The Relationship Between Illusory Health Beliefs, Recommended Health Behaviours, and Complementary and Alternative Medicine: An Investigation Across Multiple Time Points
Abstract
1. Introduction
Current Study
2. Method
2.1. Participants
2.2. Instruments
2.2.1. Time Point One Measure
2.2.2. Time Point Two Measures
2.2.3. Time Point Three Measures
2.3. Procedure and Ethics
2.4. Analysis Plan
3. Results
3.1. Data Screening and Correlations
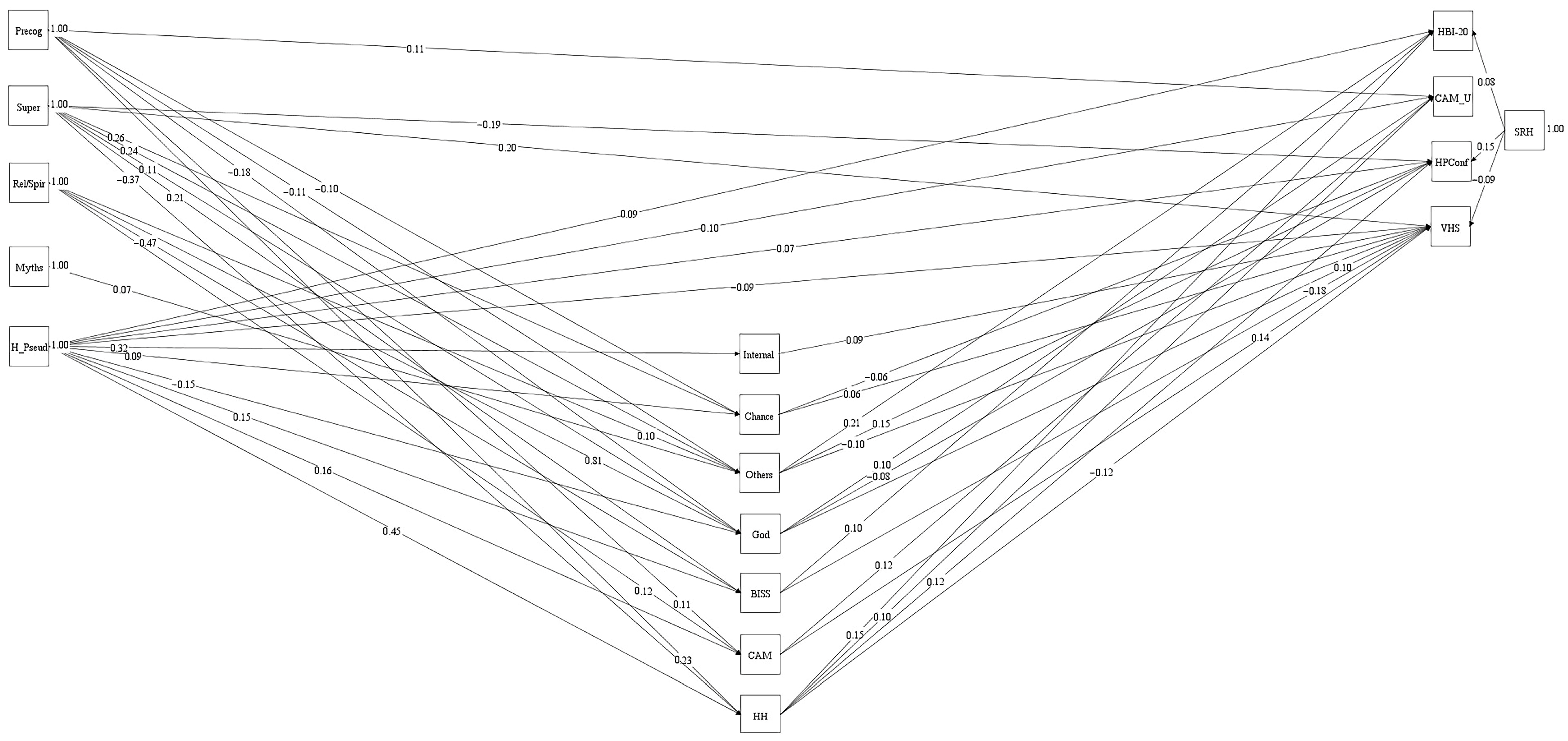
3.2. Path Analysis
4. Discussion
4.1. Theoretical and Practical Implications
4.2. Limitations
4.3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aharon, A. A., Nehama, H., Rishpon, S., & Baron-Epel, O. (2018). A path analysis model suggesting the association between health locus of control and compliance with childhood vaccinations. Human Vaccines & Immunotherapeutics, 14(7), 1618–1625. [Google Scholar] [CrossRef]
- Aktaş, B., & Bakan, A. B. (2021). Relationship between attitudes about medication adherence and complementary and alternative medicines in elderly individuals with chronic diseases. Alternative Therapies in Health & Medicine, 27(4), 14–18. [Google Scholar]
- Asparouhov, T., & Muthén, B. (2010). Computing the strictly positive Satorra-Bentler chi-square test in Mplus. Mplus Web Notes, 12, 1–12. [Google Scholar]
- Attwell, K., Ward, P. R., Meyer, S. B., Rokkas, P. J., & Leask, J. (2018). “Do-it-yourself”: Vaccine rejection and complementary and alternative medicine (CAM). Social Science and Medicine, 196, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Bauml, J. M., Chokshi, S., Schapira, M. M., Im, E. O., Li, S. Q., Langer, C. J., Ibrahim, S. A., & Mao, J. J. (2015). Do attitudes and beliefs regarding complementary and alternative medicine impact its use among patients with cancer? A cross-sectional survey. Cancer, 121(14), 2431–2438. [Google Scholar] [CrossRef] [PubMed]
- Bishop, F. L., Yardley, L., & Lewith, G. T. (2007). A systematic review of beliefs involved in the use of complementary and alternative medicine. Journal of Health Psychology, 12(6), 851–867. [Google Scholar] [CrossRef]
- Bollen, K. A., & Pearl, J. (2013). Eight myths about causality and structural equation modeling. In S. L. Morgan (Ed.), Handbook of causal analysis for social research (pp. 301–328). Springer. [Google Scholar]
- Boyd, J. M., & Wilcox, S. (2020). Examining the relationship between health locus of control and god locus of health control: Is god an internal or external source? Journal of Health Psychology, 25(7), 931–940. [Google Scholar] [CrossRef]
- Brincks, A. M., Feaster, D. J., Burns, M. J., & Mitrani, V. B. (2010). The influence of health locus of control on the patient–provider relationship. Psychology, Health & Medicine, 15(6), 720–728. [Google Scholar] [CrossRef]
- Bryden, G. M., & Browne, M. (2016). Development and evaluation of the RI-CAM-Q as a brief summative measure of CAM utilisation. Complementary Therapies in Medicine, 27, 82–86. [Google Scholar] [CrossRef]
- Buchbinder, R., & McGrail, K. (2005). Beliefs and use of complementary and alternative medicine among patients with chronic illness. Psychology and Health, 20(2), 233–244. [Google Scholar]
- Cheng, C., Cheung, M. W. L., & Lo, B. C. (2016). Relationship of health locus of control with specific health behaviours and global health appraisal: A meta-analysis and effects of moderators. Health Psychology Review, 10(4), 460–477. [Google Scholar] [CrossRef]
- Clarke, A., & van Ameringen, M. (2015). The relationship between health anxiety and treatment-seeking behaviors. Journal of Health Psychology, 20(6), 689–697. [Google Scholar]
- Dagnall, N., Denovan, A., Drinkwater, K., Parker, A., & Clough, P. (2017). Statistical bias and endorsement of conspiracy theories. Applied Cognitive Psychology, 31(4), 368–378. [Google Scholar] [CrossRef]
- Dagnall, N., Denovan, A., Drinkwater, K. G., & Escolà-Gascón, Á. (2022). Paranormal belief and well-being: The moderating roles of transliminality and psychopathology-related facets. Frontiers in Psychology, 13, 915860. [Google Scholar] [CrossRef] [PubMed]
- Dagnall, N., Denovan, A., Drinkwater, K. G., & Parker, A. (2019). An evaluation of the belief in science scale. Frontiers in Psychology, 10, 861. [Google Scholar] [CrossRef] [PubMed]
- Dagnall, N., Drinkwater, K., Denovan, A., Parker, A., & Rowley, K. (2016). Misperception of chance, conjunction, framing effects and belief in the paranormal: A further evaluation. Applied Cognitive Psychology, 30(3), 409–419. [Google Scholar] [CrossRef]
- Dagnall, N., Drinkwater, K., Parker, A., & Rowley, K. (2014). Misperception of chance, conjunction, belief in the paranormal and reality testing: A reappraisal. Applied Cognitive Psychology, 28(5), 711–719. [Google Scholar] [CrossRef]
- Dagnall, N., Drinkwater, K. G., Denovan, A., & Gascón, A. E. (2024). Variations in positive well-being as a function of the interaction between paranormal belief and schizotypy. Frontiers in Psychology, 15, 1396485. [Google Scholar] [CrossRef]
- Dagnall, N., Parker, A., Munley, G., & Drinkwater, K. (2010). Common paranormal belief dimensions. Journal of Scientific Exploration, 24(3), 477–494. [Google Scholar]
- Denovan, A., Dagnall, N., & Drinkwater, K. G. (2024a). The illusory health beliefs scale: Validation using exploratory structural equation modelling and multidimensional Rasch analysis. Frontiers in Psychology, 16, 1491759. [Google Scholar] [CrossRef]
- Denovan, A., Dagnall, N., & Drinkwater, K. G. (2024b). The paranormal health beliefs scale: An evaluation using cognitive interviewing. Frontiers in Psychology, 15, 1306372. [Google Scholar] [CrossRef] [PubMed]
- Denovan, A., Dagnall, N., Drinkwater, K. G., & Gascón, À. E. (2024c). The illusory health beliefs scale: Preliminary validation using exploratory factor and Rasch analysis. Frontiers in Psychology, 16, 1408734. [Google Scholar] [CrossRef]
- Donizzetti, A. R. (2018). Paranormal health beliefs: Relations between social dominance orientation and mental illness. The Open Psychology Journal, 11(1), 35–45. [Google Scholar] [CrossRef]
- Donizzetti, A. R., & Petrillo, G. (2017). Validation of the paranormal health beliefs scale for adults. Health Psychology Open, 4(2), 1–8. [Google Scholar] [CrossRef] [PubMed]
- Drinkwater, K. G., Denovan, A., & Dagnall, N. (2024). Paranormal belief, psychopathological symptoms, and well-being: Latent profile analysis and longitudinal assessment of relationships. PLoS ONE, 19(3), e0297403. [Google Scholar] [CrossRef] [PubMed]
- Drinkwater, K. G., Denovan, A., Dagnall, N., & Parker, A. (2018). The Australian sheep-goat scale: An evaluation of factor structure and convergent validity. Frontiers in Psychology, 9, 1594. [Google Scholar] [CrossRef]
- Epstein, S., Pacini, R., Denes-Raj, V., & Heier, H. (1996). Individual differences in intuitive–experiential and analytical–rational thinking styles. Journal of Personality and Social Psychology, 71(2), 390–405. [Google Scholar] [CrossRef]
- Farias, M., Newheiser, A. K., Kahane, G., & de Toledo, Z. (2013). Scientific faith: Belief in science increases in the face of stress and existential anxiety. Journal of Experimental Social Psychology, 49(6), 1210–1213. [Google Scholar] [CrossRef]
- Fasce, A., & Picó, A. (2019). Conceptual foundations and validation of the pseudoscientific belief scale. Applied Cognitive Psychology, 33(4), 617–628. [Google Scholar] [CrossRef]
- Galbraith, N., Moss, T., Galbraith, V., & Purewal, S. (2018). A systematic review of the traits and cognitions associated with use of and belief in complementary and alternative medicine (CAM). Psychology, Health & Medicine, 23(7), 854–869. [Google Scholar] [CrossRef]
- Gayatri, D., Efremov, L., Kantelhardt, E. J., & Mikolajczyk, R. (2021). Quality of life of cancer patients at palliative care units in developing countries: Systematic review of the published literature. Quality of Life Research, 30, 315–343. [Google Scholar] [CrossRef] [PubMed]
- Gignac, G. E., & Szodorai, E. T. (2016). Effect size guidelines for individual differences researchers. Personality and Individual Differences, 102, 74–78. [Google Scholar] [CrossRef]
- Goode, E. (2000). Paranoia and the role of the media in the cultivation of beliefs in health risks. Social Science & Medicine, 51(8), 1183–1194. [Google Scholar]
- Grotz, M., Hapke, U., Lampert, T., & Baumeister, H. (2011). Health locus of control and health behaviour: Results from a nationally representative survey. Psychology, Health and Medicine, 16(2), 129–140. [Google Scholar] [CrossRef] [PubMed]
- Hair, J. F., Black, W. C., Babin, B. J., Anderson, R. E., & Tatham, R. L. (Eds.). (2010). Multivariate data analysis (7th ed.). Pearson. [Google Scholar]
- Horne, R., & Weinman, J. (2002). Self-regulation and self-management in chronic illness. In A. Baum, & J. Singer (Eds.), Handbook of psychology and health (Vol. 3, pp. 61–91). Psychology Press. [Google Scholar]
- Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar] [CrossRef]
- Hyland, M. E., Lewith, G. T., & Westoby, C. (2003). Developing a measure of attitudes: The holistic complementary and alternative medicine questionnaire. Complementary Therapies in Medicine, 11(1), 33–38. [Google Scholar] [CrossRef]
- Ipsos. (2024, July 11). GP patient survey 2024. Ipsos. Available online: https://www.ipsos.com/en-uk/2024-gp-patient-survey-results-released (accessed on 9 January 2025).
- Irwin, H. J. (1993). Belief in the paranormal: A review of the empirical literature. Journal of the American Society for Psychical Research, 87(1), 1–39. [Google Scholar]
- Irwin, H. J. (2000). Belief in the paranormal and a sense of control over life. European Journal of Parapsychology, 15, 68–78. [Google Scholar]
- Irwin, H. J. (2009). The psychology of paranormal belief: A researcher’s handbook. University of Hertfordshire Press. [Google Scholar]
- Irwin, H. J., Dagnall, N., & Drinkwater, K. (2012a). Paranormal belief and biases in reasoning underlying the formation of delusions. Australian Journal of Parapsychology, 12(1), 7–21. [Google Scholar]
- Irwin, H. J., Dagnall, N., & Drinkwater, K. (2012b). Paranormal beliefs and cognitive processes underlying the formation of delusions. Australian Journal of Parapsychology, 12(2), 107–126. [Google Scholar]
- Irwin, H. J., Dagnall, N., & Drinkwater, K. (2013). Parapsychological experience as anomalous experience plus paranormal attribution: A questionnaire based on a new approach to measurement. Journal of Parapsychology, 77(1), 39–53. [Google Scholar]
- Kees, J., Berry, C., Burton, S., & Sheehan, K. (2017). An analysis of data quality: Professional panels, student subject pools, and Amazon’s mechanical turk. Journal of Advertising, 46(1), 141–155. [Google Scholar] [CrossRef]
- Kouvari, K., Hadjikou, A., Heraclidou, I., & Heraclides, A. (2022). Health literacy, consciousness, and locus of control in relation to vaccine hesitancy and refusal. European Journal of Public Health, 32(Suppl. S3), ckac129.640. [Google Scholar] [CrossRef]
- Krist, A. H., Tong, S. T., Aycock, R. A., & Longo, D. R. (2017). Engaging patients in decision-making and behavior change to promote prevention. Information Services & Use, 37(2), 105–122. [Google Scholar] [CrossRef]
- Lange, R., Ross, R. M., Dagnall, N., Irwin, H. J., Houran, J., & Drinkwater, K. (2019). Anomalous experiences and paranormal attributions: Psychometric challenges in studying their measurement and relationship. Psychology of Consciousness: Theory, Research, and Practice, 6(4), 346–358. [Google Scholar] [CrossRef]
- Lazarus, R. S. (1999). Stress and emotion: A new synthesis. Springer Publishing Company. [Google Scholar]
- Levant, R. F., Wimer, D. J., & Williams, C. M. (2011). An evaluation of the Health Behavior Inventory−20 (HBI−20) and its relationships to masculinity and attitudes towards seeking psychological help among college men. Psychology of Men & Masculinity, 12(1), 26. [Google Scholar] [CrossRef]
- Li, B., Forbes, T. L., & Byrne, J. (2018). Integrative medicine or infiltrative pseudoscience? The Surgeon, 16(5), 271–277. [Google Scholar] [CrossRef]
- Lie, D., & Boker, J. (2004). Development and validation of the CAM Health Belief Questionnaire (CHBQ) and CAM use and attitudes amongst medical students. BMC Medical Education, 4(1), 2. [Google Scholar] [CrossRef]
- Lobato, E. J. C., & Zimmerman, C. (2018). The psychology of (pseudo)science: Cognitive, social, and cultural factors. In A. B. Kaufman, & J. C. Kaufman (Eds.), Pseudoscience: The conspiracy against science (pp. 21–43). Boston Review. [Google Scholar] [CrossRef]
- Luyten, J., & Beutels, P. (2016). The social value of vaccination programs: Beyond cost-effectiveness. Health Affairs, 35(2), 212–218. [Google Scholar] [CrossRef]
- Luyten, J., Bruyneel, L., & Van Hoek, A. J. (2019). Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine, 37(18), 2494–2501. [Google Scholar] [CrossRef]
- Makridakis, S., & Moleskis, A. (2015). The costs and benefits of positive illusions. Frontiers in Psychology, 6, 859. [Google Scholar] [CrossRef] [PubMed]
- Marr, J., & Wilcox, S. (2015). Self-efficacy and social support mediate the relationship between internal health locus of control and health behaviors in college students. American Journal of Health Education, 46(3), 122–131. [Google Scholar] [CrossRef]
- Meng, Q., Xie, Z., & Zhang, T. (2014). A single-item self-rated health measure correlates with objective health status in the elderly: A survey in suburban Beijing. Frontiers In Public Health, 2, 27. [Google Scholar] [CrossRef] [PubMed]
- Mjaess, G., Aoun, F., Kazzi, H., Karam, A., Albisinni, S., & Roumeguère, T. (2021). Myths, superstitions, and popular beliefs: Do they still impact our practice? Annals of Surgery, 274(6), e641–e642. [Google Scholar] [CrossRef]
- Moshki, M., Ghofranipour, F., Hajizadeh, E., & Azadfallah, P. (2007). Validity and reliability of the multidimensional health locus of control scale for college students. BMC Public Health, 7, 295. [Google Scholar] [CrossRef]
- Mozafari, S., Yang, A., & Talaei-Khoei, J. (2024). Health locus of control and medical behavioral interventions: Systematic review and recommendations. Interactive Journal of Medical Research, 13(1), e52287. [Google Scholar] [CrossRef]
- Norman, P., Bennett, P., Smith, C., & Murphy, S. (1998). Health locus of control and health behaviour. Journal of Health Psychology, 3(2), 171–180. [Google Scholar] [CrossRef]
- Olagoke, A. A., Olagoke, O. O., & Hughes, A. M. (2021). Intention to vaccinate against the novel 2019 coronavirus disease: The role of health locus of control and religiosity. Journal of Religion and Health, 60, 65–80. [Google Scholar] [CrossRef]
- Petrillo, G., & Donizzetti, A. R. (2012). Credenze illusorie sulla salute in adolescenza: Validazione di uno strumento di rilevazione. Giornale Italiano di Psicologia, 39(2), 407–434. [Google Scholar] [CrossRef]
- Pettersen, S., & Olsen, R. V. (2007). Exploring predictors of health sciences students’ attitudes towards complementary-alternative medicine. Advances in Health Sciences Education, 12(1), 35–53. [Google Scholar] [CrossRef]
- Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [Google Scholar] [CrossRef]
- Rodriguez, A., Delbourgo Patton, C., & Stephenson-Hunter, C. (2023). Impact of locus of control on patient–provider communication: A systematic review. Journal of Health Communication, 28(3), 190–204. [Google Scholar] [CrossRef]
- Schumaker, J. F. (1990). Wings of illusion: The origin, nature, and future of paranormal belief. Prometheus Books. [Google Scholar]
- Shapiro, G. K., Tatar, O., Dube, E., Amsel, R., Knauper, B., Naz, A., Perez, S., & Rosberger, Z. (2018). The vaccine hesitancy scale: Psychometric properties and validation. Vaccine, 36(5), 660–667. [Google Scholar] [CrossRef] [PubMed]
- Stosic, M. D., Helwig, S., & Ruben, M. A. (2021). Greater belief in science predicts mask-wearing behavior during COVID-19. Personality and Individual Differences, 176, 110769. [Google Scholar] [CrossRef] [PubMed]
- Tobbia, I., Bella, A., Safrany, S., Greengrass, C., Al Banna, A., Mann-Isah, N., & Walsh, P. (2019). Debating the merits and dangers of complementary and alternative medicine. Bahrain Medical Bulletin, 41(2), 65–66. [Google Scholar]
- Torres, M. N., Barberia, I., & Rodríguez-Ferreiro, J. (2020). Causal illusion as a cognitive basis of pseudoscientific beliefs. British Journal of Psychology, 111(4), 840–852. [Google Scholar] [CrossRef]
- Unterrassner, L., Wyss, T. A., Wotruba, D., Ajdacic-Gross, V., Haker, H., & Rössler, W. (2017). Psychotic-like experiences at the healthy end of the psychosis continuum. Frontiers in Psychology, 8, 775. [Google Scholar] [CrossRef]
- Van den Bulck, J., & Custers, K. (2010). Belief in complementary and alternative medicine is related to age and paranormal beliefs in adults. European Journal of Public Health, 20(2), 227–230. [Google Scholar] [CrossRef]
- Wallston, B. S., Wallston, K. A., Kaplan, G. D., & Maides, S. A. (1976). Development and validation of the Health Locus of Control (HLC) scale. Journal of Consulting and Clinical Psychology, 44(4), 580–585. [Google Scholar] [CrossRef]
- Wallston, K. A. (1992). Hocus-pocus, the focus isn’t strictly on locus: Rotter’s social learning theory modified for health. Cognitive Therapy and Research, 16(2), 183–199. [Google Scholar] [CrossRef]
- Wallston, K. A., Malcarne, V. L., Flores, L., Hansdottir, I., Smith, C. A., Stein, M. J., Weisman, M. H., & Clements, P. J. (1999). Does god determine your health? The god locus of health control scale. Cognitive Therapy and Research, 23(2), 131–142. [Google Scholar] [CrossRef]
- Wallston, K. A., Strudler Wallston, B., & DeVellis, R. (1978). Development of the Multidimensional Health Locus of Control (MHLC) scales. Health Education Monographs, 6(1), 160–170. [Google Scholar] [CrossRef]
- Ward, J. K., Gauna, F., Deml, M. J., MacKendrick, N., & Peretti-Watel, P. (2023). Diversity of attitudes towards complementary and alternative medicine (CAM) and vaccines: A representative cross-sectional study in France. Social Science & Medicine, 328, 115952. [Google Scholar] [CrossRef]
- Williams, C., Denovan, A., Drinkwater, K., & Dagnall, N. (2022). Thinking style and paranormal belief: The role of cognitive biases. Imagination, Cognition and Personality, 41(3), 274–298. [Google Scholar] [CrossRef]
- Wilson, J. A. (2018). Reducing pseudoscientific and paranormal beliefs in university students through a course in science and critical thinking. Science & Education, 27, 183–210. [Google Scholar] [CrossRef]
- Yarritu, I., Matute, H., & Luque, D. (2015). The dark side of cognitive illusions: When an illusory belief interferes with the acquisition of evidence-based knowledge. British Journal of Psychology, 106(4), 597–608. [Google Scholar] [CrossRef]
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time 1 | |||||||||||||||||||
| 1 Precognitive | 13.38 | 6.06 | 0.81 ** | 0.80 ** | 0.56 ** | 0.54 ** | 0.23 ** | 0.17 ** | 0.22 ** | 0.49 ** | −0.12 ** | 0.26 ** | 0.19 ** | 0.09 ** | 0.34 ** | −0.16 ** | 0.29 ** | 0.02 | |
| 2 Superstition | 17.22 | 7.84 | 0.79 ** | 0.62 ** | 0.45 ** | 0.20 ** | 0.23 ** | 0.29 ** | 0.54 ** | −0.08 ** | 0.22 ** | 0.04 | 0.10 ** | 0.32 ** | −0.22 ** | 0.33 ** | −0.02 | ||
| 3 Religious Belief | 21.54 | 9.95 | 0.59 ** | 0.51 ** | 0.22 ** | 0.20 ** | 0.27 ** | 0.68 ** | −0.21 ** | 0.24 ** | 0.15 ** | 0.09 ** | 0.33 ** | −0.15 ** | 0.29 ** | 0.02 | |||
| 4 Health Myths | 15.61 | 4.72 | 0.55 ** | 0.23 ** | 0.19 ** | 0.25 ** | 0.40 ** | −0.02 | 0.14 ** | 0.16 ** | 0.09 ** | 0.24 ** | −0.11 ** | 0.20 ** | 0.02 | ||||
| 5 Health Pseudoscience | 31.78 | 7.45 | 0.33 ** | 0.17 ** | 0.18 ** | 0.22 ** | 0.02 | 0.24 ** | 0.41 ** | 0.19 ** | 0.31 ** | 0.01 | 0.06 * | 0.08 ** | |||||
| Time 2 | |||||||||||||||||||
| 6 InternalHLOC | 23.35 | 4.60 | 0.31 ** | 0.36 ** | 0.22 ** | 0.21 ** | −0.06 * | 0.47 ** | 0.20 ** | 0.17 ** | 0.04 | 0.01 | 0.21 ** | ||||||
| 7 ChanceHLOC | 21.37 | 4.85 | 0.41 ** | 0.30 ** | 0.24 ** | −0.17 ** | 0.30 ** | 0.13 ** | 0.10 ** | −0.03 | 0.02 | 0.01 | |||||||
| 8 OthersHLOC | 19.44 | 5.48 | 0.38 ** | 0.30 ** | −0.18 ** | 0.21 ** | 0.27 ** | 0.15 ** | 0.07 * | −0.05 * | 0.01 | ||||||||
| 9 GodHLOC | 13.14 | 8.27 | −0.13 ** | 0.12 ** | 0.05 | 0.08 ** | 0.25 ** | −0.15 ** | 0.26 ** | 0.03 | |||||||||
| 10 Belief in Science | 40.97 | 10.41 | −0.43 ** | 0.28 ** | 0.20 ** | 0.01 | 0.15 ** | −0.32 ** | 0.12 ** | ||||||||||
| 11 CAM | 25.45 | 6.17 | −0.20 ** | −0.06 * | 0.17 ** | −0.14 ** | 0.30 ** | −0.04 | |||||||||||
| 12 Holistic Health | 22.05 | 4.37 | 0.24 ** | 0.17 ** | 0.16 ** | −0.18 ** | 0.16 ** | ||||||||||||
| Time 3 | |||||||||||||||||||
| 13 HBI−20 | 79.34 | 15.97 | 0.27 ** | 0.20 ** | −0.21 ** | 0.12 ** | |||||||||||||
| 14 CAM_USE | 3.10 | 3.51 | −0.02 | 0.10 ** | 0.04 | ||||||||||||||
| 15 HPConf | 2.55 | 0.62 | −0.38 ** | 0.17 ** | |||||||||||||||
| 16 Vaccine Hesitancy | 22.18 | 8.07 | −0.12 ** | ||||||||||||||||
| 17 SRH | 68.03 | 20.60 |
| HBI-20 | CAM_USE | HPConf | VHS | |
|---|---|---|---|---|
| Indirect path | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) |
| Precognitive > OthersHLOC | 0.02 * (0.01, 0.04) | - | 0.02 * (0.01, 0.03) | - |
| Precognitive > GodHLOC | - | −0.02 * (−0.03, −0.01) | 0.01 * (0.01, 0.03) | −0.02 * (−0.03, −0.01) |
| Precognitive > CAM | - | 0.01 * (0.01, 0.03) | - | 0.02 * (0.01, 0.03) |
| Precognitive > HH | 0.04 ** (0.02, 0.05) | 0.02 * (0.01, 0.04) | 0.03 * (0.01, 0.04) | −0.03 * (−0.04, −0.01) |
| Superstition > ChanceHLOC | - | - | −0.02 * (−0.03, −0.01) | 0.02 * (0.01, 0.03) |
| Superstition > OthersHLOC | 0.05 ** (0.03, 0.08) | - | 0.04 ** (0.02, 0.06) | −0.03 * (−0.04, −0.01) |
| Superstition > GodHLOC | - | −0.01 * (−0.02, −0.01) | - | −0.01 * (−0.02, −0.01) |
| Superstition > BIS | 0.02 * (0.01, 0.04) | - | - | −0.04 ** (−0.05, −0.02) |
| Superstition > HH | 0.06 ** (0.03, 0.07) | 0.04 * (0.01, 0.06) | 0.04 ** (0.02, 0.06) | −0.04 ** (−0.06, −0.02) |
| Health Pseudoscience > InternalHLOC | - | - | - | −0.03 * (−0.04, −0.01) |
| Health Pseudoscience > GodHLOC | - | −0.02 * (−0.03, −0.01) | 0.01* (0.01, 0.02) | −0.02 * (−0.03, −0.01) |
| Health Pseudoscience > BIS | 0.02 * (0.01, 0.03) | - | - | −0.03 ** (−0.04, −0.02) |
| Health Pseudoscience > CAM | - | 0.02 ** (0.01, 0.03) | - | 0.02 ** (0.01, 0.04) |
| Health Pseudoscience > HH | 0.07 ** (0.04, 0.09) | 0.04 * (0.02, 0.07) | 0.05 ** (0.03, 0.08) | −0.05 ** (−0.08, −0.03) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denovan, A.; Dagnall, N.; Drinkwater, K.G. The Relationship Between Illusory Health Beliefs, Recommended Health Behaviours, and Complementary and Alternative Medicine: An Investigation Across Multiple Time Points. Behav. Sci. 2025, 15, 614. https://doi.org/10.3390/bs15050614
Denovan A, Dagnall N, Drinkwater KG. The Relationship Between Illusory Health Beliefs, Recommended Health Behaviours, and Complementary and Alternative Medicine: An Investigation Across Multiple Time Points. Behavioral Sciences. 2025; 15(5):614. https://doi.org/10.3390/bs15050614
Chicago/Turabian StyleDenovan, Andrew, Neil Dagnall, and Kenneth G. Drinkwater. 2025. "The Relationship Between Illusory Health Beliefs, Recommended Health Behaviours, and Complementary and Alternative Medicine: An Investigation Across Multiple Time Points" Behavioral Sciences 15, no. 5: 614. https://doi.org/10.3390/bs15050614
APA StyleDenovan, A., Dagnall, N., & Drinkwater, K. G. (2025). The Relationship Between Illusory Health Beliefs, Recommended Health Behaviours, and Complementary and Alternative Medicine: An Investigation Across Multiple Time Points. Behavioral Sciences, 15(5), 614. https://doi.org/10.3390/bs15050614






