Differential Effects of Hazardous Drinking on Post-Traumatic Stress Disorder Outcomes Across Two Prolonged Exposure Treatment Formats †
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Massed Prolonged Exposure (M-PE)
2.3. Intensive Outpatient Program-Prolonged Exposure (IOP-PE)
3. Measures
3.1. Demographic and Military Characteristics
3.2. PTSD
3.3. Hazardous Drinking
4. Data Analysis Plan
5. Results
5.1. Baseline PTSD and Drinking Severity
| Hazardous Drinking Absent | Hazardous Drinking Present | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| IOP-PE | M-PE | IOP-PE | M-PE | ||||||
| Outcome | Time | M | SE | M | SE | M | SE | M | SE |
| PCL-5 | Baseline | 51.28 | 1.51 | 50.70 | 1.43 | 50.16 | 2.24 | 50.96 | 2.56 |
| 1MFU | 26.22 | 1.95 | 28.85 | 1.71 | 34.70 | 2.63 | 35.96 | 3.13 | |
| 3MFU | 25.41 | 1.97 | 28.41 | 1.79 | 32.37 | 2.86 | 41.74 | 3.39 | |
| 6MFU | 28.88 | 1.96 | 30.95 | 1.92 | 32.86 | 2.80 | 38.70 | 3.43 | |
| CAPS-5 | Baseline | 36.60 | 0.95 | 36.48 | 0.90 | 36.26 | 1.41 | 36.44 | 1.61 |
| 1MFU | 20.95 | 1.28 | 21.65 | 1.12 | 26.58 | 1.72 | 26.10 | 2.06 | |
| 3MFU | 18.72 | 1.32 | 22.37 | 1.16 | 24.23 | 1.84 | 26.30 | 2.15 | |
| 6MFU | 21.81 | 1.33 | 25.42 | 1.31 | 22.63 | 1.88 | 28.20 | 2.34 | |
| Hazardous Drinking Present | |||||
|---|---|---|---|---|---|
| IOP-PE | M-PE | ||||
| QDS | Time | M | SE | M | SE |
| Total Drinks in Past Week | Baseline | 12.69 | 2.13 | 13.09 | 2.42 |
| 1MFU | 7.97 | 2.54 | 10.66 | 3.03 | |
| 3MFU | 4.04 | 2.62 | 12.10 | 3.05 | |
| 6MFU | 6.70 | 2.85 | 8.35 | 3.47 | |
| Past Week Drinking Days | Baseline | 2.83 | 0.38 | 3.24 | 0.43 |
| 1MFU | 2.54 | 0.44 | 2.79 | 0.51 | |
| 3MFU | 1.84 | 0.44 | 2.45 | 0.51 | |
| 6MFU | 2.29 | 0.48 | 1.88 | 0.57 | |
| Past Week Drinks per Drinking Day | Baseline | 4.74 | 0.51 | 4.74 | 0.51 |
| 1MFU | 2.37 | 0.63 | 2.37 | 0.63 | |
| 3MFU | 1.62 | 0.70 | 1.62 | 0.70 | |
| 6MFU | 2.61 | 0.74 | 2.61 | 0.74 | |
| Past Week Heavy Drinking Days | Baseline | 1.48 | 0.37 | 1.29 | 0.42 |
| 1MFU | 1.25 | 0.45 | 0.84 | 0.54 | |
| 3MFU | 0.39 | 0.50 | 1.63 | 0.58 | |
| 6MFU | 1.03 | 0.52 | 0.59 | 0.64 | |
| Past Week Drinks per Heavy Drinking Day | Baseline | 5.90 | 0.65 | 5.73 | 0.74 |
| 1MFU | 3.05 | 0.79 | 3.31 | 0.95 | |
| 3MFU | 1.83 | 0.83 | 3.34 | 0.97 | |
| 6MFU | 3.34 | 0.90 | 2.34 | 1.11 | |
5.2. PTSD Outcomes
| Hazardous Drinking Absent | Hazardous Drinking Present | Haz x Time | Group Differences in Change | |||||||
| PTSD Severity | M | SE | M | SE | F | p | Mdiff | t | p | d |
| PCL-5 | 3.37 | 0.003 | ||||||||
| Baseline to 1MFU | −23.46 | 1.37 | −15.23 | 2.17 | 8.23 | 3.21 | 0.001 | 0.42 | ||
| Baseline to 3MFU | −24.07 | 1.34 | −13.51 | 2.24 | 10.57 | 4.05 | <0.001 | 0.53 | ||
| Baseline to 6MFU | −21.07 | 1.31 | −14.78 | 2.10 | 6.29 | 2.54 | 0.011 | 0.33 | ||
| CAPS-5 | 4.17 | 0.018 | ||||||||
| Baseline to 1MFU | −15.24 | 0.95 | −10.01 | 1.51 | 5.23 | 2.93 | 0.004 | 0.38 | ||
| Baseline to 3MFU | −15.99 | 0.93 | −11.08 | 1.49 | 4.92 | 2.81 | 0.005 | 0.37 | ||
| Baseline to 6MFU | −12.93 | 1.03 | −10.93 | 1.65 | 2.00 | 1.03 | 0.306 | 0.14 | ||
| Hazardous Drinking Absent | Hazardous Drinking Present | Arm x Time | Simple Main Effect of Time | |||||||
| Drinking Patterns | M | SE | M | SE | F | p | t | p | d | |
| Past Week Total Drinks | 1.42 | 0.237 | ||||||||
| Baseline to 1MFU | --- | --- | −3.57 | 2.38 | −1.70 | 0.092 | −0.42 | |||
| Baseline to 3MFU | --- | --- | −4.82 | 1.91 | −2.52 | 0.013 | −0.57 | |||
| Baseline to 6MFU | --- | --- | −5.36 | 2.36 | −2.27 | 0.025 | −0.63 | |||
| Past Week Drinking Days | 0.63 | 0.597 | ||||||||
| Baseline to 1MFU | --- | --- | −0.37 | 0.32 | −1.17 | 0.244 | −0.29 | |||
| Baseline to 3MFU | --- | --- | −0.89 | 0.28 | −3.17 | 0.002 | −0.72 | |||
| Baseline to 6MFU | --- | --- | −0.95 | 0.35 | −2.69 | 0.008 | −0.77 | |||
| Past Week Drinks per Drinking Day | 0.66 | 0.582 | ||||||||
| Baseline to 1MFU | --- | --- | −2.21 | 0.65 | −3.41 | <0.001 | −0.77 | |||
| Baseline to 3MFU | --- | --- | −2.24 | 0.64 | −3.77 | <0.001 | −0.84 | |||
| Baseline to 6MFU | --- | --- | −2.53 | 0.72 | −3.49 | <0.001 | −0.87 | |||
| Past Week Heavy Drinking Days | 1.51 | 0.218 | ||||||||
| Baseline to 1MFU | --- | --- | −0.34 | 0.38 | −0.90 | 0.369 | −0.18 | |||
| Baseline to 3MFU | --- | --- | −0.38 | 0.42 | −0.91 | 0.369 | −0.20 | |||
| Baseline to 6MFU | --- | --- | −0.58 | 0.44 | −1.32 | 0.189 | −0.31 | |||
| Past Week Drinks on Heavy Drinking Days | 0.83 | 0.481 | ||||||||
| Baseline to 1MFU | --- | --- | −2.64 | 0.70 | −3.77 | <0.001 | −0.91 | |||
| Baseline to 3MFU | --- | --- | −3.22 | 0.66 | −4.90 | <0.001 | −1.11 | |||
| Baseline to 6MFU | --- | --- | −2.97 | 0.79 | −3.77 | <0.001 | −1.03 | |||
5.3. Drinking Outcomes
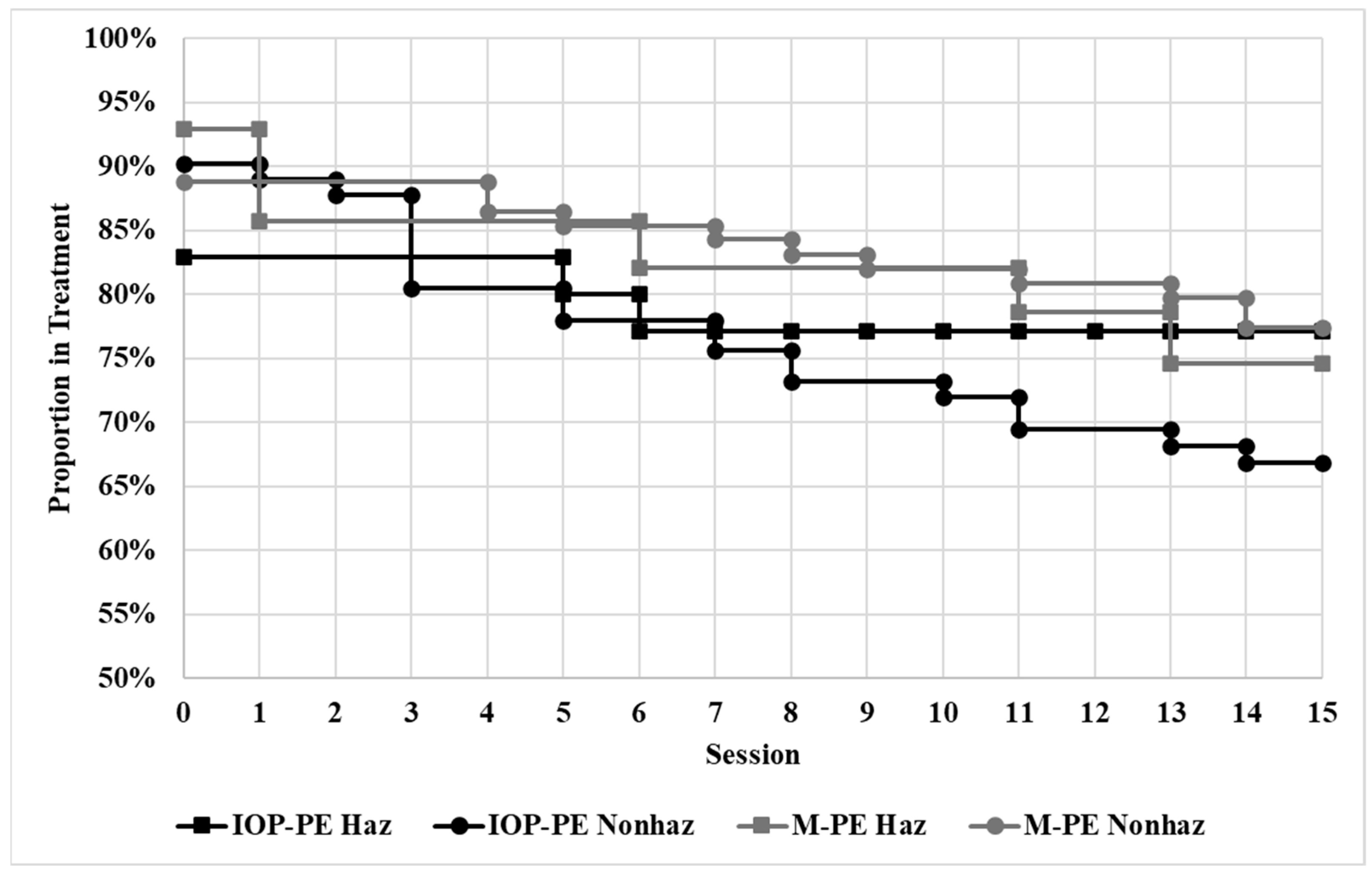
5.4. Treatment Engagement Outcomes
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. [Google Scholar] [CrossRef]
- Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). AUDIT: The Alcohol Use Disorders Identification Test, guidelines for use in primary care (2nd ed.). World Health Organization. [Google Scholar]
- Back, S. E., Brady, K. T., Jaanimägi, U., & Jackson, J. L. (2006). Cocaine dependence and PTSD: A pilot study of symptom interplay and treatment preferences. Addictive Behaviors, 31(2), 351–354. [Google Scholar] [CrossRef] [PubMed]
- Back, S. E., Foa, E. B., Killeen, T. K., Mills, K. L., Teesson, M., Cotton, B. D., Carroll, K. M., & Brady, K. T. (2014). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE) therapist guide. Oxford University Press. [Google Scholar]
- Back, S. E., Killeen, T., Badour, C. L., Flanagan, J. C., Allan, N. P., Ana, E. S., Lozano, B., Korte, K. J., Foa, E. B., & Brady, K. T. (2019). Concurrent treatment of substance use disorders and PTSD using prolonged exposure: A randomized clinical trial in military veterans. Addictive Behaviors, 90, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Back, S. E., Waldrop, A. E., & Brady, K. T. (2009). Treatment Challenges Associated with Comorbid Substance Use and Posttraumatic Stress Disorder: Clinicians’ Perspectives. American Journal on Addictions, 18(1), 15–20. [Google Scholar] [CrossRef]
- Becker, C. B., Zayfert, C., & Anderson, E. (2004). A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy, 42(3), 277–292. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C., Xu, Y., Brady, K., Pérez-Fuentes, G., Okuda, M., & Wang, S. (2013). Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from national epidemiological survey on alcohol and related conditions. Drug and Alcohol Dependence, 132(3), 630–638. [Google Scholar] [CrossRef]
- Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for the diagnostic and statistical manual of mental disorders—Fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. [Google Scholar] [CrossRef]
- Coffey, S. F., Schumacher, J. A., Nosen, E., Littlefield, A. K., Henslee, A., Lappen, A., & Stasiewicz, P. R. (2016). Trauma-focused exposure therapy for chronic PTSD in alcohol and drug dependent patients: A randomized controlled trial. Psychology of Addictive Behaviors, 30(7), 778–790. [Google Scholar] [CrossRef]
- Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., & Vervliet, B. (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. [Google Scholar] [CrossRef]
- Debell, F., Fear, N. T., Head, M., Batt-Rawden, S., Greenberg, N., Wessely, S., & Goodwin, L. (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1401–1425. [Google Scholar] [CrossRef]
- Dondanville, K. A., Wachen, J. S., Hale, W. J., Mintz, J., Roache, J. D., Carson, C., Litz, B. T., Yarvis, J. S., Young-McCaughan, S., Peterson, A. L., Resick, P. A., & for the STRONG STAR Consortium. (2019). Examination of treatment effects on hazardous drinking among service members with PTSD. Journal of Traumatic Stress, 32(2), 310–316. [Google Scholar] [CrossRef]
- Fleming, M. F., Barry, K. L., & MacDonald, R. (1991). The alcohol use disorders identification test (AUDIT) in a college sample. The International Journal of the Addictions, 26(11), 1173–1185. [Google Scholar] [CrossRef] [PubMed]
- Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2019). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide (2nd ed.). Oxford University Press. [Google Scholar]
- Foa, E. B., & Kozak, M. J. (1985). Treatment of anxiety disorders: Implications for psychopathology. In A. H. Tuma, & J. D. Maser (Eds.), Anxiety and the anxiety disorders (pp. 421–452). Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Foa, E. B., McLean, C. P., Zang, Y., Rosenfield, D., Yadin, E., Yarvis, J. S., Mintz, J., Young-McCaughan, S., Borah, E. V., Dondanville, K. A., Fina, B. A., Hall-Clark, B. N., Lichner, T., Litz, B. T., Roache, J., Wright, E. C., Peterson, A. L., & STRONG STAR Consortium. (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs. 8 weeks vs. present-centered therapy on PTSD symptom severity in military personnel: A randomized clinical trial. JAMA, 319(4), 354–364. [Google Scholar] [CrossRef]
- Foa, E. B., Yusko, D. A., McLean, C. P., Suvak, M. K., Bux, D. A., Jr., Oslin, D., O’Brien, C. P., Imms, P., Riggs, D. S., & Volpicelli, J. (2013). Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: A randomized clinical trial. JAMA, 310(5), 488–495. [Google Scholar] [CrossRef] [PubMed]
- Held, P., Steigerwald, V. L., Smith, D. L., Kaysen, D., Van Horn, R., & Karnik, N. S. (2021). Impact of hazardous alcohol use on intensive PTSD treatment outcomes among veterans. European Journal of Psychotraumatology, 12(1), 1888541. [Google Scholar] [CrossRef] [PubMed]
- Hien, D. A., Morgan-López, A. A., Saavedra, L. M., Ruglass, L. M., Ye, A., López-Castro, T., Fitzpatrick, S., Killeen, T. K., Norman, S. B., Ebrahimi, C. T., & Back, S. E. (2023). Project harmony: A meta-analysis with individual patient data on behavioral and pharmacologic trials for comorbid posttraumatic stress and alcohol or other drug use disorders. American Journal of Psychiatry, 180(2), 155–166. [Google Scholar] [CrossRef]
- Hoge, C. W., Terhakopian, A., Castro, C. A., Messer, S. C., & Engel, C. C. (2007). Association of PTSD with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. The American Journal of Psychiatry, 164(1), 150–153. [Google Scholar] [CrossRef]
- Jakupcak, M., Tull, M. T., McDermott, M. J., Kaysen, D., Hunt, S., & Simpson, T. (2010). PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors, 35(9), 840–843. [Google Scholar] [CrossRef]
- Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. [Google Scholar] [CrossRef]
- Krull, H., Farmer, C. M., Rennane, S., Goldstein, E., Armour, P., & Ruder, T. (2022). Trends in department of defense disability evaluation system ratings and awards for posttraumatic stress disorder and traumatic brain injury, 2002–2017. Rand Health Quarterly, 9(3), 22. [Google Scholar]
- Lord, E. M. (1967). A paradox in the interpretation of group comparisons. Psychological Bulletin, 68, 304–305. [Google Scholar] [CrossRef]
- LoSavio, S. T., Hale, W., Straud, C. L., Wachen, J. S., Mintz, J., Young-McCaughan, S., Vacek, S. N., Yarvis, J. S., Sloan, D. M., McGeary, D. D., Taylor, D. J., Keane, T. M., Peterson, A. L., Resick, P. A., & for the STRONG STAR Consortium and the Consortium to Alleviate PTSD. (2023). Impact of morally injurious traumatic event exposure on cognitive processing therapy outcomes among veterans and active duty service members. Journal of Military, Veteran, and Family Health, 9(2), 40–51. [Google Scholar] [CrossRef]
- Marlatt, G. A., & Witkiewitz, K. (2002). Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment. Addictive Behaviors, 27(6), 867–886. [Google Scholar] [CrossRef] [PubMed]
- McCauley, J. L., Killeen, T., Gros, D. F., Brady, K. T., & Back, S. E. (2012). PTSD and co-occurring SUD: Advances in assessment and treatment. Clinical Psychology: Science and Practice, 19(3), 283–304. [Google Scholar] [CrossRef]
- Najavits, L. M. (2002). Clinicians’ views on treating posttraumatic stress disorder and substance use disorder. Journal of Substance Abuse Treatment, 22(2), 79–85. [Google Scholar] [CrossRef] [PubMed]
- Norman, S. B., Haller, M., Hamblen, J. L., Southwick, S. M., & Pietrzak, R. H. (2018). The burden of co-occurring alcohol use disorder and PTSD in U.S. Military veterans: Comorbidities, functioning, and suicidality. Psychology of Addictive Behaviors, 32(2), 224–229. [Google Scholar] [CrossRef]
- Persson, A., Back, S. E., Killeen, T. K., Brady, K. T., Schwandt, M. L., Heilig, M., & Magnusson, Å. (2017). Concurrent Treatment of PTSD and substance use disorders using prolonged exposure (COPE): A pilot study in alcohol-dependent women. Journal of Addiction Medicine, 11(2), 119–125. [Google Scholar] [CrossRef] [PubMed]
- Peterson, A. L., Blount, T. H., Foa, E. B., Brown, L. A., McLean, C. P., Mintz, J., Schobitz, R. P., DeBeer, B. R., Mignogna, J., Fina, B. A., Evans, W. R., Synett, S., Hall-Clark, B. N., Rentz, T. O., Schrader, C., Yarvis, J. S., Dondanville, K. A., Hansen, H., Jacoby, V. M., … for the Consortium to Alleviate PTSD. (2023). Massed versus intensive outpatient prolonged exposure for combat-related posttraumatic stress disorder: A randomized clinical trial. JAMA Network Open, 6(1), e2249422. [Google Scholar] [CrossRef]
- Peterson, A. L., Foa, E. B., Blount, T. H., McLean, C. P., Shah, D. V., Young-McCaughan, S., Litz, B. T., Schobitz, R. P., Castillo, D. T., Rentz, T. O., Yarvis, J. S., Dondanville, K. A., Fina, B. A., Hall-Clark, B. N., Brown, L. A., DeBeer, B. R., Jacoby, V. M., Hancock, A. K., Williamson, D. E., … for the Consortium to Alleviate PTSD. (2018). Intensive prolonged exposure therapy for combat-related posttraumatic stress disorder: Design and methodology of a randomized clinical trial. Contemporary Clinical Trials, 72, 126–136. [Google Scholar] [CrossRef]
- Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2011). Prevalence and Axis I comorbidity of full and partial PTSD in the United States: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. Journal of Anxiety Disorders, 25(3), 456–465. [Google Scholar] [CrossRef]
- Reid, M. C., Fiellin, D. A., & O’Connor, P. G. (1999). Hazardous and harmful alcohol consumption in primary care. Archives of Internal Medicine, 159(15), 1681–1689. [Google Scholar] [CrossRef]
- Richardson, L. K., Frueh, B. C., & Acierno, R. (2010). Prevalence estimates of combat-related post-traumatic stress disorder: Critical review. The Australian and New Zealand Journal of Psychiatry, 44(1), 4–19. [Google Scholar] [CrossRef] [PubMed]
- Riggs, D. S., Rukstalis, M., Volpicelli, J. R., Kalmanson, D., & Foa, E. B. (2003). Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: Potential pitfalls to PTSD treatment. Addictive Behaviors, 28(9), 1717–1730. [Google Scholar] [CrossRef] [PubMed]
- Roberts, N. P., Roberts, P. A., Jones, N., & Bisson, J. I. (2015). Psychological interventions for PTSD and comorbid SUD: A systematic review and meta-analysis. Clinical Psychology Review, 38, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, I., & Najavits, L. M. (2007). Clinical challenges in the treatment of patients with PTSD and substance abuse. Current Opinion in Psychiatry, 20(6), 614–618. [Google Scholar] [CrossRef]
- Sinclair, M., McRee, B., & Babor, T. F. (1992). Evaluation of the reliability of AUDIT [Unpublished report]. Alcohol Research Center, University of Connecticut.
- Sobell, L. C., Agrawal, S., Sobell, M. B., Leo, G. I., Young, L. J., Cunningham, J. A., & Simco, E. R. (2003). Comparison of a Quick Drinking Screen with the Timeline Followback for individuals with alcohol problems. Journal of Studies on Alcohol, 64(6), 858–861. [Google Scholar] [CrossRef]
- Straud, C. L., Dondanville, K. A., Hale, W. J., Wachen, J. S., Mintz, J., Litz, B. T., Roache, J. D., Yarvis, J. S., Young-McCaughan, S., Peterson, A. L., Resick, P. A., & for the STRONG STAR Consortium. (2021). The impact of hazardous drinking among active duty military with posttraumatic stress disorder: Does cognitive processing therapy format matter? Journal of Traumatic Stress, 34(1), 210–220. [Google Scholar] [CrossRef]
- U.S. Department of Veterans Affairs & U.S. Department of Defense. (2023). VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder (Version 4.0). Available online: https://www.healthquality.va.gov/guidelines/MH/ptsd/ (accessed on 2 July 2025).
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013a). The clinician-administered PTSD scale for DSM-5 (CAPS-5). U.S. Department of Veterans Affairs, National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp (accessed on 2 July 2025).
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013b). The PTSD checklist for DSM-5 (PCL-5). U.S. Department of Veterans Affairs, National Center for PTSD. Available online: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp (accessed on 2 July 2025).
| Hazardous Drinking Absent | Hazardous Drinking Present | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Total (N = 234) | IOP-PE (n = 81) | M-PE (n = 89) | IOP-PE (n = 36) | M-PE (n = 28) | |||||||
| M | SE | M | SE | M | SE | M | SE | M | SE | F | p | |
| Age | 39.20 | 0.84 | 38.99 | 0.85 | 38.99 | 0.84 | 39.86 | 1.10 | 39.18 | 1.732 | 0.11 | 0.954 |
| Months in military | 181.88 | 5.42 | 185.06 | 8.82 | 182.08 | 9.19 | 182.08 | 12.52 | 171.79 | 17.42 | 0.18 | 0.911 |
| N | % | N | % | N | % | N | % | N | % | χ2 | p | |
| Men | 182 | 77.8 | 62 | 76.5 | 68 | 76.4 | 31 | 86.1 | 21 | 75.0 | 1.54 | 0.673 |
| Married | 151 | 64.5 | 56 | 69.1 | 57 | 64.0 | 24 | 66.7 | 14 | 50.0 | 3.50 | 0.320 |
| Ethnicity | 5.99 | 0.741 | ||||||||||
| Caucasian/Non-Hispanic | 102 | 43.6 | 29 | 35.8 | 41 | 46.6 | 16 | 44.4 | 16 | 59.3 | ||
| African American | 61 | 26.1 | 23 | 28.4 | 23 | 26.1 | 10 | 27.8 | 5 | 18.5 | ||
| Hispanic | 58 | 24.7 | 22 | 27.2 | 23 | 26.1 | 8 | 22.2 | 5 | 18.5 | ||
| Other | 7 | 3.0 | 4 | 4.9 | 1 | 1.1 | 1 | 2.8 | 1 | 3.7 | ||
| Education | 4.14 | 0.658 | ||||||||||
| High school or less | 14 | 5.95 | 6 | 7.4 | 5 | 5.6 | 3 | 8.3 | 0 | 0.0 | ||
| Some college/associate degree | 144 | 61.5 | 53 | 65.4 | 53 | 59.6 | 21 | 58.3 | 17 | 60.7 | ||
| College/graduate degree | 76 | 32.5 | 22 | 27.1 | 31 | 34.8 | 12 | 33.3 | 11 | 39.3 | ||
| Active b | 152 | 65.0 | 55 | 67.9 | 56 | 62.9 | 22 | 61.1 | 19 | 67.9 | 1.04 | 0.791 |
| Army | 191 | 81.6 | 69 | 85.1 | 75 | 84.3 | 23 | 63.9 | 24 | 85.7 | 6.98 | 0.072 |
| Enlisted rank | 200 | 85.5 | 70 | 86.4 | 76 | 85.3 | 31 | 86.1 | 23 | 82.1 | 3.52 | 0.741 |
| Military Occupation | 6.36 | 0.384 | ||||||||||
| Combat Arms | 81 | 34.6 | 32 | 39.5 | 23 | 25.8 | 15 | 41.7 | 11 | 39.3 | ||
| Combat Support | 63 | 26.9 | 22 | 27.2 | 25 | 28.1 | 10 | 27.8 | 6 | 21.4 | ||
| Combat Service Support | 89 | 38.0 | 26 | 32.1 | 41 | 46.1 | 11 | 30.6 | 11 | 39.3 | ||
| Number of deployments | 6.36 | 0.384 | ||||||||||
| 1 | 69 | 29.5 | 20 | 24.7 | 29 | 32.6 | 10 | 25.0 | 11 | 39.3 | ||
| 2 | 70 | 29.9 | 27 | 33.3 | 29 | 32.6 | 7 | 19.4 | 7 | 25.0 | ||
| 3 | 48 | 20.5 | 17 | 21.0 | 16 | 18.0 | 9 | 25.0 | 6 | 21.4 | ||
| 4+ | 46 | 19.7 | 17 | 21.0 | 15 | 16.9 | 10 | 27.8 | 4 | 14.3 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Straud, C.L.; Buccellato, K.H.; Foa, E.B.; Brown, L.A.; McLean, C.P.; Blount, T.H.; Schobitz, R.P.; DeBeer, B.B.; Mignogna, J.; Fina, B.A.; et al. Differential Effects of Hazardous Drinking on Post-Traumatic Stress Disorder Outcomes Across Two Prolonged Exposure Treatment Formats. Behav. Sci. 2025, 15, 954. https://doi.org/10.3390/bs15070954
Straud CL, Buccellato KH, Foa EB, Brown LA, McLean CP, Blount TH, Schobitz RP, DeBeer BB, Mignogna J, Fina BA, et al. Differential Effects of Hazardous Drinking on Post-Traumatic Stress Disorder Outcomes Across Two Prolonged Exposure Treatment Formats. Behavioral Sciences. 2025; 15(7):954. https://doi.org/10.3390/bs15070954
Chicago/Turabian StyleStraud, Casey L., Kiara H. Buccellato, Edna B. Foa, Lily A. Brown, Carmen P. McLean, Tabatha H. Blount, Richard P. Schobitz, Bryann B. DeBeer, Joseph Mignogna, Brooke A. Fina, and et al. 2025. "Differential Effects of Hazardous Drinking on Post-Traumatic Stress Disorder Outcomes Across Two Prolonged Exposure Treatment Formats" Behavioral Sciences 15, no. 7: 954. https://doi.org/10.3390/bs15070954
APA StyleStraud, C. L., Buccellato, K. H., Foa, E. B., Brown, L. A., McLean, C. P., Blount, T. H., Schobitz, R. P., DeBeer, B. B., Mignogna, J., Fina, B. A., Hall-Clark, B. N., Schrader, C. C., Yarvis, J. S., Jacoby, V. M., Evans, W. R., Litz, B. T., Meyer, E. C., Niles, B. L., Young-McCaughan, S., ... Peterson, A. L. (2025). Differential Effects of Hazardous Drinking on Post-Traumatic Stress Disorder Outcomes Across Two Prolonged Exposure Treatment Formats. Behavioral Sciences, 15(7), 954. https://doi.org/10.3390/bs15070954






