Impact of a Mental Health Consultation Program on Child Psychosocial Development over Two School Years
Abstract
1. Introduction
The Current Study
2. Materials and Methods
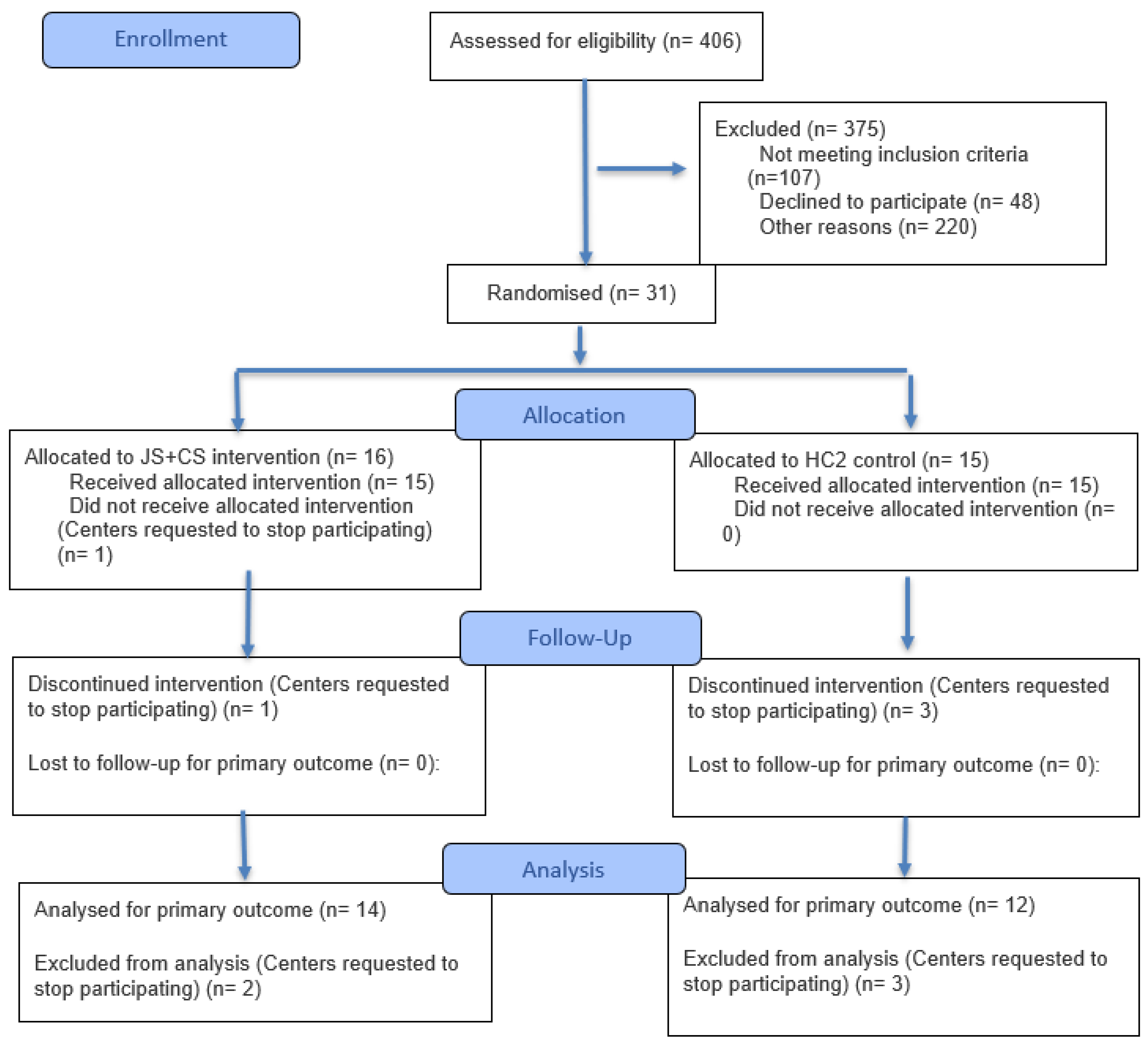
2.1. Sample
2.2. Measures
2.2.1. Demographics
2.2.2. Child Prosocial Skill Measures
2.2.3. Child Externalizing and Internalizing Behaviors Measures
2.2.4. Teacher Consultations
2.3. Procedures
2.3.1. Jump Start Plus COVID Support (JS+CS) Description
2.3.2. Healthy Caregivers—Healthy Children Control Description
2.4. Statistical Analysis Plan
2.4.1. Research Questions 1 and 2
2.4.2. Research Question 3
2.4.3. Sensitivity Analysis for Baseline Imbalance
2.4.4. Sensitivity Analysis for Attrition Bias
3. Results
3.1. Baseline Characteristics
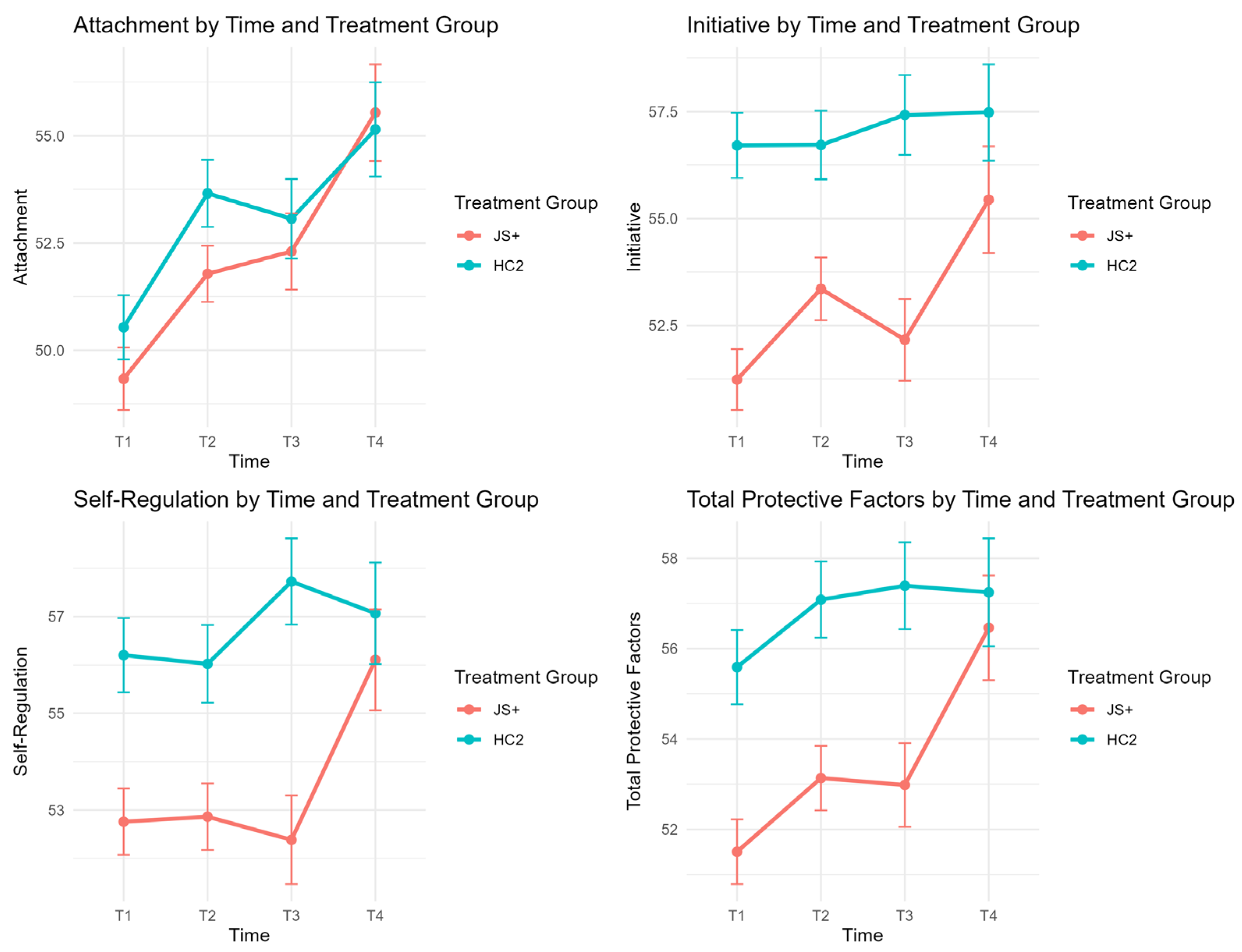
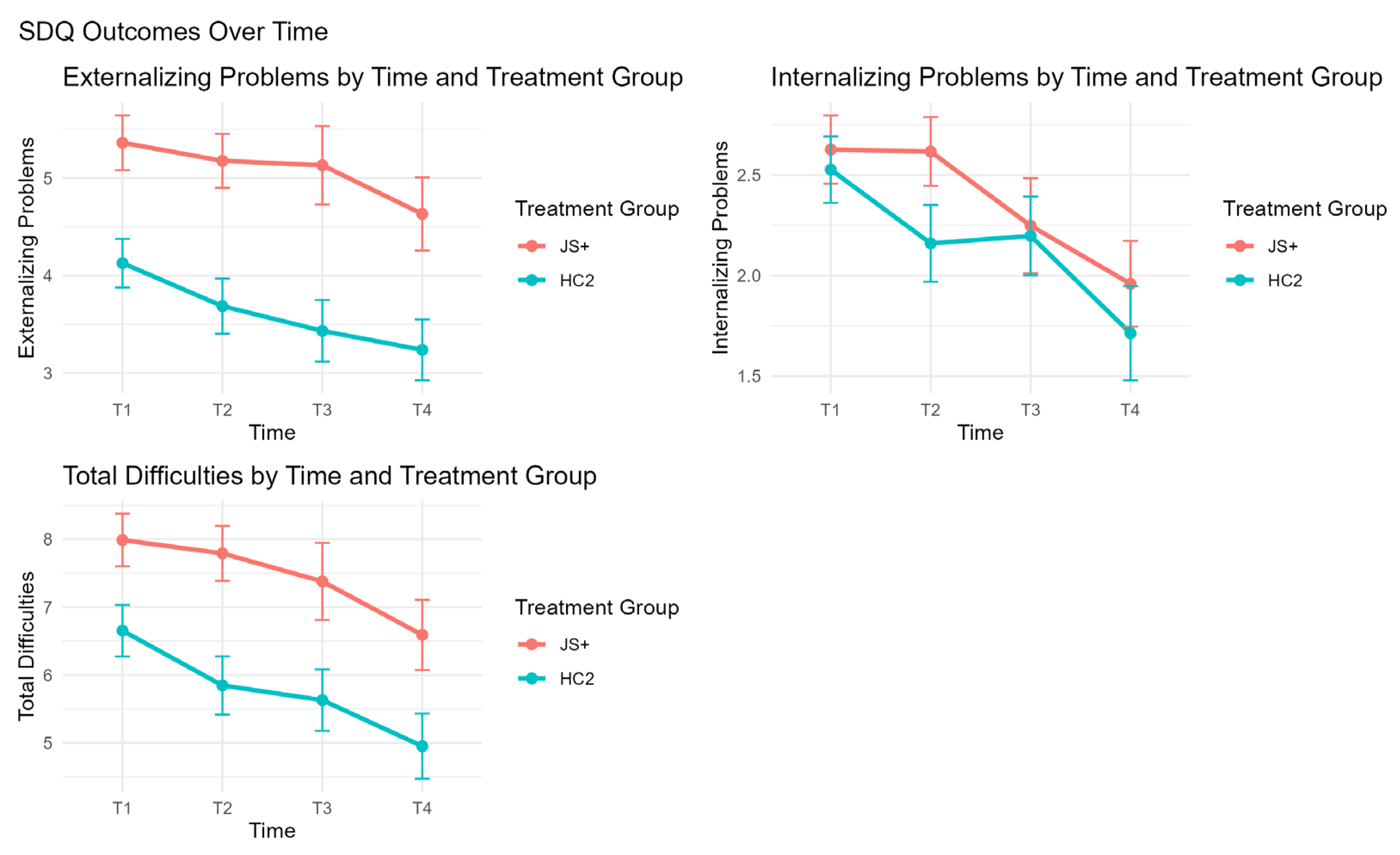
3.2. Child Outcomes over Time
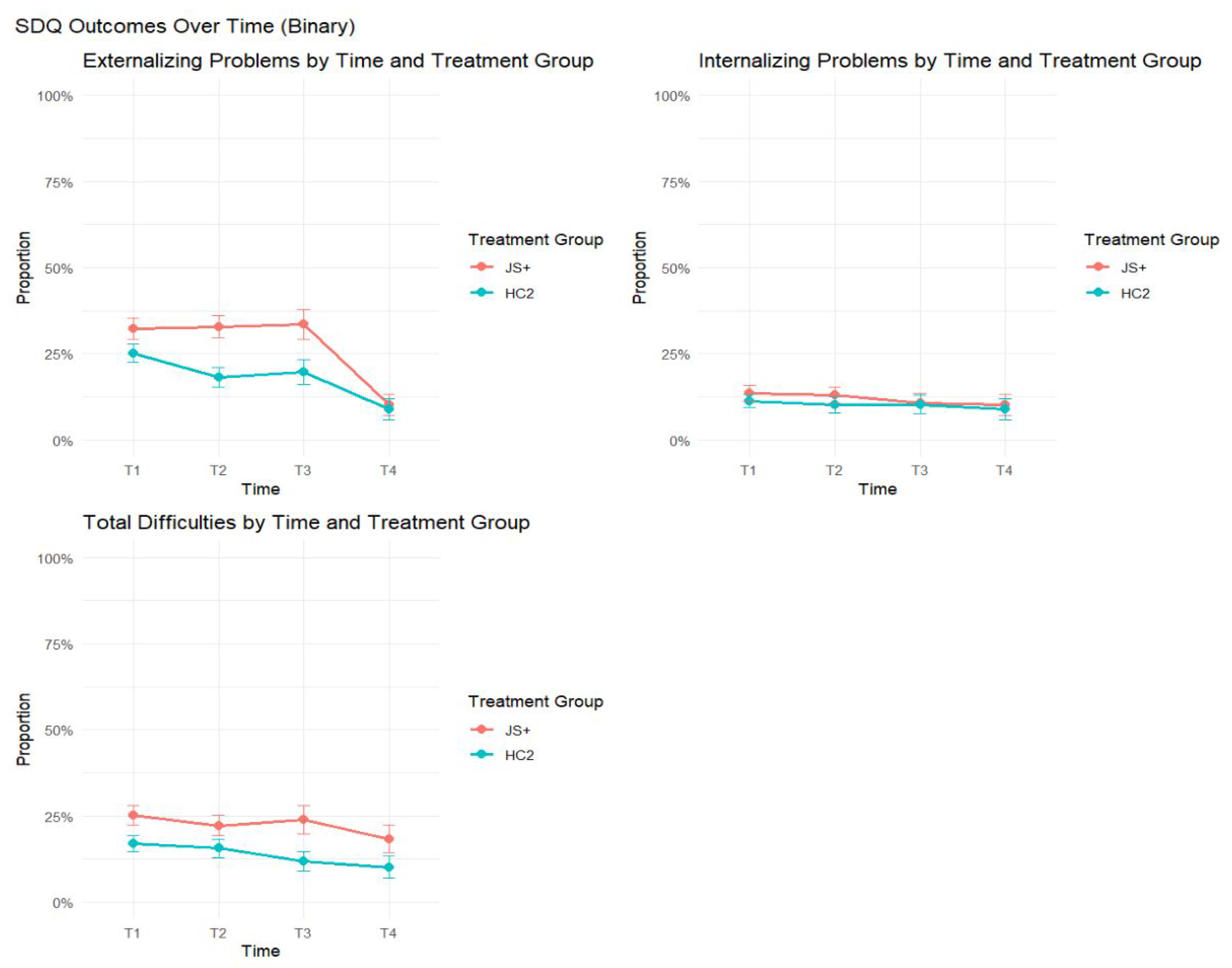
3.3. Changes over Time in Clinical Levels of Behavior by Treatment Group
3.4. Results of the Sensitivity Analysis for Baseline Imbalance
3.5. Results of the Sensitivity Analysis for Attrition Bias
4. Discussion
4.1. Limitations
4.2. Implications
4.3. Public Health Impact
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DECA | Devereux Early Childhood Assessment |
| ECE | Early care and education |
| ECMHC | Early Childhood Mental Health Consultation |
| GEE | Generalized Estimating Equations |
| HC2 | Healthy Caregivers—Healthy Children |
| IPCW | Inverse Probability of Censoring Weighting |
| IPTW | Inverse Probability of Treatment Weights |
| JS+CS | Jump Start Plus COVID Support |
| MHC | Mental health consultant |
| RA | Research assistant |
| SDQ | Strengths and Difficulties Questionnaire |
| SMD | Standardized Mean Difference |
| TPF | Total Protective Factors |
Appendix A
| Outcome | Primary GEE: JS+ vs. HC2 Diff (SE) | Primary Diff p | Primary Tx × Time p | PS-Adjusted: JS+ vs. HC2 Diff (95% CI) | PS-Adjusted Diff p | PS-Adjusted Tx × Time p |
|---|---|---|---|---|---|---|
| DECA Attachment | −0.26 (0.88) | 0.766 | 0.329 | −0.17 (−1.96, 1.62) | 0.852 | 0.536 |
| DECA Initiative | −1.18 (0.86) | 0.171 | 0.015 | −1.21 (−2.96, 0.54) | 0.174 | 0.006 |
| DECA Self-Regulation | −2.21 (0.79) | 0.005 | 0.027 | −2.18 (−3.81, −0.55) | 0.009 | 0.017 |
| DECA Total Protective | −1.01 (0.87) | 0.246 | 0.101 | −0.99 (−2.82, 0.84) | 0.291 | 0.051 |
| SDQ Externalizing | +0.76 (0.28) | 0.007 | 0.897 | +0.84 (0.26, 1.42) | 0.005 | 0.867 |
| SDQ Internalizing | +0.31 (0.18) | 0.083 | 0.925 | +0.35 (−0.01, 0.71) | 0.055 | 0.975 |
| SDQ Total Problems | +1.01 (0.39) | 0.009 | 0.937 | +1.12 (0.31, 1.93) | 0.007 | 0.973 |
| Predictor | OR (95% CI) | p-Value |
|---|---|---|
| Treatment group (JS+ vs. HC2) | 1.48 (0.89, 2.45) | 0.13 |
| Child age (years) | 0.50 (0.39, 0.64) | <0.001 |
| Gender | — | 0.22 |
| Race | — | 0.31 |
| Ethnicity | — | 0.16 |
| Primary language | — | 0.18 |
| Baseline DECA Total Protective Factors | 1.01 (0.98, 1.04) | 0.45 |
| Baseline SDQ Total Problems | 0.95 (0.90, 1.01) | 0.11 |
References
- American Academy of Pediatrics, American Public Health Association & National Resource Center for Health and Safety in Child Care and Early Education. (2019). Caring for our children: National health and safety performance standards; Guidelines for early care and education programs (4th ed.). American Academy of Pediatrics. [Google Scholar]
- Becker, D. R., McClelland, M. M., Loprinzi, P., & Trost, S. G. (2014). Physical activity, self-regulation, and early academic achievement in preschool children. Early Education and Development, 25(1), 56–70. [Google Scholar] [CrossRef]
- Bleecker, T., Sherwood, D., & Chan-Sew, S. L. (2005). San francisco high quality child care mental health consultation initiative. Available online: http://rtckids.fmhi.usf.edu/rtcconference/handouts/pdf/17/Session%201000/Bleecker%20Poster.pdf (accessed on 5 August 2025).
- Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press. [Google Scholar]
- Bronfenbrenner, U. (1994). Ecological models of human development. International Encyclopedia of Education, 3(2), 37–43. [Google Scholar]
- Bulotsky-Shearer, R. J., Fernandez, V. A., & Rainelli, S. (2013). The validity of the devereux early childhood assessment for culturally and linguistically diverse head start children. Early Childhood Research Quarterly, 28(4), 794–807. [Google Scholar] [CrossRef]
- Carlson, J. S., & Voris, D. S. T. (2017). One-year stability of the devereux early childhood assessment for preschoolers second edition. Journal of Psychoeducational Assessment, 36(8), 829–834. [Google Scholar] [CrossRef]
- Center of Excellence for Infant and Early Childhood Mental Health Consultation. (2022). Status of the evidence for infant and early childhood mental health consultation (IECMHC). Available online: https://www.iecmhc.org/documents/CoE-Evidence-Synthesis.pdf (accessed on 5 August 2025).
- Crane, J., Mincic, M., & Winsler, A. (2011). Parent–teacher agreement and reliability on the devereux early childhood assessment (deca) in english and spanish for ethnically diverse children living in poverty. Early Education and Development, 22, 520–547. [Google Scholar] [CrossRef]
- Downer, J. T., López, M. L., Grimm, K. J., Hamagami, A., Pianta, R. C., & Howes, C. (2012). Observations of teacher–child interactions in classrooms serving Latinos and dual language learners: Applicability of the classroom assessment scoring system in diverse settings. Early Childhood Research Quarterly, 27(1), 21–32. [Google Scholar] [CrossRef]
- Drake-Croft, J., Parker, A., Rabinovitz, L., Brady, R., & Horen, N. (2025). Advancing mental health and equity through infant and early childhood mental health consultation. Healthcare, 13(5), 545. [Google Scholar] [CrossRef]
- Duran, F. B., Hepburn, K. S., Kaufmann, R. K., Le, L. T., Allen, M. D., Brennan, E. M., & Green, B. L. (2010). Early childhood mental health consultation. Vanderbilt University, The Center on the Social and Emotional Foundations for Early Learning (CSEFEL). Available online: https://csefel.vanderbilt.edu/documents/rs_ecmhc.pdf (accessed on 5 August 2025).
- Feil, E. G., Frey, A., Walker, H. M., Small, J. W., Seeley, J. R., Golly, A., & Forness, S. R. (2014). The efficacy of a home–school intervention for preschoolers with challenging behaviors: A randomized controlled trial of preschool first step to success. Journal of Early Intervention, 36(3), 151–170. [Google Scholar] [CrossRef]
- Futterer, J., Mullins, C., Bulotsky-Shearer, R. J., Guzmán, E., Hildago, T., Kolomeyer, E., Howe, E., Horen, N., Sanders, L. M., & Natale, R. (2024). Initial validation of the health environment rating scale-early childhood consultation-classroom (HERS-ECC-C). Infant Mental Health Journal, 45(4), 449–463. [Google Scholar] [CrossRef] [PubMed]
- Gilliam, W. S. (2007). Early childhood consultation partnership: Results of a random-controlled evaluation: Final report and executive summary. Yale University Child Study Center. Available online: https://basicknowledge101.com/pdf/evaluation_of_cts_early_childhood_consultation_partnership.pdf (accessed on 5 August 2025).
- Gilliam, W. S., Maupin, A. N., & Reyes, C. R. (2016). Early childhood mental health consultation: Results of a statewide random-controlled evaluation. Journal of the American Academy of Child & Adolescent Psychiatry, 55(9), 754–761. [Google Scholar] [CrossRef]
- Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38(5), 581–586. [Google Scholar] [CrossRef]
- Gu, Q., & Day, C. (2007). Teachers resilience: A necessary condition for effectiveness. Teaching and Teacher Education, 23(8), 1302–1316. [Google Scholar] [CrossRef]
- Harding, J. F., & Paulsell, D. (2018). Improving access to early care and education: An equity-focused policy research agenda. Mathematica Policy Research. Available online: https://www.researchgate.net/publication/328172128 (accessed on 5 August 2025).
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [Google Scholar] [CrossRef] [PubMed]
- Hartman, S., Winsler, A., & Manfra, L. (2017). Behavior concerns among low-income, ethnically and linguistically diverse children in child care: Importance for school readiness and kindergarten achievement. Early Education and Development, 28(3), 255–273. [Google Scholar] [CrossRef]
- Hemmeter, M., Barton, E., Fox, L., Vatland, C., Henry, G., Pham, L., Horth, K., Taylor, A., Binder, D. P., von der Embse, M., & Veguilla, M. (2022). Program-wide implementation of the pyramid model: Supporting fidelity at the program and classroom levels. Early Childhood Research Quarterly, 59, 56–73. [Google Scholar] [CrossRef]
- Hoffman, T., & Kuvalanka, K. (2019). Behavior problems in child care classrooms: Insights from child care teachers. Preventing School Failure: Alternative Education for Children and Youth, 63, 1–10. [Google Scholar] [CrossRef]
- Iruka, I. U. (2020). Using a social determinants of early learning framework to eliminate educational disparities and opportunity gaps. In C. J. Russo, A. M. Goff, & A. Yoshikawa (Eds.), Getting it right: Using implementation research to improve outcomes in early care and education. Chapter 3. Foundation for Child Development. Available online: https://www.fcd-us.org/wp-content/uploads/2020/06/GettingitRight_UsingImplementationResearchtoImproveOutcomesinECE_Chapter3_2020.pdf (accessed on 5 August 2025).
- Jing, J.-Q., Yang, C.-J., Wang, Y., Su, X.-Y., & Du, Y.-J. (2024). Impact of COVID-19 on emotional and behavioral problems among preschool children: A meta-analysis. BMC Pediatrics, 24, 455. [Google Scholar] [CrossRef] [PubMed]
- LeBuffe, P. A., & Naglieri, J. A. (1999). The devereux early childhood assessment (DECA): A measure of within-child protective factors in preschool children. NHSA Dialog, 3(1), 75–80. [Google Scholar] [CrossRef]
- LeBuffe, P. A., & Naglieri, J. A. (2012). Devereux early childhood assessment for preschoolers (2nd ed.). Kaplan Early Learning Company. [Google Scholar]
- Mackrain, M., LeBuffe, P., & Powell, G. (2007). Devereux early childhood assessment for infants and toddlers. Kaplan Early Learning Company. [Google Scholar]
- Messiah, S. E., Lebron, C., Moise, R., Sunil Mathew, M., Sardinas, K., Chang, C., Palenzuela, J., Walsh, J., Shelnutt, K. P., Spector, R., Altare, F., & Natale, R. (2017). Healthy caregivers-healthy children (HC2) phase 2: Integrating culturally sensitive childhood obesity prevention strategies into childcare center policies. Contemporary Clinical Trials, 53, 60–67. [Google Scholar] [CrossRef]
- Mullins, C., Ullery, M. A., Mallar, C., Bulotsky-Shearer, R., Hernandez, J., Berkovits, M., Jent, J., Delamater, A. M., & Natale, R. (2025). The longitudinal psychological impacts of the COVID-19 pandemic on caregivers with young children. Family Relations, 174(4), 1385–1400. [Google Scholar] [CrossRef]
- Naglieri, J. A., LeBuffe, P. A., & Shapiro, V. B. (2013). Assessment of social-emotional competencies related to resilience. In S. Goldstein, & R. Brooks (Eds.), Handbook of resilience in children (pp. 261–272). Kluwer/Academic Press. [Google Scholar]
- Natale, R., Agosto, Y., Bulotsky Shearer, R. J., St. George, S. M., & Jent, J. (2023a). Designing a virtual mental health consultation program to support and strengthen childcare centers impacted by COVID-19: A randomized controlled trial protocol. Contemporary Clinical Trials, 124, 107022. [Google Scholar] [CrossRef]
- Natale, R., Atem, F. D., Lebron, C., Mathew, M. S., Weerakoon, S. M., Martinez, C. C., Shelnutt, K. P., Spector, R., & Messiah, S. E. (2022a). Cluster-randomised trial of the impact of an obesity prevention intervention on childcare centre nutrition and physical activity environment over 2 years. Public Health Nutrition, 25(11), 3172–3181. [Google Scholar] [CrossRef]
- Natale, R., Bailey, J., Kolomeyer, E., Futterer, J., Schenker, M., & Bulotsky-Shearer, R. (2023b). Early childhood teacher workplace stress and classroom practices. Journal of Early Childhood Teacher Education, 44(4), 897–914. [Google Scholar] [CrossRef]
- Natale, R., Kenworthy LaMarca, T., Pan, Y., Howe, E., Agosto, Y., Bulotsky-Shearer, R. J., St. George, S. M., Rahman, T., Velasquez, C., & Jent, J. F. (2025). Strengthening early childhood protective factors through safe and supportive classrooms: Findings from jump start + COVID support. Children, 12(7), 812. [Google Scholar] [CrossRef]
- Natale, R., Kenworthy LaMarca, T., Rahman, T., Howe, E., Bulotsky-Shearer, R. J., Agosto, Y., & Jent, J. (2024). Using RE-AIM to assess infant early childhood mental health practices in classrooms serving children with and without disabilities. Healthcare, 12(24), 2501. [Google Scholar] [CrossRef]
- Natale, R., Kolomeyer, E., Futterer, J., Mahmoud, D. F., Schenker, M., Robleto, A., Horen, N., & Spector, R. (2022b). Infant and early childhood mental health consultation in a diverse metropolitan area. Infant Mental Health Journal, 43(3), 440–454. [Google Scholar] [CrossRef] [PubMed]
- Natale, R., Lopez-Mitnik, G., Uhlhorn, S., Asfour, L., & Messiah, S. E. (2014). Effect of a child care center-based obesity prevention program on body mass index and nutrition practices among preschool-aged children. Health Promotion Practice, 15(5), 695–705. [Google Scholar] [CrossRef]
- Natale, R., Messiah, S. E., Asfour, L. S., Uhlhorn, S. B., Englebert, N. E., & Arheart, K. L. (2017). Obesity prevention program in childcare centers: Two-year follow-up. American Journal of Health Promotion, 31(6), 502–510. [Google Scholar] [CrossRef] [PubMed]
- National Center for Immunization and Respiratory Diseases. (2021). COVID-19 guidance for operating early care and education/child care programs. Available online: https://stacks.cdc.gov/view/cdc/107881 (accessed on 5 August 2025).
- Panchal, U., Salazar de Pablo, G., Franco, M., Moreno, C., Parellada, M., Arango, C., & Fusar-Poli, P. (2021). The impact of COVID-19 lockdown on child and adolescent mental health: A systematic review. European Child & Adolescent Psychiatry, 32(7), 1151–1177. [Google Scholar] [CrossRef] [PubMed]
- Patel, J., Smith, R., O’Farrelly, C., Iles, J., Rosan, C., Ryan, R., & Ramchandani, P. (2021). Assessing behavior in children aged 12–24 months using the strengths and difficulties questionnaire. Infancy, 26(5), 724–734. [Google Scholar] [CrossRef]
- Perry, D. F., Dunne, M. C., McFadden, L., & Campbell, D. (2008). Reducing the risk for preschool expulsion: Mental health consultation for young children with challenging behaviors. Journal of Child and Family Studies, 17(1), 44–54. [Google Scholar] [CrossRef]
- Rakap, S., & Balikci, S. (2024). Enhancing preschool teachers’ use of pyramid model practices through coaching intervention. Journal of Behavioral Education. Advance online publication. [Google Scholar] [CrossRef]
- Raver, C. C., Jones, S. M., Li-Grining, C. P., Metzger, M., Smallwood, K., & Sardin, L. (2008). Improving preschool classroom processes: Preliminary findings from a randomized trial implemented in head start settings. Early Childhood Research Quarterly, 63(3), 253–255. [Google Scholar] [CrossRef]
- Ride, J., Weimar, O., Kovacs, M., Hiscock, H., & Quach, J. (2025). Systematic review of outcome measures used in evaluation of school-based mental health interventions. Mental Health & Prevention, 30, 200401. [Google Scholar] [CrossRef]
- Silver, H. C., Davis Schoch, A. E., Loomis, A. M., Park, C. E., & Zinsser, K. M. (2023). Updating the evidence: A systematic review of a decade of Infant and early childhood mental health consultation (IECMHC) research. Infant Mental Health Journal, 44(1), 5–26. [Google Scholar] [CrossRef] [PubMed]
- Upshur, C., Wenz-Gross, M., & Reed, G. (2009). A pilot study of early childhood mental health consultation for children with behavioral problems in preschool. Early Childhood Research Quarterly, 24(1), 29–45. [Google Scholar] [CrossRef]
- Yoshikawa, H., Weiland, C., Brooks-Gunn, J., Burchinal, M. R., Espinosa, L. M., Gormley, W. T., Ludwig, J., Magnuson, K. A., Phillips, D., & Zaslow, M. J. (2013). Investing in our future: The evidence base on preschool education. Society for Research in Child Development & Foundation for Child Development. Available online: https://www.fcd-us.org/wp-content/uploads/2016/04/Evidence-Base-on-Preschool-Education-FINAL.pdf (accessed on 5 August 2025).
- Zeger, S. L., & Liang, K. Y. (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 42(1), 121–130. [Google Scholar] [CrossRef]
- Zinsser, K. M., Silver, H. C., Shenberger, E. R., & Jackson, V. (2022). A systematic review of early childhood exclusionary discipline. Review of Educational Research, 92(5), 743–785. [Google Scholar] [CrossRef]

| Characteristic | JS+ (N = 304) | HC2 (N = 367) | p-Value |
|---|---|---|---|
| Age, years, M (SD) | 3.59 (1.18) | 3.34 (1.15) | 0.0068 |
| Gender, n/N (%) | <0.0001 | ||
| Female | 160/287 (55.7) | 142/317 (44.8) | |
| Male | 127/287 (44.3) | 175/317 (55.2) | |
| Race, n/N (%) | <0.0001 | ||
| White | 206/278 (74.1) | 198/307 (64.5) | |
| Non-Hispanic Black | 48/278 (17.3) | 87/307 (28.3) | |
| Native American | 4/278 (1.4) | 4/307 (1.3) | |
| Asian Pacific Islander | 1/278 (0.4) | 0/307 (0.0) | |
| Multiracial | 14/278 (5.0) | 9/307 (2.9) | |
| Other | 5/278 (1.8) | 9/307 (2.9) | |
| Ethnicity, n/N (%) | <0.0001 | ||
| Hispanic | 238/284 (83.8) | 217/315 (68.9) | |
| Non-Hispanic White | 11/284 (3.9) | 16/315 (5.1) | |
| Non-Hispanic Black | 24/284 (8.5) | 60/315 (19.0) | |
| Haitian | 7/284 (2.5) | 18/315 (5.7) | |
| Other | 4/284 (1.4) | 4/315 (1.3) | |
| Primary Language, n/N (%) | <0.0001 | ||
| English | 90/285 (31.6) | 151/317 (47.6) | |
| Spanish | 194/285 (68.1) | 164/317 (51.7) | |
| Creole | 1/285 (0.4) | 2/317 (0.6) | |
| Total Teacher Consults, M (SD) | 18.71 (5.97) | 11.96 (4.32) | <0.0001 |
| Outcome | JS+ T1 M (SE) | JS+ T2 M (SE) | JS+ T3 M (SE) | JS+ T4 M (SE) | HC2 T1 M (SE) | HC2 T2 M (SE) | HC2 T3 M (SE) | HC2 T4 M (SE) | JS+ vs. HC2 Diff (SE) | Chi Square Diff | Difference p-Value | Chi Square-Tx × Time | Tx × Time p-Value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DECA Attachment | 49.33 (0.73) | 51.78 (0.65) | 52.30 (0.89) | 55.54 (1.13) | 50.53 (0.75) | 53.66 (0.78) | 53.06 (0.93) | 55.14 (1.10) | −0.26 (0.88) | 0.09 | 0.7664 | 3.44 | 0.3289 |
| DECA Initiative | 51.24 (0.71) | 53.36 (0.73) | 52.16 (0.96) | 55.44 (1.25) | 56.71 (0.76) | 56.72 (0.80) | 57.42 (0.93) | 57.48 (1.13) | −1.18 (0.86) | 1.77 | 0.171 | 10.49 | 0.0148 |
| DECA Self-Regulation | 52.76 (0.69) | 52.86 (0.69) | 52.38 (0.92) | 56.11 (1.04) | 56.20 (0.77) | 56.02 (0.80) | 57.73 (0.89) | 57.07 (1.05) | −2.21 (0.79) | 6.71 | 0.0054 | 9.19 | 0.0269 |
| DECA Total Protective Factors | 51.50 (0.72) | 53.13 (0.71) | 52.98 (0.93) | 56.46 (1.16) | 55.59 (0.82) | 57.08 (0.84) | 57.39 (0.96) | 57.25 (1.20) | −1.01 (0.87) | 1.26 | 0.2459 | 6.24 | 0.1006 |
| SDQ Externalizing Problems | 5.36 (0.28) | 5.18 (0.28) | 5.13 (0.40) | 4.63 (0.37) | 4.13 (0.25) | 3.69 (0.28) | 3.43 (0.32) | 3.24 (0.31) | 0.76 (0.28) | 6.81 | 0.0066 | 0.60 | 0.8972 |
| SDQ Internalizing Problems | 2.63 (0.17) | 2.62 (0.17) | 2.25 (0.24) | 1.96 (0.21) | 2.53 (0.17) | 2.16 (0.19) | 2.20 (0.20) | 1.71 (0.23) | 0.31 (0.18) | 2.95 | 0.083 | 0.47 | 0.9247 |
| SDQ Total Problems | 7.99 (0.39) | 7.79 (0.40) | 7.38 (0.57) | 6.59 (0.52) | 6.65 (0.38) | 5.85 (0.43) | 5.63 (0.45) | 4.95 (0.48) | 1.01 (0.39) | 6.4 | 0.0093 | 0.41 | 0.9372 |
| Outcome | JS+ T1 Concern/ n (%) | JS+ T2 Concern/ n (%) | JS+ T3 Concern/ n (%) | JS+ T4 Concern/ n (%) | HC2 T1 Concern/ n (%) | HC2 T2 Concern/n (%) | HC2 T3 Concern/n (%) | HC2 T4 Concern/ n (%) | OR (95% CI) | Chi Square Difference | Difference p-Value | Chi Square Tx × Time | Tx × Time p-Value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DECA Attachment | 53/237 (22.4%) | 20/214 (9.3%) | 12/116 (10.3%) | 7/93 (7.5%) | 61/251 (24.3%) | 26/180 (14.4%) | 17/126 (13.5%) | 4/76 (5.3%) | 0.61 (0.26–1.45) | 0.09 | 0.2645 | 2.77 | 0.4286 |
| DECA Initiative | 45/234 (19.2%) | 28/213 (13.2%) | 16/116 (13.8%) | 11/91 (12.1%) | 25/248 (10.1%) | 12/171 (7.0%) | 7/123 (5.7%) | 4/73 (5.5%) | 1.87 (0.73–4.79) | 1.77 | 0.1947 | 1.95 | 0.5826 |
| DECA Self-Regulation | 38/240 (15.8%) | 25/216 (11.6%) | 12/115 (10.4%) | 8/93 (8.6%) | 31/241 (12.9%) | 16/175 (9.1%) | 5/121 (4.1%) | 4/73 (5.5%) | 1.34 (0.55–3.28) | 6.71 | 0.516 | 3.39 | 0.3359 |
| DECA Total Protective Factors | 34/222 (15.3%) | 22/200 (11.0%) | 13/113 (11.5%) | 10/91 (11.0%) | 28/230 (12.2%) | 10/154 (6.5%) | 8/117 (6.8%) | 3/69 (4.3%) | 1.40 (0.54–3.63) | 1.26 | 0.492 | 2.81 | 0.4212 |
| SDQ Externalizing Problems | 74/230 (32.2%) | 71/216 (32.9%) | 38/113 (33.6%) | 10/98 (10.2%) | 67/266 (25.2%) | 34/186 (18.3%) | 25/127 (19.7%) | 8/89 (9.0%) | 1.05 (0.54–2.02) | 6.81 | 0.8893 | 1.04 | 0.7924 |
| SDQ Internalizing Problems | 31/230 (13.5%) | 28/216 (13.0%) | 12/113 (10.6%) | 10/98 (10.2%) | 30/266 (11.3%) | 19/186 (10.2%) | 13/127 (10.2%) | 8/89 (9.0%) | 1.31 (0.64–2.69) | 2.95 | 0.4557 | 0.1 | 0.9921 |
| SDQ Total Problems | 58/230 (25.2%) | 48/216 (22.2%) | 27/113 (23.9%) | 18/98 (18.4%) | 45/266 (16.9%) | 29/186 (15.6%) | 15/127 (11.8%) | 9/89 (10.1%) | 1.62 (0.82–3.20) | 6.4 | 0.1638 | 4.48 | 0.2138 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Natale, R.; Pan, Y.; Agosto, Y.; Velasquez, C.; Mansoor, E.; Bulotsky-Shearer, R.J.; Messiah, S.E.; Jent, J.F. Impact of a Mental Health Consultation Program on Child Psychosocial Development over Two School Years. Behav. Sci. 2025, 15, 1497. https://doi.org/10.3390/bs15111497
Natale R, Pan Y, Agosto Y, Velasquez C, Mansoor E, Bulotsky-Shearer RJ, Messiah SE, Jent JF. Impact of a Mental Health Consultation Program on Child Psychosocial Development over Two School Years. Behavioral Sciences. 2025; 15(11):1497. https://doi.org/10.3390/bs15111497
Chicago/Turabian StyleNatale, Ruby, Yue Pan, Yaray Agosto, Carolina Velasquez, Elana Mansoor, Rebecca Jane Bulotsky-Shearer, Sarah E. Messiah, and Jason F. Jent. 2025. "Impact of a Mental Health Consultation Program on Child Psychosocial Development over Two School Years" Behavioral Sciences 15, no. 11: 1497. https://doi.org/10.3390/bs15111497
APA StyleNatale, R., Pan, Y., Agosto, Y., Velasquez, C., Mansoor, E., Bulotsky-Shearer, R. J., Messiah, S. E., & Jent, J. F. (2025). Impact of a Mental Health Consultation Program on Child Psychosocial Development over Two School Years. Behavioral Sciences, 15(11), 1497. https://doi.org/10.3390/bs15111497







