Suicidal Ideation in Bereavement: A Systematic Review
Abstract
1. Introduction
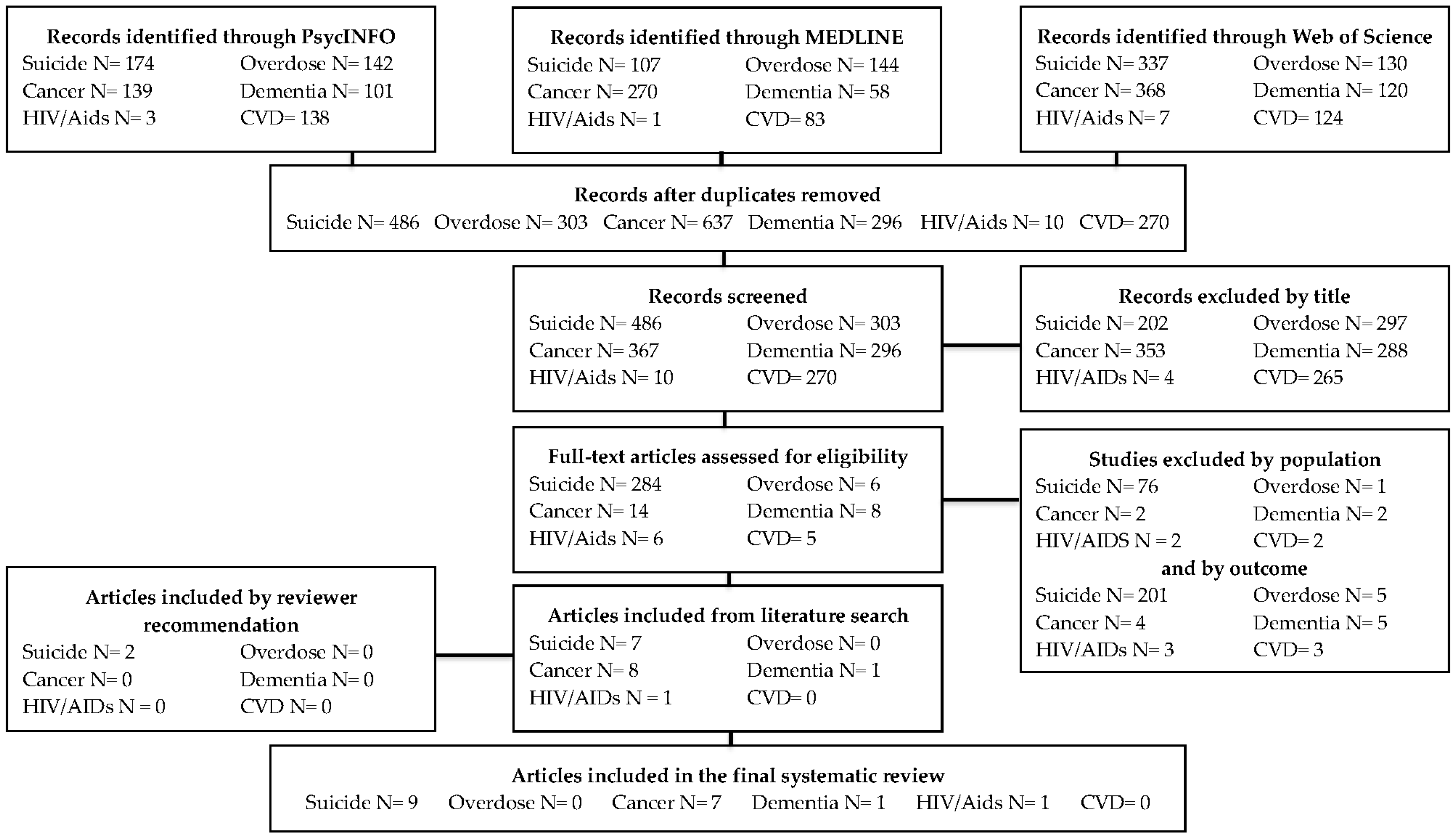
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
3. Results
3.1. Suicide-Bereaved
3.2. Accidental Drug Overdose-Bereaved
3.3. Cancer-Bereaved
3.4. Dementia-Bereaved
3.5. Human Immunodeficiency Virus Infection and Acquired Immune Deficiency Syndrome (HIV/AIDS)-Bereaved
3.6. Cardiovascular Disease-Bereaved (CVD)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Trevino, K.M.; Maciejewski, P.K.; Fasciano, K.; Greer, J.; Partridge, A.; Kacel, E.L.; Block, S.; Prigerson, H.G. Coping and psychological distress in young adults with advanced cancer. J. Support. Oncol. 2012, 10, 124–130. [Google Scholar] [CrossRef]
- Carey, I.M.; Shah, S.M.; DeWilde, S.; Harris, T.; Victor, C.R.; Cook, D.G. Increased Risk of Acute Cardiovascular Events after Partner Bereavement: A Matched Cohort Study. JAMA Intern. Med. 2014, 174, 598–605. [Google Scholar] [CrossRef]
- Stroebe, M.; Schut, H.; Stroebe, W. Health outcomes of bereavement. Lancet 2007, 8, 1960–1973. [Google Scholar] [CrossRef]
- Shear, M.K.; Skritskaya, N.A. Bereavement and anxiety. Curr. Psychiatry Rep. 2012, 14, 169–175. [Google Scholar] [CrossRef]
- Cole, M.G.; Dendukuri, N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. Am. J. Psychiatry 2003, 160, 1147–1156. [Google Scholar] [CrossRef]
- Prigerson, H.G.; Horowitz, M.J.; Jacobs, S.C.; Parkes, C.M.; Aslan, M.; Goodkin, K.; Raphael, B.; Marwit, S.J.; Wortman, C.; Neimeyer, R.A.; et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 2009, 6. [Google Scholar] [CrossRef] [PubMed]
- Stroebe, M.; Stroebe, W.; Abakoumkin, G. The broken heart: Suicidal ideation in bereavement. Am. J. Psychiatry 2005, 162, 2178–2180. [Google Scholar] [CrossRef] [PubMed]
- Guldin, M.B.; Ina Siegismund Kjaersgaard, M.; Fenger-Grøn, M.; Thorlund Partner, E.; Li, J.; Prior, A.; Vestergaard, M. Risk of suicide, deliberate self-harm and psychiatric illness after the loss of a close relative: A nationwide cohort study. World Psychiatry 2017, 16, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.A.; Keating, N.L.; Balboni, T.A.; Matulonis, U.A.; Block, S.D.; Prigerson, H.G. Place of Death: Correlations with Quality of Life of Patients with Cancer and Predictors of Bereaved Caregivers’ Mental Health. J. Clin. Oncol. 2010, 28, 4457–4464. [Google Scholar] [CrossRef]
- Wright, A.A.; Zhang, B.; Ray, A.; Mack, J.W.; Trice, E.; Balboni, T.; Mitchell, S.L.; Jackson, V.A.; Block, S.D.; Maciejewski, P.K.; et al. Associations Between End-of-Life Discussions, Patient Mental Health, Medical Care Near Death, and Caregiver Bereavement Adjustment. JAMA 2008, 300, 1665–1673. [Google Scholar] [CrossRef] [PubMed]
- Abbott, C.H.; Prigerson, H.G.; Maciejewski, P.K. The influence of patients’ quality of life at the end of life on bereaved caregivers’ suicidal ideation. J. Pain Symptom Manag. 2014, 48, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Pitman, A.; Rantell, K.; Marston, L.; King, M.; Osborn, D. Perceived Stigma of Sudden Bereavement as a Risk Factor for Suicidal Thoughts and Suicide Attempt: Analysis of British Cross-Sectional Survey Data on 3387 Young Bereaved Adults. Int. J. Environ. Res. Public Health 2017, 14, 286. [Google Scholar] [CrossRef]
- Feigelman, W.; Gorman, B.S.; Jordan, J.R. Stigmatization and Suicide Bereavement. Death Stud. 2009, 33, 591–608. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.Q.; Murphy, S.L.; Kochanek, K.D.; Bastian, B.; Arias, E. Deaths: Final Data for 2016; National Vital Statistics Reports; National Center for Health Statistics: Hyattsville, MD, USA, 2018; p. 67.
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Pitman, A.L.; Osborn, D.P.J.; Rantell, K.; King, M.B. Bereavement by suicide as a risk factor for suicide attempt: A cross-sectional national UK-wide study of 3432 young bereaved adults. BMJ Open 2016, 6, e009948. [Google Scholar] [CrossRef] [PubMed]
- Cerel, J.; Roberts, T.A. Suicidal behavior in the family and adolescent risk behavior. J. Adolesc. Health 2005, 36, 352.e8–352.e14. [Google Scholar] [CrossRef]
- Mitchell, A.M.; Kim, Y.; Prigerson, H.G.; Mortimer, M.K. Complicated Grief and Suicidal Ideation in Adult Survivors of Suicide. Suicide Life Threat. Behav. 2005, 35, 498–506. [Google Scholar] [CrossRef] [PubMed]
- De Groot, M.; Neeleman, J.; van der Meer, K.; Burger, H. The Effectiveness of Family-Based Cognitive-Behavior Grief Therapy to Prevent Complicated Grief in Relatives of Suicide Victims: The Mediating Role of Suicide Ideation. Suicide Life Threat. Behav. 2010, 40, 425–437. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.L.; Eddinger, J.R.; Rynearson, E.K.; Rheingold, A.A. Prevalence and Correlates of Suicidal Ideation in a Treatment-Seeking Sample of Violent Loss Survivors. Crisis 2018, 39, 377–385. [Google Scholar] [CrossRef]
- Kõlves, K.; Zhao, Q.; Ross, V.; Hawgood, J.; Spence, S.H.; de Leo, D. Suicide and other sudden death bereavement of immediate family members: An analysis of grief reactions six-months after death. J. Affect. Disord. 2019, 243, 96–102. [Google Scholar] [CrossRef]
- Song, I.H.; Kwon, S.W.; Kim, J.E. Association Between Suicidal Ideation and Exposure to Suicide in Social Relationships Among Family, Friend, and Acquaintance Survivors in South Korea. Suicide Life Threat. Behav. 2015, 45, 376–390. [Google Scholar] [CrossRef]
- Santos, S.; Campos, R.C.; Tavares, S. Suicidal ideation and distress in family members bereaved by suicide in Portugal. Death Stud. 2015, 39, 332–341. [Google Scholar] [CrossRef]
- Reynolds, W.M. Suicidal Ideation Questionnaire (SIQ); Psychological Assessment Resources: Odessa, FL, USA, 1987. [Google Scholar]
- De Groot, M.; Kollen, B.J. Course of bereavement over 8-10 years in first degree relatives and spouses of people who committed suicide: Longitudinal community based cohort study. Br. Med. J. 2013, 347, f5519. [Google Scholar] [CrossRef]
- Templeton, L.; Valentine, C.; McKell, J.; Ford, A.; Velleman, R.; Walter, T.; Hay, G.; Bauld, L.; Hollywood, J. Bereavement following a fatal overdose: The experiences of adults in England and Scotland. Drugs Educ. Prev. Policy 2017, 24, 58–66. [Google Scholar] [CrossRef]
- Abbott, C.H.; Prigerson, H.G.; Maciejewski, P.K. Caregivers’ perception of advanced cancer patients’ quality of death: Impact on caregiver suicidal ideation in bereavement. J. Clin. Oncol. 2013, 31 (Suppl. 15), 9522. [Google Scholar]
- Song, J.I.; Shin, D.W.; Choi, J.; Kang, J.; Baek, Y.; Mo, H.; Seo, M.; Hwang, Y.H.; Lim, Y.; Lee, O.K. Quality of life and mental health in the bereaved family members of patients with terminal cancer. Psycho-Oncology 2012, 21, 1158–1166. [Google Scholar] [CrossRef]
- Peteet, J.R.; Maytal, G.; Rokni, H. Unimaginable loss: Contingent suicidal ideation in family members of oncology patients. Psychosomatics 2010, 51, 166–170. [Google Scholar] [CrossRef]
- Barrett, T.W.; Scott, T.B. Development of the grief experience questionnaire. Suicide Life Threat. Behav. 1989, 19, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Houck, J.A. A Comparison of Grief Reactions in Cancer, HIV/AIDS, and Suicide Bereavement. J. HIV/Aids Soc. Serv. 2007, 6, 97–112. [Google Scholar] [CrossRef]
- Pfeffer, C.R.; Karus, D.; Siegel, K.; Jiang, H. Child survivors of parental death from cancer or suicide: Depressive and behavioral outcomes. Psycho-Oncology 2000, 9, 1–10. [Google Scholar] [CrossRef]
- O’Dwyer, S.T.; Moyle, W.; Zimmer-Gembeck, M.; De Leo, D. Suicidal ideation in family carers of people with dementia. Aging Ment. Health 2016, 20, 222–230. [Google Scholar] [CrossRef]
- Rosengard, C.; Folkman, S. Suicidal ideation, bereavement, HIV serostatus and psychosocial variables in partners of men with AIDS. AIDS Care 1997, 9, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Co-operation and Development (OECD). Health Data: Suicide Rates 2016. Available online: http://www.webcitation.org/76nVOTKwC (accessed on 11 March 2018).
- Song, J.I.; Shin, D.W.; Choi, J.Y.; Kang, J.; Baik, J.Y.; Mo, H.; Park, M.H.; Choi, S.E.; Kwak, J.H.; Kim, E.J. Quality of life and mental health in family caregivers of patients with terminal cancer. Support. Care Cancer 2011, 19, 1519. [Google Scholar] [CrossRef] [PubMed]
- Bailley, S.E.; Kral, M.J.; Dunham, K. Survivors of suicide do grieve differently: Empirical support for a common sense proposition. Suicide Life Threat. Behav. 1999, 29, 256. [Google Scholar]
- Cvinar, J.G. Do Suicide Survivors Suffer Social Stigma: A Review of the Literature. Perspect. Psychiatr. Care 2005, 41, 14–21. [Google Scholar] [CrossRef]
- Jordan, J.R. Is Suicide Bereavement Different? A Reassessment of the Literature. Suicide Life Threat. Behav. 2001, 31, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, L.; Corrigan, P.W.; Al-Khouja, M.A.; Lewy, S.A.; Major, D.R.; Mead, J.; Redmon, M.; Rubey, C.T.; Weber, S. Behind Closed Doors: The Stigma of Suicide Loss Survivors. Omega 2018, 77, 330–349. [Google Scholar] [CrossRef]
- Reed, M.D.; Greenwald, J.Y. Survivor-victim status, attachment, and sudden death bereavement. Suicide Life Threat. Behav. 1991, 21, 385–401. [Google Scholar]
- Pitman, A.L.; Osborn, D.P.J.; Rantell, K.; King, M.B. The stigma perceived by people bereaved by suicide and other sudden deaths: A cross-sectional UK study of 3432 bereaved adults. J. Psychosom. Res. 2016, 87, 22–29. [Google Scholar] [CrossRef]
- Wilcox, H.C.; Kuramoto, S.J.; Lichtenstein, P.; Langstrom, N.; Brent, D.A.; Runeson, B. Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 514–523. [Google Scholar]
- Burrell, L.V.; Mehlum, L.; Qin, P. Risk factors for suicide in offspring bereaved by sudden parental death from external causes. J. Affect. Disord. 2017, 222, 71–78. [Google Scholar] [CrossRef]
- Rostila, M.; Saarela, J.; Kawachi, I. Suicide following the death of a sibling: A nationwide follow-up study from Sweden. BMJ Open 2013, 3, 002618. [Google Scholar] [CrossRef]
- Joiner, T.E. Why People Die by Suicide; Harvard University Press: Cambridge, MA, USA, 2005. [Google Scholar]
- Garssen, J.; Deerenberg, I.; Mackenbach, J.P.; Kerkhof, A.; Kunst, A.E. Familial risk of early suicide: Variations by age and sex of children and parents. Suicide Life Threat. Behav. 2011, 41, 585–593. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. J. Soc. Work Educ. 2008, 44, 105–113. [Google Scholar] [CrossRef]
- Stone, R.; Cafferata, G.L.; Sangl, J. Caregivers of the frail elderly: A national profile. Gerontologist 1987, 27, 616–626. [Google Scholar] [CrossRef] [PubMed]
- Freeman, A.; Mergl, R.; Kohls, E.; Székely, A.; Gusmao, R.; Arensman, E.; Koburger, N.; Hegerl, U.; Rummel-Kluge, C. A cross-national study on gender differences in suicide intent. BMC Psychiatry 2017, 17, 234. [Google Scholar] [CrossRef]
- Jalal, H.; Buchanich, J.M.; Roberts, M.S.; Balmert, L.C.; Zhang, K.; Burke, D.S. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science 2018, 361, eaau1184. [Google Scholar] [CrossRef]
| Cause of Death | Search Terms |
|---|---|
| Suicide | (suicide bereavement OR bereaved by suicide) AND (family OR carers OR caregivers) AND (suicide risk OR suicidal ideation OR suicide) |
| Accidental overdose | (accidental overdose bereavement OR bereaved by accidental overdose OR accidental overdose OR substance misuse death bereavement OR bereaved by substance misuse death OR substance misuse death OR overdose bereavement OR bereaved by overdose OR overdose) AND (family OR carers OR caregivers) AND (suicide risk OR suicidal ideation OR suicide) |
| Cancer | (cancer bereavement OR bereaved by cancer OR cancer) AND (family OR carers OR caregivers) AND (suicide risk OR suicidal ideation OR suicide) |
| Dementia | (dementia bereavement OR bereaved by dementia OR dementia) AND (family OR carers OR caregivers) AND (suicide risk OR suicidal ideation OR suicide) |
| HIV/AIDs | (HIV bereavement OR AIDS bereavement OR bereaved by AIDS OR bereaved by HIV) AND (family OR carers OR caregivers) AND (suicide risk OR suicidal ideation OR suicide) |
| Cardiovascular Disease | (cardiovascular disease bereavement OR bereaved by cardiovascular disease OR cardiovascular disease OR stroke bereavement OR bereaved by stroke OR stroke OR heart disease bereavement OR bereaved by heart disease OR heart disease) AND (family OR carers OR caregivers) AND (suicide risk OR suicidal ideation OR suicide) |
| Cause of Death | % of Sample Endorsing SI | Time Since Death | Measured by | Population | Citation |
|---|---|---|---|---|---|
| Suicide | 16% | 1 month | Beck Depression Inventory (BDI); item 9 | N = 60; First-degree relatives and spouses part of a crisis intervention study | Mitchell et al., 2005 [18] |
| 22% | <8 weeks | BDI; item 9 | N = 122; First-degree relatives and spouses | de Groot et al., 2010 [19] | |
| 43% | 44.4 months (mean) | BDI; item 9 | N= 28; Family members seeking mental health services | Williams et al., 2018 [20] | |
| 14.1% a | 6 months | Beck Scale for Suicide Ideation (BSS) | N = 142; Adults, family, and friends of deceased | Kõlves et al., 2019 [21] | |
| 26% | 2.5 months | Paykel suicide items (PSI) b | N = 153; First-degree relatives and spouses | de Groot et al., 2013 [25] | |
| 9% | 8–10 years | Paykel suicide items (PSI) b | N = 68; First-degree relatives and spouses | de Groot et al., 2013 [25] | |
| 26.7% | Not reported | Endorsement of “Have you ever seriously contemplated suicide in the past one year?” c | N = 30; family members | Song et al., 2005 [22] | |
| 42% | Less than 3 years (n = 20; 21.5%) More than 3 years (n = 73; 78.5%) | Suicidal Ideation Questionnaire (SIQ) | N = 93; family members | Santos et al., 2015 [23] | |
| 49% | 5.1 years | Endorsement of “Have you ever thought of taking your life, even though you would not actually do it?” d | N = 614; 48% of sample was blood-related to deceased | Pitman, et al., 2016 [16] | |
| 27.3% | <12 months | Endorsement of “During the past 12 months did you ever seriously think about committing suicide?” | N = 68; family members | Cerel et al., 2005 [17] | |
| Accidental overdose | No results found | ||||
| Cancer | 16.5% | 6.5 months (median) | Yale Evaluation of Suicidality (YES) | N = 127; Adult informal caregivers from recruited from major metropolitan hospitals | Abbott et al., 2014 [11] |
| 31.4% | 2–6 months | Endorsement of “Have you had suicidal thoughts at any time during the previous year?” | N = 501; Family members of deceased patients from registered from the Korean Terminal Cancer Patient Information System | Song et al., 2012 [28] | |
| Dementia | 13.7% | <2 years | Suicidal Behaviors Questionnaire—Revised (SBQ—R); item 2 e | N = 566; Adult informal caregivers from the mainly from Australia, Canada, and the US | O’Dwyer et al., 2015 [33] |
| HIV/AIDs | Not reported f | Rosengard et al., 1997 [34] | |||
| Cardiovascular Disease | No results found |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Molina, N.; Viola, M.; Rogers, M.; Ouyang, D.; Gang, J.; Derry, H.; Prigerson, H.G. Suicidal Ideation in Bereavement: A Systematic Review. Behav. Sci. 2019, 9, 53. https://doi.org/10.3390/bs9050053
Molina N, Viola M, Rogers M, Ouyang D, Gang J, Derry H, Prigerson HG. Suicidal Ideation in Bereavement: A Systematic Review. Behavioral Sciences. 2019; 9(5):53. https://doi.org/10.3390/bs9050053
Chicago/Turabian StyleMolina, Nicolette, Martin Viola, Madeline Rogers, Daniel Ouyang, James Gang, Heather Derry, and Holly G. Prigerson. 2019. "Suicidal Ideation in Bereavement: A Systematic Review" Behavioral Sciences 9, no. 5: 53. https://doi.org/10.3390/bs9050053
APA StyleMolina, N., Viola, M., Rogers, M., Ouyang, D., Gang, J., Derry, H., & Prigerson, H. G. (2019). Suicidal Ideation in Bereavement: A Systematic Review. Behavioral Sciences, 9(5), 53. https://doi.org/10.3390/bs9050053





