COVID-19 and the Environment, Review and Analysis
Abstract
1. Introduction
2. Literature Review
| PM2.5 or PM10: | 230 |
| PM2.5 or PM10 + NO2: | 137 |
| PM2.5 or PM10 + NO2 + O3 | 77 |
| PM2.5 or PM10 + NO2 + traffic: | 23 |
| PM2.5 + carbon (not CO) | 5 |
| traffic + carbon (not CO) | 11 |
| Indoor | 81 |
| time-series | 20 |
| China: | 213 |
| Global: | 160 |
| Europe | 110 |
| India: | 110 |
| United States: | 80 |
| Canada: | 35 |
| California: | 28 |
| New York | 25 |
| Japan: | 24 |
| Africa: | 19 |
| South America: | 14 |
| Israel: | 4 |
2.1. Short-Term Associations between COVID-19 and Ambient Air Quality
2.2. Long-Term Associations between COVID-19 and Ambient Air Quality
3. Air Quality Considerations
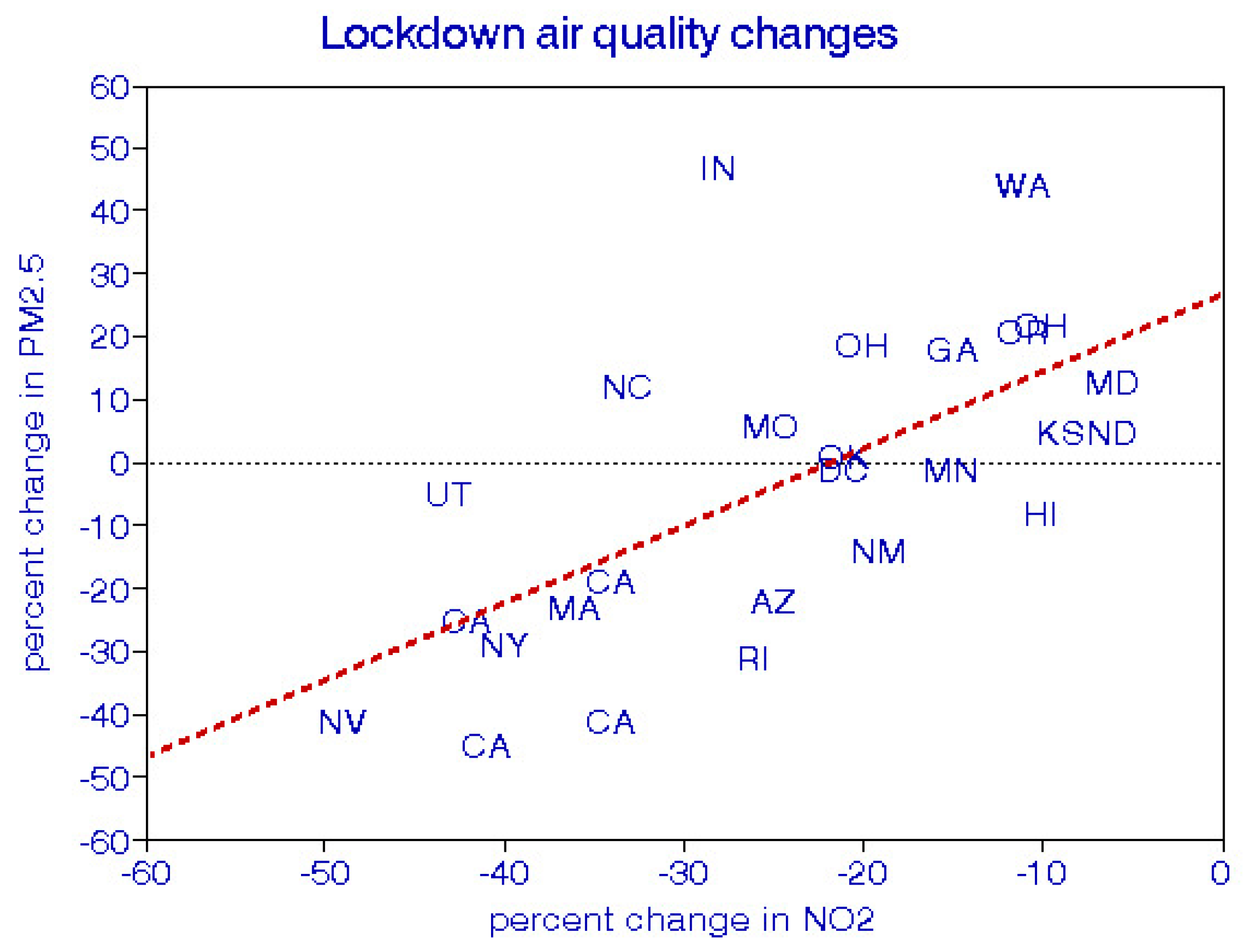
3.1. Effects of Pandemic Restrictions
3.2. Indoor Air Quality
3.3. Air Pollution and Virus Transmission
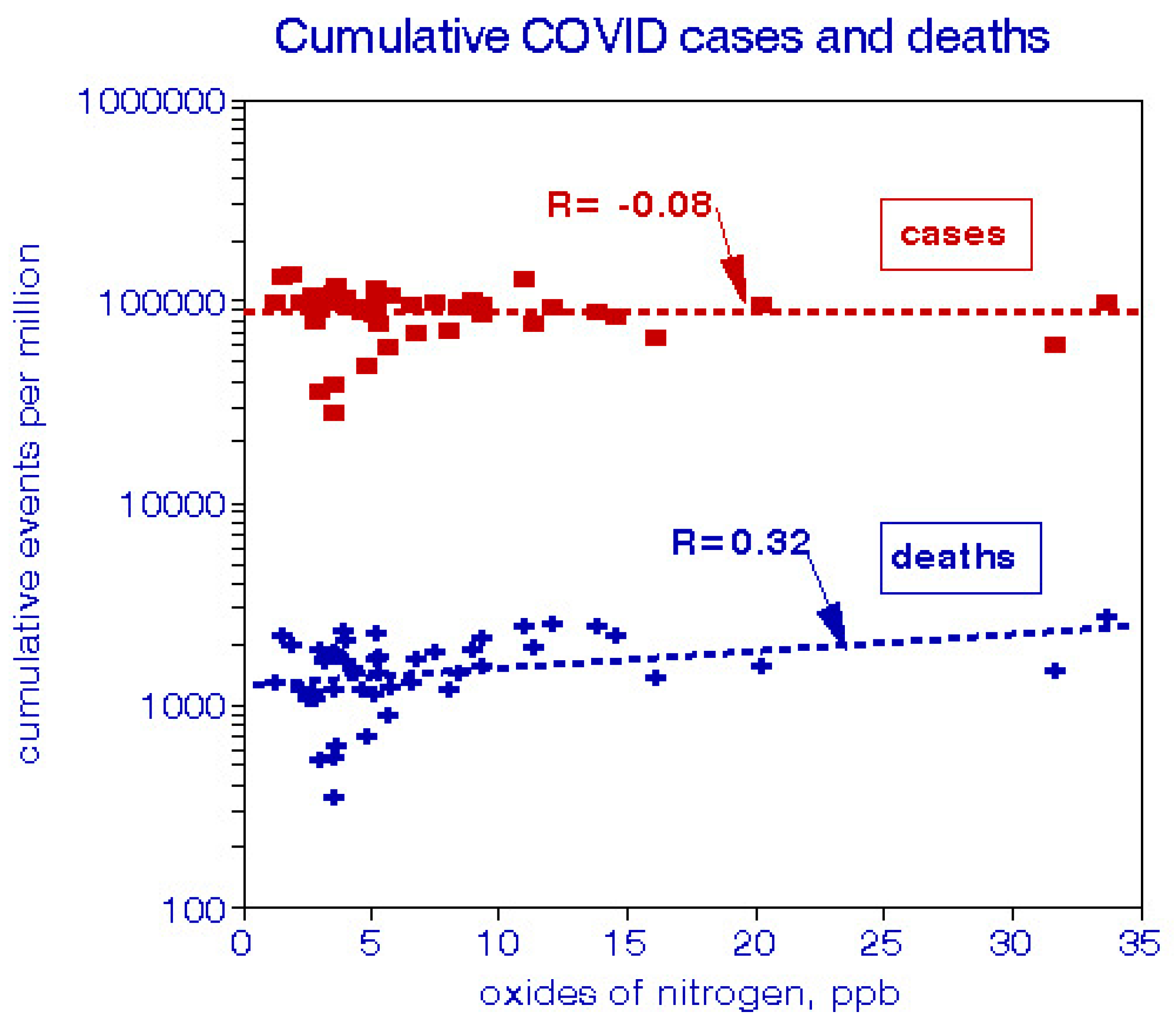
4. Cross-Sectional Analysis of Air Quality and Cumulative COVID-19 Cases and Deaths by State
4.1. Data and Methods
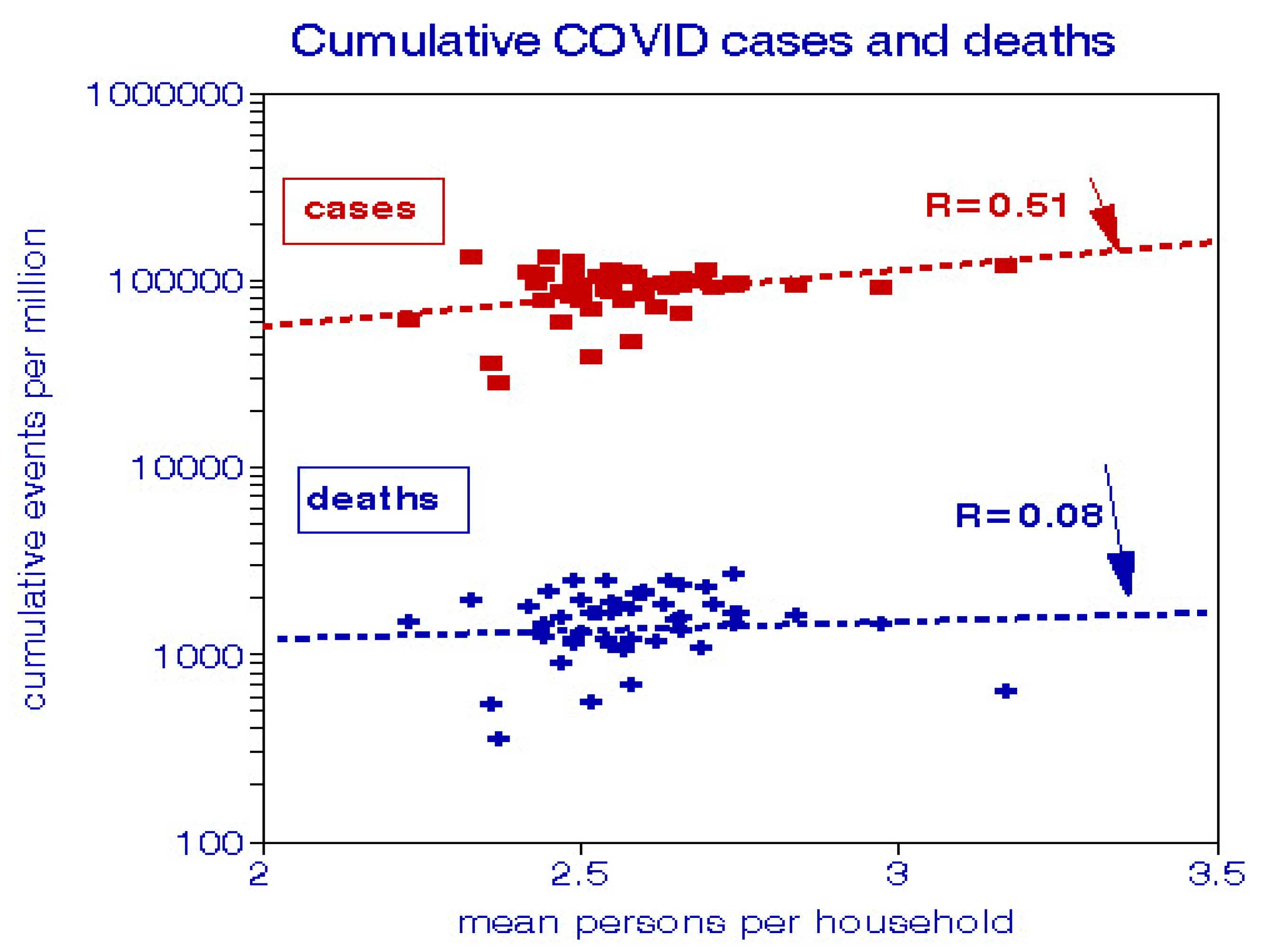
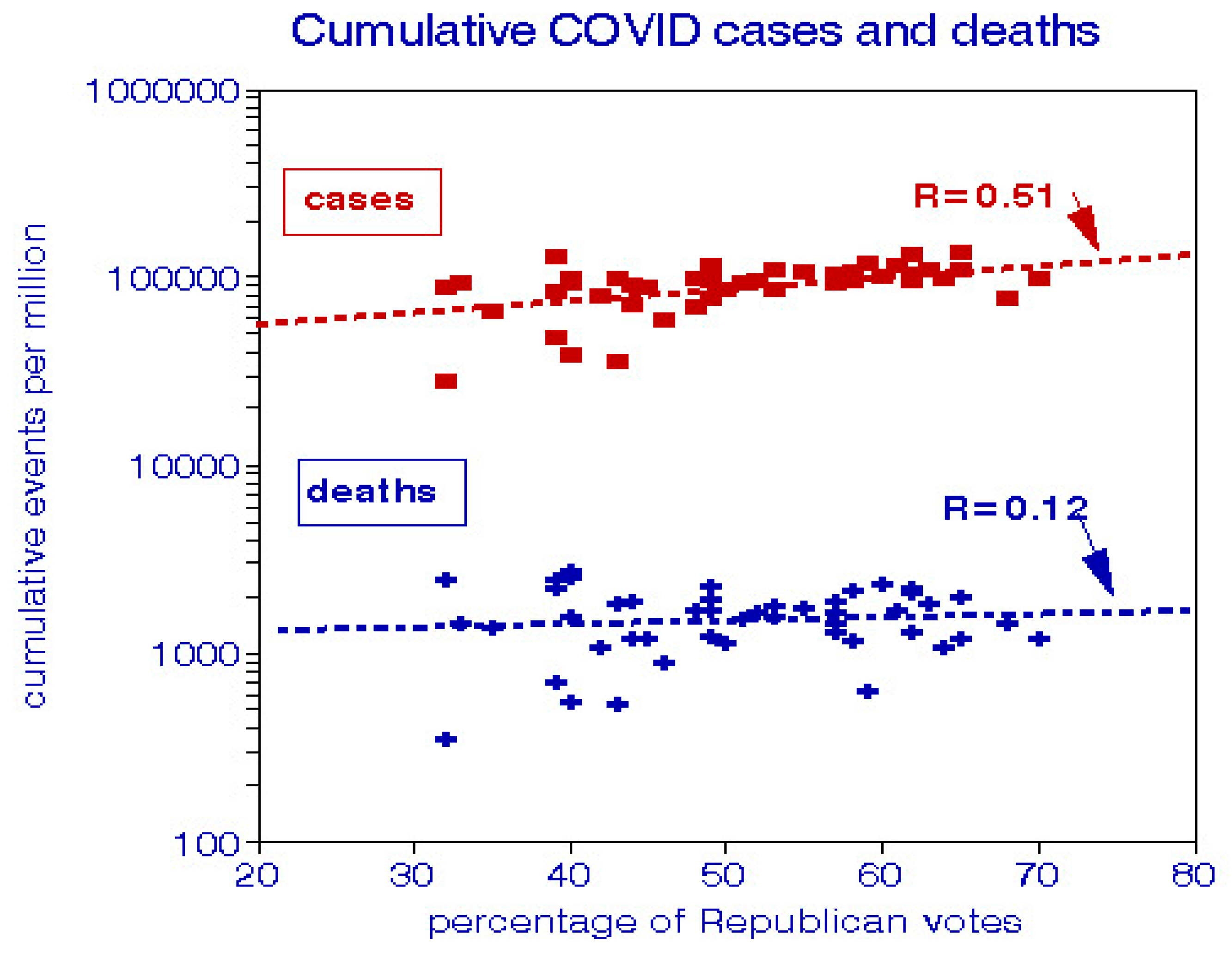
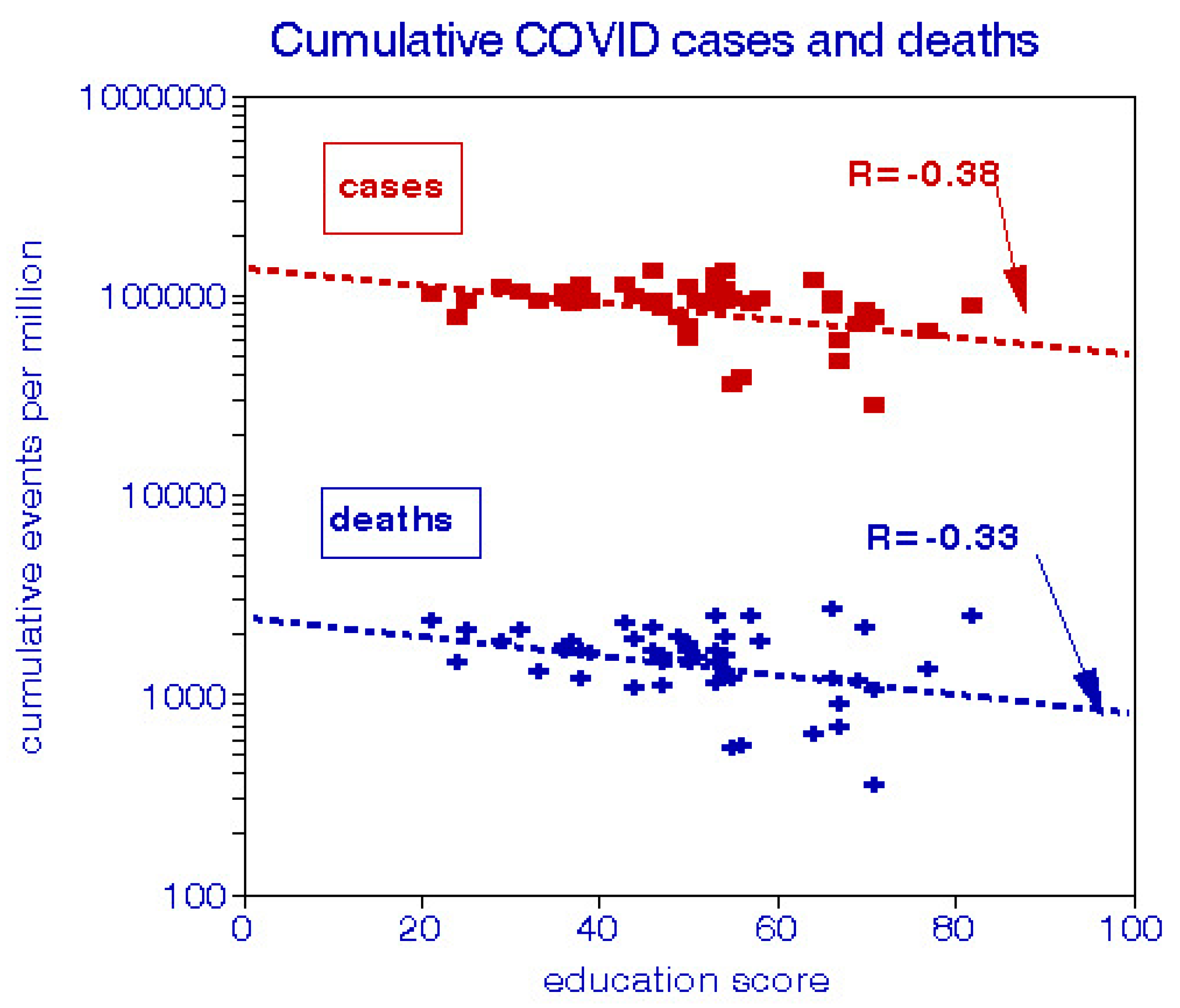
4.2. Results
4.3. Regression Analysis Discussion
4.4. Summary of the New Analysis
5. Overall Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- Abu-Rayash A, Dincer I. Analysis of mobility trends during the COVID-19 coronavirus pandemic: Exploring the impacts on global aviation and travel in selected cities. Energy Res Soc Sci. 2020 Oct;68:101693, doi:10.1016/j.erss.2020.101693.
- Adhikari A, Yin J. Short-Term Effects of Ambient Ozone, PM2.5 and Meteorological Factors on COVID-19 Confirmed Cases and Deaths in Queens, New York. Int J Environ Res Public Health. 2020 Jun 5;17(11):4047, doi:10.3390/ijerph17114047.
- Ali N, Islam F. The Effects of Air Pollution on COVID-19 Infection and Mortality-A Review on Recent Evidence. Front Public Health. 2020 Nov 26;8:580057, doi:10.3389/fpubh.2020.580057.
- Aljahdali MO, Alhassan AB, Albeladi MN. Impact of novel coronavirus disease (COVID-19) lockdown on ambient air quality of Saudi Arabia. Saudi J Biol Sci. 2021 Feb;28(2):1356-1364, doi:10.1016/j.sjbs.2020.11.065.
- Altuwayjiri A, Soleimanian E, Moroni S et al., The impact of stay-home policies during Coronavirus-19pandemic on the chemical and toxicological characteristics of ambient PM<sub>2.5</sub> in the metropolitan area of Milan, Italy. Sci Total Environ. 2021 Mar 1;758:143582, doi:0.1016/j.scitotenv.2020.143582.
- Arora S, Bhaukhandi KD, Mishra PK. Coronavirus lockdown helped the environment to bounce back. Sci Total Environ. 2020 Nov 10;742:140573, doi:10.1016/j.scitotenv.2020.140573.
- Azuma K, Yanagi U, Kagi N et al., Environmental factors involved in SARS-CoV-2 transmission: effect and role of indoor environmental quality in the strategy for COVID-19 infection control. Environ Health Prev Med. 2020 Nov 3;25(1):66, doi:10.1186/s12199-020-00904-2.
- Baldasano JM. COVID-19 lockdown effects on air quality by NO2 in the cities of Barcelona and Madrid (Spain). Sci Total Environ. 2020 Nov 1;741:140353, doi:10.1016/j.scitotenv.2020.140353.
- Bashir MF, Ma BJ, Bilal, Komal B et al. Correlation between environmental pollution indicators and COVID-19 pandemic: A brief study in Californian context. Environ Res. 2020 Aug;187:109652, doi:10.1016/j.envres.2020.109652.
- Bekbulat B, Apte JS, Millet DB et al. Changes in criteria air pollution levels in the US before, during, and after Covid-19 stay-at-home orders: Evidence from regulatory monitors. Sci Total Environ. 2021 May 15;769:144693, doi:10.1016/j.scitotenv.2020.144693.
- Bilal, Bashir MF, Benghoul M et al. Environmental pollution and COVID-19 outbreak: insights from Germany. Air Qual Atmos Health. 2020 Aug 3:1-10, doi:10.1007/s11869-020-00893-9.
- Borisova T, Komisarenko S. Air pollution particulate matter as a potential carrier of SARS-CoV-2 to the nervous system and/or neurological symptom enhancer: arguments in favor. Environ Sci Pollut Res Int. 2020 Oct 13:1–7, doi:10.1007/s11356-020-11183-3.
- Boroujeni M, Saberian M, Li J. Environmental impacts of COVID-19 on Victoria, Australia, witnessed two waves of Coronavirus. Environ Sci Pollut Res Int. 2021 Jan 28:1–10, doi:10.1007/s11356-021-12556-y.
- Bourdrel T, Annesi-Maesano I, Alahmad B, Maesano CN, Bind MA. The impact of outdoor air pollution on COVID-19: a review of evidence from <i>in vitro</i>, animal, and human studies. Eur Respir Rev. 2021 Feb 9;30(159):200242, doi:10.1183/16000617.0242-2020.
- Brandt EB, Mersha TB. Environmental Determinants of Coronavirus Disease 2019 (COVID-19). Curr Allergy Asthma Rep. 2021 Mar 5;21(3):15, doi:10.1007/s11882-021-00993-1.
- Cao Y, Shao L, Jones T et al., Multiple relationships between aerosol and COVID-19: A framework for global studies. Gondwana Res. 2021 May;93:243-251, doi:10.1016/j.gr.2021.02.002.
- Cascetta E, Henke I, Di Francesco L. The Effects of Air Pollution, Sea Exposure and Altitude on COVID-19 Hospitalization Rates in Italy. Int J Environ Res Public Health. 2021 Jan 8;18(2):452, doi:10.3390/ijerph18020452.
- Chauhan A, Singh RP. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ Res. 2020 Aug;187:109634, doi:10.1016/j.envres.2020.109634.
- Chen B, Jia P, Han J. Role of indoor aerosols for COVID-19 viral transmission: a review. Environ Chem Lett. 2021 Jan 13:1-18, doi:10.1007/s10311-020-01174-8.
- Chen LA, Chien LC, Li Y, Lin G. Nonuniform impacts of COVID-19 lockdown on air quality over the United States. Sci Total Environ. 2020 Nov 25;745:141105, doi:10.1016/j.scitotenv.2020.141105.
- Chirizzi D, Conte M, Feltracco M et al., SARS-CoV-2 concentrations and virus-laden aerosol size distributions in outdoor air in north and south of Italy. Environ Int. 2021 Jan;146:106255, doi:10.1016/j.envint.2020.106255.
- Cole MA, Ozgen C, Strobl E. Air Pollution Exposure and Covid-19 in Dutch Municipalities. Environ Resour Econ (Dordr). 2020 Aug 4:1-30, doi:10.1007/s10640-020-00491-4.
- Collivignarelli MC, Abbà A, Bertanza G et al., Lockdown for CoViD-2019 in Milan: What are the effects on air quality? Sci Total Environ. 2020 Aug 25;732:139280, doi:10.1016/j.scitotenv.2020.139280.
- Collivignarelli MC, Abbà A, Caccamo FM et al. Can particulate matter be identified as the primary cause of the rapid spread of CoViD-19 in some areas of Northern Italy? Environ Sci Pollut Res Int. 2021 Feb 26:1–13, doi:10.1007/s11356-021-12735-x.
- Comunian S, Dongo D, Milani C, Palestini P. Air Pollution and Covid-19: The Role of Particulate Matter in the Spread and Increase of Covid-19’s Morbidity and Mortality. Int J Environ Res Public Health. 2020 Jun 22;17(12):4487, doi:10.3390/ijerph17124487.
- Connerton P, Vicente de Assunção J et al., Air Quality during COVID-19 in Four Megacities: Lessons and Challenges for Public Health. Int J Environ Res Public Health. 2020 Jul 14;17(14):5067, doi:0.3390/ijerph17145067.
- Copat C, Cristaldi A, Fiore M et al. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: A systematic review. Environ Res. 2020 Dec;191:110129, doi:10.1016/j.envres.2020.110129.
- Cox LA Jr, Popken DA. Should air pollution health effects assumptions be tested? Fine particulate matter and COVID-19 mortality as an example. Glob Epidemiol. 2020 Nov;2:100033, doi:0.1016/j.gloepi.2020.100033.
- Crane-Godreau MA, Clem KJ, Payne P, Fiering S. Vitamin D Deficiency and Air Pollution Exacerbate COVID-19 Through Suppression of Antiviral Peptide LL37. Front Public Health. 2020 May 28;8:232, doi:10.3389/fpubh.2020.00232.
- Dai Q, Ding J, Song C et al., Changes in source contributions to particle number concentrations after the COVID-19 outbreak: Insights from a dispersion normalized PMF. Sci Total Environ. 2021 Mar 10;759:143548, doi:10.1016/j.scitotenv.2020.143548.
- Dai Q, Liu B, Bi X et al., Dispersion Normalized PMF Provides Insights into the Significant Changes in Source Contributions to PM2.5 after the COVID-19 Outbreak. Environ Sci Technol. 2020 Aug 18;54(16):9917-9927, doi:10.1021/acs.est.0c02776.
- Datta A, Rahman MH, Suresh R. Did the COVID-19 lockdown in Delhi and Kolkata improve the ambient air quality of the two cities? J Environ Qual. 2021 Jan 7.doi:10.1002/jeq2.20192.
- Dettori M, Deiana G, Balletto G et al., Air pollutants and risk of death due to COVID-19 in Italy. Environ Res. 2021 Jan;192:110459, doi:10.1016/j.envres.2020.110459.
- Dhaka SK, Chetna, Kumar V et al., PM2.5 Diminution and haze events over Delhi during the COVID-19 lockdown period: an interplay between the baseline pollution and meteorology. Sci Rep. 2020 Aug 10;10(1):13442, doi:10.1038/s41598-020-70179-8.
- Dharmaraj S, Ashokkumar V, Hariharan S et al., The COVID-19 pandemic face mask waste: A blooming threat to the marine environment. Chemosphere. 2021 Jan 9;272:129601, doi:10.1016/j.chemosphere.2021.129601.
- Diamond MS, Wood R. Limited Regional Aerosol and Cloud Microphysical Changes Despite Unprecedented Decline in Nitrogen Oxide Pollution During the February 2020 COVID-19 Shutdown in China. Geophys Res Lett. 2020 Sep 16;47(17):e2020GL088913, doi:10.1029/2020GL088913.
- Dobson R, Semple S. Changes in outdoor air pollution due to COVID-19 lockdowns differ by pollutant: evidence from Scotland. Occup Environ Med. 2020 Nov;77(11):798-800, doi:10.1136/oemed-2020-106659.
- Domingo JL, Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ Res. 2020 Aug;187:109650, doi:10.1016/j.envres.2020.109650.
- Domínguez-Amarillo S, Fernández-Agüera J, Cesteros-García S, González-Lezcano RA. Bad Air Can Also Kill: Residential Indoor Air Quality and Pollutant Exposure Risk during the COVID-19 Crisis. Int J Environ Res Public Health. 2020 Sep 30;17(19):7183, doi:10.3390/ijerph17197183.
- Donzelli G, Cioni L, Cancellieri M et al., Relations between Air Quality and Covid-19 Lockdown Measures in Valencia, Spain. Int J Environ Res Public Health. 2021 Feb 26;18(5):2296, doi:10.3390/ijerph18052296.
- Dragone R, Licciardi G, Grasso G, Del Gaudio C, Chanussot J. Analysis of the Chemical and Physical Environmental Aspects that Promoted the Spread of SARS-CoV-2 in the Lombard Area. Int J Environ Res Public Health. 2021 Jan 29;18(3):1226, doi:10.3390/ijerph18031226.
- El-Sheekh MM, Hassan IA. Lockdowns and reduction of economic activities during the COVID-19 pandemic improved air quality in Alexandria, Egypt. Environ Monit Assess. 2020 Dec 15;193(1):11, doi:10.1007/s10661-020-08780-7.
- Elliott J, Bodinier B, Whitaker M et al., COVID-19 mortality in the UK Biobank cohort: revisiting and evaluating risk factors. Eur J Epidemiol. 2021 Feb 15:1–11, doi:10.1007/s10654-021-00722-y.
- Fan Z, Zhan Q, Yang C, Liu H, Zhan M. How Did Distribution Patterns of Particulate Matter Air Pollution (PM2.5 and PM10) Change in China during the COVID-19 Outbreak: A Spatiotemporal Investigation at Chinese City-Level. Int J Environ Res Public Health. 2020 Aug 28;17(17):6274, doi:10.3390/ijerph17176274.
- Fiasca F, Minelli M, Maio D et al., Associations between COVID-19 Incidence Rates and the Exposure to PM2.5 and NO2: A Nationwide Observational Study in Italy. Int J Environ Res Public Health. 2020 Dec 13;17(24):9318, doi:10.3390/ijerph17249318.
- Gama C, Relvas H, Lopes M, Monteiro A. The impact of COVID-19 on air qualityls in Portugal: A way to assess traffic contribution. Environ Res. 2021 Feb;193:110515, doi:10.1016/j.envres.2020.110515.
- Gautam S. The Influence of COVID-19 on Air Quality in India: A Boon or Inutile. Bull Environ Contam Toxicol. 2020 Jun;104(6):724-726, doi:10.1007/s00128-020-02877-y.
- Gayen A, Haque SM, Mishra SV. COVID-19 induced lockdown and decreasing particulate matter (PM10): An empirical investigation of an Asian megacity. Urban Clim. 2021 Mar;36:100786, doi:10.1016/j.uclim.2021.100786.
- Girdhar A, Kapur H, Kumar V, Kaur M, Singh D, Damasevicius R. Effect of COVID-19 outbreak on urban health and environment. Air Qual Atmos Health. 2020 Oct 10:1-9, doi:10.1007/s11869-020-00944-1.
- Gualtieri G, Brilli L, Carotenuto F, Vagnoli C, Zaldei A, Gioli B. Quantifying road traffic impact on air quality in urban areas: A Covid19-induced lockdown analysis in Italy. Environ Pollut. 2020 Dec;267:115682, doi:10.1016/j.envpol.2020.115682.
- Hendryx M, Luo J. COVID-19 prevalence and fatality rates in association with air pollution emission concentrations and emission sources. Environ Pollut. 2020 Oct;265(Pt A):115126, doi:10.1016/j.envpol.2020.115126.
- Hudda N, Simon MC, Patton AP, Durant JL. Reductions in traffic-related black carbon and ultrafine particle number concentrations in an urban neighborhood during the COVID-19 pandemic. Sci Total Environ. 2020 Nov 10;742:140931, doi:10.1016/j.scitotenv.2020.140931.
- Jephcote C, Hansell AL, Adams K, Gulliver J. Changes in air quality during COVID-19 ’lockdown’ in the United Kingdom. Environ Pollut. 2021 Mar 1;272:116011, doi:10.1016/j.envpol.2020.116011.
- Ju MJ, Oh J, Choi YH. Changes in air pollution levels after COVID-19 outbreak in Korea. Sci Total Environ. 2021 Jan 1;750:141521, doi:10.1016/j.scitotenv.2020.141521.
- Han BS, Park K, Kwak KH et al. Air Quality Change in Seoul, South Korea under COVID-19 Social Distancing: Focusing on PM2.5. Int J Environ Res Public Health. 2020 Aug 27;17(17):6208, doi:10.3390/ijerph17176208.
- Hashim BM, Al-Naseri SK, Al-Maliki A, Al-Ansari N. Impact of COVID-19 lockdown on NO<sub>2</sub>, O3, PM2.5 and PM10 concentrations and assessing air quality changes in Baghdad, Iraq. Sci Total Environ. 2021 Feb 1;754:141978, doi:10.1016/j.scitotenv.2020.141978.
- He C, Hong S, Zhang L,et al. Global, continental, and national variation in PM2.5, O3, and NO2 concentrations during the early 2020 COVID-19 lockdown. Atmos Pollut Res. 2021 Mar;12(3):136-145, doi:10.1016/j.apr.2021.02.002.
- Hoang T, Nguyen TQ, Tran TTA. Short-term exposure to ambient air pollution in association with COVID-19 of two clusters in South Korea. Trop Med Int Health. 2020 Dec 15, doi:10.1111/tmi.13538.
- Hou CK, Qin YF, Wang G et al., Impact of a long-term air pollution exposure on the case fatality rate of COVID-19 patients-A multicity study. J Med Virol. 2021 Jan 20, doi:10.1002/jmv.26807.
- Hutter HP, Poteser M, Moshammer H et al., Air Pollution Is Associated with COVID-19 Incidence and Mortality in Vienna, Austria. Int J Environ Res Public Health. 2020 Dec 11;17(24):9275, doi:10.3390/ijerph17249275.
- Ikhlasse H, Benjamin D, Vincent C, Hicham M. Environmental impacts of pre/during and post-lockdown periods on prominent air pollutants in France. Environ Dev Sustain. 2021 Jan 23:1-22, doi:10.1007/s10668-021-01241-2.
- Jiang Y, Wu XJ, Guan YJ. Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infect Control Hosp Epidemiol. 2020 Sep;41(9):1011-1015, doi:10.1017/ice.2020.222.
- Jiaxin C, Hui H, Feifei W,e al. Air quality characteristics in Wuhan (China) during the 2020 COVID-19 pandemic. Environ Res. 2021 Feb 16:110879, doi:10.1016/j.envres.2021.110879.
- Ju MJ, Oh J, Choi YH. Changes in air pollution levels after COVID-19 outbreak in Korea. Sci Total Environ. 2021 Jan 1;750:141521, doi:10.1016/j.scitotenv.2020.141521.
- Kerimray A, Baimatova N, Ibragimova OP et al., Changes in air quality related to the control of coronavirus in China: Implications for traffic and industrial emissions. Sci Total Environ. 2020 Aug 20;731:139133, doi:10.1016/j.scitotenv.2020.139133.
- Kerimray A, Baimatova N, Ibragimova OP et al. Assessing air quality changes in large cities during COVID-19 lockdowns: The impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci Total Environ. 2020 Aug 15;730:139179, doi:10.1016/j.scitotenv.2020.139179.
- Khan I, Shah D, Shah SS. COVID-19 pandemic and its positive impacts on environment: an updated review. Int J Environ Sci Technol (Tehran). 2020 Nov 16:1-10, doi:10.1007/s13762-020-03021-3.
- Kolluru SSR, Patra AK, Nazneen, Shiva Nagendra SM. Association of air pollution and meteorological variables with COVID-19 incidence: Evidence from five megacities in India. Environ Res. 2021 Feb 6;195:110854, doi:10.1016/j.envres.2021.110854.
- Konstantinoudis G, Padellini T, Bennett et al. Long-term exposure to air-pollution and COVID-19 mortality in England: a hierarchical spatial analysis. medRxiv [Preprint]. 2020 Aug 11:2020.08.10.20171421, doi:10.1101/2020.08.10.20171421. Update in: Environ Int. 2021 Jan;146:106316.
- Kumar H, Arora R, Kumar Arora P et al. Effect of nation-wide lock-down due to Covid-19 over industrial pollution in Delhi, India. Mater Today Proc. 2021 Jan 26, doi:10.1016/j.matpr.2021.01.264.
- Kumar P, Hama S, Omidvarborna H et al., Temporary reduction in fine particulate matter due to anthropogenic emissions switch-off’ during COVID-19 lockdown in Indian cities. Sustain Cities Soc. 2020 Nov;62:102382, doi:10.1016/j.scs.2020.102382.
- Kumar S, Sonkar SK, Atam I et al., Socio-economic impact of first 21 days nationwide lockdown- 1 on the spread of SARS-COV-2 in India in relation to health. J Family Med Prim Care. 2020 Sep 30;9(9):4557-4562, doi:10.4103/jfmpc.jfmpc_662_20.
- Kumari P, Toshniwal D. Impact of lockdown on air quality over major cities across the globe during COVID-19 pandemic. Urban Clim. 2020 Dec;34:100719, doi:10.1016/j.uclim.2020.100719.
- Kutralam-Muniasamy G, Pérez-Guevara F, Roy PD, Elizalde-Martínez I, Shruti VC. Impacts of the COVID-19 lockdown on air quality and its association with human mortality trends in megapolis Mexico City. Air Qual Atmos Health. 2020 Oct 28:1-10, doi:10.1007/s11869-020-00960-1.
- Landoni G, Lembo R, Cianfanelli L, Frontera A. Air pollutants and SARS-CoV-2 in 33 European countries. Acta Biomed. 2021 Feb 16;92(1):e2021166, doi:10.23750/abm.v92i1.11155.
- Latif MT, Dominick D, Hawari NSSL, Mohtar AAA, Othman M. The concentration of major air pollutants during the movement control order due to the COVID-19 pandemic in the Klang Valley, Malaysia. Sustain Cities Soc. 2021 Mar;66:102660, doi:10.1016/j.scs.2020.102660
- Le T, Wang Y, Liu L et al., Unexpected air pollution with marked emission reductions during the COVID-19 outbreak in China. Science. 2020 Aug 7;369(6504):702-706, doi:10.1126/science.abb7431.
- Li J, Wang Z, Yuan B, Liang H, Liang W. The Episode of National Lockdown in the Pandemic: Air Traffic Restriction as the Control Strategy and Its Impact on Existing Cases and Recovery Rate of Novel Coronavirus Disease in Megacities of China. Disaster Med Public Health Prep. 2020 Oct;14(5):e19-e23, doi:10.1017/dmp.2020.294.
- Li H, Xu XL, Dai DW et al. Air pollution and temperature are associated with increased COVID-19 incidence: A time series study. Int J Infect Dis. 2020 Aug;97:278-282, doi:10.1016/j.ijid.2020.05.076.
- Lian X, Huang J, Huang R et al., Impact of city lockdown on the air quality of COVID-19-hit of Wuhan city. Sci Total Environ. 2020 Nov 10;742:140556, doi:10.1016/j.scitotenv.2020.140556.
- Liang D, Shi L, Zhao J et al., Urban Air Pollution May Enhance COVID-19 Case-Fatality and Mortality Rates in the United States. Innovation (N Y). 2020 Nov 25;1(3):100047, doi:10.1016/j.xinn.2020.100047.
- Liang D, Shi L, Zhao J et al., Urban Air Pollution May Enhance COVID-19 Case-Fatality and Mortality Rates in the United States. medRxiv [Preprint]. 2020 May 7:2020.05.04.20090746, doi:0.1101/2020.05.04.20090746. Update in: Innovation (N Y). 2020 Sep 21;:100047.
- Liu F, Wang M, Zheng M. Effects of COVID-19 lockdown on global air quality and health. Sci Total Environ. 2021 Feb 10;755(Pt 1):142533, doi:10.1016/j.scitotenv.2020.142533.
- Lv Z, Wang X, Deng F, Ying Q et al., Source-Receptor Relationship Revealed by the Halted Traffic and Aggravated Haze in Beijing during the COVID-19 Lockdown. Environ Sci Technol. 2020 Dec 15;54(24):15660-15670, doi:10.1021/acs.est.0c04941.
- López-Feldman A, Heres D, Marquez-Padilla F. Air pollution exposure and COVID-19: A look at mortality in Mexico City using individual-level data. Sci Total Environ. 2021 Feb 20;756:143929, doi:10.1016/j.scitotenv.2020.143929.
- Magazzino C, Mele M, Sarkodie SA. The nexus between COVID-19 deaths, air pollution and economic growth in New York state: Evidence from Deep Machine Learning. J Environ Manage. 2021 Mar 2;286:112241, doi:10.1016/j.jenvman.2021.112241.
- Magazzino C, Mele M, Schneider N. The relationship between air pollution and COVID-19-related deaths: An application to three French cities. Appl Energy. 2020 Dec 1;279:115835, doi:10.1016/j.apenergy.2020.115835.
- Manoj MG, Satheesh Kumar MK et al., Potential link between compromised air quality and transmission of the novel corona virus (SARS-CoV-2) in affected areas. Environ Res. 2020 Nov;190:110001, doi:10.1016/j.envres.2020.110001.
- Markandeya, Verma PK, Mishra V et al. Spatio-temporal assessment of ambient air quality, their health effects and improvement during COVID-19 lockdown in one of the most polluted cities of India. Environ Sci Pollut Res Int. 2021 Mar;28(9):10536-10551, doi:10.1007/s11356-020-11248-3.
- Manigrasso M, Protano C, Guerriero E, Vitali M. May SARS-CoV-2 diffusion be favored by alkaline aerosols and ammonia emissions? Atmosphere 2020, 11(9), 995; doi:10.3390/atmos11090995.
- Megahed NA, Ghoneim EM. Indoor Air Quality: Rethinking rules of building design strategies in post-pandemic architecture. Environ Res. 2021 Feb;193:110471, doi:10.1016/j.envres.2020.110471.
- Mele M, Magazzino C, Schneider N, Strezov V. NO2 levels as a contributing factor to COVID-19 deaths: The first empirical estimate of threshold values. Environ Res. 2021 Mar;194:110663, doi:10.1016/j.envres.2020.110663.
- Mendez-Espinosa JF, Rojas NY, Vargas J, Pachón JE, Belalcazar LC, Ramírez O. Air quality variations in Northern South America during the COVID-19 lockdown. Sci Total Environ. 2020 Dec 20;749:141621, doi:10.1016/j.scitotenv.2020.141621.
- Mendy A, Wu X, Keller JL et al. Long-term exposure to fine particulate matter and hospitalization in COVID-19 patients. Respir Med. 2021 Mar;178:106313, doi:10.1016/j.rmed.2021.106313.
- Meng J, Li Z, Zhou R, Chen M et al., Enhanced photochemical formation of secondary organic aerosols during the COVID-19 lockdown in Northern China. Sci Total Environ. 2021 Mar 1;758:143709, doi:10.1016/j.scitotenv.2020.143709.
- Menut L, Bessagnet B, Siour G, e al. Impact of lockdown measures to combat Covid-19 on air quality over western Europe. Sci Total Environ. 2020 Nov 1;741:140426, doi:10.1016/j.scitotenv.2020.140426.
- Meo SA, Abukhalaf AA, Alomar AA et al. Effect of environmental pollutants PM2.5, carbon monoxide, and ozone on the incidence and mortality of SARS-COV-2 infection in ten wildfire affected counties in California. Sci Total Environ. 2021 Feb 25;757:143948, doi:10.1016/j.scitotenv.2020.143948.
- Meo SA, Abukhalaf AA, Alomar AA, Alessa OM. Wildfire and COVID-19 pandemic: effect of environmental pollution PM-2.5 and carbon monoxide on the dynamics of daily cases and deaths due to SARS-COV-2 infection in San-Francisco USA. Eur Rev Med Pharmacol Sci. 2020 Oct;24(19):10286-10292, doi:10.26355/eurrev_202010_23253.
- Miyazaki K, Bowman K, Sekiya T et al. Air Quality Response in China Linked to the 2019 Novel Coronavirus (COVID-19) Lockdown. Geophys Res Lett. 2020 Oct 16;47(19):e2020GL089252, doi:10.1029/2020GL089252.
- Mousazadeh M, Paital B, Naghdali Z et al., Positive environmental effects of the coronavirus 2020 episode: a review. Environ Dev Sustain. 2021 Feb 4:1-23, doi:10.1007/s10668-021-01240-3.
- Naethe P, Delaney M, Julitta T. Changes of NOx in urban air detected with monitoring VIS-NIR field spectrometer during the coronavirus pandemic: A case study in Germany. Sci Total Environ. 2020 Dec 15;748:141286, doi:10.1016/j.scitotenv.2020.141286.
- Nakada LYK, Urban RC. COVID-19 pandemic: Impacts on the air quality during the partial lockdown in São Paulo state, Brazil. Sci Total Environ. 2020 Aug 15;730:139087, doi:0.1016/j.scitotenv.2020.139087.
- Naqvi HR, Mutreja G, Shakeel A, Siddiqui MA. Spatio-temporal analysis of air quality and its relationship with major COVID-19 hotspot places in India. Remote Sens Appl. 2021 Apr;22:100473, doi:10.1016/j.rsase.2021.100473.
- Naqvi HR, Datta M, Mutreja G et al., Improved air quality and associated mortalities in India under COVID-19 lockdown. Environ Pollut. 2021 Jan 1;268(Pt A):115691, doi:10.1016/j.envpol.2020.115691.
- Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin-Neelon SE. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. medRxiv [Preprint]. 2020 Sep 11:2020.09.09.20191643, doi:10.1101/2020.09.09.20191643.
- Nigam R, Pandya K, Luis AJ et al., Positive effects of COVID-19 lockdown on air quality of industrial cities (Ankleshwar and Vapi) of Western India. Sci Rep. 2021 Feb 19;11(1):4285, doi:10.1038/s41598-021-83393-9.
- Pant G, Alka, Garlapati D, Gaur A et al. Air quality assessment among populous sites of major metropolitan cities in India during COVID-19 pandemic confinement. Environ Sci Pollut Res Int. 2020 Dec;27(35):44629-44636, doi:10.1007/s11356-020-11061-y.
- Pata UK. How is COVID-19 affecting environmental pollution in US cities? Evidence from asymmetric Fourier causality test. Air Qual Atmos Health. 2020 Jul 15:1-7, doi:10.1007/s11869-020-00877-9.
- Patel H, Talbot N, Salmond J et al., Implications for air quality management of changes in air quality during lockdown in Auckland (New Zealand) in response to the 2020 SARS-CoV-2 epidemic. Sci Total Environ. 2020 Dec 1;746:141129, doi:10.1016/j.scitotenv.2020.141129.
- Pei L, Wang X, Guo B et al., Do air pollutants as well as meteorological factors impact Corona Virus Disease 2019 (COVID-19)? Evidence from China based on the geographical perspective. Environ Sci Pollut Res Int. 2021 Mar 5:1–13, doi:10.1007/s11356-021-12934-6.
- Pradillo BL, Rancan L, Ramiro ED,et al. Determination of SARS-CoV-2 RNA in different particulate matter size fractions of outdoor air samples in Madrid during the lockdown. Environ Res. 2021 Feb 17;195:110863, doi:10.1016/j.envres.2021.110863.
- Pata UK. How is COVID-19 affecting environmental pollution in US cities? Evidence from asymmetric Fourier causality test. Air Qual Atmos Health. 2020 Jul 15:1-7, doi:10.1007/s11869-020-00877-9.
- Pei L, Wang X, Guo B et al., Do air pollutants as well as meteorological factors impact Corona Virus Disease 2019 (COVID-19)? Evidence from China based on the geographical perspective. Environ Sci Pollut Res Int. 2021 Mar 5:1–13, doi:10.1007/s11356-021-12934-6.
- Pradillo BL, Rancan L, Ramiro ED,et al. Determination of SARS-CoV-2 RNA in different particulate matter size fractions of outdoor air samples in Madrid during the lockdown. Environ Res. 2021 Feb 17;195:110863, doi:10.1016/j.envres.2021.110863.
- Rojas JP, Urdanivia FR, Garay RA et al., Effects of COVID-19 pandemic control measures on air pollution in Lima metropolitan area, Peru in South America. Air Qual Atmos Health. 2021 Feb 4:1-9, doi:10.1007/s11869-021-00990-3.
- Ropkins K, Tate JE. Early observations on the impact of the COVID-19 lockdown on air quality trends across the UK. Sci Total Environ. 2021 Feb 1;754:142374, doi:10.1016/j.scitotenv.2020.142374.
- Roy S, Singha N. Reduction in concentration of PM<sub>2.5</sub> in India’s top most polluted cities: with special reference to post-lockdown period. Air Qual Atmos Health. 2021 Jan 8:1-9, doi:10.1007/s11869-020-00974-9.
- Rupani PF, Nilashi M, Abumalloh RA et al., Coronavirus pandemic (COVID-19) and its natural environmental impacts. Int J Environ Sci Technol (Tehran). 2020 Sep 1:1-12, doi:10.1007/s13762-020-02910-x.
- Saadat S, Rawtani D, Hussain CM. Environmental perspective of COVID-19. Sci Total Environ. 2020 Aug 1;728:138870, doi:10.1016/j.scitotenv.2020.138870.
- Saez M, Tobias A, Barceló MA. Effects of long-term exposure to air pollutants on the spatial spread of COVID-19 in Catalonia, Spain. Environ Res. 2020 Dec;191:110177, doi:10.1016/j.envres.2020.110177.
- Sahoo Mangla S, Pathak AK, Salãmao GN, Sarkar D. Pre-to-post lockdown impact on air quality and the role of environmental factors in spreading the COVID-19 cases - a study from a worst-hit state of India. Int J Biometeorol. 2021 Feb;65(2):205-222, doi:10.1007/s00484-020-02019-3.
- SanJuan-Reyes S, Gómez-Oliván LM, Islas-Flores H. COVID-19 in the environment. Chemosphere. 2021 Jan;263:127973, doi:10.1016/j.chemosphere.2020.127973.
- Sannigrahi S, Kumar P, Molter A et al. Examining the status of improved air quality in world cities due to COVID-19 led temporary reduction in anthropogenic emissions. Environ Res. 2021 Mar 3:110927, doi:10.1016/j.envres.2021.110927.
- Sbai SE, Mejjad N, Norelyaqine A, Bentayeb F. Air quality change during the COVID-19 pandemic lockdown over the Auvergne-Rhône-Alpes region, France. Air Qual Atmos Health. 2021 Jan 19:1-12, doi:10.1007/s11869-020-00965-w.
- Senatore V, Zarra T, Buonerba A et al., Indoor versus outdoor transmission of SARS-COV-2: environmental factors in virus spread and underestimated sources of risk. EuroMediterr J Environ Integr. 2021;6(1):30, doi:10.1007/s41207-021-00243-w.
- Shakoor A, Chen X, Farooq TH et al. Fluctuations in environmental pollutants and air quality during the lockdown in the USA and China: two sides of COVID-19 pandemic. Air Qual Atmos Health. 2020 Aug 9:1-8, doi:10.1007/s11869-020-00888-6.
- Shakil MH, Munim ZH, Tasnia M, Sarowar S. COVID-19 and the environment: A critical review and research agenda. Sci Total Environ. 2020 Nov 25;745:141022, doi:10.1016/j.scitotenv.2020.141022.
- Skalny AV, Lima TRR, Ke T et al. Toxic metal exposure as a possible risk factor for COVID-19 and other respiratory infectious diseases. Food Chem Toxicol. 2020 Dec;146:111809, doi:10.1016/j.fct.2020.111809. Erratum in: Food Chem Toxicol. 2021 Mar;149:111999.
- Sharma AK, Balyan P. Air pollution and COVID-19: Is the connect worth its weight? Indian J Public Health. 2020 Jun;64(Supplement):S132-S134, doi:10.4103/ijph.IJPH_466_20.
- Singh V, Singh S, Biswal A, Diurnal and temporal changes in air pollution during COVID-19 strict lockdown over different regions of India. Environ Pollut. 2020 Nov;266(Pt 3):115368, doi:10.1016/j.envpol.2020.115368.
- Son JY, Fong KC, Heo S, et l. Reductions in mortality resulting from reduced air pollution levels due to COVID-19 mitigation measures. Sci Total Environ. 2020 Nov 20;744:141012, doi:0.1016/j.scitotenv.2020.141012.
- Suwanwongse K, Shabarek N. Epidemiology, clinical features, and outcomes of hospitalized infants with COVID-19 in the Bronx, New York. Arch Pediatr. 2020 Oct;27(7):400-401, doi:10.1016/j.arcped.2020.07.009.
- Tanwar V, Adelstein JM, Wold LE. Double trouble: combined cardiovasculareffects of particulate matter exposure and coronavirus disease 2019. Cardiovasc Res. 2021 Jan 1;117(1):85-95, doi:10.1093/cvr/cvaa293.
- Toro A R, Catalán F, Urdanivia FR et al. Air pollution and COVID-19 lockdown in a large South American city: Santiago Metropolitan Area, Chile. Urban Clim. 2021 Mar;36:100803, doi:10.1016/j.uclim.2021.100803.
- Versaci F, Gaspardone A, Danesi A,et al. Interplay between COVID-19, pollution, and weather features on changes in the incidence of acute coronary syndromes in early 2020. Int J Cardiol. 2021 Apr 15;329:251-259, doi:10.1016/j.ijcard.2020.12.059.
- Villeneuve PJ, Goldberg MS. Methodological Considerations for Epidemiological Studies of Air Pollution and the SARS and COVID-19 Coronavirus Outbreaks. Environ Health Perspect. 2020 Sep;128(9):95001, doi:10.1289/EHP7411.
- Vultaggio M, Varrica D, Alaimo MG. Impact on Air Quality of the COVID-19 Lockdown in the Urban Area of Palermo (Italy). Int J Environ Res Public Health. 2020 Oct 9;17(20):7375, doi:10.3390/ijerph17207375.
- Wang H, Miao Q, Shen L et al. Characterization of the aerosol chemical composition during the COVID-19 lockdown period in Suzhou in the Yangtze River Delta, China. J Environ Sci (China). 2021 Apr;102:110-122, doi:10.1016/j.jes.2020.09.019.
- Wang B, Chen H, Chan YL, Oliver BG. Is there an association between the level of ambient air pollution and COVID-19? Am J Physiol Lung Cell Mol Physiol. 2020 Sep 1;319(3):L416-L421, doi:10.1152/ajplung.00244.2020. Epub 2020 Jul 22.
- Woodby B, Arnold MM, Valacchi G. SARS-CoV-2 infection, COVID-19 pathogenesis, and exposure to air pollution: What is the connection? Ann N Y Acad Sci. 2021 Feb;1486(1):15-38, doi:.1111/nyas.14512.
- Wu CL, Wang HW, Cai WJ et al., Impact of the COVID-19 lockdown on roadside traffic-related air pollution in Shanghai, China. Build Environ. 2021 May;194:107718, doi:10.1016/j.buildenv.2021.107718.
- Yao Y, Pan J, Wang W et al. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci Total Environ. 2020 Nov 1;741:140396, doi:10.1016/j.scitotenv.2020.140396.
- Zhang X, Tang M, Guo F et al., Associations between air pollution and COVID-19 epidemic during quarantine period in China. Environ Pollut. 2021 Jan 1;268(Pt A):115897, doi:0.1016/j.envpol.2020.115897.
- Zheng P, Chen Z, Liu Y et al., Association between coronavirus disease 2019 (COVID-19) and long-term exposure to air pollution: Evidence from the first epidemic wave in China. Environ Pollut. 2021 Feb 8;276:116682, doi:10.1016/j.envpol.2021.116682.
- Zhu J, Chen L, Liao H et al., Enhanced PM2.5 Decreases and O3 Increases in China During COVID-19 Lockdown by Aerosol-Radiation Feedback. Geophys Res Lett. 2021 Jan 28;48(2):e2020GL090260.doi:10.1029/2020GL090260.
- Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ. 2020 Jul 20;727:138704, doi:10.1016/j.scitotenv.2020.138704.
- Zoran MA, Savastru RS, Savastru DM, Tautan MN. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci Total Environ. 2020 Oct 10;738:139825, doi:10.1016/j.scitotenv.2020.139825.
References
- DiRenna, J. COVID-19: A Different Kind of Warfare. Mo Med. 2020, 117, 170. [Google Scholar]
- Murray, C.J.; Lipfert, F.W. Inferring frail life expectancies in Chicago from daily fluctuations in elderly mortality. Inhal. Toxicol. 2013, 25, 461–479. [Google Scholar] [CrossRef]
- Adhikari, A.; Yin, J. Short-Term Effects of Ambient Ozone, PM2.5 and Meteorological Factors on COVID-19 Confirmed Cases and Deaths in Queens, New York. Int. J. Environ. Res. Public Health 2020, 17, 4047. [Google Scholar] [CrossRef]
- Hoang, T.; Nguyen, T.Q.; Tran, T.T.A. Short-term exposure to ambient air pollution in association with COVID-19 of two clusters in South Korea. Trop. Med. Int. Health 2020, 15. [Google Scholar] [CrossRef]
- Jiang, Y.; Wu, X.J.; Guan, Y.J. Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infect. Control Hosp. Epidemiol. 2020, 41, 1011–1015. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xu, X.L.; Dai, D.W.; Huang, Z.Y.; Ma, Z.; Guan, Y.J. Air pollution and temperature are associated with increased COVID-19 incidence: A time series study. Int. J. Infect. Dis. 2020, 97, 278–282. [Google Scholar] [CrossRef]
- Zhu, Y.; Xie, J.; Huang, F.; Cao, L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci. Total Environ. 2020, 727, 138704. [Google Scholar] [CrossRef] [PubMed]
- Bashir, M.F.; Ma, B.J.; Bilal Komal, B.; Bashir, M.A.; Farooq, T.H.; Iqbal, N.; Bashir, M. Correlation between environmental pollution indicators and COVID-19 pandemic: Abrief study in Californian context. Environ. Res. 2020, 187, 109652. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, E.; Renzetti, S.; Volta, M.; Donato, F.; Calza, S.; Placidi, D.; Lucchini, R.G.; Rota, M. COVID-19 incidence and mortality in Lombardy, Italy: An ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ. Res. 2021, 195, 110777. [Google Scholar] [CrossRef]
- Elliott, J.; Bodinier, B.; Whitaker, M.; Delpierre, C.; Vermeulen, R.; Tzoulaki, I.; Elliott, P.; Chadeau-Hyam, M. COVID-19 mortality in the UK Biobank cohort:revisiting and evaluating risk factors. Eur. J. Epidemiol. 2021, 36, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Liang, D.; Shi, L.; Zhao, J.; Liu, P.; Sarnat, J.A.; Gao, S.; Schwartz, J.; Liu, Y.; Ebelt, S.T.; Scovronick, N.; et al. Urban Air Pollution May Enhance COVID-19 Case-Fatality and Mortality Rates in the United States. Innovation 2020, 1, 100047. [Google Scholar] [CrossRef] [PubMed]
- Magazzino, C.; Mele, M.; Sarkodie, S.A. The nexus between COVID-19 deaths, air pollution and economic growth in New York state: Evidence from Deep Machine Learning. J. Environ. Manag. 2021, 286, 112241. [Google Scholar] [CrossRef] [PubMed]
- Magazzino, C.; Mele, M.; Schneider, N. The relationship between air pollution and COVID-19-related deaths: An application to three French cities. Appl. Energy 2020, 279, 115835. [Google Scholar] [CrossRef] [PubMed]
- Mendy, A.; Wu, X.; Keller, J.L.; Fassler, C.S.; Apewokin, S.; Mersha, T.B.; Xie, C.; Pinney, S.M. Long-term exposure to fine particulate matter and hospitalization in COVID-19 patients. Respir. Med. 2021, 178, 106313. [Google Scholar] [CrossRef] [PubMed]
- Neelon, B.; Mutiso, F.; Mueller, N.T.; Pearce, J.L.; Benjamin-Neelon, S.E. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. medRxiv 2020. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef]
- Bekbulat, B.; Apte, J.S.; Millet, D.B.; Robinson, A.L.; Wells, K.C.; Presto, A.A.; Marshall, J.D. Changes in criteria air pollution levels in the US before, during, and after Covid-19 stay-at-home orders: Evidence from regulatory monitors. Sci. Total Environ. 2021, 769, 144693. [Google Scholar] [CrossRef]
- Chauhan, A.; Singh, R.P. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ. Res. 2020, 187, 109634. [Google Scholar] [CrossRef]
- Hudda, N.; Simon, M.C.; Patton, A.P.; Durant, J.L. Reductions in traffic-related black carbon and ultrafine particle number concentrations in an urban neighborhood during the COVID-19 pandemic. Sci. Total Environ. 2020, 742, 140931. [Google Scholar] [CrossRef]
- Chen, L.A.; Chien, L.C.; Li, Y.; Lin, G. Nonuniform impacts of COVID-19 lockdown on air quality over the United States. Sci. Total Environ. 2020, 745, 141105. [Google Scholar] [CrossRef]
- Jephcote, C.; Hansell, A.L.; Adams, K.; Gulliver, J. Changes in air quality during COVID-19 ’lockdown’ in the United Kingdom. Environ. Pollut. 2021, 272, 116011. [Google Scholar] [CrossRef]
- Xiang, J.; Austin, E.; Gould, T.; Larson, T.; Shirai, J.; Liu, Y.; Marshall, J.; Seto, E. Impacts of the COVID-19 responses on traffic-related air pollution in a Northwestern US city. Sci. Total Environ. 2020, 747, 141325. [Google Scholar] [CrossRef]
- Lipfert, F.W. An assessment of air pollution exposure information for health studies. Atmosphere 2015, 6, 1736–1752. [Google Scholar] [CrossRef]
- Domínguez-Amarillo, S.; Fernández-Agüera, J.; Cesteros-García, S.; González-Lezcano, R.A. Bad Air Can Also Kill: Residential Indoor Air Quality and Pollutant Exposure Risk during the COVID-19 Crisis. Int. J. Environ. Res. Public Health 2020, 17, 7183. [Google Scholar] [CrossRef]
- Chirizzi, D.; Conte, M.; Feltracco, M.; Dinoi, A.; Gregoris, E.; Barbaro, E.; La Bella, G.; Ciccarese, G.; La Salandra, G.; Gambaro, A.; et al. SARS-CoV-2 concentrations and virus-laden aerosol size distributions in outdoor air in north and south of Italy. Environ. Int. 2021, 146, 106255. [Google Scholar] [CrossRef]
- Faridi, S.; Niazi, S.; Sadeghi, K. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 2020, 725, 138401. [Google Scholar] [CrossRef] [PubMed]
- Lipfert, F.W.; Wyzga, R.E.; Baty, J.D.; Miller, J.P. Air pollution and survival within the Washington University-EPRI Veterans Cohort: Risks based on modeled estimates of ambient levels of hazardous and criteria air pollutants. J. Air Waste Manag. Assoc. 2009, 59, 473–489. [Google Scholar] [CrossRef] [PubMed]
- Lipfert, F.W.; Baty, J.D.; Miller, J.P.; Wyzga, R.E. PM2.5 constituents and related air quality variables as predictors of survival in a cohort of U.S. military veterans. Inhal. Toxicol. 2006, 18, 645–657. [Google Scholar] [CrossRef] [PubMed]

| 1st Author | Location | Time Period | Lag | PM2.5 | O3 | NO2 | SO2 | CO | PM10 |
|---|---|---|---|---|---|---|---|---|---|
| Adhikari [3] | Queens, NY | March, April 2020 | 21 d | − | + | ||||
| Hoang [4] | South Korea (1) | February, September 2020 | 7 d | + | − | + | + | + | + |
| (2) | + | + | + | + | + | + | |||
| Jiang [5] | China (1) | February 2020 | 0 | + | − | + | + | + | − |
| (2) | + | − | + | + | + | − | |||
| (3) | + | + | + | + | − | − | |||
| Li [6] | China (1) | February 2020 | 4 d | + | + | + | + | ||
| (2) | + | + | − | + | |||||
| Zhu [7] | 120 Chinese cities | February 2020 | 21 d | + | + | + | − | + | + |
| 1st Author | Location | Time Period | Outcome | PM2.5 | O3 | NO2 | SO2 | CO | PM10 |
|---|---|---|---|---|---|---|---|---|---|
| Bashir [8] | California | March, April 2020 | cases | − | − | + | − | ||
| deaths | − | − | + | − | |||||
| De Angelis [9] | Italy | February–April 2020 | cases | + | − | + | |||
| death | + | − | + | ||||||
| Elliott [10] | UK | February, September 2020 | death | + | + | + | |||
| Liang [11] | US countries | February–July 2020 | death | + | − | + | |||
| case-fat rate | + | − | + | ||||||
| Magazzino [12] | NY state | March–June 2020 | death | + | + | ||||
| Magazzino [13] | France (1) | March–April 2020 | death | + | + | ||||
| (2) | death | + | + | ||||||
| (3) | death | + | + | ||||||
| Mendy [14] | Cincinnati, OH | March–July 2020 | hospitalization | + (only with prior asthma or COPD) | |||||
| Neelon [15] | US counties | March–August 2020 | death | + | |||||
| Wu [16] | US counties | February–April 2020 | death | + |
| Mean (Median) | Case Corr | Death Corr | Case Δ%/Unit | Death Δ%/Per Unit | |
|---|---|---|---|---|---|
| Cases per million | (87,601) | ||||
| Deaths per million | (1458) | ||||
| Case-fatality rate | 0.0173 | ||||
| Population density (sq mi) * | (524) | −0.08 | 0.22 | ||
| Persons per household * | 2.58 | 0.51 | 0.08 | 16 | |
| % Black residents * | 11.5 | 0.05 | 0.35 | 1.4 | |
| % Hispanic residents * | 11.2 | 0.13 | 0.19 | ||
| Household income * | $52,400 | −0.20 | −0.05 | ||
| Education level index * | 51 | −0.38 | −0.33 | −4.9 | −5.1 |
| % Republican voters ** | 50 | 0.51 | 0.12 | 1.4 | |
| Face mask usage score *** | 298 | −0.30 | 0.12 | −4.9 | |
| Distance from NYC **** | 688 | 0.14 | −0.26 | ||
| PM2.5 (2003) µg/m3 ***** | 11.8 | 0.07 | 0.34 | 5.2 | |
| PM2.5 (2016) µg/m3 ***** | 8.2 | 0.14 | 0.26 | ||
| NOx (2002), ppb [27] | 7.1 | −0.08 | 0.32 | 2.1 | |
| EC (2002) µg/m3 [27] | 0.29 | 0.11 | 0.30 | 4.5 |
| Pollutant | COVID-19 Mortality * | All-Cause Mortality # |
|---|---|---|
| EC | 1.07 (0.94–1.23) | 1.07 (1.05–1.10) |
| NOx | 1.10 (0.95–1.26) | 1.08 (1.06–1.09) |
| PM2.5 | 1.48 (0.84–2.62) | 1.09 (0.90–1.33) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lipfert, F.W.; Wyzga, R.E. COVID-19 and the Environment, Review and Analysis. Environments 2021, 8, 42. https://doi.org/10.3390/environments8050042
Lipfert FW, Wyzga RE. COVID-19 and the Environment, Review and Analysis. Environments. 2021; 8(5):42. https://doi.org/10.3390/environments8050042
Chicago/Turabian StyleLipfert, Frederick W., and Ronald E. Wyzga. 2021. "COVID-19 and the Environment, Review and Analysis" Environments 8, no. 5: 42. https://doi.org/10.3390/environments8050042
APA StyleLipfert, F. W., & Wyzga, R. E. (2021). COVID-19 and the Environment, Review and Analysis. Environments, 8(5), 42. https://doi.org/10.3390/environments8050042





