Change in Stress Among Individuals with Chronic Health Conditions and Low Health Literacy Using a Tailored Communication App Promoting Self-Management
Abstract
1. Introduction
2. Materials and Methods
2.1. App Development
2.2. Study Design
2.3. Participant Recruitment and Screening
2.4. Outcome Measures
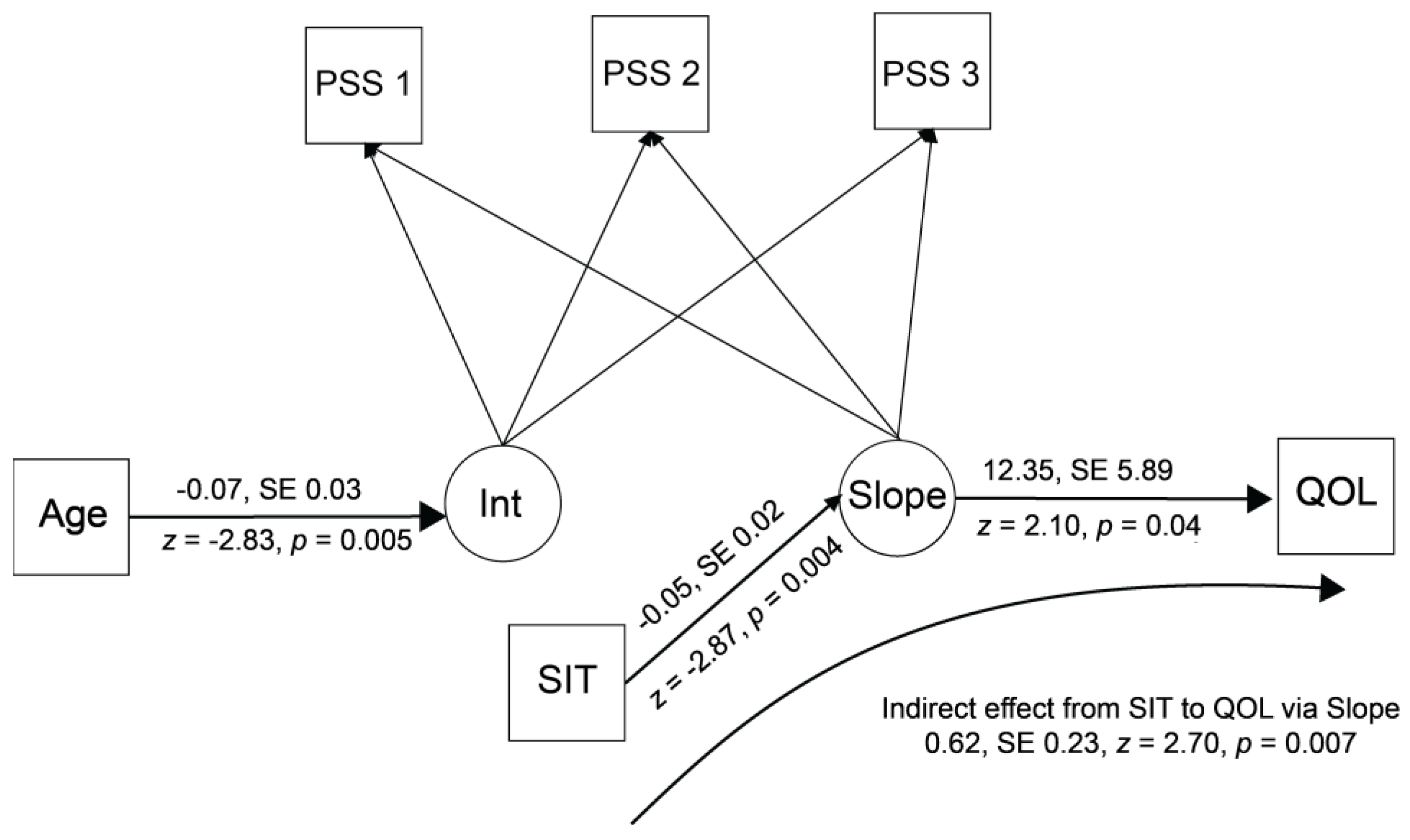
2.5. Statistical Analysis
2.6. Ethics Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CDSM | Chronic disease self-management |
| PAM | Patient Activation Measure |
| CDSE | Chronic Disease Self-Efficacy Scale |
| HRQOL | Health-related quality of life |
| PSS | Perceived Stress Scale |
| SIT | Success in Tailoring Scale |
| LGM | Latent growth curve model |
| Int | Intercept in latent growth curve model |
References
- Adorni, R., Zanatta, F., Cappelletti, E. R., Greco, A., Steca, P., & D’Addario, M. (2024). Effectiveness of a tailored communication intervention to improve physical activity in hypertensive patients: A twelve-month randomized controlled trial. BMC CCardiovascular Disorders, 24(1), 143. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Kuwaiti, A., Nazer, K., Al-Reedy, A., Al-Shehri, S., Al-Muhanna, A., Subbarayalu, A. V., Al Muhanna, D., & Al-Muhanna, F. A. (2023). A review of the role of artificial intelligence in healthcare. Journal of Personalized Medicine, 13(6), 951. [Google Scholar] [CrossRef] [PubMed Central]
- Assari, S., & Bazargan, M. (2019). Race/ethnicity, socioeconomic status, and polypharmacy among older Americans. Pharmacy, 7(2), 41. [Google Scholar] [CrossRef]
- Boger, E., Ellis, J., Latter, S., Foster, C., Kennedy, A., Jones, F., Fenerty, V., Kellar, I., & Demain, S. (2015). Self-management and self-management support outcomes: A systematic review and mixed research synthesis of stakeholder views. PLoS ONE, 10(7), e0130990. [Google Scholar] [CrossRef] [PubMed]
- Bonet-Olivencia, S., Carrillo-Leal, J., Rao, A., & Sasangohar, F. (2024). User-centered design of a diabetes self-management tool for underserved populations. Journal of Diabetes Science and Technology, 18(1), 22–29. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brady, T. J., Murphy, L., O’Colmain, B. J., Beauchesne, D., Daniels, B., & Greenberg, M. (2013). A meta-analysis of health status, health behaviors, and health care utilization outcomes of the chronic disease self-management program. Preventing Chronic Disease, 10, E07. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services. (2012). Chronic conditions among medicare beneficiaries (2012nd ed.). Centers for Medicare and Medicaid Services. [Google Scholar]
- Cohen, S., & Janicki-Deverts, D. (2012). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology, 42(6), 1320–1334. [Google Scholar] [CrossRef]
- Colloca, L. (2018). Preface: The fascinating mechanisms and implications of the placebo effect. International Review of Neurobiology, 138, xv–xx. [Google Scholar] [CrossRef] [PubMed Central]
- Cook, R. F., Billings, D. W., Hersch, R. K., Back, A. S., & Hendrickson, A. (2007). A field test of a web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: Randomized controlled trial. Journal of Medical Internet Research, 9(2), e17. [Google Scholar] [CrossRef]
- Cosijn, E., & Ingwersen, P. (2000). Dimensions of relevance. Information Processing & Management, 36(4), 533–550. [Google Scholar] [CrossRef]
- Davies, L. E., Spiers, G., Kingston, A., Todd, A., Adamson, J., & Hanratty, B. (2020). Adverse outcomes of polypharmacy in older people: Systematic review of reviews. Journal of the American Medical Directors Association, 21(2), 181–187. [Google Scholar] [CrossRef] [PubMed]
- Enders, C. K., & Bandalos, D. L. (2014). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8, 430–457. [Google Scholar] [CrossRef]
- Franklin, M., Lewis, S., Willis, K., Bourke-Taylor, H., & Smith, L. (2018). Patients’ and healthcare professionals’ perceptions of self-management support interactions: Systematic review and qualitative synthesis. Chronic Illness, 14(2), 79–103. [Google Scholar] [CrossRef]
- Fried, T. R., O’Leary, J., Towle, V., Goldstein, M. K., Trentalange, M., & Martin, D. K. (2014). Health outcomes associated with polypharmacy in community-dwelling older adults: A systematic review. Journal of the American Geriatrics Society, 62(12), 2261–2272. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gertsman, S., Ene, I. C., Palmert, S., Liu, A., Makkar, M., Shao, I., Shapiro, J., & Williams, C. (2023). Clinical empathy as perceived by patients with chronic illness in Canada: A qualitative focus group study. CMAJ Open, 11(5), E859–E868. [Google Scholar] [CrossRef] [PubMed Central]
- Gonzalez, J. S., Schneider, H. E., Wexler, D. J., Psaros, C., Delahanty, L. M., Cagliero, E., & Safren, S. A. (2013). Validity of medication adherence self-reports in adults with type 2 diabetes. Diabetes Care, 36(4), 831–837. [Google Scholar] [CrossRef]
- Groll, D. L., To, T., Bombardier, C., & Wright, J. G. (2005). The development of a comorbidity index with physical function as the outcome. Journal of Clinical Epidemiology, 58(6), 595–602. [Google Scholar] [CrossRef]
- Hales, C. M., Servais, J., Martin, C. B., & Kohen, D. (2019). Prescription drug use among adults aged 40–79 in the United States and Canada. National Center for Health Statistics. [Google Scholar]
- Hao, L., Goetze, S., Alessa, T., & Hawley, M. S. (2023). Effectiveness of computer-tailored health communication in increasing physical activity in people with or at risk of long-term conditions: Systematic review and meta-analysis. Journal of Medical Internet Research, 25, e46622. [Google Scholar] [CrossRef]
- Hibbard, J. H., Stockard, J., Mahoney, E. R., & Tusler, M. (2004). Development of the patient activation measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39((4 Pt 1)), 1005–1026. [Google Scholar] [CrossRef]
- Huang, Y., Li, S., Lu, X., Chen, W., & Zhang, Y. (2024). The effect of self-management on patients with chronic diseases: A systematic review and meta-analysis. Healthcare, 12(21), 2151. [Google Scholar] [CrossRef]
- Jacobs, R. J., Lou, J. Q., Ownby, R. L., & Caballero, J. (2016). A systematic review of eHealth interventions to improve health literacy. Health Informatics Journal, 22(2), 81–98. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R. J., Ownby, R. L., Acevedo, A., & Waldrop-Valverde, D. (2017). A qualitative study examining health literacy and chronic illness self-management in Hispanic and non-Hispanic older adults. Journal of Multidisciplinary Healthcare, 10, 167–177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, E. (2024). Exploring the relationship between health literacy and depression among individuals with chronic conditions: Insights from the KCHS. Healthcare, 12(19), 1927. [Google Scholar] [CrossRef] [PubMed]
- Lee, A. A., Piette, J. D., Heisler, M., Janevic, M. R., Langa, K. M., & Rosland, A. M. (2017). Family members’ experiences supporting adults with chronic illness: A national survey. Families, Systems, & Health, 35(4), 463–473. [Google Scholar] [CrossRef] [PubMed Central]
- Liu, F., Wang, Y., Feng, Q., Zhu, L., & Li, G. (2024). Optimizing e-learning environments: Leveraging large language models for personalized education pathways. In Proceedings of the 2024 5th International Conference on Education, Knowledge and Information Management (ICEKIM 2024) (pp. 811–817). Atlantis Press. [Google Scholar]
- Lorig, K., Stewart, A., Ritter, P., Gonzalez, V. M., Laurent, D., & Lynch, J. (1996). Outcome measures for health education and other health care interventions. Sage. [Google Scholar]
- Lorig, K. R., Ritter, P., Stewart, A. L., Sobel, D. S., Brown, B. W., Jr., Bandura, A., Gonzalez, V. M., Laurent, D. D., & Holman, H. R. (2001). Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care, 39(11), 1217–1223. [Google Scholar] [CrossRef]
- Magallón-Botaya, R., Méndez-López, F., Oliván-Blázquez, B., Carlos Silva-Aycaguer, L., Lerma-Irureta, D., & Bartolomé-Moreno, C. (2023). Effectiveness of health literacy interventions on anxious and depressive symptomatology in primary health care: A systematic review and meta-analysis. Front Public Health, 11, 1007238. [Google Scholar] [CrossRef] [PubMed Central]
- Mucherino, S., Gimeno-Miguel, A., Carmona-Pirez, J., Gonzalez-Rubio, F., Ioakeim-Skoufa, I., Moreno-Juste, A., Orlando, V., Aza-Pascual-Salcedo, M., Poblador-Plou, B., Menditto, E., & Prados-Torres, A. (2021). Changes in multimorbidity and polypharmacy patterns in young and adult population over a 4-year period: A 2011–2015 comparison using real-world data. International Journal of Environmental Research and Public Health, 18(9), 4422. [Google Scholar] [CrossRef] [PubMed Central]
- Munster-Segev, M., Fuerst, O., Kaplan, S. A., & Cahn, A. (2017). Incorporation of a stress reducing mobile app in the care of patients with type 2 diabetes: A prospective study. JMIR Mhealth Uhealth, 5(5), e75. [Google Scholar] [CrossRef]
- Muthén, L. K., & Muthén, B. O. (2017). Mplus user’s guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Ownby, R. L. (2024). Can a study that’s not statistically significant be meaningful? American Journal of Aging Science and Research, 4(1), 1–4. [Google Scholar] [CrossRef] [PubMed Central]
- Ownby, R. L., Acevedo, A., Waldrop-Valverde, D., Caballero, J., Simonson, M., Davenport, R., Kondwani, K., & Jacobs, R. J. (2017). A mobile app for chronic disease self-management: Protocol for a randomized controlled trial. JMIR Research Protocols, 6(4), e53. [Google Scholar] [CrossRef]
- Ownby, R. L., Simonson, M., Caballero, J., Thomas-Purcell, K., Davenport, R., Purcell, D., Ayala, V., Gonzalez, J., Patel, N., & Kondwani, K. (2024). A mobile app for chronic disease self-management for individuals with low health literacy: A multisite randomized controlled clinical trial. Journal of Ageing and Longevity, 4(2), 51–71. [Google Scholar] [CrossRef] [PubMed]
- Patel, N., Waldrop, D., & Ownby, R. L. (2023). Creating a tailored info app to promote self-management skills in persons with chronic health conditions: Development strategies and user experience. Distance Learning (Greenwich), 20(1), 9–18. [Google Scholar]
- Pathirana, T. I., & Jackson, C. A. (2018). Socioeconomic status and multimorbidity: A systematic review and meta-analysis. Australian and New Zealand Journal of Public Health, 42(2), 186–194. [Google Scholar] [CrossRef]
- Petty, R. E., & Cacioppo, J. T. (1986). The elaboration likelihood model of persuasion. In L. Berkowitz (Ed.), Advances in experimenal social psychology (pp. 123–205). Academic Press. [Google Scholar]
- Quiñones, A. R., Botoseneanu, A., Markwardt, S., Nagel, C. L., Newsom, J. T., Dorr, D. A., & Allore, H. G. (2019). Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS ONE, 14(6), e0218462. [Google Scholar] [CrossRef] [PubMed]
- Rosland, A. M., Heisler, M., Janevic, M. R., Connell, C. M., Langa, K. M., Kerr, E. A., & Piette, J. D. (2013). Current and potential support for chronic disease management in the United States: The perspective of family and friends of chronically ill adults. Families, Systems, & Health, 31(2), 119–131. [Google Scholar] [CrossRef] [PubMed Central]
- Schapira, M. M., Swartz, S., Ganschow, P. S., Jacobs, E. A., Neuner, J. M., Walker, C. M., & Fletcher, K. E. (2017). Tailoring educational and behavioral interventions to level of health literacy: A systematic review. MDM Policy & Practice, 2(1), 2381468317714474. [Google Scholar] [CrossRef] [PubMed Central]
- Schooley, B., Singh, A., Hikmet, N., Brookshire, R., & Patel, N. (2020). Integrated digital patient education at the bedside for patients with chronic conditions: Observational study. JMIR Mhealth Uhealth, 8(12), e22947. [Google Scholar] [CrossRef] [PubMed Central]
- Schulman-Green, D., Jaser, S., Martin, F., Alonzo, A., Grey, M., McCorkle, R., Redeker, N. S., Reynolds, N., & Whittemore, R. (2012). Processes of self-management in chronic illness. Journal of Nursing Scholarship, 44(2), 136–144. [Google Scholar] [CrossRef] [PubMed Central]
- Stogios, N., Kaur, B., Huszti, E., Vasanthan, J., & Nolan, R. P. (2020). Advancing digital health interventions as a clinically applied science for blood pressure reduction: A systematic review and meta-analysis. Canadian Journal of Cardiology, 36(5), 764–774. [Google Scholar] [CrossRef]
- van der Heide, I., Poureslami, I., Mitic, W., Shum, J., Rootman, I., & FitzGerald, J. M. (2018). Health literacy in chronic disease management: A matter of interaction. Journal of Clinical Epidemiology, 102, 134–138. [Google Scholar] [CrossRef]
- Van Wilder, L., Pype, P., Mertens, F., Rammant, E., Clays, E., Devleesschauwer, B., Boeckxstaens, P., & De Smedt, D. (2021). Living with a chronic disease: Insights from patients with a low socioeconomic status. BMC Family Practice, 22(1), 233. [Google Scholar] [CrossRef] [PubMed]
- Ware, J. E., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 478–483. [Google Scholar] [CrossRef]
- Wieczorek, M., Meier, C., Vilpert, S., Reinecke, R., Borrat-Besson, C., Maurer, J., & Kliegel, M. (2023). Association between multiple chronic conditions and insufficient health literacy: Cross-sectional evidence from a population-based sample of older adults living in Switzerland. BMC Public Health, 23(1), 253. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, S., Walther, J.-K., Hecht, M., & Nagengast, B. (2022). What is the maximum likelihood estimate when the initial solution to the optimization problem is inadmissible? The case of negatively estimated variances. Psych, 4(3), 343–356. [Google Scholar] [CrossRef]
| Variable | Count |
|---|---|
| Men | 144 |
| Women | 165 |
| White | 41 |
| Black | 268 |
| Mean (SD) | |
| Age in Years | 57.63 (8.41) |
| Education Years | 11.86 (1.85) |
| Total Number of Health Conditions | 6.47 (2.78) |
| HRQOL (SF General Health) 1 | 60.19 (19.66) |
| Perceived Stress Scale—Baseline | 22.46 (3.81) |
| Perceived Stress Scale—Follow-Up 1 | 21.54 (3.76) |
| Perceived Stress Scale—Follow-Up 2 | 21.84 (3.27) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ownby, R.L.; Caballero, J. Change in Stress Among Individuals with Chronic Health Conditions and Low Health Literacy Using a Tailored Communication App Promoting Self-Management. Behav. Sci. 2025, 15, 783. https://doi.org/10.3390/bs15060783
Ownby RL, Caballero J. Change in Stress Among Individuals with Chronic Health Conditions and Low Health Literacy Using a Tailored Communication App Promoting Self-Management. Behavioral Sciences. 2025; 15(6):783. https://doi.org/10.3390/bs15060783
Chicago/Turabian StyleOwnby, Raymond L., and Joshua Caballero. 2025. "Change in Stress Among Individuals with Chronic Health Conditions and Low Health Literacy Using a Tailored Communication App Promoting Self-Management" Behavioral Sciences 15, no. 6: 783. https://doi.org/10.3390/bs15060783
APA StyleOwnby, R. L., & Caballero, J. (2025). Change in Stress Among Individuals with Chronic Health Conditions and Low Health Literacy Using a Tailored Communication App Promoting Self-Management. Behavioral Sciences, 15(6), 783. https://doi.org/10.3390/bs15060783







