Knowledge and Education on Physical Activity Health Benefits and Prescription Principles Among Greek Medical Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Questionnaire
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adedokun, C. A., Curles, W. G., DeMaio, E. L., & Asif, I. M. (2021). Analysis of American medical students’ knowledge of physical activity recommendations. PRiMER, 5, 31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brittain, E. L., Han, L., Annis, J., Master, H., Hughes, A., Roden, D. M., Harris, P. A., & Ruderfer, D. M. (2024). Physical activity and incident obesity across the spectrum of genetic risk for obesity. JAMA Netw Open, 7(3), e243821. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K., Buman, M. P., Cardon, G., Carty, C., Chaput, J. P., Chastin, S., Chou, R., Dempsey, P. C., DiPietro, L., Ekelund, U., Firth, J., Friedenreich, C. M., Garcia, L., Gichu, M., Jago, R., Katzmarzyk, P. T., … Willumsen, J. F. (2020). World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicin, 54(24), 1451–1462. [Google Scholar] [CrossRef] [PubMed Central]
- Butsch, W. S., Kushner, R. F., Alford, S., & Smolarz, B. G. (2020). Low priority of obesity education leads to lack of medical students’ preparedness to effectively treat patients with obesity: Results from the U.S. medical school obesity education curriculum benchmark study. BMC Medical Education, 20(1), 23. [Google Scholar] [CrossRef]
- Chatterjee, R., Chapman, T., Brannan, M. G., & Varney, J. (2017). GPs’ knowledge, use, and confidence in national physical activity and health guidelines and tools: A questionnaire-based survey of general practice in England. British Journal of Sports Medicine, 67(663), e668–e675. [Google Scholar] [CrossRef] [PubMed Central]
- Chew, E. J. C., Ho, Y. N., Kee, G. J., & Sirisena, D. (2019). Scoping review and international multi-centre cohort study investigating teaching, knowledge and beliefs regarding physical activity as a health intervention among medical students: A comparison between Singapore and the UK. Singapore Medical Journal, 60(12), 642–651. [Google Scholar] [CrossRef] [PubMed Central]
- Dale, L. P., Vanderloo, L., Moore, S., & Faulkner, G. (2019). Physical activity and depression, anxiety, and self-esteem in children and youth: An umbrella systematic review. Mental Health and Physical Activity, 16, 66–79. [Google Scholar] [CrossRef]
- Deisz, M., Papproth, C., Ambler, E., Glick, M., & Eno, C. (2024). Correlates and barriers of exercise, stress, and wellness in medical students. Medical Science Educator, 34(6), 1433–1444. [Google Scholar] [CrossRef] [PubMed Central]
- Edwards, J. J., Deenmamode, A. H. P., Griffiths, M., Arnold, O., Cooper, N. J., Wiles, J. D., & O’Driscoll, J. M. (2023). Exercise training and resting blood pressure: A large-scale pairwise and network meta-analysis of randomised controlled trials. British Journal of Sports Medicine, 57(20), 1317–1326. [Google Scholar] [CrossRef]
- Ekelund, U., Sanchez-Lastra, M. A., Dalene, K. E., & Tarp, J. (2024). Dose-response associations, physical activity intensity and mortality risk: A narrative review. Journal of Sport and Health Science, 13(1), 24–29. [Google Scholar] [CrossRef] [PubMed Central]
- Fiuza-Luces, C., Garatachea, N., Berger, N. A., & Lucia, A. (2013). Exercise is the real polypill. Physiology, 28(5), 330–358. [Google Scholar] [CrossRef]
- Frates, B., Ortega, H. A., Freeman, K. J., Co, J. P. T., & Bernstein, M. (2024). Lifestyle medicine in medical education: Maximizing impact. Mayo Clinic Proceedings Innovations Quality & Outcomes, 8(5), 451–474. [Google Scholar] [CrossRef] [PubMed Central]
- Fritz, C. O., Morris, P. E., & Richler, J. J. (2012). Effect size estimates: Current use, calculations, and interpretation. Journal of Experimental Psychology: General, 141(1), 2–18. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Gómez, D., Salazar-Martínez, E., Alfonso-Rosa, R. M., Ramos-Munell, J., Del Pozo-Cruz, J., Del Pozo Cruz, B., & Álvarez-Barbosa, F. (2024). Optimal dose and type of physical activity to improve glycemic control in people diagnosed with type 2 diabetes: A systematic review and meta-analysis. Diabetes Care, 47(2), 295–303. [Google Scholar] [CrossRef]
- Garry, J. P., Diamond, J. J., & Whitley, T. W. (2002). Physical activity curricula in medical schools. Academic Medicine, 77(8), 818–820. [Google Scholar] [CrossRef]
- Hacker, K. (2024). The burden of chronic disease. Mayo Clinic Proceedings Innovations Quality & Outcomes, 8(1), 112–119. [Google Scholar] [CrossRef] [PubMed Central]
- Hambrecht, R., Walther, C., Möbius-Winkler, S., Gielen, S., Linke, A., Conradi, K., Erbs, S., Kluge, R., Kendziorra, K., Sabri, O., Sick, P., & Schuler, G. (2004). Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: A randomized trial. Circulation, 109(11), 1371–1378. [Google Scholar] [CrossRef]
- Harris, E. (2023). Public had most trust in advice from physicians, nurses during pandemic. JAMA, 329(13), 1053. [Google Scholar] [CrossRef]
- Kang, H. (2013). The prevention and handling of the missing data. Korean Journal of Anesthesiology, 64(5), 402–406. [Google Scholar] [CrossRef] [PubMed Central]
- Katzmarzyk, P. T., Friedenreich, C., Shiroma, E. J., & Lee, I. M. (2022). Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. British Journal of Sports Medicine, 56(2), 101–106. [Google Scholar] [CrossRef] [PubMed Central]
- Mirzaei, A., Carter, S. R., Patanwala, A. E., & Schneider, C. R. (2022). Missing data in surveys: Key concepts, approaches, and applications. Research in Social and Administrative Pharmacy, 18(2), 2308–2316. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, C., DeMartino, S., Ivers, L., Brown, A., Maccabee, E., Griffith, B., & Pankey, C. L. (2024). Development and implementation of the “Exercise is Medicine” elective at an osteopathic medical school. Medical Science Educator, 35(1), 227–232. [Google Scholar] [CrossRef]
- Mutlu, S., Pasin, Ö., & Konar, N. (2024). The effect of nutrition, physical activity, and sleep pattern on success in medical students. Medical Science Educator, 35(1), 245–256. [Google Scholar] [CrossRef] [PubMed]
- Naci, H., & Ioannidis, J. P. (2015). Comparative effectiveness of exercise and drug interventions on mortality outcomes: Metaepidemiological study. British Journal of Sports Medicine, 49(21), 1414–1422. [Google Scholar] [CrossRef] [PubMed Central]
- Naghavi, M., Abajobir, A. A., Abbafati, C., Abbas, K. M., Abd-Allah, F., Abera, S. F., Aboyans, V., Adetokunboh, O., Afshin, A., Agrawal, A., Ahmadi, A., Ahmed, M. B., Aichour, A. N., Aichour, M. T. E., Aichour, I., Aiyar, S., Alahdab, F., Al-Aly, Z., Alam, K., … Murray, C. J. L. (2017). Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390(10100), 1151–1210. [Google Scholar] [CrossRef]
- Ng, V., & Irwin, J. D. (2013). Prescriptive medicine: The importance of preparing Canadian medical students to counsel patients toward physical activity. Journal of Physical Activity and Health, 10(6), 889–899. [Google Scholar] [CrossRef]
- Paluch, A. E., Boyer, W. R., Franklin, B. A., Laddu, D., Lobelo, F., Lee, D. C., McDermott, M. M., Swift, D. L., Webel, A. R., & Lane, A. (2024). Resistance exercise training in individuals with and without cardiovascular disease: 2023 Update: A scientific statement from the American Heart Association. Circulation, 149(3), e217–e231. [Google Scholar] [CrossRef] [PubMed Central]
- Pardo, A., Mitjans, A., Baranda, L., Salamero, M., McKenna, J., Arteman, A., & Violán, M. (2016). The transition of medical students through residency: Effects on physical activity and other lifestyle-related behaviors. Journal of Physical Activity and Health, 13(5), 488–493. [Google Scholar] [CrossRef]
- Pasarica, M., Daly, K., Yalim, A. C., Kay, D., DeLeon, A., Neely, L. C., Díaz, D. A., & Bailey, M. (2025). Long-term impact of an interprofessional health promotion curriculum in healthcare students. Medical Science Educator, 35, 1529–1536. [Google Scholar] [CrossRef]
- Pearce, M., Garcia, L., Abbas, A., Strain, T., Schuch, F. B., Golubic, R., Kelly, P., Khan, S., Utukuri, M., Laird, Y., Mok, A., Smith, A., Tainio, M., Brage, S., & Woodcock, J. (2022). Association between physical activity and risk of depression: A systematic review and meta-analysis. JAMA Psychiatry, 79(6), 550–559. [Google Scholar] [CrossRef] [PubMed Central]
- Pearson, S. D., & Raeke, L. H. (2000). Patients’ trust in physicians: Many theories, few measures, and little data. Journal of General Internal Medicine, 15(7), 509–513. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pedersen, B. K., & Saltin, B. (2015). Exercise as medicine—evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports, 25(Suppl. S3), 1–72. [Google Scholar] [CrossRef]
- Radenkovic, D., Aswani, R., Ahmad, I., Kreindler, J., & Robinson, R. (2019). Lifestyle medicine and physical activity knowledge of final year UK medical students. BMJ Open Sport & Exercise Medicine, 5(1), e000518. [Google Scholar] [CrossRef] [PubMed Central]
- Sahlqvist, S., Rees, B., Hoffmann, S., McCoombe, S., Santoro, G., & Kremer, P. (2022). Physical activity knowledge, attitudes and behaviours of pre-clinical medical students attending an Australian university. BMC Medical Education, 22(1), 642. [Google Scholar] [CrossRef] [PubMed Central]
- Sandefur, K., & Bansal, S. (2024). Filling the gap: An innovative lifestyle medicine curriculum for medical students. Medical Science Educator, 34(2), 485–489. [Google Scholar] [CrossRef] [PubMed]
- Schofield, G., Croteau, K., & McLean, G. (2005). Trust levels of physical activity information sources: A population study. Health Promotion Journal of Australia, 16(3), 221–224. [Google Scholar] [CrossRef]
- Shailendra, P., Baldock, K. L., Li, L. S. K., Gorzelitz, J., Matthews, C. E., Trabert, B., Bennie, J. A., & Boyle, T. (2024). Weight training and risk of all-cause, cardiovascular disease and cancer mortality among older adults. International Journal of Epidemiology, 53(3), dyae074. [Google Scholar] [CrossRef] [PubMed Central]
- Sousa, J. R., Afreixo, V., Carvalho, J., & Silva, P. (2024). Nutrition and physical activity education in medical school: A narrative review. Nutrients, 16(16), 2809. [Google Scholar] [CrossRef]
- Stoutenberg, M., Lewis, L. K., Jones, R. M., Portacio, F., Vidot, D. C., & Kornfeld, J. (2023). Assessing the current and desired levels of training and applied experiences in chronic disease prevention of students during medical school. BMC Medical Education, 23(1), 54. [Google Scholar] [CrossRef] [PubMed Central]
- Thornton, J. S., Frémont, P., Khan, K., Poirier, P., Fowles, J., Wells, G. D., & Frankovich, R. J. (2016). Physical activity prescription: A critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: A position statement by the Canadian Academy of Sport and Exercise Medicine. British Journal of Sports Medicine, 50(18), 1109–1114. [Google Scholar] [CrossRef]
| Variable | n (%) |
|---|---|
| Sex | |
| Male | 44 (32.6) |
| Female | 91 (67.4) |
| Year of study | |
| 4th year | 49 (36.3) |
| 5th year | 23 (17.0) |
| 6th year | 47 (34.8) |
| Preparing to Graduate | 16 (11.9) |
| Have you been taught the value of PA during medical school courses? | |
| No | 29 (21.5) |
| Yes | 106 (78.5) |
| Course type (n = 105) * | |
| Mandatory | 53 (50.5) |
| Elective | 29 (27.6) |
| Clinical practice | 11 (10.5) |
| Mandatory and Elective | 4 (3.8) |
| All of these | 4 (3.8) |
| Briefly covered in various courses | 4 (3.8) |
| In which year was the course taught? (selected all that apply) (n = 104, 2 missing values) * | |
| 1st year | 24 (22.6) |
| 2nd year | 45 (42.5) |
| 3rd year | 42 (39.6) |
| 4th year | 44 (42.3) |
| 5th year (n = 86) ** | 26 (30.2) |
| 6th year (n = 63) ** | 13 (20.6) |
| Total hours of instruction (n = 106) * | |
| <2 h | 32 (30.2) |
| 2–5 h | 32 (30.2) |
| 5–10 h | 22 (20.8) |
| 11–20 h | 13 (12.3) |
| >20 h | 7 (6.6) |
| Readiness to discuss PA topics with patients (select all that apply) | |
| Benefits of PA | 105 (77.8) |
| Cardiopulmonary exercise testing | 63 (46.7) |
| Exercise and behavior change (e.g., Motivational interviewing) | 52 (38.5) |
| Exercise physiology | 50 (37.0) |
| Exercise prescription (individualized by health condition) | 36 (26.7) |
| Exercise intensity/Safe and beneficial exercise zones | 20 (14.8) |
| None of the above | 14 (10.4) |
| Knowledge of current PA guidelines (WHO/KESY) | 34 (25.2) |
| Knowledge of specific recommendations for adults: | |
| 150–300 min of moderate-intensity aerobic PA per week | 83 (61.5) |
| Muscle strengthening exercises ≥2 times per week | 54 (40) |
| Perceived value of additional education on PA | |
| Very important | 58 (43) |
| Important | 52 (38.5) |
| Moderate | 21 (15.6) |
| A little | 3 (2.2) |
| Not at all | 1 (0.7) |
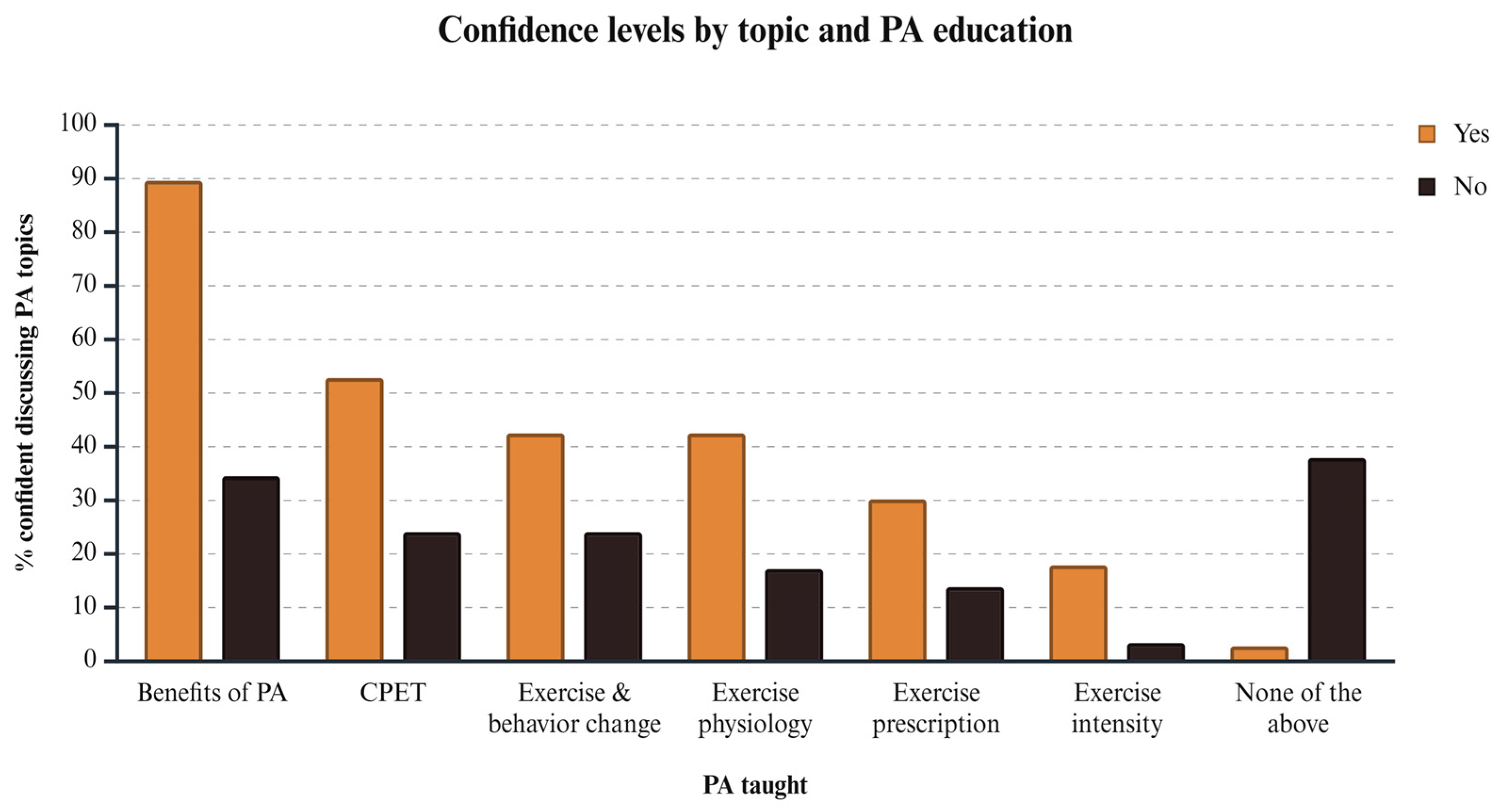
| χ2 | p-Value | φ | OR [95% CI] | Adjusted OR [95% CI], p-Value | |
|---|---|---|---|---|---|
| Benefits of PA | 40.055 | <0.001 | 0.545 | 16.4 [6.1, 44.1] | 17.3 [5.8, 51.7], <0.001 |
| CPET | 7.532 | 0.006 | 0.236 | 3.5 [1.4, 8.9] | 3.3 [1.3, 8.8], 0.014 |
| Exercise physiology | 6.206 | 0.013 | 0.214 | 3.5 [1.3, 10.0] | 4.4 [1.5, 13.1], 0.008 |
| Exercise and behavior change | 3.562 | 0.059 | 0.162 | 2.3 [0.9, 5.9] | 2.5 [0.9, 6.5], 0.072 |
| Exercise prescription | 3.130 | 0.077 | 0.152 | 2.7 [0.9, 8.4] | 2.5 [0.8, 8.0], 0.127 |
| Exercise intensity | 3.781 | 0.052 | 0.167 | 6.1 [0.8, 47.8] | 6.8 [0.8, 54.6], 0.072 |
| Nove of the above | 30.183 | <0.001 | −0.473 | 0.48 [0.12, 0.19] | 0.03 [0.006, 0.2], <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyriakoulakou, E.; Skouras, A.Z.; Tsolakis, C.; Koulouvaris, P.; Philippou, A. Knowledge and Education on Physical Activity Health Benefits and Prescription Principles Among Greek Medical Students. Behav. Sci. 2025, 15, 925. https://doi.org/10.3390/bs15070925
Kyriakoulakou E, Skouras AZ, Tsolakis C, Koulouvaris P, Philippou A. Knowledge and Education on Physical Activity Health Benefits and Prescription Principles Among Greek Medical Students. Behavioral Sciences. 2025; 15(7):925. https://doi.org/10.3390/bs15070925
Chicago/Turabian StyleKyriakoulakou, Eirini, Apostolos Z. Skouras, Charilaos Tsolakis, Panagiotis Koulouvaris, and Anastassios Philippou. 2025. "Knowledge and Education on Physical Activity Health Benefits and Prescription Principles Among Greek Medical Students" Behavioral Sciences 15, no. 7: 925. https://doi.org/10.3390/bs15070925
APA StyleKyriakoulakou, E., Skouras, A. Z., Tsolakis, C., Koulouvaris, P., & Philippou, A. (2025). Knowledge and Education on Physical Activity Health Benefits and Prescription Principles Among Greek Medical Students. Behavioral Sciences, 15(7), 925. https://doi.org/10.3390/bs15070925






