing medical waste. Disabil. Rehabil. Assist. Technol. 2020, 15, 21–28. [Google Scholar] [CrossRef]
- Harding, C.; Van Loon, J.; Moons, I.; De Win, G.; Du Bois, E. Design opportunities to reduce waste in operating rooms. Sustainability 2021, 13, 2207. [Google Scholar] [CrossRef]
- Lee, B.-K.; Ellenbecker, M.J.; Moure-Eraso, R. Analyses of the recycling potential of medical plastic wastes. Waste Manag. 2002, 22, 461–470. [Google Scholar] [CrossRef]
- Patrício Silva, A.L.; Prata, J.C.; Walker, T.R.; Campos, D.; Duarte, A.C.; Soares, A.M.V.M.; Barcelò, D.; Rocha-Santos, T. Rethinking and optimising plastic waste management under COVID-19 pandemic: Policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020, 742, 140565. [Google Scholar] [CrossRef]
- Talvitie, J.; Mikola, A.; Koistinen, A.; Setälä, O. Solutions to microplastic pollution—Removal of microplastics from wastewater effluent with advanced wastewater treatment technologies. Water Res. 2017, 123, 401–407. [Google Scholar] [CrossRef]
- Zheng, J.; Suh, S. Strategies to reduce the global carbon footprint of plastics. Nat. Clim. Chang. 2019, 9, 374–378. [Google Scholar] [CrossRef]
- United Nations (UN). Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: https://sdgs.un.org/2030agenda (accessed on 8 May 2022).
- Sharma, R.; Sharma, M.; Sharma, R.; Sharma, V. The impact of incinerators on human health and environment. Rev. Environ. Health 2013, 28, 67–72. [Google Scholar] [CrossRef]
- Rizan, C.; Bhutta, M.F.; Reed, M.; Lillywhite, R. The carbon footprint of waste streams in a UK hospital. J. Clean. Prod. 2021, 286, 125446. [Google Scholar] [CrossRef]
- Van Straten, B.; Dankelman, J.; van der Eijk, A.; Horeman, T. A Circular healthcare economy; a feasibility study to reduce surgical stainless steel waste. Sustain. Prod. Consum. 2021, 27, 169–175. [Google Scholar] [CrossRef]
- Tsai, W.-T. Analysis of medical waste management and impact analysis of COVID-19 on its generation in Taiwan. Waste Manag. Res. 2021, 39, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Windfeld, E.S.; Brooks, M.S.-L. Medical waste management—A review. J. Environ. Manag. 2015, 163, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Komilis, D.; Makroleivaditis, N.; Nikolakopoulou, E. Generation and composition of medical wastes from private medical microbiology laboratories. Waste Manag. 2017, 61, 539–546. [Google Scholar] [CrossRef]
- Zhou, H.; Yu, X.; Alhaskawi, A.; Dong, Y.; Wang, Z.; Jin, Q.; Hu, X.; Liu, Z.; Kota, V.G.; Abdulla, M.H.A.H.; et al. A deep learning approach for medical waste classification. Sci. Rep. 2022, 12, 2159. [Google Scholar] [CrossRef] [PubMed]
- Commision of the European Communities. Guidance on Classification of Waste According to EWC-Stat Categories, Supplement to the Manual for the Implementation of the Regulation (EC) No 2150/2002 on Waste Statistics; Commision of the European Communities: Brussels, Belgium, 2010; Volume 2. [Google Scholar]
- Huang, M.-C.; Lin, J.J. Characteristics and management of infectious industrial waste in Taiwan. Waste Manag. 2008, 28, 2220–2228. [Google Scholar] [CrossRef]
- International Committee of the Red Cross (ICRC). Medical Waste Management; ICRC: Geneva, Switzerland, 2011; pp. 12–14, 51–77. [Google Scholar]
- Akter, N. Medical waste management: A review. Res. Rep. Health Stud. 2000, XXVIII, 370–394. [Google Scholar]
- Power, B.; Brady, R.; Connell, P. Analysing the carbon footprint of an intravitreal injection. J. Ophthalmic Vis. Res. 2021, 16, 367–376. [Google Scholar] [CrossRef]
- Giakoumakis, G.; Politi, D.; Sidiras, D. Medical waste treatment technologies for energy, fuels, and materials production: A review. Energies 2021, 14, 8065. [Google Scholar] [CrossRef]
- Wielgosiński, G.; Czerwińska, J.; Szymańska, O.; Bujak, J. Simultaneous NOx and dioxin removal in the SNCR process. Sustainability 2020, 12, 5766. [Google Scholar] [CrossRef]
- Ababneh, A.; Al-Rousan, R.; Gharaibeh, W.; Abu-Dalo, M. Recycling of pre-treated medical waste fly ash in mortar mixtures. J. Mater. Cycles Waste Manag. 2020, 22, 207–220. [Google Scholar] [CrossRef]
- Wyssusek, K.H.; Keys, M.T.; van Zundert, A.A.J. Operating room greening initiatives—The old, the new, and the way forward: A narrative review. Waste Manag. Res. 2018, 37, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.; Nunes, K.R. Recycling behaviour in healthcare: Waste handling at work. Ergonomics 2014, 57, 525–535. [Google Scholar] [CrossRef]
- Hansen, D.; Mikloweit, U.; Ross, B.; Popp, W. Healthcare waste management in Germany. Int. J. Infect. Control. 2014, 10, 3. [Google Scholar] [CrossRef]
- Shah, S.A.A.; Longsheng, C.; Solangi, Y.A.; Ahmad, M.; Ali, S. Energy trilemma based prioritisation of waste-to-energy technologies: Implications for post-COVID-19 green economic recovery in Pakistan. J. Clean. Prod. 2021, 284, 124729. [Google Scholar] [CrossRef] [PubMed]
- Yong, Z.; Gang, X.; Guanxing, W.; Tao, Z.; Dawei, J. Medical waste management in China: A case study of Nanjing. Waste Manag. 2009, 29, 1376–1382. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Huang, Q.; Wang, Q.; Zhou, B.; Li, J. Hazardous waste generation and management in China: A review. J. Hazard. Mater. 2008, 158, 221–227. [Google Scholar] [CrossRef]
- Lee, C.; Huffman, G. Medical waste management/incineration. J. Hazard. Mater. 1996, 48, 1–30. [Google Scholar] [CrossRef]
- Martini, C.L. Medical waste regulation in the United States: A dire need for recognition and reform. Northwestern J. Int. Law Bus. 1993, 14, 206. [Google Scholar]
- Pizarro-Ortega, C.I.; Dioses-Salinas, D.C.; Fernández Severini, M.D.; Forero López, A.D.; Rimondino, G.N.; Benson, N.U.; Dobaradaran, S.; De-la-Torre, G.E. Degradation of plastics associated with the COVID-19 pandemic. Mar. Pollut. Bull. 2022, 176, 113474. [Google Scholar] [CrossRef]
- Shareefdeen, Z.M. Medical waste management and control. J. Environ. Prot. 2012, 3, 1625. [Google Scholar] [CrossRef]
- Shareefdeen, Z.; Ashoobi, N.; Ilyas, U. Medical Waste Management and Treatment Technologies. In Hazardous Waste Management; Springer: Cham, Switzerland, 2022; pp. 113–133. [Google Scholar]
- Hasan, M.M.; Rahman, M.H. Assessment of healthcare waste management paradigms and its suitable treatment alternative: A case study. J. Environ. Public Health 2018, 2018, 6879751. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Salam, M.M. Hospital waste management in El-Beheira Governorate, Egypt. J. Environ. Manag. 2010, 91, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Hassan, I.A.; Younis, A.; Al Ghamdi, M.A.; Almazroui, M.; Basahi, J.M.; El-Sheekh, M.M.; Abouelkhair, E.K.; Haiba, N.S.; Alhussaini, M.S.; Hajjar, D. Contamination of the marine environment in Egypt and Saudi Arabia with personal protective equipment during COVID-19 pandemic: A short focus. Sci. Total Environ. 2022, 810, 152046. [Google Scholar] [CrossRef]
- Mostafa, M.K.; Gamal, G.; Wafiq, A. The impact of COVID 19 on air pollution levels and other environmental indicators—A case study of Egypt. J. Environ. Manag. 2021, 277, 111496. [Google Scholar] [CrossRef]
- Soliman, S.M.; Ahmed, A.I. Overview of biomedical waste management in selected Governorates in Egypt: A pilot study. Waste Manag. 2007, 27, 1920–1923. [Google Scholar] [CrossRef]
- Abd El-Wahab, E.W.; Eassa, S.M.; Lotfi, S.E.; El Masry, S.A.; Shatat, H.Z.; Kotkat, A.M. Adverse health problems among municipality workers in Alexandria (Egypt). Int. J. Prev. Med. 2014, 5, 545–556. [Google Scholar]
- Benson, N.U.; Fred-Ahmadu, O.H.; Bassey, D.E.; Atayero, A.A. COVID-19 pandemic and emerging plastic-based personal protective equipment waste pollution and management in Africa. J. Environ. Chem. Eng. 2021, 9, 105222. [Google Scholar] [CrossRef]
- Datta, P.; Mohi, G.K.; Chander, J. Biomedical waste management in India: Critical appraisal. J. Lab. Physicians 2018, 10, 6–14. [Google Scholar] [CrossRef]
- Patil, A.D.; Shekdar, A.V. Health-care waste management in India. J. Environ. Manag. 2001, 63, 211–220. [Google Scholar] [CrossRef]
- Walkinshaw, E. Medical waste-management practices vary across Canada. Can. Med. Assoc. J. 2011, 183, E1307. [Google Scholar] [CrossRef] [PubMed]
- Government of Quebec. Regulation Respecting Biomedical Waste; Quebec Official Publisher: L’Anse-Saint-Jean, QC, Canada, 2022. [Google Scholar]
- Andeobu, L.; Wibowo, S.; Grandhi, S. Medical Waste from COVID-19 pandemic—A systematic review of management and environmental impacts in Australia. Int. J. Environ. Res. Public Health 2022, 19, 1381. [Google Scholar] [CrossRef] [PubMed]
- Medical Technology Association of Australia (MTAA). Medical Devices Waste: Who Is Responsible? Available online: https://www.mtaa.org.au/news/medical-device-waste-who-responsible (accessed on 4 November 2022).
- Rupani, P.F.; Nilashi, M.; Abumalloh, R.A.; Asadi, S.; Samad, S.; Wang, S. Coronavirus pandemic (COVID-19) and its natural environmental impacts. Int. J. Environ. Sci. Technol. 2020, 17, 4655–4666. [Google Scholar] [CrossRef] [PubMed]
- Teymourian, T.; Teymoorian, T.; Kowsari, E.; Ramakrishna, S. Challenges, strategies, and recommendations for the huge surge in plastic and medical waste during the global COVID-19 pandemic with circular economy approach. Mater. Circ. Econ. 2021, 3, 6. [Google Scholar] [CrossRef]
- Zhao, H.-L.; Wang, L.; Liu, F.; Liu, H.-Q.; Zhang, N.; Zhu, Y.-W. Energy, environment and economy assessment of medical waste disposal technologies in China. Sci. Total Environ. 2021, 796, 148964. [Google Scholar] [CrossRef]
- Abu-Qdais, H.A.; Al-Ghazo, M.A.; Al-Ghazo, E.M. Statistical analysis and characteristics of hospital medical waste under novel Coronavirus outbreak. Glob. J. Environ. Sci. Manag. 2020, 6, 21–30. [Google Scholar]
- Chowdhury, T.; Chowdhury, H.; Rahman, M.S.; Hossain, N.; Ahmed, A.; Sait, S.M. Estimation of the healthcare waste generation during COVID-19 pandemic in Bangladesh. Sci. Total Environ. 2022, 811, 152295. [Google Scholar] [CrossRef]
- Mondal, R.; Mishra, S.; Pillai, J.S.K.; Sahoo, M.C. COVID 19 Pandemic and biomedical waste management practices in healthcare system. J. Fam. Med. Prim. Care 2022, 11, 439–446. [Google Scholar] [CrossRef]
- Voudrias, E.A. Technology selection for infectious medical waste treatment using the analytic hierarchy process. J. Air Waste Manag. Assoc. 2016, 66, 663–672. [Google Scholar] [CrossRef]

| Category (Examples) | World Health Organization (WHO) | EU | Source | |
|---|---|---|---|---|
| Hazardous | Sharps | Sharps | Sharps | Hospitals, clinics, laboratories, blood banks, nursing homes, veterinary clinics and labs |
| Organic matter, including body parts and blood | Pathological | Human tissue, body parts, organs, and blood preserves and bags | Hospitals, clinics, laboratories, mortuary and autopsy facilities, veterinary clinics and labs | |
| Waste with restrictions in collection and disposal due to infectivity | Infectious | Human and Animal Infectious | Hospitals, clinics, and laboratories | |
| Waste with no restrictions or special requirements for collection and disposal due to infectivity (e.g., plasters, casts, dressings, bed sheets, disposable clothing, etc.) | Infectious | Infectious | Hospitals, clinics, and laboratories | |
| Dangerous chemical materials and substances | Chemical | Chemical | Hospitals, clinics, and laboratories | |
| Other chemicals | Chemical | Chemical/ Unused hazardous medicines | Hospitals, clinics, and laboratories | |
| Cytotoxic and cytostatic medicines | Cytotoxic | Discarded unused medicines | Hospitals and laboratories | |
| Non-hazardous | Other chemicals (non-hazardous) | Pharmaceutical | Unused non-hazardous medicines | Hospitals, clinics, and laboratories |
| Dental clinics (care centres) amalgam waste | Amalgam (tooth filling) waste from dental clinics/centres | Amalgam waste from dental clinics/centres | Dental care centres and clinics |
| Treatment Method | Advantages | Disadvantages |
|---|---|---|
| Incineration |
|
|
| Autoclave disinfection |
|
|
| Microwave disinfection |
|
|
| Chemical disinfection |
|
|
| No. | Type of Waste Category | Name of the Regulatory Framework |
|---|---|---|
| 1. | Regulated medical waste | Medical Waste Tracking Act (MWTA), 1988; States Regulations and EPA Guidelines; Resource Conservation and Recovery Act (RCRA) (40 Code of Federal Regulations (CFR) 240.101) |
| 2. | Non-regulated medical waste | States Regulations |
| 3. | Hazardous waste | RCRA (40 CFR 260–265 and 122–124) and States Regulations |
| 4. | Radioactive waste | Nuclear Regulatory Commission (NRC) Standards (10 CFR 20) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attrah, M.; Elmanadely, A.; Akter, D.; Rene, E.R. A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments 2022, 9, 146. https://doi.org/10.3390/environments9110146
Attrah M, Elmanadely A, Akter D, Rene ER. A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments. 2022; 9(11):146. https://doi.org/10.3390/environments9110146
Chicago/Turabian StyleAttrah, Mustafa, Amira Elmanadely, Dilruba Akter, and Eldon R. Rene. 2022. "A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options" Environments 9, no. 11: 146. https://doi.org/10.3390/environments9110146
APA StyleAttrah, M., Elmanadely, A., Akter, D., & Rene, E. R. (2022). A Review on Medical Waste Management: Treatment, Recycling, and Disposal Options. Environments, 9(11), 146. https://doi.org/10.3390/environments9110146







