The Impact of Sensory Reactivity and Oral Praxis on Feeding Participation in Children with Autism (SemAlTea Study)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Variables and Evaluation Tools
2.1.1. Socio-Demographic Variables
2.1.2. Classification of Autism Spectrum Disorder
2.1.3. Feeding Participation
2.1.4. Sensorimotor Factors
2.1.5. Anthropometry
2.1.6. Caregiver Stress
2.2. Sample Size Calculation
2.3. Statistical Methods
3. Results
3.1. Participation in Feeding
3.2. Oral Praxis
3.3. Sensory Reactivity (SP-2)
3.4. Anthropometry
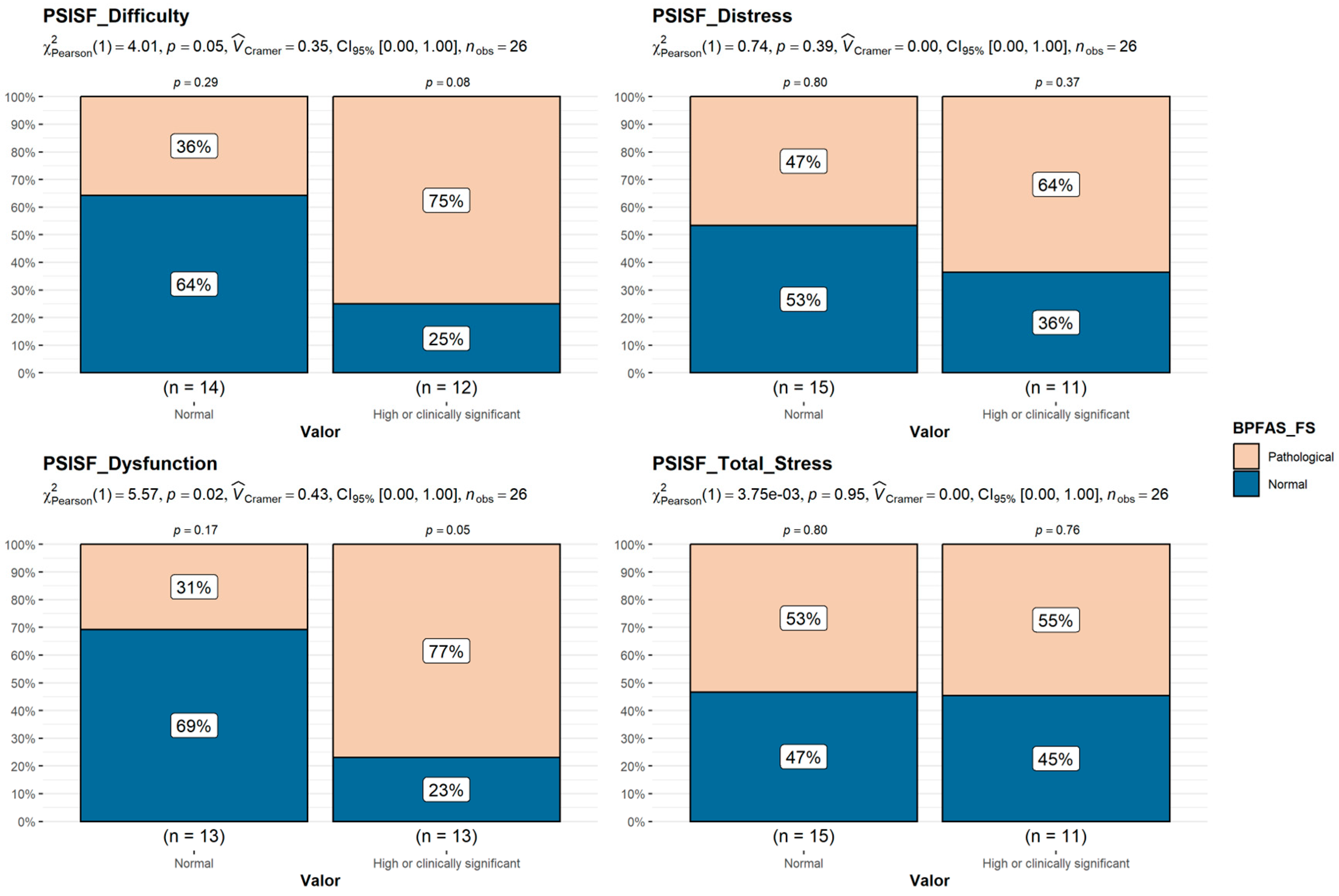
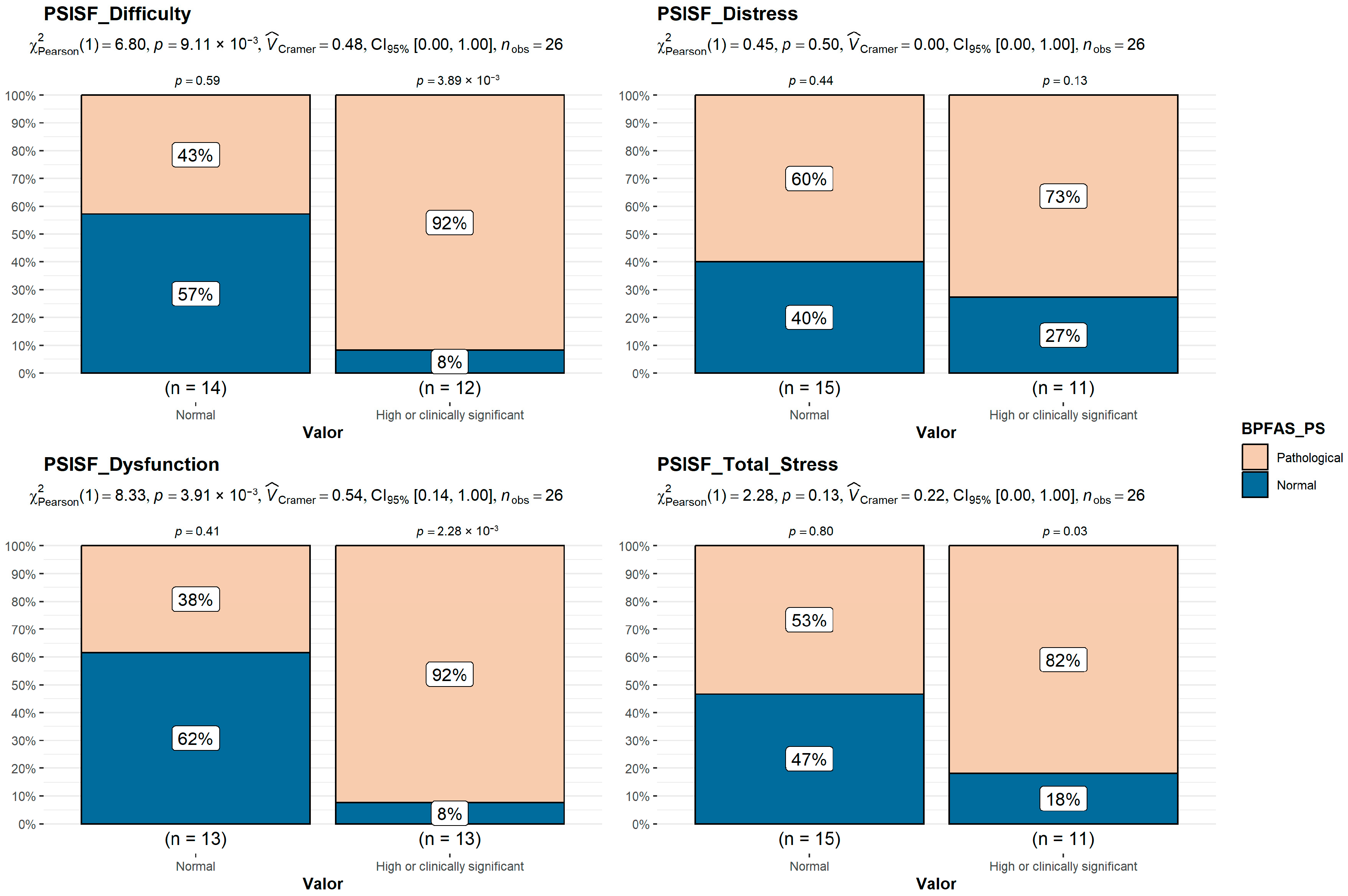
3.5. Caregiver Stress (PSI-4-SF)
4. Discussion
4.1. Limitations
4.2. Implications for Therapy Interventions
- Occupational therapy interventions for children with ASD who experience difficulties participating in feeding and mealtimes, that consider sensory integration problems of the tactile and oral systems, can be useful for improving the processing of these stimuli and the ability of the child with ASD to touch, explore, and eat food.
- Improvements in the underlying sensory factors and basic skills linked to feeding can lead to improvements in eating behaviors and mealtime participation, thus reducing the risk of suffering from an eating disorder, reducing caregiver stress, and improving the parent–child relationship.
- Larger studies are needed to confirm our results. Until then, if practitioners choose to implement this approach clinically, they need to carefully document treatment content, client responses to the treatment, and changes in client functioning (or occupational engagement) from the start to the termination of treatment.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASD | Autism Spectrum Disorder |
| FPPs | Feeding Participation Problems |
| BPFAS | Behavioral Pediatrics Feeding Assessment Scale |
| FS | Frequency Score |
| PS | Problem Score |
| SP | Sensory Profile 2 |
| OPr | Oral Praxis |
| SIPT | Sensory Integration and Praxis Tests |
| PSI-4-SF | Parental Stress Index–Short Form |
| BMI | Body Mass Index |
| ROC | Receiver Operating Characteristic |
| ESeC | European Socio-Economic Classification |
References
- Abidin, R. R. (2012). Parenting stress index: PSI-4. Professional manual. PAR. [Google Scholar]
- Allen, S. L., Smith, I. M., Duku, E., Vaillancourt, T., Szatmari, P., Bryson, S., Fombonne, E., Volden, J., Waddell, C., Zwaigenbaum, L., Roberts, W., Mirenda, P., Bennett, T., Elsabbagh, M., & Georgiades, S. (2018). Behavioral pediatrics feeding assessment scale in young children with autism spectrum disorder: Psychometrics and associations with child and parent variables. Journal of Pediatric Psychology, 40(6), 581–590. [Google Scholar] [CrossRef]
- American Psychiatric Association. (2013). Manual diagnóstico y estadístico de los trastornos mentales (DSM-5). Available online: https://biblioteca.inci.gov.co/handle/inci/18445 (accessed on 25 July 2025).
- Ashley, K., Steinfeld, M. B., Young, G. S., & Ozonoff, S. (2020). Onset, trajectory, and pattern of feeding difficulties in toddlers later diagnosed with autism. Journal of Developmental and Behavioral Pediatrics, 41(3), 165–171. [Google Scholar] [CrossRef]
- Ayres, A. J. (1989). Sensory Integration and Praxis Test. In F. R. Volkmar (Ed.), Encyclopedia of autism spectrum disorders (pp. 2791–2795). Springer. [Google Scholar] [CrossRef]
- Baranek, G. T., Little, L. M., Parham, L. D., Ausderau, K. K., & Sabatos-DeVito, M. G. (2014). Sensory features in autism spectrum disorders. In Handbook of autism and pervasive developmental disorders (4th ed., pp. 378–407). John Wiley & Sons, Inc. [Google Scholar] [CrossRef]
- Baraskewich, J., von Ranson, K. M., McCrimmon, A., & McMorris, C. A. (2021). Feeding and eating problems in children and adolescents with autism: A scoping review. Autism, 25(6), 1505–1519. [Google Scholar] [CrossRef] [PubMed]
- Beaudry-Bellefeuille, I., Pomoni, M., Welch, A., Moriyon-Iglesias, T., Suarez-Gonzalez, M., & Ramos-Polo, E. (2021). Multidisciplinary approach to assessment and intervention of feeding problems in children with autism spectrum disorders: A clinical perspective. Irish Journal of Occupational Therapy, 49(2), 77–83. [Google Scholar] [CrossRef]
- Cermak, S. A., Curtin, C., & Bandini, L. G. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110(2), 238–246. [Google Scholar] [CrossRef]
- Chistol, L. T., Bandini, L. G., Must, A., Phillips, S., Cermak, S. A., & Curtin, C. (2018). Sensory sensitivity and food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(2), 583–591. [Google Scholar] [CrossRef]
- Crist, W., & Napier-Phillips, A. (2001). Mealtime behaviors of young children: A comparison of normative and clinical data. Journal of Developmental and Behavioral Pediatrics, 22(5), 279–286. [Google Scholar] [CrossRef] [PubMed]
- Curtin, C., Hubbard, K., Anderson, S. E., Mick, E., Must, A., & Bandini, L. G. (2015). Food selectivity, mealtime behavior problems, spousal stress, and family food choices in children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(10), 3308–3315. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M., Garza, C., Onyango, A. W., & Martorell, R. (2006). WHO child growth standards Acta Pediátrica (supplement 450, pp. 76–85). WHO. [Google Scholar]
- De Onis, M., Onyango, A. W., Borghi, E., Siyam, A., Nishida, C., & Siekmann, J. (2007). Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization, 85(9), 660–667. [Google Scholar] [CrossRef]
- Dunn, W. (1999). Sensory profile. User’s manual. Psychological Corp. [Google Scholar]
- Gándara-Gafo, B., Beaudry-Bellefeuille, I., Mailloux, Z., Moriyón, T., Parham, L. D., Riego, S. S., Serrada-Tejeda, S., Roley, S. S., Toledo, P., & Schaaf, R. C. (2021). Cultural adaptation of the evaluation in ayres sensory Integration® (EASI) for spanish-speaking populations. The American Journal of Occupational Therapy, 75(5), 7505205090. [Google Scholar] [CrossRef]
- Goday, P. S., Huh, S. Y., Silverman, A., Lukens, C. T., Dodrill, P., Cohen, S. S., Delaney, A. L., Feuling, M. B., Noel, R. J., Gisel, E., Kenzer, A., Kessler, D. B., Kraus de Camargo, O., Browne, J., & Phalen, J. A. (2019). Pediatric feeding disorder: Consensus definition and conceptual framework. Journal of Pediatric Gastroenterology and Nutrition, 68(1), 124–129. [Google Scholar] [CrossRef]
- Harrison, E., & Rose, D. (2006). The European socio-economic classification (ESeC) user guide. Institute for Social and Economic Research, University of Essex. [Google Scholar]
- Ismael, N., Lawson, L. M., & Hartwell, J. (2018). Relationship between sensory processing and participation in daily occupations for children with autism spectrum disorder: A systematic review of studies that used Dunn’s sensory processing framework. The American Journal of Occupational Therapy, 72(3), 7203205030p1–7203205030p9. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y. Q., Teo, C. M., Tan, M. L., Aw, M. M., Chan, Y. H., & Chong, S. C. (2022). Feeding difficulties in Asian children with autism spectrum disorder. Pediatrics and Neonatology, 63(1), 48–56. [Google Scholar] [CrossRef]
- Kim, A.-R., Kwon, J.-Y., Yi, S.-H., & Kim, E.-H. (2021). Sensory based feeding intervention for toddlers with food refusal: A randomized controlled trial. Annals of Rehabilitation Medicine, 45(5), 393–400. [Google Scholar] [CrossRef]
- Kirby, A. V., Williams, K. L., Watson, L. R., Sideris, J., Bulluck, J., & Baranek, G. T. (2019). Sensory features and family functioning in families of children with autism and developmental disabilities: Longitudinal associations. The American Journal of Occupational Therapy, 73(2), 7302205040p1–7302205040p14. [Google Scholar] [CrossRef]
- Leader, G., Tuohy, E., Chen, J. L., Mannion, A., & Gilroy, S. P. (2020). Feeding problems, gastrointestinal symptoms, challenging behavior and sensory issues in children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(4), 1401–1410. [Google Scholar] [CrossRef]
- Maenner, M. J. (2020). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR. Surveillance Summaries, 69(4), 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mayes, S. D., & Zickgraf, H. (2019). Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Research in Autism Spectrum Disorders, 64, 76–83. [Google Scholar] [CrossRef]
- Posar, A., & Visconti, P. (2018). Sensory abnormalities in children with autism spectrum disorder. Jornal De Pediatria, 94(4), 342–350. [Google Scholar] [CrossRef] [PubMed]
- Reche-Olmedo, L., Torres-Collado, L., Compañ-Gabucio, L. M., & Garcia-de-la-Hera, M. (2021). The role of occupational therapy in managing food selectivity of children with autism spectrum disorder: A scoping review. Children, 8(11), 1024. [Google Scholar] [CrossRef]
- Roley, S., Mailloux, Z., Parham, L., Schaaf, R., Lane, C., & Cermak, S. (2015). Sensory integration and praxis patterns in children with autism. The American Journal of Occupational Therapy, 69, 6901220010p1–6901220010p8. [Google Scholar] [CrossRef]
- Romero-Ayuso, D., Labrador, C., & Pérez, C. (2016). Perfil sensorial 2. Winnie Dunn. Pearson. [Google Scholar] [CrossRef]
- Ros Arnal, I., Herrero Álvarez, M., Castell Miñana, M., López Ruzafa, E., Galera Martínez, R., & Moráis López, A. (2011). Valoración sistematizada del estado nutricional. Acta Pediatrica, 69(4), 165–172. [Google Scholar]
- Schulz, S. E., & Stevenson, R. A. (2019). Sensory hypersensitivity predicts repetitive behaviours in autistic and typically-developing children. Autism: The International Journal of Research and Practice, 23(4), 1028–1041. [Google Scholar] [CrossRef] [PubMed]
- Serra Majem, L., Aranceta Bartina, J., Pérez Rodrigo, C., Moreno Esteban, B., Tojo Sierra, R., & Delgado Rubio, A. (2002). Curvas de referencia para la tipificación ponderal. Población infantil y juvenil: Dossier de consenso. IM&C. [Google Scholar]
- Şahan, A. K., Öztürk, N., Demir, N., Karaduman, A. A., & Serel Arslan, S. (2021). A comparative analysis of chewing function and feeding behaviors in children with autism. Dysphagia, 36(6), 993–998. [Google Scholar] [CrossRef]
- Zeidan, J., Fombonne, E., Scorah, J., Ibrahim, A., Durkin, M. S., Saxena, S., Yusuf, A., Shih, A., & Elsabbagh, M. (2022). Global prevalence of autism: A systematic review update. Autism Research: Official Journal of the International Society for Autism Research, 15(5), 778–790. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M., You, Y., Chen, S., Li, L., Du, X., & Wang, Y. (2021). Effects of a web-based parent–child physical activity program on mental health in parents of children with ASD. International Journal of Environmental Research and Public Health, 18(24), 12913. [Google Scholar] [CrossRef]
- Zlomke, K., Rossetti, K., Murphy, J., Mallicoat, K., & Swingle, H. (2020). Feeding problems and maternal anxiety in children with autism spectrum disorder. Maternal and Child Health Journal, 24(10), 1278–1287. [Google Scholar] [CrossRef]
| BPFAS FS Pathological | BPFAS PS Pathological | |||||
|---|---|---|---|---|---|---|
| No | Yes | p | No | Yes | p | |
| SP-2 Sensitivity | 52.25 | 59.50 | 0.118 | 51.11 | 58.82 | 0.095 |
| SP-2 Avoidance | 48.50 | 55.07 | 0.193 | 45.33 | 55.59 | 0.013 * |
| SP-2 Oral | 24.58 | 34.29 | 0.006 * | 22.33 | 33.76 | 0.001 * |
| SP-2 Tactile | 23.17 | 28.64 | 0.118 | 21.89 | 28.35 | 0.051 |
| SP-2 Behavioral | 21.92 | 26.14 | 0.212 | 22.33 | 25.18 | 0.494 |
| BPFAS FS Pathological | BPFAS PS Pathological | |||||
|---|---|---|---|---|---|---|
| Mean No | Mean Yes | p | Mean No | Mean Yes | p | |
| SP-2 Sensitivity | 52.82 | 57.54 | 0.277 | 51.11 | 57.93 | 0.084 |
| SP-2 Avoidance | 48.09 | 53.154 | 0.252 | 45.33 | 54.13 | 0.021 * |
| SP-2 Oral | 23.91 | 33.54 | 0.007 * | 22.33 | 33.20 | 0.002 * |
| SP-2 Tactile | 24.18 | 28.15 | 0.277 | 21.89 | 29.00 | 0.03 * |
| SP-2 Behavioral | 22.73 | 25.00 | 0.494 | 22.33 | 24.03 | 0.238 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Martínez, I.; Galera-Martínez, R.; Aparicio-Mota, A.; López-Martín, J.M.; Beaudry-Bellefeuille, I.; Parrón-Carreño, T. The Impact of Sensory Reactivity and Oral Praxis on Feeding Participation in Children with Autism (SemAlTea Study). Behav. Sci. 2025, 15, 1577. https://doi.org/10.3390/bs15111577
López-Martínez I, Galera-Martínez R, Aparicio-Mota A, López-Martín JM, Beaudry-Bellefeuille I, Parrón-Carreño T. The Impact of Sensory Reactivity and Oral Praxis on Feeding Participation in Children with Autism (SemAlTea Study). Behavioral Sciences. 2025; 15(11):1577. https://doi.org/10.3390/bs15111577
Chicago/Turabian StyleLópez-Martínez, Inmaculada, Rafael Galera-Martínez, Adrián Aparicio-Mota, José María López-Martín, Isabelle Beaudry-Bellefeuille, and Tesifón Parrón-Carreño. 2025. "The Impact of Sensory Reactivity and Oral Praxis on Feeding Participation in Children with Autism (SemAlTea Study)" Behavioral Sciences 15, no. 11: 1577. https://doi.org/10.3390/bs15111577
APA StyleLópez-Martínez, I., Galera-Martínez, R., Aparicio-Mota, A., López-Martín, J. M., Beaudry-Bellefeuille, I., & Parrón-Carreño, T. (2025). The Impact of Sensory Reactivity and Oral Praxis on Feeding Participation in Children with Autism (SemAlTea Study). Behavioral Sciences, 15(11), 1577. https://doi.org/10.3390/bs15111577






