Impact of Inpatient Treatment for Obesity in Patients with Comorbid Psychiatric Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Therapeutic Interventions
2.3. Assessments
- Waist: 2 cm below the last rib;
- Hip: at the level of the greater trochanter;
- Calf: at the widest circumference of the dominant leg.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| F | Females |
| NS | Non-significant statistical difference |
| DG | Depression group |
| DEP | Depression |
| BG | Binge-eating disorder group |
| BED | Binge-eating disorder |
| DBG | Depression and binge-eating disorder group |
| CG | Control group (without psychiatric disorders) |
| BMI | Body mass index |
| WC | Waist circumference |
| HC | Hip circumference |
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed. text rev.). American Psychiatric Publishing. [Google Scholar]
- Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica. (2022). Diretrizes. Departamento de Nutrição. Available online: https://abeso.org.br/diretrizes (accessed on 1 September 2025).
- Bauman, A., Ainsworth, B. E., Sallis, J. F., Hagströmer, M., Craig, C. L., Bull, F. C., Pratt, M., Venugopal, K., Chau, J., Sjöström, M., & IPS Group. (2011). The descriptive epidemiology of sitting: A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). American Journal of Preventive Medicine, 41(2), 228–235. [Google Scholar] [CrossRef]
- Chartrand, D. J., Murphy-Després, A., Alméras, N., Lemieux, I., Larose, E., & Després, J. P. (2022). Overweight, obesity, and CVD risk: A focus on visceral/ectopic fat. Current Atherosclerosis Reports, 24(4), 185–195. [Google Scholar] [CrossRef]
- Cho, J. M., Oh, J. I., Koh, J. H., Kim, M., Kim, S. G., Cho, S., Lee, S., Kim, Y., Kim, Y. C., Han, S. S., Le, H., Joo, K. W., Kim, Y. S., Kim, D. K., Choi, K., & Park, S. (2025). New-onset mental disorders increase among patients with metabolic diseases after the COVID-19 pandemic. Scientific Reports, 15(1), 16021. [Google Scholar] [CrossRef]
- Faulconbridge, L. F., & Bechtel, C. F. (2014). Depression and disordered eating in the obese person. Current Obesity Reports, 3(1), 127–136. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A. P. D. S., Szwarcwald, C. L., Damacena, G. N., & Souza Júnior, P. R. B. D. (2021). Increasing trends in obesity prevalence from 2013 to 2019 and associated factors in Brazil. Revista Brasileira de Epidemiologia, 24, e210009. [Google Scholar] [CrossRef] [PubMed]
- Flegal, K. M., Kruszon-Moran, D., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2016). Trends in obesity among adults in the United States, 2005 to 2014. JAMA, 315(21), 2284–2291. [Google Scholar] [CrossRef]
- Garcia, C. A. B., Meira, K. C., Souza, A. H., Oliveira, A. L. D. G., & Guimarães, N. S. (2024). Obesity and associated factors in Brazilian adults: Systematic review and meta-analysis of representative studies. International Journal of Environmental Research and Public Health, 21(8), 1022. [Google Scholar] [CrossRef]
- GBD Collaborators. (2024). Global burden of 88 risk factors in 204 countries and territories, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. The Lancet, 403(10442), 2162–2203. [Google Scholar] [CrossRef]
- Giel, K. E., Bulik, C. M., Fernandez-Aranda, F., Hay, P., Keski-Rahkonen, A., Schag, K., Schmidt, U., Thomas, J. J., Weissman, R. S., & Zipfel, S. (2022). Binge eating disorder. Nature Reviews Disease Primers, 8(1), 16. [Google Scholar] [CrossRef]
- Goyal, J., & Rakhra, G. (2024). Sedentarism and chronic health problems. Korean Journal of Family Medicine, 45(5), 239–257. [Google Scholar] [CrossRef]
- Grilo, C. M., & Juarascio, A. (2023). Binge-eating disorder interventions: Review, current status, and implications. Current Obesity Reports, 12(3), 406–416. [Google Scholar] [CrossRef]
- Grilo, C. M., Masheb, R. M., Wilson, G. T., Gueorguieva, R., & White, M. A. (2011). Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79(5), 675–685. [Google Scholar] [CrossRef]
- Gutmann, V. L. R., Santos, D., Silva, C. D., Vallejos, C. C. C., Acosta, D. F., & Mota, M. S. (2022). Reasons that take women and men to seek the basic health units. Journal of Nursing and Health, 12(2), e2212220880. [Google Scholar]
- Hoffmann, K., Kopciuch, D., Michalak, M., Bryl, W., Kus, K., Marzec, K., Raakow, J., Pross, M., Berghaus, R., Nowakowska, E., Kostrzewska, M., Zaprutko, T., Ratajczak, P., & Paczkowska, A. (2022). Adherence of obese patients from Poland and Germany and its impact on the effectiveness of morbid obesity treatment. Nutrients, 14(18), 3880. [Google Scholar] [CrossRef]
- Júnior, C. D. S., Souza, J. R., Silva, N. S., Almeida, S. P., & Torres, L. M. (2022). Saúde do homem na atenção básica: Fatores que influenciam a busca pelo atendimento. Revista Ciências Plurais, 8(2), 1–18. [Google Scholar] [CrossRef]
- Langan, A., Bader, A., Goedkoop, S., Cummings, S., Tsikitas, M., Nogueira, I., Campoverde Reyes, K. J., & Stanford, F. C. (2020). A longitudinal study to investigate the effects of a 12-week comprehensive lifestyle weight management program on body weight and quality of life. Clinical Nutrition ESPEN, 40, 125–132. [Google Scholar] [CrossRef]
- Li, H., Liang, L., Song, Z., & Li, Y. (2025). Global, regional, and national burden of cardiovascular disease attributable to high body mass index from 1990 to 2021 and projection to 2045. Frontiers in Endocrinology, 16, 1546176. [Google Scholar] [CrossRef]
- Lobo, I., da Luz, F. Q., Hay, P., Gaeta, T. L., Teixeira, P. C., Cordás, T. A., Sainsbury, A., & Salis, Z. (2023). Is binge eating associated with poor weight loss outcomes in people with a high body weight? A systematic review with meta-analyses. Eating and Weight Disorders—Studies on Anorexia, Bulimia and Obesity, 28(1), 89. [Google Scholar] [CrossRef]
- Luppino, F. S., de Wit, L. M., Bouvy, P. F., Stijnen, T., Cuijpers, P., Penninx, B. W. J. H., & Zitman, F. G. (2010). Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry, 67(3), 220–229. [Google Scholar] [CrossRef] [PubMed]
- Messias, B. M. M., Gontijo, C. A., Boaventura, C. M., de Sousa, L. C., da Silva, P. E., & Delfino, H. B. P. (2024). Comportamento alimentar de indivíduos com obesidade: Relação com os mecanismos de controle homeostático e hedônico da ingestão alimentar. Revista Brasileira de Obesidade, Nutrição e Emagrecimento, 18(114), 636–650. [Google Scholar]
- Osmari, D. G., Garcez, A., Dias-da-Costa, J. S., & Olinto, M. T. A. (2024). Association between obesity and common mental disorders in women: A population-based study in Southern Brazil. Social Psychiatry and Psychiatric Epidemiology, 59(9), 1577–1585. [Google Scholar] [CrossRef]
- Pacanowski, C. R., Linde, J. A., & Neumark-Sztainer, D. (2018). Weight change over the course of binge eating disorder treatment. Eating and Weight Disorders, 23(3), 353–361. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC5915913/ (accessed on 21 October 2025).
- Pearl, R. L., & Puhl, R. M. (2018). Weight bias internalization and health: A systematic review. Obesity Reviews, 19(8), 1141–1163. [Google Scholar] [CrossRef] [PubMed]
- Pruccoli, J., Mack, I., Klos, B., Schild, S., Stengel, A., Zipfel, S., Giel, K. E., & Schag, K. (2023). Mental health variables impact weight loss, especially in patients with obesity and binge eating: A mediation model on the role of eating disorder pathology. Nutrients, 15(18), 3915. [Google Scholar] [CrossRef]
- Rios, D. L., Oliveira, M. C., Braga, S. Q., Chamorro, M. J., Cunha, B. L., Reis, A. C., Guimarães, A. P., Silva, A. D. N., Silva, D. A. R., Araújo, E. M. Q., & Pimentel, M. M. (2025). Inpatient treatment for severe obesity: A retrospective cohort study in Brazil, comparing exposure variables in a secondary data analysis. PLoS ONE, 20(1), e0303489. [Google Scholar] [CrossRef] [PubMed]
- Rondanelli, M., Gasparri, C., Rigon, C., Ferraris, C., Riva, A., Petrangolini, G., Peroni, G., Faliva, M. A., Naso, M., & Perna, S. (2023). A meta-analysis on the changes of BMI during an inpatient treatment with different follow-up lengths (short and long term) compared with the outpatient phase in obese patients. International Journal of Obesity, 47(7), 538–545. [Google Scholar] [CrossRef]
- Ross, R., Neeland, I. J., Yamashita, S., Shai, I., Seidell, J., Magni, P., Santos, R. D., Arsenault, B., Cuevas, A., Hu, F. B., Griffin, B. A., Zambon, A., Barter, P., Fruchart, J. C., Eckel, R. H., Matsuzawa, Y., & Després, J. P. (2020). Waist circumference as a vital sign in clinical practice: A consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nature Reviews Endocrinology, 16(3), 177–189. [Google Scholar] [CrossRef] [PubMed]
- Stefanakis, K., Kokkorakis, M., & Mantzoros, C. S. (2024). The impact of weight loss on fat-free mass, muscle, bone and hematopoiesis health: Implications for emerging pharmacotherapies aiming at fat reduction and lean mass preservation. Metabolism, 156, 107719. [Google Scholar] [CrossRef]
- Wadden, T. A., Tronieri, J. S., & Butryn, M. L. (2020). Lifestyle modification approaches for the treatment of obesity in adults. American Psychologist, 75(2), 235. [Google Scholar] [CrossRef]
- Wagner, B. E., & Cook, S. (2024). Weight bias and stigma in pediatric obesity. Pediatric Clinics, 71(5), 819–830. [Google Scholar] [CrossRef]
- Watanabe, L. M., Delfino, H. B. P., Pinhel, M. A. S., Noronha, N. Y., Diani, L. M., Assumpcao, L. C. P., Nicoletti, C. F., & Nonino, C. B. (2022). Food and nutrition public policies in Brazil: From malnutrition to obesity. Nutrients, 14(12), 2472. [Google Scholar] [CrossRef]
- Werneck, A. O., Baldew, S. S., Miranda, J. J., Diaz Arnesto, O., Stubbs, B., Silva, D. R., & the South American Physical Activity and Sedentary Behavior Network (SAPASEN) Collaborators. (2019). Physical activity and sedentary behavior patterns and sociodemographic correlates in 116,982 adults from six South American countries: The South American Physical Activity and Sedentary Behavior Network (SAPASEN). International Journal of Behavioral Nutrition and Physical Activity, 16(1), 55. [Google Scholar] [CrossRef]
- Wong, V. W. H., Ho, F. Y. Y., Shi, N. K., Sarris, J., Chung, K. F., & Yeung, W. F. (2021). Lifestyle medicine for depression: A meta-analysis of randomized controlled trials. Journal of Affective Disorders, 284, 203–216. [Google Scholar] [CrossRef]
- World Health Organization. (2010). A healthy lifestyle—WHO recommendations. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (accessed on 1 September 2025).
- World Health Organization. (2023). WHO STEPS surveillance manual: Part 3—Section 5—Physical measurements. Available online: https://cdn.who.int/media/docs/default-source/ncds/ncd-surveillance/steps/part3-section5.pdf?sfvrsn=a46653c7_2 (accessed on 1 September 2025).
- World Health Organization. (2025). Obesity and overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 1 September 2025).
- Yumuk, V., Tsigos, C., Fried, M., Schindler, K., Busetto, L., Micic, D., & Toplak, H. (2015). European guidelines for obesity management in adults. Obesity Facts, 8(6), 402–424. [Google Scholar] [CrossRef]
- Zhao, G., Ford, E. S., Li, C., Balluz, L. S., Giles, W. H., & Mokdad, A. H. (2011). Waist circumference, abdominal obesity, and depression among overweight and obese U.S. adults: National Health and Nutrition Examination Survey 2005–2006. BMC Psychiatry, 11, 130. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y., Duan, J., Zhu, J., Huang, Y., Zhou, J., Li, F., Wang, X., Chen, R., Yang, T., Zhang, L., & Liu, Q. (2025). Separating the effects of childhood and adult obesity on depression, subjective well-being, and suicide attempt: A Mendelian randomization study. European Archives of Psychiatry and Clinical Neuroscience. Advance online publication. [Google Scholar] [CrossRef] [PubMed]
| DG (n = 279) | BG (n = 58) | DBG (n = 38) | CG (n = 622) | p | |
|---|---|---|---|---|---|
| Gender (%F) | 226 (81) | 42 (72.4) | 30 (78.9) | 390 (62.7) | <0.001 |
| Sedentary | 245 (87.8) | 48 (82.8) | 31 (81.6) | 509 (81.8) | NS |
| Age (years) | 48.3 ± 16.3 a | 43.1 ± 15.5 abc | 39.4 ± 13.5 b | 46.9 ± 16.4 ac | 0.004 |
| Hospitalization (days) | 117.7 ± 43.4 | 118.5 ± 54.2 | 120.3 ± 40.0 | 118.5 ± 50.5 | NS |
| DG (n = 279) | BG (n = 58) | DBG (n = 38) | CG (n = 622) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | p | η2p | |
| BMI | 42.9 ± 6.2 | 34.2 ± 4.2 | 44.6 ± 6.3 | 35.2 ± 5.6 | 42.3 ± 4.2 | 33.8 ± 3.9 | 43.3 ± 5.4 | 34.2 ± 4.7 | <0.001 * | 0.914 |
| WC | 115.2 ± 12.8 | 102.1 ± 12.0 | 117.5 ± 15.2 | 98.4 ± 9.1 | 113.9 ± 9.4 | 106.1 ± 8.3 | 116.7 ± 12.4 | 104.9 ± 10.2 | <0.001 * | 0.843 |
| HC | 131.5 ± 11.5 | 122.0 ± 9.9 | 134.7 ± 14.6 | 115.4 ± 10.2 | 130.3 ± 8.3 | 117.7 ± 8.0 | 131.9 ± 11.4 | 121.1 ± 8.5 | <0.001 * | 0.853 |
| CC | 43.3 ± 4.4 | 40.6 ± 4.4 | 44.4 ± 4.5 | 42.8 ± 4.1 | 44.0 ± 3.8 | 40.8 ± 3.8 | 44.4 ± 4.6 | 42.5 ± 4.7 | <0.001 * | 0.838 |
| DG (n = 279) | BG (n = 58) | DBG (n = 38) | CG (n = 622) | p | |
|---|---|---|---|---|---|
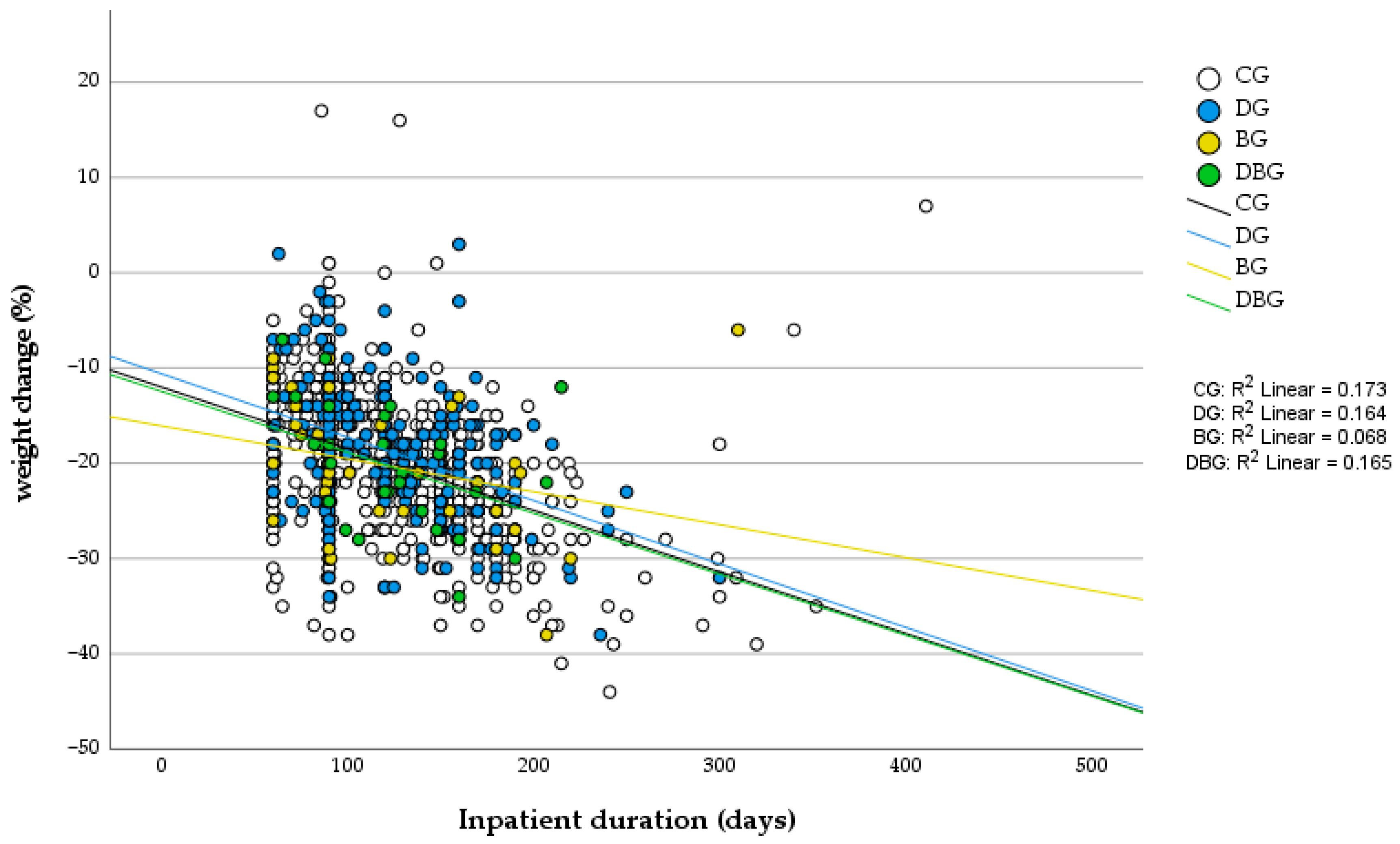
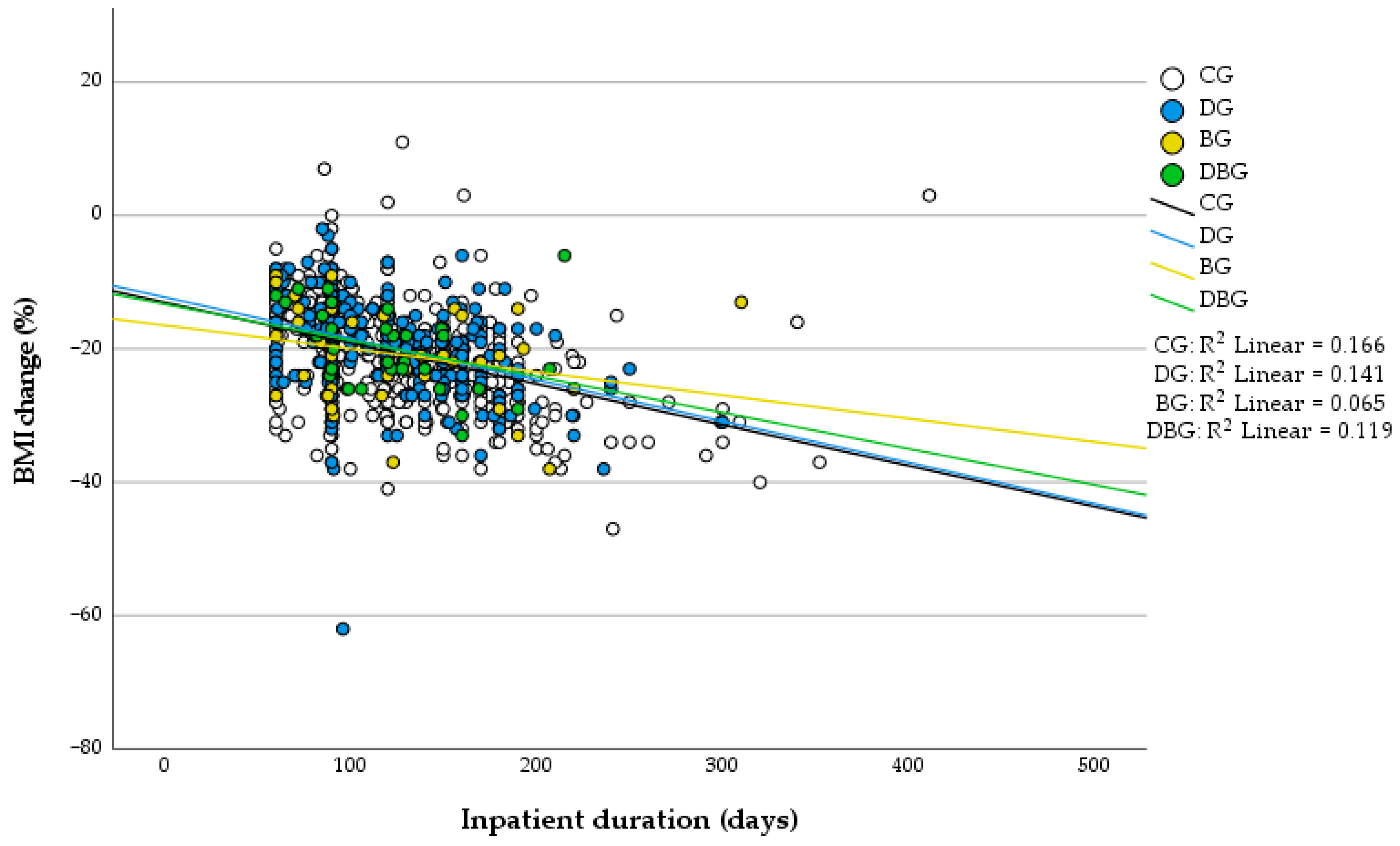
| % weight change | −18.7 ± 6.9 | −20.3 ± 7.2 | −20.3 ± 6.3 | −19.9 ± 7.6 | 0.131 |
| % BMI change | −19.8 ± 6.9 | −20.7 ± 7.4 | −19.9 ± 6.3 | −20.5 ± 7.4 | 0.447 |
| % WC change | −10.9 ± 6.6 | −9.4 ± 5.0 | −11.0 ± 5.3 | −12.1 ± 7.0 | 0.529 |
| % Weight Change × TL | % BMI Change × TL | % WC Change × TL | ||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| DG | −0.404 | <0.001 | −0.375 | <0.001 | 0.148 | 0.490 |
| BG | −0.260 | 0.084 | −0.254 | 0.092 | −0.127 | 0.839 |
| DBG | −0.407 | 0.023 | −0.345 | 0.05 | −0.113 | 0.852 |
| CG | −0.416 | <0.001 | −0.416 | <0.001 | −0.128 | 0.499 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, M.C.A.M.; Nepomuceno, C.M.M.; Trindade, F.M.d.C.; Marinho, C.C.C.e.; Portela, C.G.d.; Braga, S.O.; Pinheiro, N.S.; Barboza, F.F.; Silva, J.L.S.d.; Oliveira, N.C.d. Impact of Inpatient Treatment for Obesity in Patients with Comorbid Psychiatric Disorders. Behav. Sci. 2025, 15, 1562. https://doi.org/10.3390/bs15111562
Oliveira MCAM, Nepomuceno CMM, Trindade FMdC, Marinho CCCe, Portela CGd, Braga SO, Pinheiro NS, Barboza FF, Silva JLSd, Oliveira NCd. Impact of Inpatient Treatment for Obesity in Patients with Comorbid Psychiatric Disorders. Behavioral Sciences. 2025; 15(11):1562. https://doi.org/10.3390/bs15111562
Chicago/Turabian StyleOliveira, Marcia Cristina Almeida Magalhães, Carina Marcia Magalhães Nepomuceno, Francielle Maria da Cruz Trindade, Carolina Chacra Carvalho e Marinho, Cristiano Gidi de Portela, Sérgio Oliveira Braga, Neidjane Sholl Pinheiro, Frederico Fidellis Barboza, José Lucas Sena da Silva, and Natália Cristina de Oliveira. 2025. "Impact of Inpatient Treatment for Obesity in Patients with Comorbid Psychiatric Disorders" Behavioral Sciences 15, no. 11: 1562. https://doi.org/10.3390/bs15111562
APA StyleOliveira, M. C. A. M., Nepomuceno, C. M. M., Trindade, F. M. d. C., Marinho, C. C. C. e., Portela, C. G. d., Braga, S. O., Pinheiro, N. S., Barboza, F. F., Silva, J. L. S. d., & Oliveira, N. C. d. (2025). Impact of Inpatient Treatment for Obesity in Patients with Comorbid Psychiatric Disorders. Behavioral Sciences, 15(11), 1562. https://doi.org/10.3390/bs15111562






