Complex Intervention Programs Integrating Multiple Intervention Strategies Were Not More Effective than Active Control Groups: Evidence from Randomized Controlled Trials
Abstract
1. Introduction
1.1. Global Prevalence of Depression and Insomnia
1.2. The Evidence-Based Psychological Intervention for Depression and Sleep Problems
1.3. The Complex Intervention Program Integrating Multiple Intervention Strategies
1.4. Challenges and Concerns Regarding the Effectiveness of Complex Intervention Programs
1.5. Current Study
2. Study 1
2.1. Methods
2.1.1. Participants
2.1.2. Procedure
2.1.3. Intervention
2.1.4. Measures
2.1.5. Data Analysis
2.2. Results
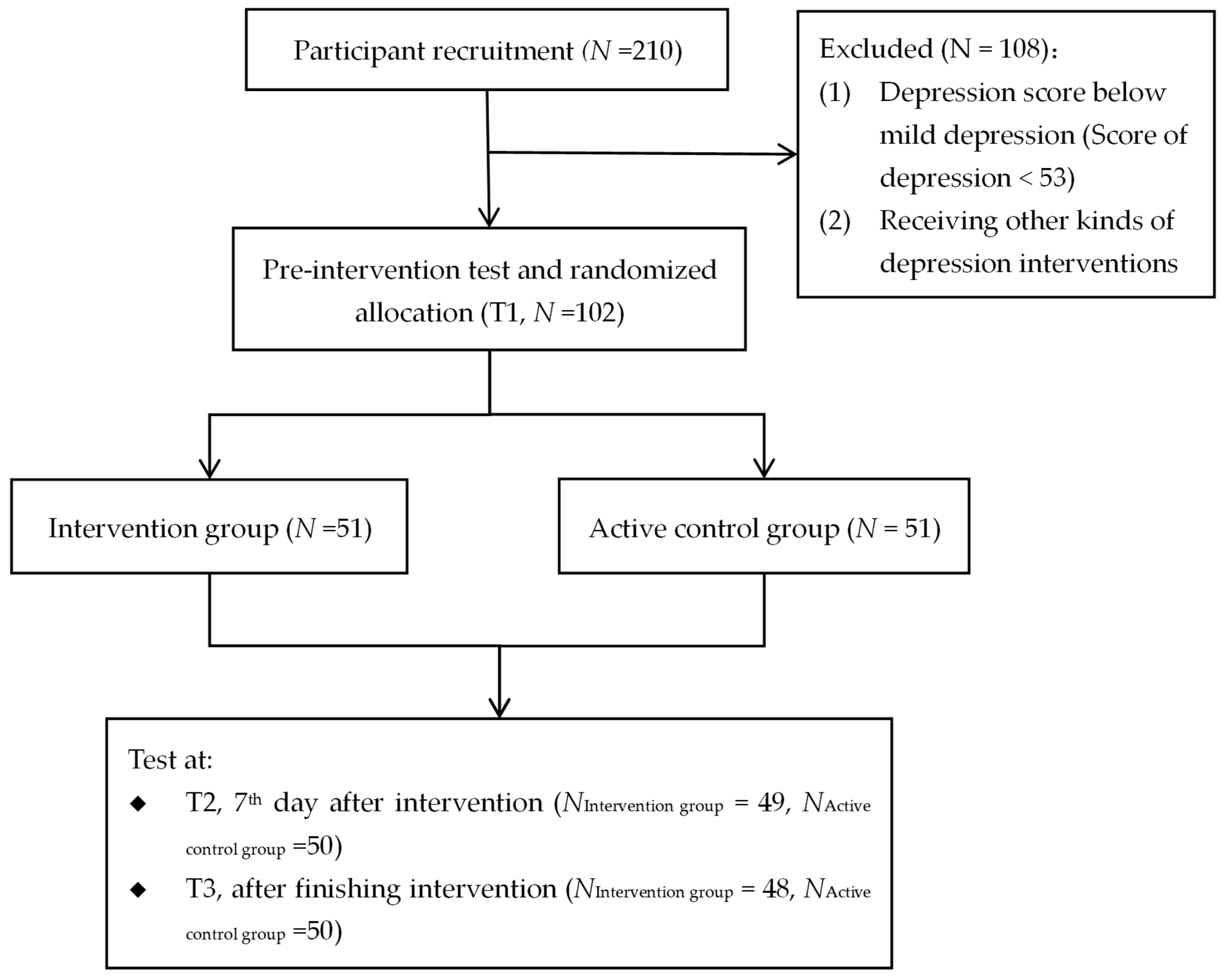
2.2.1. Participants Enrollment
2.2.2. Common Method Bias for Study 1
2.2.3. Baseline Between-Group Comparisons
2.2.4. Intervention Effect Test of Study 1
2.3. Discussion of Study 1
3. Study 2
3.1. Methods
3.1.1. Participants
3.1.2. Procedure
3.1.3. Intervention
3.1.4. Measures
3.1.5. Data Analysis
3.2. Results
3.2.1. Participants Enrollment
3.2.2. Common Method Bias
3.2.3. Baseline Between-Group Comparisons
3.2.4. Intervention Effect Test of Study 2
3.3. Discussion of Study 2
4. General Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beevers, C. G., Pearson, R., Hoffman, J. S., Foulser, A. A., Shumake, J., & Meyer, B. (2017). Effectiveness of an internet intervention (Deprexis) for depression in a united states adult sample: A parallel-group pragmatic randomized controlled trial. Journal of Consulting and Clinical Psychology, 85(4), 367. [Google Scholar] [CrossRef] [PubMed]
- Berger, T., Krieger, T., Sude, K., Meyer, B., & Maercker, A. (2018). Evaluating an e-mental health program (“deprexis”) as adjunctive treatment tool in psychotherapy for depression: Results of a pragmatic randomized controlled trial. Journal of Affective Disorders, 227, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Biagianti, B., Foti, G., Di Liberto, A., Bressi, C., & Brambilla, P. (2023). CBT-informed psychological interventions for adult patients with anxiety and depression symptoms: A narrative review of digital treatment options. Journal of Affective Disorders, 325, 682–694. [Google Scholar] [CrossRef] [PubMed]
- Bolier, L., Haverman, M., Westerhof, G. J., Riper, H., Smit, F., & Bohlmeijer, E. (2013). Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health, 13(1), 119. [Google Scholar] [CrossRef]
- Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. [Google Scholar] [CrossRef]
- Buysse, D. J., Reynolds, C. F., III, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. [Google Scholar] [CrossRef]
- Carr, A., Cullen, K., Keeney, C., Canning, C., Mooney, O., Chinseallaigh, E., & O’Dowd, A. (2020). Effectiveness of positive psychology interventions: A systematic review and meta-analysis. The Journal of Positive Psychology, 16(6), 749–769. [Google Scholar] [CrossRef]
- Carr, A., & Finnegan, L. (2015). The say ‘yes’ to life (SYTL) program: A positive psychology group intervention for depression. Journal of Contemporary Psychotherapy, 45(2), 109–118. [Google Scholar] [CrossRef]
- Christensen, H., Griffiths, K. M., & Jorm, A. F. (2004). Delivering interventions for depression by using the internet: Randomised controlled trial. British Medical Journal, 328, 265–268. [Google Scholar] [CrossRef]
- Clancy, F., Prestwich, A., Caperon, L., Tsipa, A., & O’connor, D. B. (2020). The association between worry and rumination with sleep in non-clinical populations: A systematic review and meta-analysis. Health Psychology Review, 14(4), 427–448. [Google Scholar] [CrossRef]
- Cleary, M. A., Richardson, C., Ross, R. J., Heussler, H. S., Wilson, A., Downs, J., & Walsh, J. (2025). Effectiveness of current digital cognitive behavioural therapy for insomnia interventions for adolescents with insomnia symptoms: A systematic review and meta-analysis. Journal of Sleep Research, 34(6), e14466. [Google Scholar] [CrossRef]
- Cohen, J. (1969). Statistical power analysis for the behavioural sciences. Academic Press. [Google Scholar]
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [Google Scholar] [CrossRef]
- Cristóbal-Narváez, P., Haro, J. M., & Koyanagi, A. (2020). Perceived stress and depression in 45 low-and middle-income countries. Journal of Affective Disorders, 274, 799–805. [Google Scholar] [CrossRef] [PubMed]
- de Entrambasaguas, M., Díaz-Silveira, C., Burgos-Julián, F. A., & Santed, M. A. (2023). Can mindfulness-based interventions improve outcomes in cognitive-behavioural therapy for chronic insomnia disorder in the general population? Systematic review and meta-analysis. Clinical Psychology & Psychotherapy, 30(5), 965–978. [Google Scholar]
- de Graaf, L. E., Huibers, M. J., Riper, H., Gerhards, S. A., & Arntz, A. (2009). Use and acceptability of unsupported online computerized cognitive behavioral therapy for depression and associations with clinical outcome. Journal of Affective Disorders, 116(3), 227–231. [Google Scholar] [CrossRef]
- Dennis, J. P., & Vander Wal, J. S. (2010). The cognitive flexibility inventory: Instrument development and estimates of reliability and validity. Cognitive Therapy and Research, 34, 241–253. [Google Scholar] [CrossRef]
- Didonna, F., Lanfredi, M., Xodo, E., Ferrari, C., Rossi, R., & Pedrini, L. (2019). Mindfulness-based cognitive therapy for obsessive-compulsive disorder: A pilot study. Journal of Psychiatric Practice, 25(2), 156–170. [Google Scholar] [CrossRef]
- Fairholme, C. P., & Manber, R. (2015). Sleep, emotions, and emotion regulation: An overview. Sleep and Affect, 2015, 45–61. [Google Scholar]
- Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior research methods, 39(2), 175–191. [Google Scholar] [CrossRef]
- Friedrich, A., & Schlarb, A. (2018). Let’s talk about sleep: A systematic review of psychological interventions to improve sleep in university students. European Sleep Research Society, 27, 4–22. [Google Scholar] [CrossRef]
- Gard, D. E., Gard, M. G., Kring, A. M., & John, O. P. (2006). Anticipatory and consummatory components of the experience of pleasure: A scale development study. Journal of Research in Personality, 40(6), 1086–1102. [Google Scholar] [CrossRef]
- Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. [Google Scholar] [CrossRef]
- Han, X., & Yang, H. (2009). Chinese version of Nolen-Hoeksema Ruminative Responses Scale (RRS) used in 912 college students: Reliability and validity. Chinese Journal of Clinical Psychology, 17(5), 549–551. [Google Scholar]
- Hedman-Lagerlöf, M., Hedman-Lagerlöf, E., & Öst, L. G. (2018). The empirical support for mindfulness-based interventions for common psychiatric disorders: A systematic review and meta-analysis. Psychological Medicine, 48, 2116–2129. [Google Scholar] [CrossRef] [PubMed]
- Hill, V., Ferguson, S., Rebar, A., Shriane, A., & Vincent, G. (2022). Go to bed! A systematic review and meta-analysis of bedtime procrastination determinants and sleep outcomes. SLEEP, 45, A1-A1. [Google Scholar] [CrossRef]
- Ho, F. Y. Y., Chung, K. F., Yeung, W. F., Ng, T. H., Kwan, K. S., Yung, K. P., & Cheng, S. K. (2015). Self-help cognitive-behavioral therapy for insomnia: A meta-analysis of randomized controlled trials. Sleep Medicine Reviews, 19, 17–28. [Google Scholar] [CrossRef]
- Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y., He, Z., Zeng, Z., Zhan, L., & Shen, Z. (2023). Influence of parent-child relationship on adolescent depression: The roles of cognitive flexibility and friendship quality. Chinese Journal of Clinical Psychology, 31(3), 682–687. [Google Scholar]
- Huang, Y., Hu, Y., & Mai, W. (2012). Stress and sleep disturbance—A connection in CVD. Nature Reviews Cardiology, 9(10), 598. [Google Scholar] [CrossRef]
- Hum, K. M., Chan, C. J., Gane, J., Conway, L., McAndrews, M. P., & Smith, M. L. (2019). Do distance-delivery group interventions improve depression in people with epilepsy? Epilepsy & Behavior, 98, 153–160. [Google Scholar] [CrossRef]
- Hundt, N. E., Mignogna, J., Underhill, C., & Cully, J. A. (2013). The relationship between use of CBT skills and depression treatment outcome: A theoretical and methodological review of the literature. Behavior Therapy, 44(1), 12–26. [Google Scholar] [CrossRef] [PubMed]
- Jovarauskaite, L., Dumarkaite, A., Truskauskaite-Kuneviciene, I., Jovaisiene, I., Andersson, G., & Kazlauskas, E. (2021). Internet-based stress recovery intervention FOREST for healthcare staff amid COVID-19 pandemic: Study protocol for a randomized controlled trial. Trials, 22(1), 559. [Google Scholar] [CrossRef] [PubMed]
- Karma, J., Jane, K. R., & Dusana, D. (2019). Feasibility and efficacy of an adapted mindfulness-based intervention (MBI) in areas of socioeconomic deprivation (SED). Mindfulnes, 10(2), 325–338. [Google Scholar]
- Klainin-Yobas, P., Cho, M. A. A., & Creedy, D. (2012). Efficacy of mindfulness-based interventions on depressive symptoms among people with mental disorders: A meta-analysis. International Journal of Nursing Studies, 49(1), 109–121. [Google Scholar] [CrossRef]
- Klein, J. P., Berger, T., Schröder, J., Späth, C., Meyer, B., Caspar, F., Arndt, A., Greiner, W., Gräfe, V., & Hohagen, F. (2016). Effects of a psychological internet intervention in the treatment of mild to moderate depressive symptoms: Results of the EVIDENT study, a randomized controlled trial. Psychotherapy and Psychosomatics, 85(4), 218–228. [Google Scholar] [CrossRef]
- Kodsi, A., Bullock, B., Kennedy, G. A., & Tirlea, L. (2021). Psychological interventions to improve sleep in young adults: A systematic review and meta-analysis of randomized controlled trials. Behavioral Sleep Medicine, 6, 1–18. [Google Scholar] [CrossRef]
- Koles, J. (2012). Review of cognitive behaviour therapy: Basics and beyond (2nd ed.). The Australian Educational and Developmental Psychologist, 29(1), 78–79. [Google Scholar] [CrossRef][Green Version]
- Koydemir, S., Sökmez, A. B., & Schütz, A. (2021). A meta-analysis of the effectiveness of randomized controlled positive psychological interventions on subjective and psychological well-being. Applied Research in Quality of Life, 16(3), 1145–1185. [Google Scholar] [CrossRef]
- Kroese, F. M., De Ridder, D. T., Evers, C., & Adriaanse, M. A. (2014). Bedtime procrastination: Introducing a new area of procrastination. Frontiers in Psychology, 5, 89333. [Google Scholar] [CrossRef]
- Latalova, K., Kamaradova, D., & Prasko, J. (2014). Perspectives on perceived stigma and self-stigma in adult male patients with depression. Neuropsychiatric Disease and Treatment, 2014, 1399–1405. [Google Scholar] [CrossRef]
- Li, Y., Guo, Y., Hong, Y. A., Zeng, Y., Monroe-Wise, A., Zeng, C., Zhu, M., Zhang, H., Qiao, J., Xu, Z., Cai, W., Li, L., & Liu, C. (2022). Dose–response effects of patient engagement on health outcomes in an mHealth intervention: Secondary analysis of a randomized controlled trial. JMIR mHealth and uHealth, 10(1), e25586. [Google Scholar] [CrossRef]
- Liu, B., Sun, S., Sun, W., & Chang, C. (2013). The application of Depression Stigma Scale on young peopleged 15 to 24 in Beijing. School of Public Health, 29(2), 116–119. [Google Scholar]
- Liu, J., Li, F., & Lian, Y. (2008). Investigation of reliability and validity of the social support scale. Journal of Xinjiang Medical University, 1, 1–3. [Google Scholar]
- Liu, X., Liu, L., Yang, J., Chai, F., Wang, A., Sun, L., Zhao, G., & Ma, D. (1997). Validity and reliability of the Adolescent Self-Rating Life Events Checklist (ASLEC). Chinese Journal of Clinical Psychology, 5(1), 39–41. [Google Scholar]
- Liu, X. C., Tang, M. Q., Hu, L., Wang, A. Z., Wu, H. X., Zhao, G. F., Gao, C. N., & Li, W. S. (1996). Reliability and validity of the Pittsburgh Sleep Quality Index. Chinese Journal of Psychiatry, 29(2), 103–107. [Google Scholar]
- Loong, L. W., & Stephanie, T. (2023). The effectiveness of positive psychology interventions for promoting well-being of adults experiencing depression compared to other active psychological treatments: A systematic review and meta-analysis. Journal of Happiness Studies, 24(1), 249–273. [Google Scholar]
- Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy, 33(3), 335–343. [Google Scholar] [CrossRef] [PubMed]
- Ma, X. H., Zhu, L. W., Guo, J., Zhao, Y., Fu, Y. M., & Mu, L. (2021). Reliability and validity of the bedtime procrastination scale in Chinese college students. Chinese Journal of Clinical Psychology, 29(4), 717–720. [Google Scholar]
- Mahmud, S., Mohsin, M., Dewan, M. N., & Muyeed, A. (2023). The global prevalence of depression, anxiety, stress, and insomnia among general population during COVID-19 pandemic: A systematic review and meta-analysis. Trends in Psychology, 31(1), 143–170. [Google Scholar] [CrossRef] [PubMed]
- Meneo, D., Samea, F., Tahmasian, M., & Baglioni, C. (2023). The emotional component of insomnia disorder: A focus on emotion regulation and affect dynamics in relation to sleep quality and insomnia. Journal of Sleep Research, 32(6), e13983. [Google Scholar] [CrossRef]
- Meyer, B., & Garcia-Roberts, L. (2007). Congruence between reasons for depression and motivations for specific interventions. Psychology and Psychotherapy: Theory, Research and Practice, 80(4), 525–542. [Google Scholar] [CrossRef] [PubMed]
- Mhango, W., Crowter, L., Michelson, D., & Gaysina, D. (2023). Psychoeducation as an active ingredient for interventions for perinatal depression and anxiety in youth: A mixed-method systematic literature review and lived experience synthesis. BJPsych Open, 10, e10. [Google Scholar] [CrossRef]
- Morr, C. E., Ritvo, P., Ahmad, F., & Moineddin, R. (2020). Effectiveness of an 8-week web-based mindfulness virtual community intervention for university students on symptoms of stress, anxiety, and depression: Randomized controlled trial. JMIR Mental Health, 7(7), e18595. [Google Scholar] [CrossRef]
- Mullan, B. A. (2014). Sleep, stress and health: A commentary. Stress and Health, 30(5), 433–435. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100(4), 569. [Google Scholar] [CrossRef]
- Ong, J. C., Manber, R., Segal, Z., Xia, Y., Shapiro, S., & Wyatt, J. K. (2014). A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep: Journal of Sleep and Sleep Disorders Research, 37(9), 1553–1566. [Google Scholar] [CrossRef]
- Pedersen, G. A., Lakshmin, P., Schafer, A., Watts, S., & Kohrt, B. A. (2020). Common factors in psychological treatments delivered by non-specialists in low- and middle-income countries: Manual review of competencies. Journal of Behavioral and Cognitive Therapy, 30(3), 165–186. [Google Scholar] [CrossRef]
- Peter, L., Reindl, R., Zauter, S., Hillemacher, T., & Richter, K. (2019). Effectiveness of an online CBT-I intervention and a face-to-face treatment for shift work sleep disorder: A comparison of sleep diary data. International Journal of Environmental Research and Public Health, 16(17), 3081. [Google Scholar] [CrossRef] [PubMed]
- Pizzagalli, D. A. (2014). Depression, stress, and anhedonia: Toward a synthesis and integrated model. Annual Review of Clinical Psychology, 10(1), 393–423. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z., & Jiang, G. (2014). The effects and influential factors of computerized psychological treatments for depression: Meta-analysis and meta-regression of randomized controlled trials. Journal of Psychological Science, 37(3), 748–755. [Google Scholar]
- Ren, Z., Li, X., Zhao, L., Yu, X., Li, Z., Lai, L., Ruan, Y., & Jiang, G. (2016). Effectiveness and mechanism of internet-based self-help intervention for depression: The Chinese version of MoodGYM. Acta Psychologica Sinica, 48(7), 818–832. [Google Scholar] [CrossRef]
- Rigas, C., Park, H., Marouane, N., Chien-Lin, S., Greenway, K., Lipman, M., McVeigh, C., Novak, M., Trinh, E., Alam, A., & Suri, R. S. (2022). Long-term effects of a brief mindfulness intervention versus a health enhancement program for treating depression and anxiety in patients undergoing hemodialysis: A randomized controlled trial. Canadian Journal of Kidney Health & Disease, 9, 20543581221074562. [Google Scholar]
- Ritterband, L. M., Thorndike, F. P., Ingersoll, K. S., Lord, H. R., Gonder-Frederick, L., Frederick, C., Quigg, M. S., Cohn, W. F., & Morin, C. M. (2017). Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: A randomized clinical trial. JAMA Psychiatry, 74(1), 68–75. [Google Scholar] [CrossRef]
- Ryan, R. M., & Deci, E. L. (2017). Self-determination theory: Basic psychological needs in motivation, development, and wellness. The Guilford Press. [Google Scholar]
- Saddichha, S., Al-Desouki, M., Lamia, A., Linden, I. A., & Krausz, M. (2014). Online interventions for depression and anxiety—A systematic review. Health Psychology and Behavioral Medicine: An Open Access Journal, 2(1), 841–881. [Google Scholar] [CrossRef]
- Santos, F. R. M. D., Lacerda, S. S., Coelhoso, C. C., Barrichello, C. R., & Kozasa, E. H. (2021). The integration of meditation and positive psychology practices to relieve stress in women workers (flourish): Effects in two pilot studies. Behavioral Sciences, 11(4), 43. [Google Scholar] [CrossRef]
- Sevilla-Llewellyn-Jones, J., Santesteban-Echarri, O., Pryor, I., McGorry, P., & Alvarez-Jimenez, M. (2018). Web-based mindfulness interventions for mental health treatment: Systematic review and meta-analysis. JMIR Mental Health, 5(3), e10278. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y. F., Chen, C. Q., Wang, Y., & Wang, Y. N. (2009, November). Factor analysis of the Chinese version of the temporal experience of pleasure scale (TEPS). China National Academic Conference on Psychology, Shandong, China. [Google Scholar]
- Steger, M. F., Shim, Y., Barenz, J., & Shin, J. Y. (2014). Through the windows of the soul: A pilot study using photography to enhance meaning in life. Journal of Contextual Behavioral Science, 3(1), 27–30. [Google Scholar] [CrossRef]
- Sverre, K. T., Nissen, E. R., Farver-Vestergaard, I., Johannsen, M., & Zachariae, R. (2023). Comparing the efficacy of mindfulness-based therapy and cognitive-behavioral therapy for depression in head-to-head randomized controlled trials: A systematic review and meta-analysis of equivalence. Clinical Psychology Review, 100, 102234. [Google Scholar] [CrossRef]
- Taouk, M., Lovibond, P. F., & Laube, R. (2001). Psychometric properties of a Chinese version of the 21-item depression anxiety stress scales (DASS21) (Report for New South Wales Transcultural Mental Health Centre). Cumberland Hospital. [Google Scholar]
- Twomey, C., O’Reilly, G., & Meyer, B. (2017). Effectiveness of an individually-tailored computerised CBT programme (Deprexis) for depression: A meta-analysis. Psychiatry Research, 256, 371–377. [Google Scholar] [CrossRef]
- van Straten, A., & Cuijpers, P. (2009). Self-help therapy for insomnia: A meta-analysis. Sleep Medicine Reviews, 13(1), 61–71. [Google Scholar] [CrossRef]
- Vedaa, Ø., Kallestad, H., Scott, J., Smith, O. R., Pallesen, S., Morken, G., Langsrud, K., Gehrman, P., Thorndike, F. P., Ritterband, L. M., Harvey, A. G., Stiles, T., & Sivertsen, B. (2020). Effects of digital cognitive behavioural therapy for insomnia on insomnia severity: A large-scale randomised controlled trial. The Lancet Digital Health, 2(8), e397–e406. [Google Scholar] [CrossRef]
- Wang, C. F., Cai, Z. H., & Xu, Q. (2009). Evaluation analysis of self-rating disorder scale in 1340 people. Chinese Journal of Nervous and Mental Diseases, 12, 267–268. [Google Scholar]
- Wang, J., & Wu, H. (2014). The interventions in depression based on the theory of positive mental health education. Chinese Journal of Special Education, 3, 80–84. [Google Scholar]
- Wang, Y., Yang, Y., Xiao, W. T., & Su, Q. (2016). Validity and reliability of the Chinese version of the cognitive flexibility inventory in college students. Chinese Mental Health Journal, 30(1), 58–62. [Google Scholar]
- Wang, Z., & Chi, Y. (1984). Self-Rating Depression Scale (SDS). Shanghai Archives of Psychiatry, 2, 71–72. [Google Scholar]
- Wang, Z., Shalihaer, K., Hofmann, S. G., Feng, S., & Liu, X. (2024). The role of attentional control in mindfulness intervention for emotional distress: A randomized controlled trial with longitudinal mediation analyses. Clinical Psychology & Psychotherapy, 31, e2981. [Google Scholar] [CrossRef] [PubMed]
- Watkins, E. R. (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134(2), 163. [Google Scholar] [CrossRef] [PubMed]
- Wood, L., Birtel, M., Alsawy, S., Pyle, M., & Morrison, A. (2014). Public perceptions of stigma towards people with schizophrenia, depression, and anxiety. Psychiatry Research, 220(1–2), 604–608. [Google Scholar] [CrossRef]
- Xiao, S. (1994). Theoretical basis and research applications of the social support rating scale. Journal of Clinical Psychiatry, 2, 98–100. [Google Scholar]
- Yang, T. Z., & Huang, H. T. (2003). Epidemiological study on psychological stress among urban residents during social transition. Chinese Journal of Epidemiology, 24(9), 760–764. [Google Scholar]
- Yang, Z., Han, S., Zhang, L., Sun, M., Hu, Q., Hu, Y., & Wu, B. (2024). Dose–response effects of patient engagement on anxiety and depression in a cognitive-behavioral intervention: Secondary analysis of a pilot randomized controlled trial and a clinical controlled trial. AIDS and Behavior, 28(6), 1923–1935. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S., Liu, Y., Song, S., Peng, S., Mao, S., & Mao, X. (2022). The psychological nursing interventions based on pygmalion effect could alleviate negative emotions of patients with suspected COVID-19 patients: A retrospective analysis. International Journal of General Medicine, 15, 513–522. [Google Scholar] [CrossRef]
- Zhou, H., & Long, L. (2004). Statistical remedies for common method biases. Advances in Psychological Science, 12(6), 924–950. [Google Scholar]
- Zhou, S., Zhao, J., & Zhang, L. (2022). Application of artificial intelligence on psychological interventions and diagnosis: An overview. Frontiers in Psychiatry, 13, 811665. [Google Scholar] [CrossRef]
- Zhou, Y., Zhao, D., Zhu, X., Liu, L., Meng, M., Shao, X., Zhu, X., Xiang, J., He, J., Zhao, Y., & Yuan, Y. (2023). Psychological interventions for the prevention of depression relapse: Systematic review and network meta-analysis. Translational Psychiatry, 13, 300. [Google Scholar] [CrossRef] [PubMed]
- Zung, W. W. (1965). A self-rating depression scale. Archives of General Psychiatry, 12(1), 63–70. [Google Scholar] [CrossRef] [PubMed]

| Day | Course | Practice |
|---|---|---|
| 1 | Introduction of depression | Photograph-based intervention |
| 2 | Introduction of negative emotion | “Three Good Things” intervention |
| 3 | Recognizing the emergence of emotions I | Photograph-based intervention |
| 4 | Recognizing the emergence of emotions II | “Three Good Things” intervention |
| 5 | Assessing the intensity of emotions | Photograph-based intervention |
| 6 | Distinguish between thoughts and facts | “Three Good Things” intervention |
| 7 | Recognizing Irrational Thinking I | Photograph-based intervention |
| 8 | Challenging Irrational Thinking I | Mindfulness meditation |
| 9 | CBT exercises I | Mindfulness meditation |
| 10 | CBT exercises II | Mindfulness meditation |
| 11 | CBT exercises III | Mindfulness meditation |
| 12 | CBT exercises IV | Mindfulness meditation |
| 13 | Daily dairy | Mindfulness meditation |
| 14 | Daily dairy | Mindfulness meditation |
| Group | M | SD | |
|---|---|---|---|
| Age | Intervention | 20.88 | 1.90 |
| control | 20.50 | 1.46 | |
| Depression | Intervention | 62.37 | 5.89 |
| control | 61.65 | 6.21 | |
| Cognitive flexibility | Intervention | 55.61 | 10.00 |
| control | 58.24 | 10.85 | |
| Rumination | Intervention | 63.59 | 10.56 |
| control | 63.33 | 10.32 | |
| Perceived stress | Intervention | 25.75 | 5.52 |
| control | 25.61 | 6.11 | |
| Temporal pleasurable experience | Intervention | 75.96 | 12.88 |
| control | 81.08 | 15.50 | |
| Depression stigma | Intervention | 35.41 | 10.77 |
| control | 38.12 | 10.03 | |
| Life experience | Intervention | 80.22 | 24.91 |
| control | 83.43 | 22.72 | |
| Social support | Intervention | 22.65 | 5.38 |
| control | 25.04 | 6.48 |
| T1 (M ± SD) | T2 (M ± SD) | T3 (M ± SD) | F (Time) | η2 (Time) | F (Group) | F (Time × Group) | ||
|---|---|---|---|---|---|---|---|---|
| Depression | Intervention | 62.42 ± 5.65 | 46.13 ± 9.07 | 42.79 ± 9.29 | 9.25 *** | 0.092 | 2.29 | 0.78 |
| Control | 61.59 ± 6.00 | 43.43 ± 8.70 | 38.73 ± 8.51 | |||||
| DS | Intervention | 35.42 ± 11.01 | 34.08 ± 12.95 | 34.17 ± 13.38 | 11.79 *** | 0.113 | 1.83 | 2.53 |
| Control | 38.45 ± 9.84 | 37.16 ± 9.72 | 34.73 ± 12.34 | |||||
| Rumination | Intervention | 63.65 ± 10.69 | 56.13 ± 10.52 | 52.10 ± 11.75 | 14.86 *** | 0.138 | 1.43 | 2.13 |
| Control | 63.08 ± 10.14 | 52.31 ± 11.49 | 47.37 ± 12.31 | |||||
| CF | Intervention | 55.23 ± 10.13 | 56.69 ± 8.49 | 62.06 ± 10.90 | 8.48 *** | 0.084 | 4.34 * | 1.51 |
| Control | 57.88 ± 10.80 | 62.47 ± 11.54 | 67.90 ± 12.16 | |||||
| PS | Intervention | 26.00 ± 5.50 | 21.69 ± 5.43 | 20.15 ± 6.46 | 16.25 *** | 0.149 | 0.97 | 2.21 |
| Control | 25.59 ± 5.89 | 20.27 ± 5.77 | 17.34 ± 7.00 | |||||
| TPE | Intervention | 75.65 ± 13.21 | 79.54 ± 12.78 | 84.63 ± 14.50 | 12.43 *** | 0.118 | 2.6 | 0.03 |
| Control | 81.29 ± 15.65 | 83.35 ± 13.36 | 89.76 ± 10.80 |
| Group | M | SD | |
|---|---|---|---|
| Age | Intervention | 21.15 | 1.91 |
| Control | 21.36 | 2.08 | |
| Sleep quality | Intervention | 10.92 | 2.79 |
| Control | 11.51 | 2.97 | |
| Sleep procrastination | Intervention | 35.37 | 6.58 |
| Control | 34.91 | 5.68 | |
| Rumination | Intervention | 51.87 | 13.40 |
| Control | 55.48 | 11.09 | |
| Perceive stress | Intervention | 41.96 | 11.02 |
| Control | 43.73 | 7.94 | |
| Negative affect | Intervention | 22.01 | 14.53 |
| Control | 25.33 | 11.26 |
| T1 (M ± SD) | T2 (M ± SD) | T3 (M ± SD) | F (Time) | η2 (Time) | F (Group) | F (Time × Group) | ||
|---|---|---|---|---|---|---|---|---|
| SQP | Intervention | 10.93 ± 2.79 | 9.04 ± 2.62 | 7.54 ± 2.46 | 77.03 *** | 0.416 | 2.91 | 0.50 |
| control | 11.52 ± 2.97 | 9.59 ± 2.79 | 8.55 ± 2.54 | |||||
| SP | Intervention | 35.37 ± 0.82 | 29.98 ± 0.94 | 28.55 ± 1.01 | 5.43 ** | 0.274 | 0.93 | 1.84 |
| control | 34.91 ± 0.81 | 31.81 ± 0.92 | 30.22 ± 0.99 | |||||
| Rumination | Intervention | 51.87 ± 1.68 | 47.83 ± 1.63 | 45.39 ± 1.53 | 4.35 * | 0.170 | 4.30 * | 0.44 |
| control | 55.48 ± 1.65 | 51.64 ± 1.60 | 50.52 ± 1.50 | |||||
| PS | Intervention | 41.96 ± 1.30 | 38.44 ± 1.29 | 35.81 ± 1.26 | 3.14 * | 0.204 | 2.00 | 0.40 |
| control | 43.73 ± 1.28 | 40.36 ± 1.27 | 38.82 ± 1.24 | |||||
| NA | Intervention | 22.02 ± 1.77 | 16.94 ± 1.72 | 13.98 ± 1.61 | 52.72 *** | 0.233 | 1.87 | 0.03 |
| control | 25.34 ± 1.74 | 18.43 ± 1.68 | 17.64 ± 1.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.; Zhang, C.; Huang, J.; Liu, T.; Xu, W. Complex Intervention Programs Integrating Multiple Intervention Strategies Were Not More Effective than Active Control Groups: Evidence from Randomized Controlled Trials. Behav. Sci. 2025, 15, 1554. https://doi.org/10.3390/bs15111554
Wang S, Zhang C, Huang J, Liu T, Xu W. Complex Intervention Programs Integrating Multiple Intervention Strategies Were Not More Effective than Active Control Groups: Evidence from Randomized Controlled Trials. Behavioral Sciences. 2025; 15(11):1554. https://doi.org/10.3390/bs15111554
Chicago/Turabian StyleWang, Shoushi, Chunyang Zhang, Jingyuan Huang, Tianyuan Liu, and Wei Xu. 2025. "Complex Intervention Programs Integrating Multiple Intervention Strategies Were Not More Effective than Active Control Groups: Evidence from Randomized Controlled Trials" Behavioral Sciences 15, no. 11: 1554. https://doi.org/10.3390/bs15111554
APA StyleWang, S., Zhang, C., Huang, J., Liu, T., & Xu, W. (2025). Complex Intervention Programs Integrating Multiple Intervention Strategies Were Not More Effective than Active Control Groups: Evidence from Randomized Controlled Trials. Behavioral Sciences, 15(11), 1554. https://doi.org/10.3390/bs15111554






