Validation of the Effectiveness of a Behavioral Activation-Based Digital App for Treatment of Depressive Symptoms: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
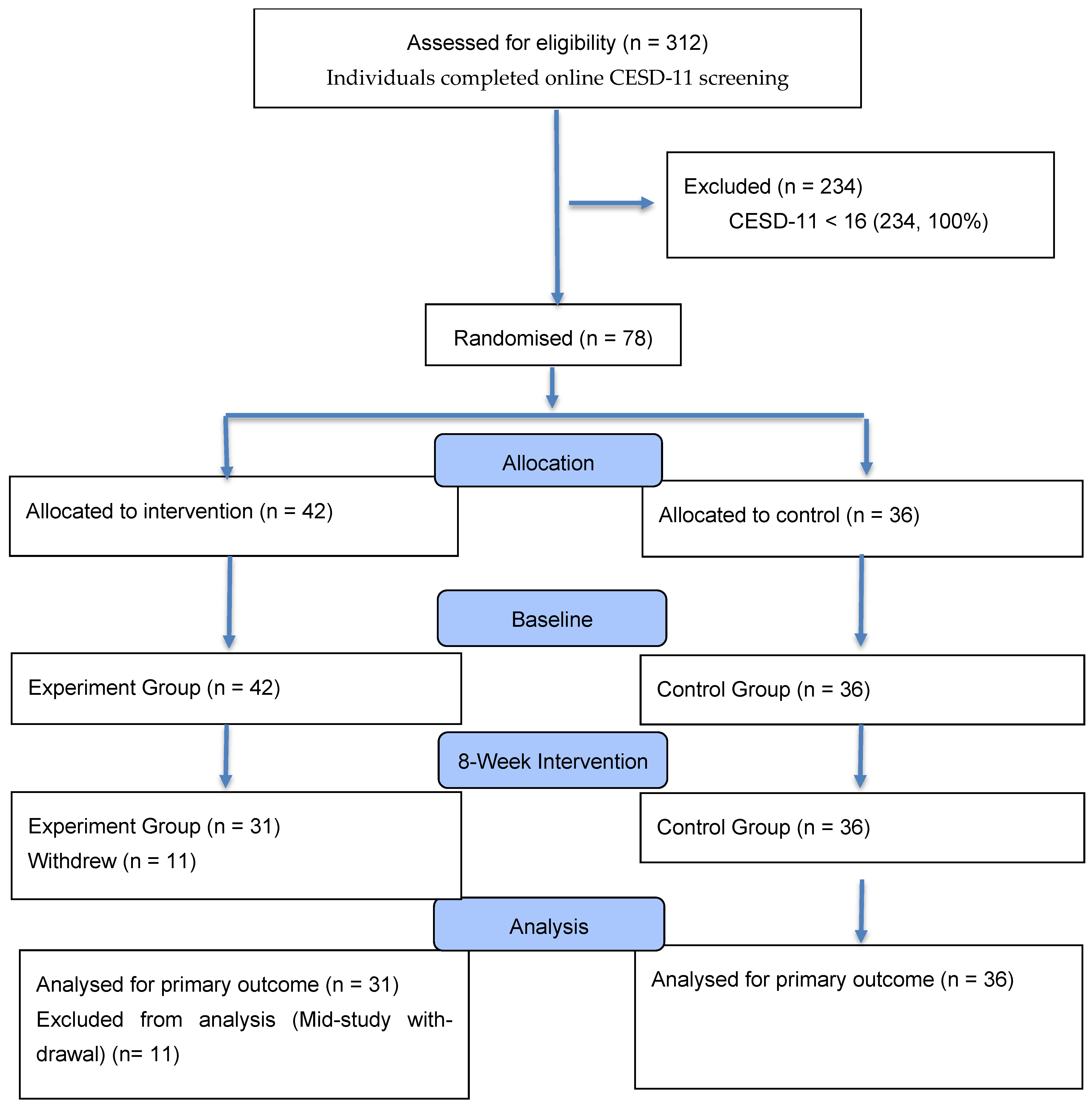
2.1. Participants
2.2. Measurements
2.2.1. Depression: Center for Epidemiologic Studies Depression Scale (CESD-11)
2.2.2. Stress: Korean Version of the Perceived Stress Scale (PSS)
2.2.3. Life Satisfaction: Korean Version of the Satisfaction with Life Scale (SWLS)
2.3. Procedure
The Maummove Treatment Program Consisted of Two Stages
2.4. Analysis
2.5. Power Analysis
3. Results
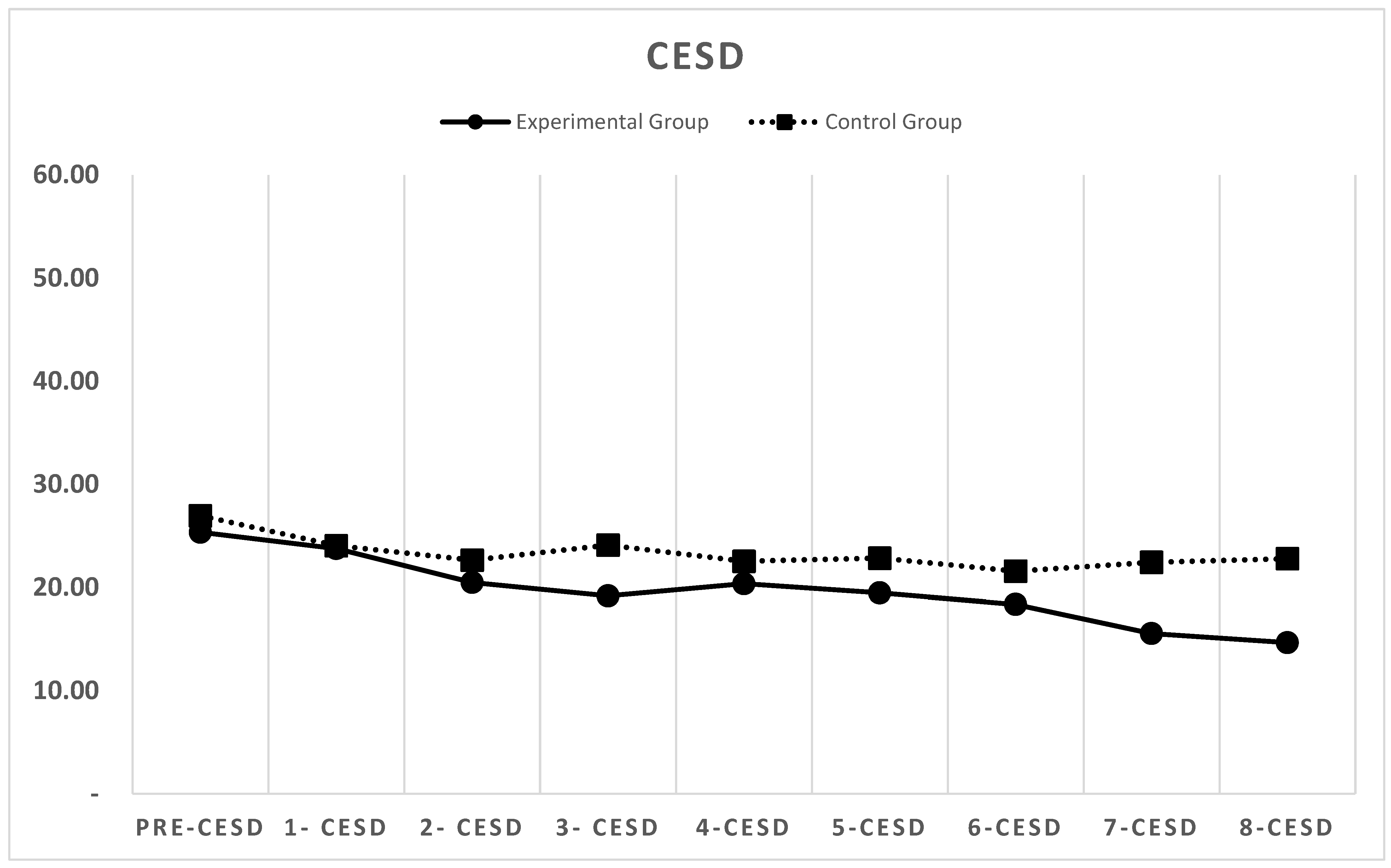
3.1. Depression
3.2. Perceived Stress
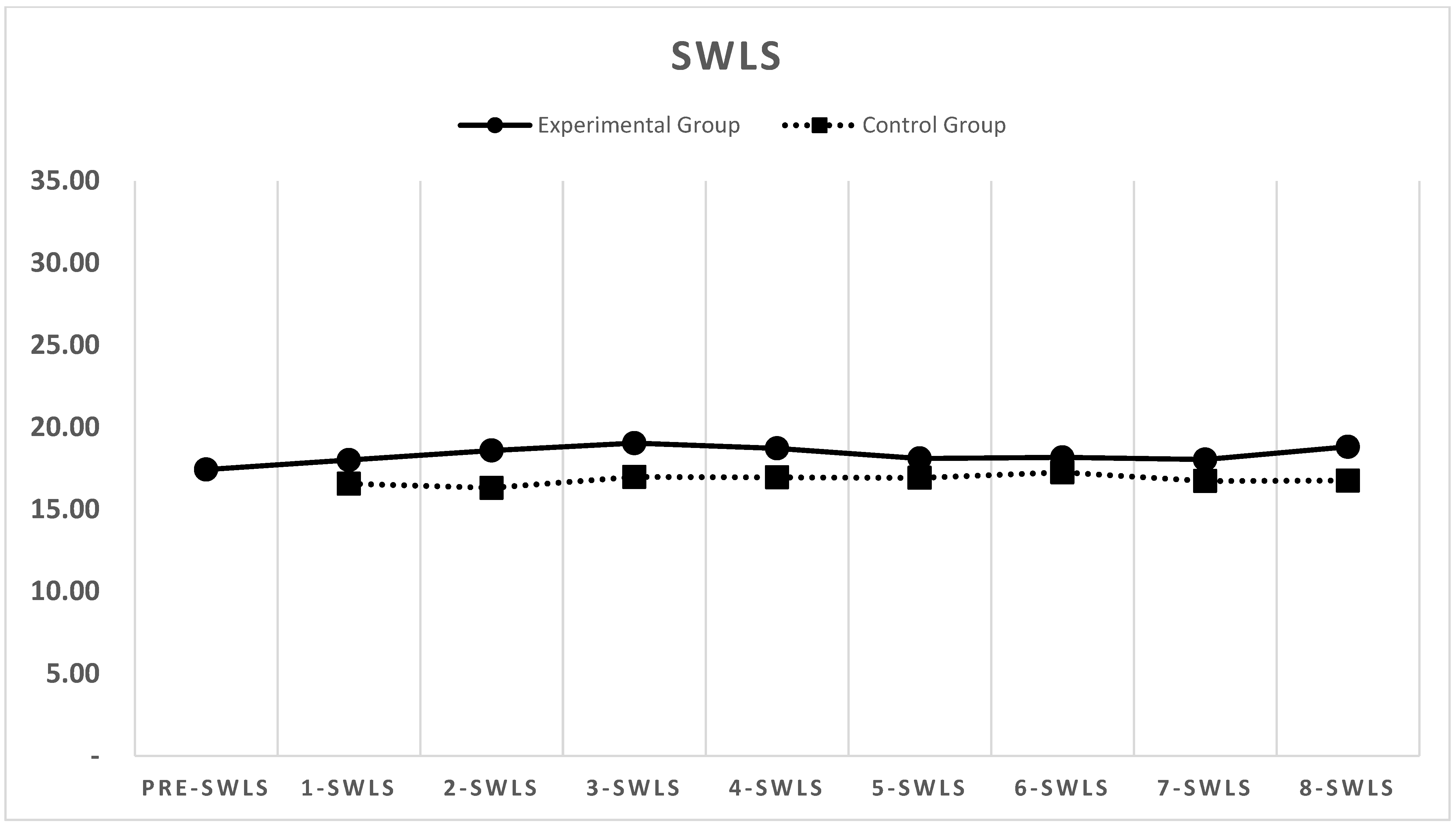
3.3. Life Satisfaction
3.4. Effectiveness of the Behavioral Activation-Based Application
Conservative ITT-Style Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alber, C. S., Krämer, L. V., Rosar, S. M., & Mueller-Weinitschke, C. (2023). Internet-based behavioral activation for depression: Systematic review and meta-analysis. Journal of Medical Internet Research, 25, e41643. [Google Scholar] [CrossRef]
- Auerbach, R. P., Mortier, P., Bruffaerts, R., Alonso, J., Benjet, C., Cuijpers, P., Demyttenaere, K., Ebert, D. D., Green, J. G., Hasking, P., Murray, E., Nock, M. K., Pinder-Amaker, S., Sampson, N. A., Stein, D. J., Vilagut, G., Zaslavsky, A. M., Kessler, R. C., & WHO WMH-ICS Collaborators. (2018). WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. Journal of Abnormal Psychology, 127(7), 623–638. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, H., Reichler, L., Munzinger, M., & Lin, J. (2019). The impact of guidance on internet-based mental health interventions: A systematic review. Internet Interventions, 1(4), 205–215. [Google Scholar] [CrossRef]
- Borrelli, B., Bartlett, Y. K., Fulford, D., Frasco, G., Armitage, C. J., & Wearden, A. (2024). Behavioral activation mobile app to motivate smokers to quit: Feasibility and pilot randomized controlled trial. JMIR Formative Research, 8, e54912. [Google Scholar] [CrossRef] [PubMed]
- Brenes, G. A., Danhauer, S. C., Lyles, M. F., Hogan, P. E., & Miller, M. E. (2015). Barriers to mental health treatment in rural older adults. The American Journal of Geriatric Psychiatry, 23(11), 1172–1178. [Google Scholar] [CrossRef]
- Brody, D. J., & Hughes, J. P. (2025). Depression prevalence in adolescents and adults: United States, August 2021–August 2023. In NCHS data brief, no. 527. National Center for Health Statistics. [Google Scholar] [CrossRef]
- Carl, E., Witcraft, S. M., Kauffman, B. Y., Gillespie, E. M., Becker, E. S., Cuijpers, P., Van Ameringen, M., Smits, J. A. J., & Powers, M. B. (2020). Psychological and pharmacological treatments for generalized anxiety disorder (GAD): A meta-analysis of randomized controlled trials. Cognitive Behaviour Therapy, 49(1), 1–21. [Google Scholar] [CrossRef]
- Cerqueira, L., Freire, S., Neves, D. F., Bastos, J. P. S., Santana, B., Spínola, R., Mendonça, M., & Santos, J. A. M. (2024). Empathy and its effects on software practitioners’ well-being and mental health. IEEE Software, 41(4), 95–104. [Google Scholar] [CrossRef]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [Google Scholar] [CrossRef]
- Colombo, L., Johannes, B. D., Krank, M., Torous, J., & Zitko, J. (2019). Artificial intelligence for mental healthcare: Clinical applications, barriers, facilitators, and future directions. Current Opinion in Psychology, 36, 70–74. [Google Scholar]
- Cuijpers, P., Van Straten, A., & Warmerdam, L. (2007). Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review, 27(3), 318–326. [Google Scholar] [CrossRef]
- Dahne, J., Collado, A., Lejuez, C. W., Risco, C. M., Diaz, V. A., Coles, L., Kustanowitz, J., Zvolensky, M. J., & Carpenter, M. J. (2019). Pilot randomized controlled trial of a Spanish-language Behavioral Activation mobile app (¡Aptívate!) for the treatment of depressive symptoms among United States Latinx adults with limited English proficiency. Journal of Affective Disorders, 250, 210–217. [Google Scholar] [CrossRef]
- Diener, E., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). Development of the satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. [Google Scholar] [CrossRef]
- Dimidjian, S., Hollon, S. D., Dobson, K. S., Schmaling, K. B., Kohlenberg, R. J., Addis, M. E., Gallop, R., McGlinchey, J. B., Markley, D. K., Gollan, J. K., Atkins, D. C., Dunner, D. L., & Jacobson, N. S. (2006). Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology, 74(4), 658–670. [Google Scholar] [CrossRef]
- Ekers, D., Webster, L., Van Straten, A., Cuijpers, P., Richards, D., & Gilbody, S. (2014). Behavioural activation for depression: An update of meta-analysis of effectiveness and subgroup analysis. PLoS ONE, 9(6), e100100. [Google Scholar] [CrossRef] [PubMed]
- Estrella-Proaño, A., Rivadeneira, M. F., Alvarado, J., Murtagh, M., Guijarro, S., Alomoto, L., & Cañarejo, G. (2024). Anxiety and depression in first-year university students: The role of family and social support. Frontiers in Psychology, 15, 1462948. [Google Scholar] [CrossRef]
- Firth, J., Torous, J., Nicholas, J., Carney, R., Pratap, A., Rosenbaum, S., & Sarris, J. (2017). The efficacy of smartphone-based mental health interventions for depressive symptoms: A meta-analysis of randomized controlled trials. World Psychiatry, 16(3), 287–298. [Google Scholar] [CrossRef]
- Fleming, T., Bavin, L., Lucassen, M., Stasiak, K., Hopkins, S., & Merry, S. (2019). Beyond the trial: Systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. Journal of Medical Internet Research, 20(6), e199. [Google Scholar] [CrossRef] [PubMed]
- Gawrysiak, M., Nicholas, C., & Hopko, D. R. (2009). Behavioral activation for moderately depressed university students: Randomized controlled trial. Journal of Counseling Psychology, 56(3), 468–475. [Google Scholar] [CrossRef]
- Gilbody, S., Littlewood, E., Hewitt, C., Brierley, G., Tharmanathan, P., Araya, R., Barkham, M., Bower, P., Cooper, C., Gask, L., Kessler, D., Lester, H., Lovell, K., Parry, G., Richards, D. A., Andersen, P., Brabyn, S., Knowles, S., Shepherd, C., … White, D. (2015). Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): Large scale pragmatic randomised controlled trial. BMJ, 351, h5627. [Google Scholar] [CrossRef]
- Hopko, D. R., Lejuez, C. W., Lepage, J. P., Hopko, S. D., & McNeil, D. W. (2003). A brief behavioral activation treatment for depression: A randomized pilot trial within an inpatient psychiatric hospital. Behavior Modification, 27(4), 458–469. [Google Scholar] [CrossRef]
- Huguet, A., Miller, A., Kisely, S., Rao, S., Saadat, N., & McGrath, P. J. (2018). A systematic review and meta-analysis on the efficacy of Internet-delivered behavioral activation. Journal of Affective Disorders, 235, 27–38. [Google Scholar] [CrossRef]
- Jeong, K., & Shin, J. (2023). Public perceptions of psychological service apps and digital therapeutics. Korean Journal of Health Psychology, 28(6), 1067–1093, (Original work published in Korean). [Google Scholar]
- Jung, M., Lee, J., Kim, S., Park, H., Choi, Y., & Lee, K. (2024). Behavioral activation and brain network changes in depression. Journal of Clinical Neurology, 20(4), 362–377. [Google Scholar] [CrossRef]
- Kim, T., Jo, Y., & Oh, C. (2019). The effects of behavioral activation interventions for subclinical college students with depressive symptoms. Cognitive Behavior Therapy in Korea, 19(2), 159–182. [Google Scholar]
- Kohout, F. J., Berkman, L. F., Evans, D. A., & Cornoni-Huntley, J. (1993). Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. Journal of Aging and Health, 5(2), 179–193. [Google Scholar] [CrossRef] [PubMed]
- Kooistra, L. C., Wiersma, J. E., Ruwaard, J., Neijenhuijs, K., Lokkerbol, J., van Oppen, P., Smit, F., & Riper, H. (2019). Cost and effectiveness of blended versus standard cognitive behavioral therapy for outpatient depression: Pilot randomized controlled trial. Journal of Medical Internet Research, 21(10), e14261. [Google Scholar] [CrossRef]
- Lejuez, C. W., Hopko, D. R., Acierno, R., Daughters, S. B., & Pagoto, S. L. (2011). Ten year revision of the brief behavioral activation treatment for depression: Revised treatment manual. Behavior Modification, 35(2), 111–161. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J., Cuijpers, P., Carlbring, P., Messer, M., & Fuller-Tyszkiewicz, M. (2019). The efficacy of app-supported smartphone interventions for mental health problems: A meta-analysis of randomized controlled trials. World Psychiatry, 18(3), 325–336. [Google Scholar] [CrossRef]
- Liu, X., Li, Y., & Cao, X. (2024). Bidirectional reduction effects of perceived stress and general self-efficacy among college students: A cross-lagged study. Humanities and Social Sciences Communications, 11, 271. [Google Scholar] [CrossRef]
- Martell, C. R., Dimidjian, S., & Herman-Dunn, R. (2021). Behavioral activation for depression: A clinician’s guide (2nd ed.). Guilford Press. [Google Scholar]
- McGinty, E. E., Presskreischer, R., Han, H., & Barry, C. L. (2022). Trends in psychological distress among US adults during different phases of the COVID-19 pandemic. JAMA Network Open, 5(1), e2144776. [Google Scholar] [CrossRef] [PubMed]
- Mohr, D. C., Riper, H., & Schueller, S. M. (2018). A solution-focused research approach to achieve an implementable revolution in digital mental health. JAMA Psychiatry, 75(2), 113–114. [Google Scholar] [CrossRef]
- Na, H., Jo, M., Lee, C., & Kim, D. (2022). Development and evaluation: A behavioral activation mobile application for self-management of stress for college students. Healthcare, 10(10), 1880. [Google Scholar] [CrossRef] [PubMed]
- OECD. (2021). Fitter minds, fitter jobs: From awareness to change in integrated mental health, skills and work policies. OECD Publishing. [Google Scholar] [CrossRef]
- Park, J. O., & Seo, Y. S. (2010). Validation of the perceived stress scale (PSS) on samples of Korean university students. Korean Journal Psychology, 29(3), 611–629. [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar] [CrossRef]
- Richards, D. A., Ekers, D., McMillan, D., Taylor, R. S., Byford, S., Warren, F. C., Barrett, B., Farrand, P. A., Gilbody, S., Kuyken, W., O’Mahen, H., Watkins, E. R., Wright, K. A., Hollon, S. D., Reed, N., Rhodes, S., Fletcher, E., & Finning, K. (2016). Cost and outcome of behavioural activation versus cognitive behavioural therapy for depression (COBRA): A randomised, controlled, non-inferiority trial. The Lancet, 388(10047), 871–880. [Google Scholar] [CrossRef] [PubMed]
- Santopetro, N., Jones, D., Garron, A., Meyer, A., Joyner, K., & Hajcak, G. (2024). Examining a fully automated mobile-based behavioral activation intervention in depression: Randomized controlled trial. JMIR Mental Health, 11, e54252. [Google Scholar] [CrossRef]
- Schueller, S. M., Aguilera, A., & Mohr, D. C. (2017). Ecological momentary interventions for depression and anxiety. Depression and Anxiety, 34(6), 540–545. [Google Scholar] [CrossRef]
- Stein, A. T., Carl, E., Cuijpers, P., Karyotaki, E., & Smits, J. A. J. (2021). Looking beyond depression: A meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychological Medicine, 51(9), 1491–1504. [Google Scholar] [CrossRef]
- Suh, E. (1994). Emotion norms, value, familiarity, and subjective well-being: Across-cultural examination [Unpublished Master Thesis, University of Illinois, Urbana-Champaign]. [Google Scholar]
- Takaoka, A. J. W., Jaccheri, L., & Sharma, K. (2024). Exploring self-care, anxiety, depression, and the gender gap in the software engineering pipeline. International Journal of Environmental Research and Public Health, 21(11), 1468. [Google Scholar] [CrossRef]
- Torous, J., Lipschitz, J., Ng, M., & Firth, J. (2020). Dropout rates in clinical trials of smartphone apps for depressive symptoms: A systematic review and meta-analysis. Journal of Affective Disorders, 263, 413–419. [Google Scholar] [CrossRef]
- Trinkenreich, B., Gerosa, M. A., & Steinmacher, I. (2024, April 14–20). Unraveling the drivers of sense of belonging in software delivery teams: Insights from a large-scale survey [Paper presentation]. IEEE/ACM 46th International Conference on Software Engineering (pp. 1–12), Lisbon, Portugal. [Google Scholar] [CrossRef]
- Vanderkruik, R. C., Ferguson, C., Kobylski, L. A., Locascio, J. J., Hamlett, G. E., Killenberg, P. C., Lewis, R., Jones, N., Rossa, E. T., Dineen, H., Picard, R., & Cohen, L. S. (2024). Testing a behavioral activation gaming app for depression during pregnancy: Multimethod pilot study. JMIR Formative Research, 8, e44029. [Google Scholar] [CrossRef] [PubMed]
- Wentzel, J., van der Vaart, R., Bohlmeijer, E. T., & van Gemert-Pijnen, J. E. (2016). Mixing online and face-to-face therapy: How to benefit from blended care in mental health care. JMIR Mental Health, 3(1), e9. [Google Scholar] [CrossRef] [PubMed]
- Wüllner, S., Hermenau, K., Krutkova, M., Petras, I. K., Hecker, T., & Siniatchkin, M. (2024). Mobile applications in adolescent psychotherapy during the COVID-19 pandemic: A systematic review. Frontiers in Public Health, 12, 1345808. [Google Scholar] [CrossRef] [PubMed]

| Step | Week | Weekly Process |
|---|---|---|
| 1 | 1 | During the monitoring week, participants recorded their daily activities and emotions three times a day to confirm that their behaviors and emotions were connected. |
| 2 |
| |
| 3 | Participants planned and carried out one or two pleasant activities related to their values. | |
| 4 | Participants planned and carried out up to three pleasant activities related to their values. | |
| 5 | Participants planned and carried out up to three pleasant activities related to their values. | |
| 2 | 6 |
|
| 7 | They planned and carried out 1–2 goal actions that aligned with the relevant values. | |
| 8 | They planned and carried out up to three goal actions. |
| Variable | Week 1 M (SD) | Week 8 M (SD) | Week 1–Week 8 d |
|---|---|---|---|
| depression (CESD) | 23.75 (11.85) | 14.66 (8.96) | 0.87 |
| Stress (PSS) | 21.71 (5.29) | 17.10 (5.15) | 0.88 |
| Life Satisfaction (SWLS) | 18.00 (6.43) | 18.81 (6.31) | 0.13 |
| Variable | Week 1 M (SD) | Week 8 M (SD) | Week 1–Week 8 d |
|---|---|---|---|
| depression (CESD) | 24.04 (13.12) | 22.78 (15.75) | 0.09 |
| Stress (PSS) | 21.86 (6.08) | 21.14 (5.15) | 0.13 |
| Life Satisfaction (SWLS) | 16.56 (6.47) | 16.75 (7.59) | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
So, Y.; Shin, J.; Won, S.-D.; Im, W.; Seok, K.-H.; Jin, M.J.; Lee, S.H.; Bae, S.-M. Validation of the Effectiveness of a Behavioral Activation-Based Digital App for Treatment of Depressive Symptoms: A Randomized Controlled Trial. Behav. Sci. 2025, 15, 1496. https://doi.org/10.3390/bs15111496
So Y, Shin J, Won S-D, Im W, Seok K-H, Jin MJ, Lee SH, Bae S-M. Validation of the Effectiveness of a Behavioral Activation-Based Digital App for Treatment of Depressive Symptoms: A Randomized Controlled Trial. Behavioral Sciences. 2025; 15(11):1496. https://doi.org/10.3390/bs15111496
Chicago/Turabian StyleSo, Yongjoon, Jaeeun Shin, Sung-Doo Won, Wooyoung Im, Kwang-Ho Seok, Min Jin Jin, Seung Ho Lee, and Sung-Man Bae. 2025. "Validation of the Effectiveness of a Behavioral Activation-Based Digital App for Treatment of Depressive Symptoms: A Randomized Controlled Trial" Behavioral Sciences 15, no. 11: 1496. https://doi.org/10.3390/bs15111496
APA StyleSo, Y., Shin, J., Won, S.-D., Im, W., Seok, K.-H., Jin, M. J., Lee, S. H., & Bae, S.-M. (2025). Validation of the Effectiveness of a Behavioral Activation-Based Digital App for Treatment of Depressive Symptoms: A Randomized Controlled Trial. Behavioral Sciences, 15(11), 1496. https://doi.org/10.3390/bs15111496






