Primary and Emergency Care Use: The Roles of Health Literacy, Patient Activation, and Sleep Quality in a Latent Profile Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Questionnaire
2.3. Statistical Analysis
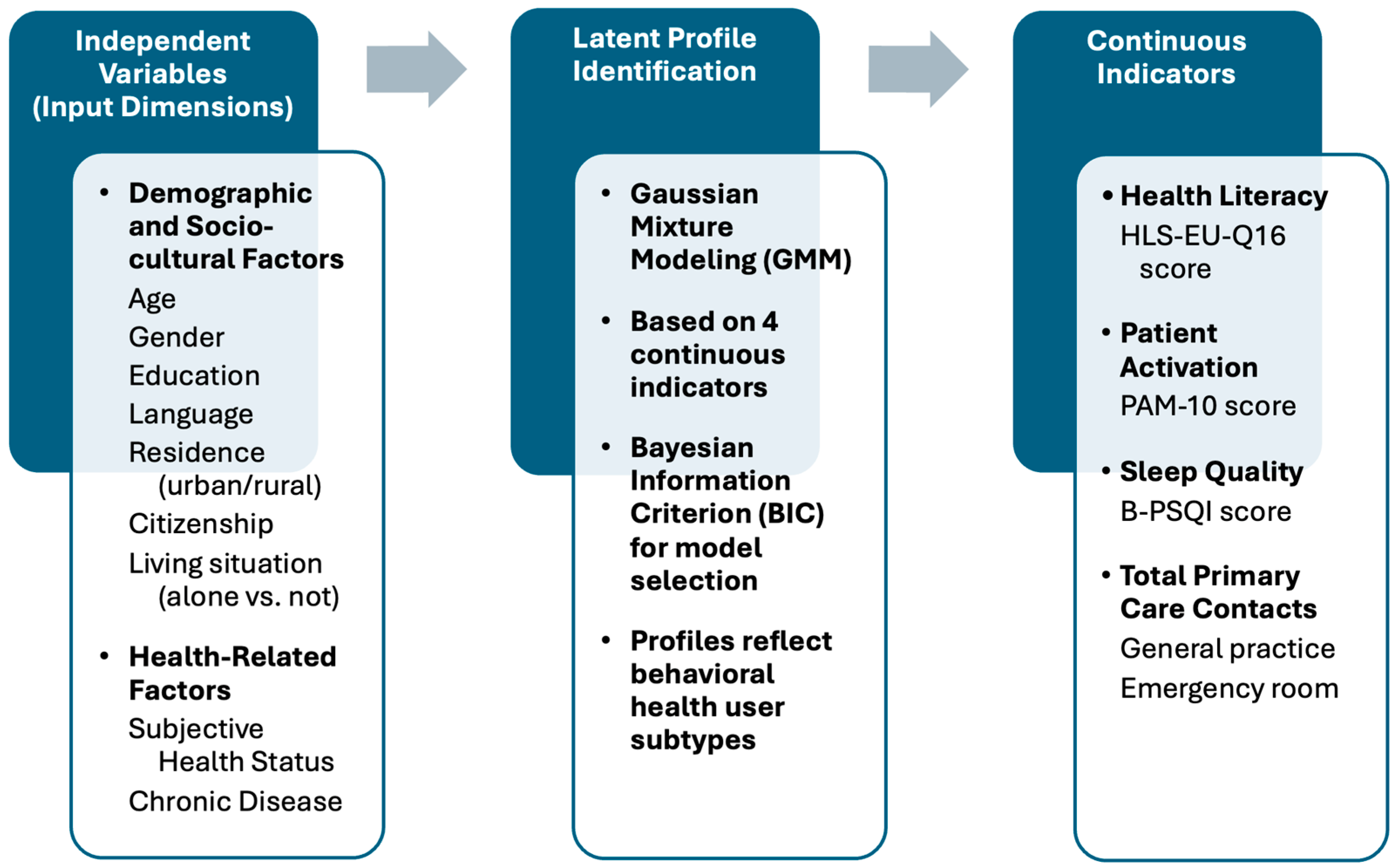
2.3.1. Latent Profile Analysis
2.3.2. Descriptive Statistics and Comparisons
2.3.3. Multinomial Logistic Regression Analysis
3. Results
3.1. Sample Characteristics
3.2. Clustering Procedure, Model Selection, Profiles, and Between-Cluster Comparisons
- Cluster 1 (n = 1197, 72.8%) represented the largest group and was characterized by moderate patient activation, slightly above-average health literacy (z = +0.125), average sleep quality, and below-average primary and urgent care service utilization in GP offices or ERs (z = −0.369). This cluster likely represents a general population profile with stable health behaviors and self-management.
- Cluster 2 (n = 424, 25.8%) displayed the lowest health literacy scores (z = −0.247), slightly reduced activation, average sleep, and increased utilization of GP and ED services (z = +0.671). This group may reflect a vulnerable subgroup at risk of overutilization due to limited comprehension and self-management capacities.
- Cluster 3 (n = 24, 1.4%) was a small but distinct group marked by extremely high patient activation (z = +1.91), slightly elevated health literacy, and the highest utilization of healthcare services.
3.3. Primary and Urgent Care Services Utilization Stratified by Behavioral Determinants
3.3.1. Sleep Quality
3.3.2. Health Literacy and Patient Activation
3.4. Multinomial Logistic Regression of Sociodemographic and Health-Related Predictors of Cluster Membership
4. Discussion
4.1. Interpretation and Comparison with Existing Literature
4.2. Implications for Practice and Policy
4.3. Strengths and Limitations
4.4. Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of Variance |
| BIC | Bayesian Information Criterion |
| B-PSQI | Brief Pittsburgh Sleep Quality Index |
| CI | Confidence Interval |
| ED | Emergency Department |
| EM | Expected Maximization |
| GMM | Gaussian Mixture Modeling |
| GP | General Practitioner |
| HLS-EU-Q | European Health Literacy Survey Questionnaire |
| IQR | Interquartile Range |
| LPA | Latent Profile Analysis |
| LR | Likelihood Ratio |
| OR | Odds Ratio |
| PAM | Patient Activation Measure |
| SD | Standard Deviation |
References
- Andersen, M. H., Hermansen, Å., Dahl, K. G., Lønning, K., Meyer, K. B., Vidnes, T. K., & Wahl, A. K. (2024). Profiles of health literacy and digital health literacy in clusters of hospitalised patients: A single-centre, cross-sectional study. BMJ Open, 14(5), e077440. [Google Scholar] [CrossRef] [PubMed]
- Andersen, R., & Newman, J. F. (2005). Societal and individual determinants of medical care utilization in the United States. The Milbank Quarterly, 83(4). Online-only. [Google Scholar] [CrossRef]
- Anderson, L. H., Whitebird, R. R., Schultz, J., McEvoy, C. E., Kreitzer, M. J., & Gross, C. R. (2014). Healthcare utilization and costs in persons with insomnia in a managed care population. The American Journal of Managed Care, 20(5), e157–e165. [Google Scholar]
- Bader, M., Zheng, L., Rao, D., Shiyanbola, O., Myers, L., Davis, T., O’Leary, C., McKee, M., Wolf, M., & Assaf, A. R. (2022). Towards a more patient-centered clinical trial process: A systematic review of interventions incorporating health literacy best practices. Contemporary Clinical Trials, 116, 106733. [Google Scholar] [CrossRef] [PubMed]
- Baker, D. W., Parker, R. M., Williams, M. V., & Clark, W. S. (1998). Health literacy and the risk of hospital admission. Journal of General Internal Medicine, 13(12), 791–798. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155, 97–107. [Google Scholar] [CrossRef]
- Brenk-Franz, K., Hibbard, J. H., Herrmann, W. J., Freund, T., Szecsenyi, J., Djalali, S., Steurer-Stey, C., Sönnichsen, A., Tiesler, F., Storch, M., Schneider, N., & Gensichen, J. (2013). Validation of the German version of the patient activation measure 13 (PAM13-D) in an international multicentre study of primary care patients. PLoS ONE, 8(9), e74786. [Google Scholar] [CrossRef]
- Bu, F., & Fancourt, D. (2021). How is patient activation related to healthcare service utilization? Evidence from electronic patient records in England. BMC Health Services Research, 21(1), 1196. [Google Scholar] [CrossRef]
- Chong, J. L., Lim, K. K., & Matchar, D. B. (2019). Population segmentation based on healthcare needs: A systematic review. Systematic Reviews, 8(1), 202. [Google Scholar] [CrossRef]
- Couture, É. M., Chouinard, M.-C., Fortin, M., & Hudon, C. (2018). The relationship between health literacy and patient activation among frequent users of healthcare services: A cross-sectional study. BMC Family Practice, 19(1), 38. [Google Scholar] [CrossRef]
- Curcio, G., Tempesta, D., Scarlata, S., Marzano, C., Moroni, F., Rossini, P. M., Ferrara, M., & De Gennaro, L. (2013). Validity of the Italian version of the Pittsburgh Sleep Quality Index (PSQI). Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology, 34(4), 511–519. [Google Scholar] [CrossRef]
- Dumitra, T., Ganescu, O., Hu, R., Fiore, J. F., Kaneva, P., Mayo, N., Lee, L., Liberman, A. S., Chaudhury, P., Ferri, L., & Feldman, L. S. (2021). Association between patient activation and health care utilization after thoracic and abdominal surgery. JAMA Surgery, 156(1), e205002. [Google Scholar] [CrossRef]
- Evans, W. D., Thomas, C. N., Favatas, D., Smyser, J., & Briggs, J. (2019). Digital segmentation of priority populations in public health. Health Education & Behavior, 46(Suppl. S2), 81S–89S. [Google Scholar] [CrossRef]
- Friis, K., Pedersen, M. H., Aaby, A., Lasgaard, M., & Maindal, H. T. (2020). Impact of low health literacy on healthcare utilization in individuals with cardiovascular disease, chronic obstructive pulmonary disease, diabetes and mental disorders. A Danish population-based 4-year follow-up study. European Journal of Public Health, 30(5), 866–872. [Google Scholar] [CrossRef]
- Goto, E., Ishikawa, H., Okuhara, T., & Kiuchi, T. (2019). Relationship of health literacy with utilization of health-care services in a general Japanese population. Preventive Medicine Reports, 14, 100811. [Google Scholar] [CrossRef]
- Graffigna, G., Barello, S., Bonanomi, A., Lozza, E., & Hibbard, J. (2015). Measuring patient activation in Italy: Translation, adaptation and validation of the Italian version of the patient activation measure 13 (PAM13-I). BMC Medical Informatics and Decision Making, 15(1), 109. [Google Scholar] [CrossRef]
- Greene, J., & Hibbard, J. H. (2012). Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. Journal of General Internal Medicine, 27(5), 520–526. [Google Scholar] [CrossRef]
- Greene, J. C., Haun, J. N., French, D. D., Chambers, S. L., & Roswell, R. H. (2019). Reduced hospitalizations, emergency room visits, and costs associated with a web-based health literacy, aligned-incentive intervention: Mixed methods study. Journal of Medical Internet Research, 21(10), e14772. [Google Scholar] [CrossRef]
- Gwynn, K. B., Winter, M. R., Cabral, H. J., Wolf, M. S., Hanchate, A. D., Henault, L., Waite, K., Bickmore, T. W., & Paasche-Orlow, M. K. (2016). Racial disparities in patient activation: Evaluating the mediating role of health literacy with path analyses. Patient Education and Counseling, 99(6), 1033–1037. [Google Scholar] [CrossRef]
- Hibbard, J. H., Greene, J., Sacks, R., Overton, V., & Parrotta, C. D. (2016). Adding a measure of patient self-management capability to risk assessment can improve prediction of high costs. Health Affairs (Project Hope), 35(3), 489–494. [Google Scholar] [CrossRef]
- Hibbard, J. H., Mahoney, E. R., Stock, R., & Tusler, M. (2007). Do increases in patient activation result in improved self-management behaviors? Health Services Research, 42(4), 1443–1463. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J. H., Mahoney, E. R., Stockard, J., & Tusler, M. (2005). Development and testing of a short form of the patient activation measure. Health Services Research, 40((6 Pt 1)), 1918–1930. [Google Scholar] [CrossRef]
- Hinz, A., Glaesmer, H., Brähler, E., Löffler, M., Engel, C., Enzenbach, C., Hegerl, U., & Sander, C. (2017). Sleep quality in the general population: Psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Medicine, 30, 57–63. [Google Scholar] [CrossRef]
- Huyett, P., & Bhattacharyya, N. (2021). Incremental health care utilization and expenditures for sleep disorders in the United States. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 17(10), 1981–1986. [Google Scholar] [CrossRef]
- Kaufmann, C. N., Canham, S. L., Mojtabai, R., Gum, A. M., Dautovich, N. D., Kohn, R., & Spira, A. P. (2013). Insomnia and health services utilization in middle-aged and older adults: Results from the health and retirement study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 68(12), 1512–1517. [Google Scholar] [CrossRef] [PubMed]
- Kinney, R. L., Lemon, S. C., Person, S. D., Pagoto, S. L., & Saczynski, J. S. (2015). The association between patient activation and medication adherence, hospitalization, and emergency room utilization in patients with chronic illnesses: A systematic review. Patient Education and Counseling, 98(5), 545–552. [Google Scholar] [CrossRef]
- Lin, C.-Y., Chung, M. L., Schuman, D. L., Biddle, M. J., Mudd-Martin, G., Miller, J. L., Hammash, M., Schooler, M. P., Rayens, M. K., Feltner, F. J., & Moser, D. K. (2023). Psychometric properties of the patient activation measure in family caregivers of patients with chronic illnesses. Nursing Research, 72(4), 292. [Google Scholar] [CrossRef] [PubMed]
- Lorini, C., Lastrucci, V., Mantwill, S., Vettori, V., Bonaccorsi, G., & Florence Health Literacy Research Group. (2019). Measuring health literacy in Italy: A validation study of the HLS-EU-Q16 and of the HLS-EU-Q6 in Italian language, conducted in Florence and its surroundings. Annali Dell’Istituto Superiore Di Sanita, 55(1), 10–18. [Google Scholar] [CrossRef]
- Morris, N. S., MacLean, C. D., Chew, L. D., & Littenberg, B. (2006). The single item literacy screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice, 7(1), 21. [Google Scholar] [CrossRef]
- Nutbeam, D., & Lloyd, J. E. (2021). Understanding and responding to health literacy as a social determinant of health. Annual Review of Public Health, 42, 159–173. [Google Scholar] [CrossRef]
- Olatunde, K., & Patton, S. (2023). Association between insomnia and healthcare utilization: A scoping review of the literature. American Journal of Lifestyle Medicine, 19(3), 403–418. [Google Scholar] [CrossRef] [PubMed]
- Pelikan, J. M., Ganahl, K., Van den Broucke, S., & Sørensen, K. (2019). Measuring health literacy in Europe: Introducing the European health literacy survey questionnaire (HLS-EU-Q). In International handbook of health literacy (pp. 115–138). Policy Press. [Google Scholar]
- Pigazzini, G., Wieczorek, M., Meier, C., & Maurer, J. (2024). Inadequate health literacy and higher healthcare utilization among older adults in Switzerland: Cross-sectional evidence from a population-based study. Swiss Medical Weekly, 154, 3515. [Google Scholar] [CrossRef] [PubMed]
- Rasu, R., Bawa, W. A., Suminski, R., Snella, K., & Warady, B. (2015). Health literacy impact on national healthcare utilization and expenditure. International Journal of Health Policy and Management, 4(11), 747–755. [Google Scholar] [CrossRef]
- Sancho-Domingo, C., Carballo, J. L., Coloma-Carmona, A., & Buysse, D. J. (2021). Brief version of the Pittsburgh Sleep Quality Index (B-PSQI) and measurement invariance across gender and age in a population-based sample. Psychological Assessment, 33(2), 111–121. [Google Scholar] [CrossRef]
- Sandlund, C., Westman, J., & Hetta, J. (2016). Factors associated with self-reported need for treatment of sleeping difficulties: A survey of the general Swedish population. Sleep Medicine, 22, 65–74. [Google Scholar] [CrossRef]
- Simon, G. E., & VonKorff, M. (1997). Prevalence, burden, and treatment of insomnia in primary care. The American Journal of Psychiatry, 154(10), 1417–1423. [Google Scholar] [CrossRef]
- Sørensen, K., Pelikan, J. M., Röthlin, F., Ganahl, K., Slonska, Z., Doyle, G., Fullam, J., Kondilis, B., Agrafiotis, D., Uiters, E., Falcon, M., Mensing, M., Tchamov, K., van den Broucke, S., Brand, H., & HLS-EU Consortium. (2015). Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). European Journal of Public Health, 25(6), 1053–1058. [Google Scholar] [CrossRef]
- Viktorsson, L., Yngman-Uhlin, P., Törnvall, E., & Falk, M. (2019). Healthcare utilization and health literacy among young adults seeking care in Sweden: Findings from a cross-sectional and retrospective study with questionnaire and registry-based data. Primary Health Care Research & Development, 20, e151. [Google Scholar] [CrossRef]
- Weiss, B. D., Mays, M. Z., Martz, W., Castro, K. M., DeWalt, D. A., Pignone, M. P., Mockbee, J., & Hale, F. A. (2005). Quick assessment of literacy in primary care: The newest vital sign. The Annals of Family Medicine, 3(6), 514–522. [Google Scholar] [CrossRef]
- Wickwire, E. M., Vadlamani, A., Tom, S. E., Johnson, A. M., Scharf, S. M., & Albrecht, J. S. (2020). Economic aspects of insomnia medication treatment among Medicare beneficiaries. Sleep, 43(1), zsz192. [Google Scholar] [CrossRef]
- Wiedermann, C. J., Barbieri, V., Lombardo, S., Gärtner, T., Rina, P., Eisendle, K., Piccoliori, G., Engl, A., & Ausserhofer, D. (2025). Health information use and trust: The role of health literacy and patient activation in a multilingual European region. International Journal of Environmental Research and Public Health, 22(4), 570. [Google Scholar] [CrossRef] [PubMed]
- Włodarczyk, D., & Chylińska, J. (2022). Profiles of health-related patient activation and their determinants: The results of a cluster analysis of older adults—Conclusions for patient counselling. International Journal of Environmental Research and Public Health, 19(4), 2487. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A. L., Liu, S., White, B. X., Liu, X. C., Durantini, M., Chan, M. S., Dai, W., Zhou, Y., Leung, M., Ye, Q., O’Keefe, D., Palmese, L., & Albarracín, D. (2024). Health-promotion interventions targeting multiple behaviors: A meta-analytic review of general and behavior-specific processes of change. Psychological Bulletin, 150(7), 798–838. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total n = 2090 | HLS-EU-Q16 Score Complete, n = 1645 | HLS-EU-Q16 Score Incomplete, n = 445 | p-Value 1 |
|---|---|---|---|---|
| Gender, n (%) | 0.361 | |||
| male | 937 (44.8%) | 746 (45.4) | 191 (42.9) | |
| female | 1153 (55.2%) | 899 (54.6) | 254 (57.1) | |
| Age group (years), n (%) | 0.041 | |||
| 18–34 | 383 (18.3) | 313 (19.0) | 70 (15.7) | |
| 35–54 | 647 (31.0) | 521 (31.7) | 126 (28.3) | |
| 55–99 | 1060 (50.7) | 811 (49.3) | 249 (56.0) | |
| Mother tongue, n (%) | <0.001 | |||
| German | 1398 (66.9) | 1074 (65.3) | 324 (72.8) | |
| Italian | 499 (23.9) | 420 (25.5) | 79 (17.8) | |
| Ladin | 82 (3.9) | 71 (4.3) | 10 (2.2) | |
| other, more than one | 112 (5.3) | 80 (4.8) | 32 (7.2) | |
| Citizenship, n (%) | 0.083 | |||
| Italian | 2011 (96.2) | 1589 (96.6) | 422 (94.8) | |
| other | 79 (3.8) | 56 (3.4) | 23 (5.2) | |
| Residence, n (%) 2 | 0.324 | |||
| urban | 381 (18.2) | 307 (18.7) | 74 (16.6) | |
| rural | 1709 (81.8) | 1338 (81.3) | 371 (83.4) | |
| Level of education, n (%) | <0.001 2 | |||
| middle school | 492 (23.5) | 339 (20.6) | 153 (34.4) | |
| vocational school | 674 (32.3) | 520 (31.6) | 154 (34.6) | |
| high school | 530 (25.4) | 432 (26.3) | 98 (22.0) | |
| university | 394 (18.8) | 534 (21.5) | 40 (9.0) | |
| Living alone, n (%) | 0.003 | |||
| yes | 383 (18.3) | 280 (17.0) | 103 (23.2) | |
| no | 1707 (81.7) | 1386 (83.0) | 342 (76.8) | |
| Healthcare worker, n (%) | <0.001 | |||
| yes | 217 (10.4) | 194 (11.8) | 23 (5.2) | |
| no | 1872 (89.6) | 1450 (88.2) | 422 (94.8) | |
| Trust in GP, n (%) | <0.001 | |||
| very much | 893 (42.7) | 727 (44.2) | 166 (37.3) | |
| some | 961 (46.0) | 752 (45.7) | 209 (47.0) | |
| a little | 193 (9.2) | 140 (8.5) | 53 (11.9) | |
| not at all | 43 (2.1) | 26 (1.6) | 17 (3.8) | |
| Chronic disease, n (%) | 0.603 | |||
| yes | 795 (38.0) | 621 (37.8) | 174 (39.1) | |
| no | 1295 (62.0) | 1024 (62.2) | 271 (61.9) | |
| Health status, median [IQR] 3 | 80.0 [20.0] | 80.0 [20.0] | 80.0 [25.0] | <0.001 |
| HLS-EU-Q16 score, median [IQR] 4 | n.d. | 12.0 [5.0] | n.d. | — |
| PAM-10 score, median [IQR] 5 | 52.9 [12.6] | 52.9 [12.6] | 51.0 [9.3] | <0.001 |
| B-PSQI score, median [IQR] 6 | 3.0 [4.0] | 3.0 [4.0] | 3.0 [4.0] | 0.732 |
| Variable | 1—Balanced Self-Regulators (n = 1197) | 2—Struggling Navigators (n = 424) | 3—Hyper-Engaged Users (n = 24) | p-Value 6 |
|---|---|---|---|---|
| Gender, n (%) | 0.059 | |||
| male | 564 (47.1) | 173 (40.8) | 9 (37.5) | |
| female | 633 (52.9) | 251 (59.2) | 15 (62.5) | |
| Age group (years), n (%) | ||||
| 18–34 | 249 (20.8%) | 61 (10.4%) | 3 (9.4%) | <0.001 |
| 35–54 | 416 (34.8%) | 100 (17.1%) | 5 (15.6%) | |
| 55–99 | 532 (44.4%) | 424 (72.5%) | 24 (75.0%) | |
| Mother tongue, n (%) | <0.001 | |||
| German | 808 (67.5%) | 263 (62.0%) | 3 (12.5%) | |
| Italian | 282 (23.6%) | 119 (28.1%) | 19 (79.2%) | |
| Ladin | 56 (4.7%) | 14 (3.3%) | 1 (4.2%) | |
| other | 31 (2.6%) | 17 (4.0%) | 0 (0.0%) | |
| more than one language | 20 (1.7%) | 11 (2.6%) | 1 (4.2%) | |
| Citizenship, n (%) | 0.925 | |||
| Italian | 1156 (96.6%) | 410 (96.7%) | 23 (95.8%) | |
| other | 41 (3.4%) | 14 (3.3%) | 1 (4.2%) | |
| Residence, n (%) 1 | 0.009 | |||
| urban | 213 (17.8%) | 84 (19.8%) | 10 (41.7%) | |
| rural | 984 (82.2%) | 340 (80.2%) | 14 (58.3%) | |
| Level of education, n (%) | <0.001 | |||
| middle school | 205 (17.1%) | 128 (30.2%) | 6 (25.0%) | |
| vocational school | 378 (31.6%) | 138 (32.5%) | 4 (16.7%) | |
| high school | 325 (27.2%) | 100 (23.6%) | 7 (29.2%) | |
| university | 289 (24.1%) | 58 (13.7%) | 7 (29.2%) | |
| Living alone, n (%) | 0.934 | |||
| no | 999 (83.5%) | 346 (81.6%) | 20 (83.3%) | |
| yes | 198 (16.5%) | 78 (18.4%) | 4 (16.7%) | |
| Healthcare worker, n (%) | 0.003 | |||
| yes | 161 (13.4%) | 31 (7.3%) | 2 (8.3%) | |
| no | 1036 (86.6%) | 392 (92.7%) | 22 (91.7%) | |
| Trust in GP, n (%) | 0.575 | |||
| very much | 525 (43.9%) | 190 (44.8%) | 12 (50.0%) | |
| some | 552 (46.1%) | 190 (44.8%) | 10 (41.7%) | |
| a little | 105 (8.8%) | 33 (7.8%) | 2 (8.3%) | |
| not at all | 15 (1.3%) | 11 (2.6%) | 0 (0.0%) | |
| Chronic disease, n (%) | <0.001 | |||
| no | 846 (70.7%) | 168 (39.6%) | 10 (41.7%) | |
| yes | 351 (29.3%) | 256 (60.4%) | 14 (58.3%) | |
| Health status perception, n (%) 2 | <0.001 | |||
| positive | 861 (71.9%) | 169 (39.9%) | 11 (45.8%) | |
| reduced | 336 (28.1%) | 255 (60.1%) | 13 (54.2%) | |
| Patient activation (PAM-10), n (%) 3 | <0.001 | |||
| disengaged and overwhelmed | 160 (13.4%) | 90 (21.2%) | 4 (16.7%) | |
| becoming aware but still struggling | 474 (39.6%) | 192 (45.3%) | 8 (33.3%) | |
| taking action | 305 (25.5%) | 86 (20.3%) | 6 (25.0%) | |
| maintaining behaviors and pushing further | 258 (21.6%) | 56 (13.2%) | 6 (25.0%) | |
| Health literacy (HLS-EU-Q16), n (%) 4 | <0.001 | |||
| inadequate | 111 (9.3%) | 144 (34.0%) | 3 (12.5%) | |
| problematic | 418 (34.9%) | 143 (33.7%) | 6 (25.0%) | |
| sufficient | 668 (55.8%) | 137 (32.3%) | 15 (62.5%) | |
| Sleep quality (B-PSQI), n (%) 5 | <0.001 | |||
| poor sleep (score > 5) | 211 (17.6%) | 229 (54.0%) | 12 (50.0%) | |
| good sleep (score ≤ 5) | 986 (82.4%) | 195 (46.0%) | 12 (50.0%) |
| Cluster 1 | Predictor | B (Log Odds) 2 | Odds Ratio 3 | 95% CI 4 | p-Value |
|---|---|---|---|---|---|
| Hyper-Engaged Users | Age (years) | 0.010 | 1.010 | 1.001–1.018 | 0.023 |
| Reduced health status | −0.414 | 0.661 | 0.515–0.849 | 0.001 | |
| Living alone (yes) | −0.516 | 0.597 | 0.385–0.927 | 0.022 | |
| Struggling Navigators | Mother tongue: Italian | 0.473 | 1.605 | 1.058–2.434 | 0.026 |
| Mother tongue: Other | 0.399 | 1.491 | 1.022–2.175 | 0.038 | |
| Chronic disease (yes) | −0.856 | 0.425 | 0.327–0.554 | <0.001 | |
| Living alone (yes) | −0.994 | 0.370 | 0.287–0.476 | <0.001 | |
| Reduced health status | −0.426 | 0.653 | 0.416–1.026 | 0.064 | |
| Work in healthcare (yes) | –0.515 | 0.597 | 0.385–0.927 | 0.022 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ausserhofer, D.; Barbieri, V.; Lombardo, S.; Gärtner, T.; Eisendle, K.; Piccoliori, G.; Engl, A.; Wiedermann, C.J. Primary and Emergency Care Use: The Roles of Health Literacy, Patient Activation, and Sleep Quality in a Latent Profile Analysis. Behav. Sci. 2025, 15, 724. https://doi.org/10.3390/bs15060724
Ausserhofer D, Barbieri V, Lombardo S, Gärtner T, Eisendle K, Piccoliori G, Engl A, Wiedermann CJ. Primary and Emergency Care Use: The Roles of Health Literacy, Patient Activation, and Sleep Quality in a Latent Profile Analysis. Behavioral Sciences. 2025; 15(6):724. https://doi.org/10.3390/bs15060724
Chicago/Turabian StyleAusserhofer, Dietmar, Verena Barbieri, Stefano Lombardo, Timon Gärtner, Klaus Eisendle, Giuliano Piccoliori, Adolf Engl, and Christian J. Wiedermann. 2025. "Primary and Emergency Care Use: The Roles of Health Literacy, Patient Activation, and Sleep Quality in a Latent Profile Analysis" Behavioral Sciences 15, no. 6: 724. https://doi.org/10.3390/bs15060724
APA StyleAusserhofer, D., Barbieri, V., Lombardo, S., Gärtner, T., Eisendle, K., Piccoliori, G., Engl, A., & Wiedermann, C. J. (2025). Primary and Emergency Care Use: The Roles of Health Literacy, Patient Activation, and Sleep Quality in a Latent Profile Analysis. Behavioral Sciences, 15(6), 724. https://doi.org/10.3390/bs15060724







