Effectiveness of Mobile Applications for Suicide Prevention: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
- Populations: Studies targeting individuals with suicidal thoughts, plans, or prior suicide attempts without age restrictions.
- Intervention: Studies were eligible if mobile applications explicitly featured suicide-related components, even when only depression or anxiety outcomes were assessed using standardized instruments, or if suicide-related outcomes were measured regardless of whether the application explicitly targeted suicide prevention. Studies were excluded if the application did not include suicide-related content or assessed suicide-related outcomes. Interventions limited to brief text messaging or email reminders were also excluded. When suicide was assessed using a single item from an existing instrument (e.g., Item 9 of PHQ-9), the study was included, but the single-item measure was excluded from the effect size calculations.
- Comparator: Studies that include a comparison group (e.g., psychoeducation, waiting list).
- Outcomes: Outcomes of interest were classified as (1) direct measures of suicidality (e.g., suicidal ideation and suicide attempts) and (2) indirect measures of suicide risk through depression and anxiety. Only studies that assessed these outcomes using self-report instruments with established psychometric reliability and validity were included. The instruments used in each study are listed in Table S1.
- Study design: Studies using randomized or nonrandomized controlled designs.
- Language: Studies published in English.
- Date range: Studies published between January 2020 and February 2025.
- Availability: Full-text articles.
2.3. Article Selection
2.4. Risk of Bias and Methodological Quality
2.5. Data Extraction
2.6. Statistical Analysis
3. Results
3.1. Selection and Inclusion of Studies
3.2. Characteristics of the Included Studies
3.3. Assessment of Study Validity
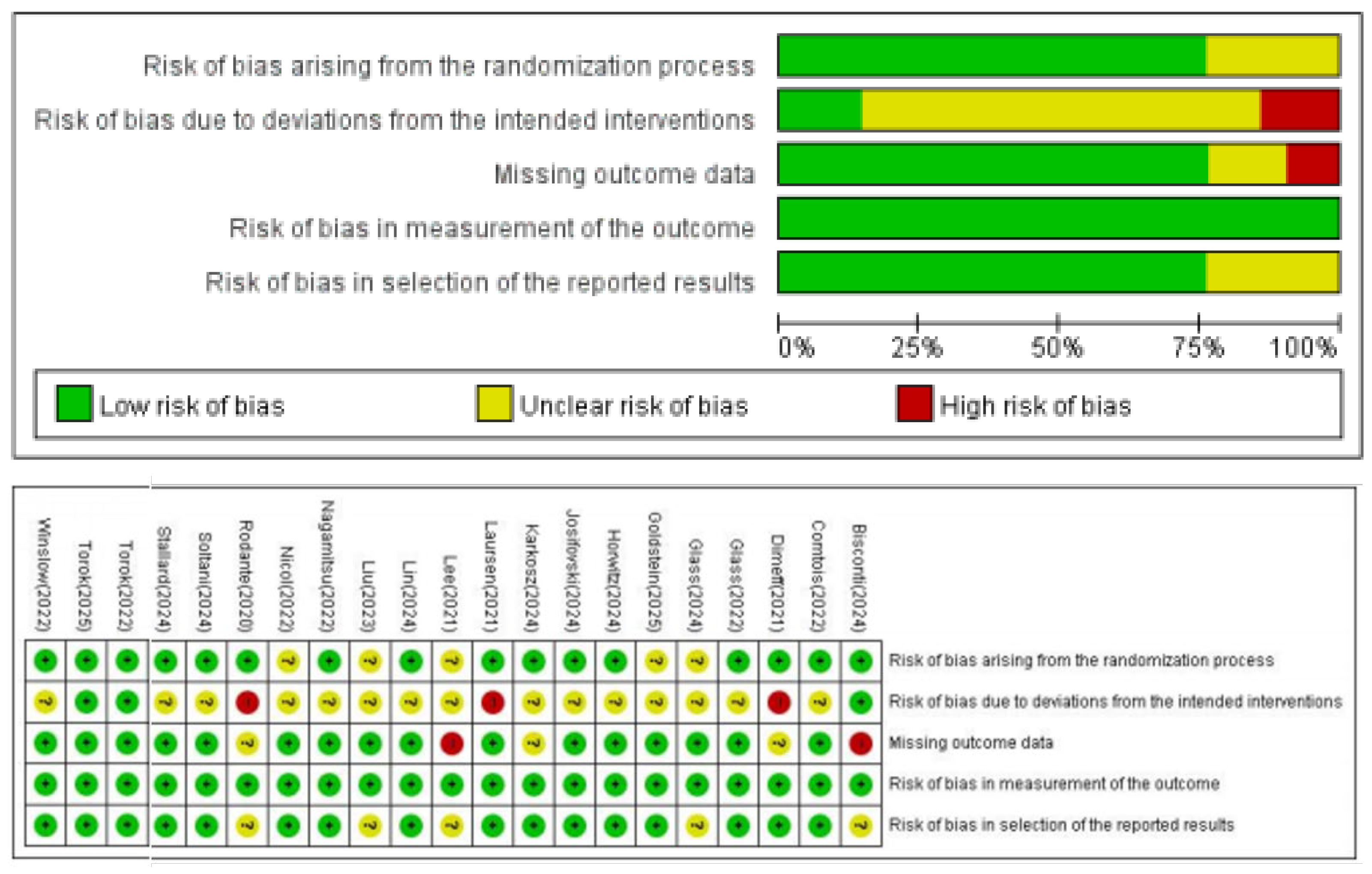
3.3.1. Risk of Bias Assessment
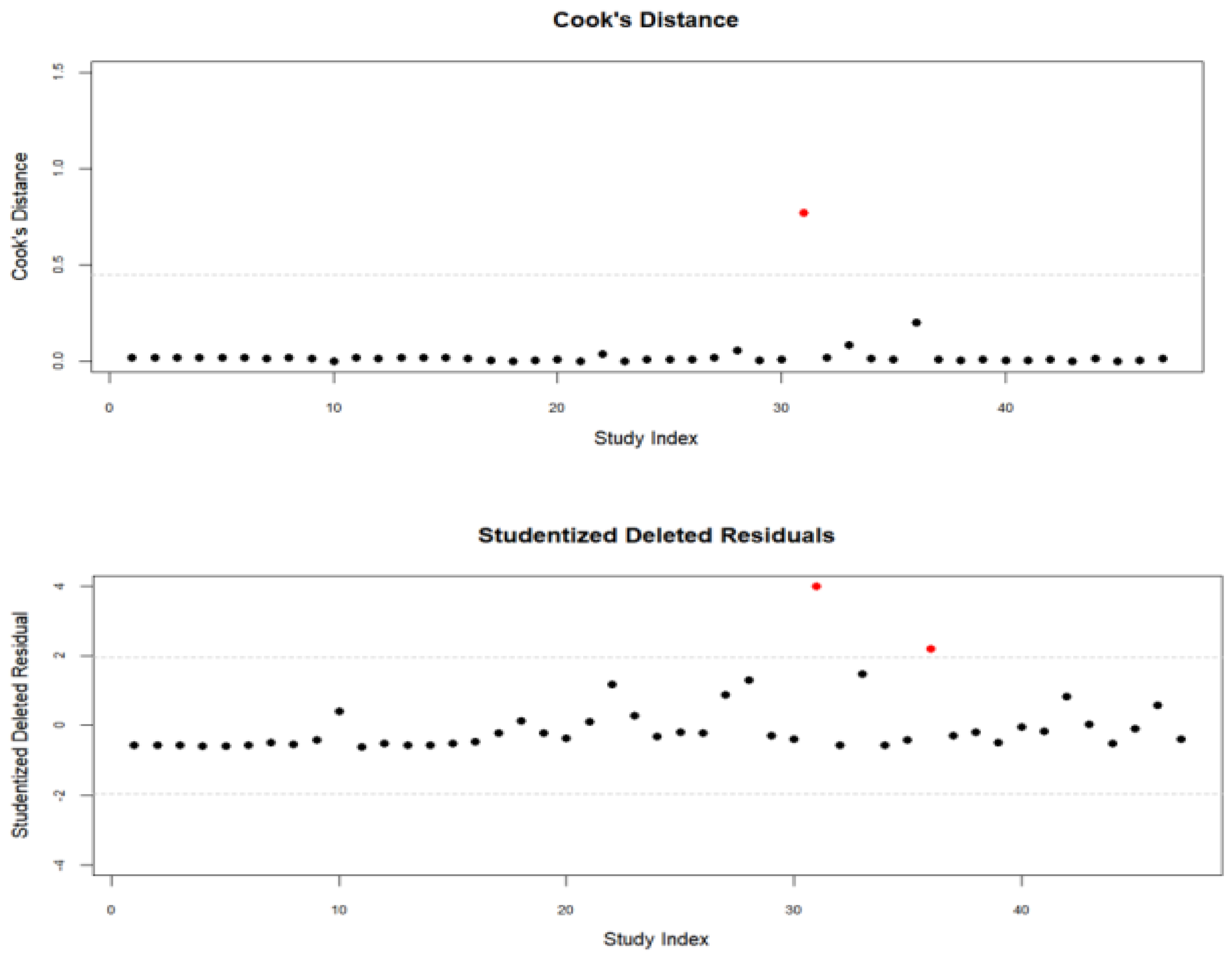
3.3.2. Outlier Analyses
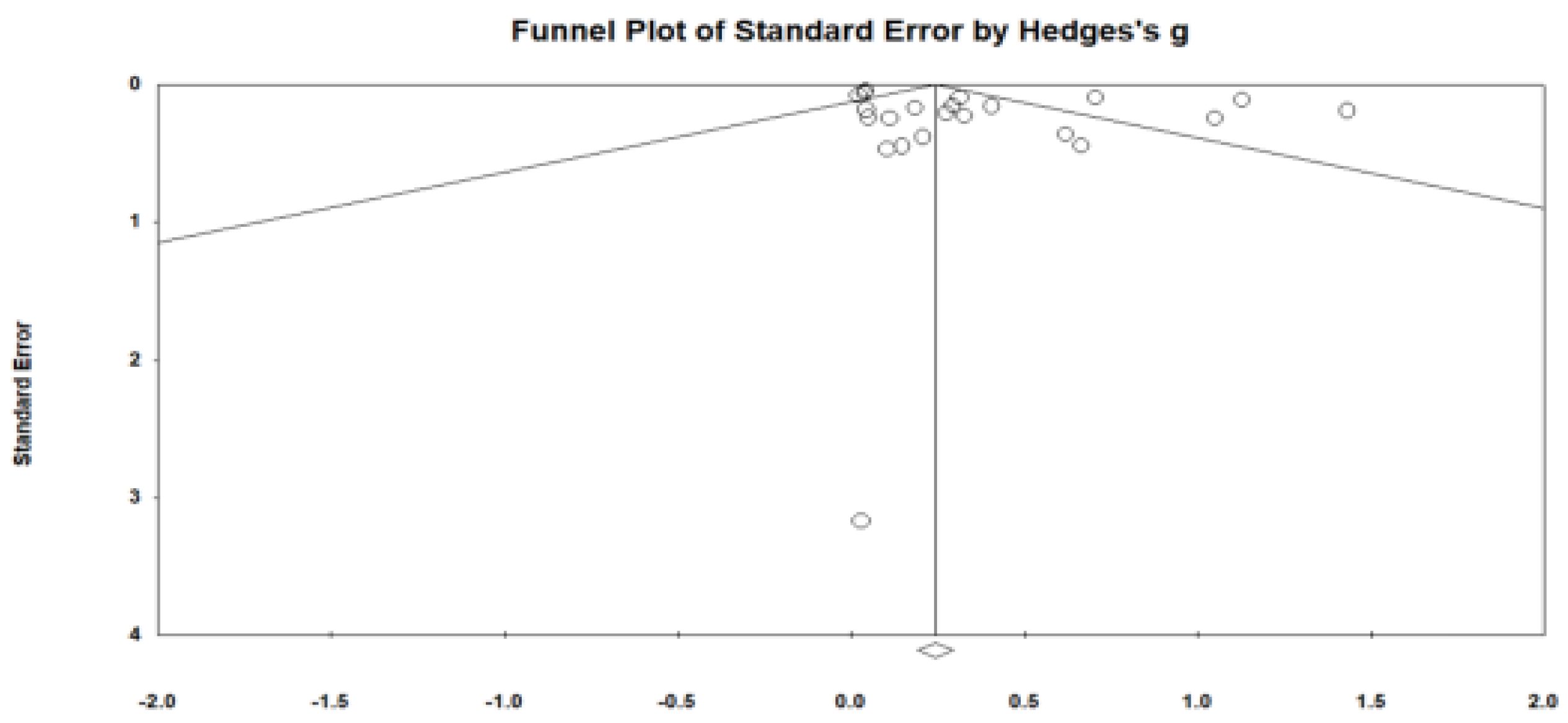
3.3.3. Publication Bias
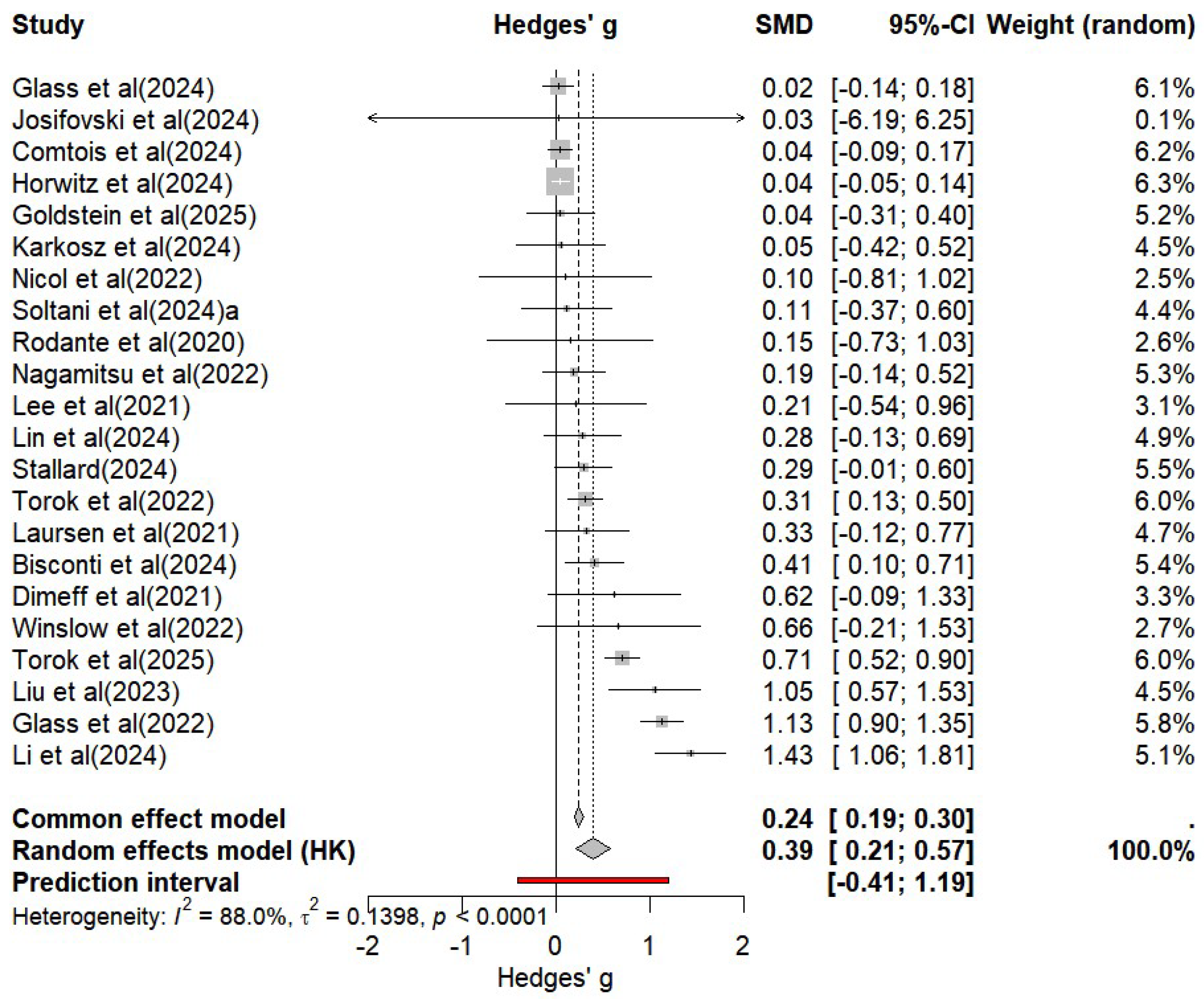
3.4. Main Effects of Mobile Applications
3.4.1. Primary Effects
3.4.2. Follow-Up Effects
3.5. Moderator Analysis
3.5.1. Participant Characteristics
3.5.2. Intervention Characteristics
3.5.3. Methodological Characteristics
3.5.4. Outcome Type
4. Discussion
4.1. Summary of Main Findings
4.2. Clinical Considerations
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abascal-Peiró, S., Peñuelas-Calvo, I., Alacreu-Crespo, A., Sáiz, P. A., De la Torre-Luque, A., Ruiz-Veguilla, M., Barrigón, M. L., Courtet, P., López-Castroman, J., Baca-García, E., & Porras-Segovia, A. (2024). Digital platform for the prevention of suicidal behaviour and non-suicidal self-injuries in adolescents: The SmartCrisis-Teen study protocol. Behavioral Science, 14(9), 740. [Google Scholar] [CrossRef]
- Barua, P. D., Vicnesh, J., Lih, O. S., Palmer, E. E., Yamakawa, T., Kobayashi, M., & Acharya, U. R. (2022). Artificial intelligence assisted tools for the detection of anxiety and depression leading to suicidal ideation in adolescents: A review. Cognitive Neurodynamics, 18(1), 1–22. [Google Scholar] [CrossRef]
- Bisconti, N., Odier, M., Becker, M., & Bullock, K. (2024). Feasibility and acceptability of a mobile app–based TEAM-CBT (Testing empathy assessment methods–Cognitive behavioral therapy) intervention (feeling good) for depression: Secondary data analysis. JMIR Mental Health, 11, e52369. [Google Scholar] [CrossRef]
- Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2009). Introduction to meta-analysis. John Wiley & Sons. [Google Scholar]
- Cardoso, N. O., Salvador, E. Z., Tagliapietra, K. R., Sanseverino, M. A., Vissoci, J. R. N., & Machado, W. L. (2023). Effectiveness of mobile applications as intervention tools in suicidal ideation: A systematic review and meta-analysis. Estudos de Psicologia (Campinas), 40, e210035. [Google Scholar] [CrossRef]
- Chen, M., & Chan, K. L. (2022). Effectiveness of digital interventions on unintentional injury, violence, and suicide: Meta-analysis. Trauma, Violence, & Abuse, 23(2), 605–619. [Google Scholar] [CrossRef]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar] [CrossRef]
- Comtois, K. A., Mata-Greve, F., Johnson, M., Pullmann, M. D., Mosser, B., & Arean, P. (2022). Effectiveness of mental health apps for distress during COVID-19 in US unemployed and essential workers: Remote pragmatic randomized clinical trial. JMIR mHealth uHealth, 10, e41689. [Google Scholar] [CrossRef] [PubMed]
- Conley, C. S., Raposa, E. B., Bartolotta, K., Broner, S. E., Hareli, M., Forbes, N., Christensen, K. M., & Assink, M. (2022). The impact of mobile technology-delivered interventions on youth wellbeing: Systematic review and 3-level meta-analysis. JMIR Mental Health, 9(7), e34254. [Google Scholar] [CrossRef]
- Cooper, H. M. (1998). Synthesizing research: A guide for literature reviews (3rd ed.). Sage. [Google Scholar]
- De la Torre, I., Castillo, G., Arambarri, J., López-Coronado, M., & Franco, M. A. (2017). Mobile apps for suicide prevention: Review of evidence and quality. JMIR mHealth and uHealth, 5(10), e130. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, M., Rhodes, K., Loughhead, M., McIntyre, H., & Procter, N. (2022). The effectiveness of the safety planning intervention for adults experiencing suicide-related distress: A systematic review. Archives of Suicide Research, 26(3), 1022–1045. [Google Scholar] [CrossRef]
- Fox, K. R., Huang, X., Guzman, E. M., Funsch, K. M., Cha, C. B., Ribeiro, J. D., & Franklin, J. C. (2020). Interventions for suicide and self-injury: A meta-analysis of randomized controlled trials across nearly 50 years of research. Psychological Bulletin, 146(12), 1117–1145. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, T. R., Kennard, B. D., Porta, G., Miller, A. O., Aguilar, K., Bigley, K., Vaughn-Coaxum, R. A., McMakin, D. L., Douaihy, A., Iyengar, S., Biernesser, C. L., Zelazny, J., & Brent, D. A. (2025). Bridging gaps in care following hospitalization for suicidal adolescents: As safe as possible (ASAP) and BRITE app. Journal of the American Academy of Child and Adolescent Psychiatry, 64(5), 612–624. [Google Scholar] [CrossRef] [PubMed]
- Graham, A. K., Greene, C. J., Kwasny, M. J., Kaiser, S. M., Lieponis, P., Powell, T., & Mohr, D. C. (2020). Coached mobile app platform for the treatment of de-pression and anxiety among primary care patients: A randomized clinical trial. JAMA Psychiatry, 77(9), 906–914. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. [Google Scholar] [CrossRef]
- Hofstra, E., van Nieuwenhuizen, C., Bakker, M., Ozgul, D., Elfeddali, I., de Jong, S. J., & van der Feltz-Cornelis, C. M. (2020). Effectiveness of suicide prevention interventions: A systematic review and meta-analysis. General Hospital Psychiatry, 63, 127–140. [Google Scholar] [CrossRef]
- Hom, M. A., Stanley, I. H., & Joiner, T. E. (2015). Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clinical Psychology Review, 40, 28–39. [Google Scholar] [CrossRef]
- Horwitz, A. G., Mills, E. D., Sen, S., & Bohnert, A. S. B. (2024). Comparative effectiveness of three digital interventions for adults seeking psychiatric services: A randomized clinical trial. JAMA Network Open, 7(7), e2422115. [Google Scholar] [CrossRef]
- Jacobson, N. C., Lekkas, D., Price, G., Heinz, M. V., Song, M., O’Malley, A. J., & Barr, P. J. (2020). Flattening the mental health curve: COVID-19 stay-at-home orders are associated with alterations in mental health search behavior in the United States. JMIR Mental Health, 7(6), e19347. [Google Scholar] [CrossRef]
- Jha, S., Chan, G., & Orji, R. (2023). Identification of risk factors for suicide and insights for developing suicide prevention technologies: A systematic review and meta-analysis. Human Behavior and Emerging Technologies, 2023, 3923097. [Google Scholar] [CrossRef]
- Josifovski, N., Torok, M., Batterham, P., Wong, Q., Beames, J. R., Theobald, A., Holland, S., Huckvale, K., Riley, J., Cockayne, N., Christensen, H., & Larsen, M. (2024). Efficacy of brighterside, a self-guided app for suicidal ideation: Randomized controlled trial. JMIR Mental Health, 11, e55528. [Google Scholar] [CrossRef]
- Knaak, S., Mantler, E., & Szeto, A. (2017). Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthcare Management Forum, 30(2), 111–116. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J., Fuller-Tyszkiewicz, M., Firth, J., Goldberg, S. B., Anderson, C., McClure, Z., & Torous, J. (2024). Systematic review and meta-analysis of adverse events in clinical trials of mental health apps. NPJ Digital Medicine, 7, 363. [Google Scholar] [CrossRef] [PubMed]
- McGillivray, L., Keng-Meng Hui, N., Wong, Q. J. J., Han, J., Qian, J., & Torok, M. (2023). The effectiveness of a smartphone intervention targeting suicidal ideation in young adults: Randomized controlled trial examining the influence of loneliness. JMIR Ment Health, 10, e44862. [Google Scholar] [CrossRef]
- Moshe, I., Terhorst, Y., Philippi, P., Domhardt, M., Cuijpers, P., Cristea, I., Pulkki-Råback, L., Baumeister, H., & Sander, L. B. (2021). Digital interventions for the treatment of depression: A meta-analytic review. Psychological Bulletin, 147(8), 749–786. [Google Scholar] [CrossRef]
- Nicol, G., Wang, R., Graham, S., Dodd, S., & Garbutt, J. (2022). Chatbot-delivered cognitive behavioral therapy in adolescents with depression and anxiety during the COVID-19 pandemic: Feasibility and acceptability study. JMIR Formative Research, 6(11), e40242. [Google Scholar] [CrossRef]
- Oh, J., Ho, J., Lee, S., & Park, J. H. (2024). Effects of digital psychotherapy on suicide: A systematic review and meta-analysis. Healthcare, 12(14), 1435. [Google Scholar] [CrossRef] [PubMed]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Priester, M. A., Browne, T., Iachini, A., Clone, S., DeHart, D., & Seay, K. D. (2016). Treatment Access barriers and disparities among individuals with co-occurring mental health and substance use disorders: An integrative literature review. Journal of Substance Abuse Treatment, 61, 47–59. [Google Scholar] [CrossRef]
- Rainbow, C., Tatnell, R., Blashki, G., Fuller-Tyszkiewicz, M., & Melvin, G. A. (2024). Digital safety plan effectiveness and use: Findings from a three-month longitudinal study. Psychiatry Research, 333, 115748. [Google Scholar] [CrossRef]
- Soltani, Z., Parizad, N., Radfar, M., Alinejad, V., Arzanlo, M., & Haghighi, M. (2024). The effect of the Yara smartphone application on anxiety, sleep quality, and suicidal thoughts in patients with major depressive disorder in Iran: A randomized controlled trial. BMC Psychiatry, 24, 1–12. [Google Scholar] [CrossRef]
- Song, H. S., & Bae, S. M. (2022). The moderating effects of the facets of mindfulness on the relationship between daily life stress and suicidal ideation among Korean college students. International Journal of Mental Health and Addiction, 20, 136–151. [Google Scholar] [CrossRef]
- Torok, M., Han, J., Baker, S., Werner-Seidler, A., Wong, I., Larsen, M. E., & Christensen, H. (2020). Suicide prevention using self-guided digital interventions: A systematic review and meta-analysis of randomized controlled trials. The Lancet Digital Health, 2(1), e25–e36. [Google Scholar] [CrossRef]
- Torok, M., Han, J., McGillivray, L., Wong, Q., Werner-Seidler, A., O’Dea, B., Calear, A., & Christensen, H. (2022). The effect of a therapeutic smartphone application on suicidal ideation in young adults: Findings from a randomized controlled trial in Australia. PLoS Medicine, 19(5), e1003978. [Google Scholar] [CrossRef] [PubMed]
- Torok, M., McGillivray, L., Gan, D. Z. Q., Han, J., Hetrick, S., & Wong, Q. J. J. (2025). Adherence and efficacy outcomes in young Australians with suicidal ideation using a self-management app and digital engagement strategy compared with a sham app: A three-arm randomised controlled trial. EClinicalMedicine, 79, 102963. [Google Scholar] [CrossRef]
- Torous, J., Wisniewski, H., Liu, G., & Keshavan, M. (2018). Mental health mobile phone app usage, concerns, and benefits among psychiatric outpatients: Comparative survey study. JMIR Mental Health, 5(4), e11715. [Google Scholar] [CrossRef]
- Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. [Google Scholar] [CrossRef]
- Viechtbauer, W., & Cheung, M. W.-L. (2010). Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods, 1(2), 112–125. [Google Scholar] [CrossRef]
- Wampold, B. E. (2007). Psychotherapy: The humanistic (and effective) treatment. American Psychologist, 62(8), 857–873. [Google Scholar] [CrossRef]
- Witt, K., Spittal, M. J., Carter, G., Priks, J., Hetrick, S., Currier, D., Robinson, J., & Milner, A. (2017). Effectiveness of online and mobile telephone applications (‘apps’) for the self-management of suicidal ideation and self-harm: A systematic review and meta-analysis. BMC Psychiatry, 17, 297. [Google Scholar] [CrossRef]
- World Health Organization. (2021). Suicide. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 3 August 2025).

| Name | Total |
|---|---|
| Number of studies | 22 |
| Publication year | |
| 2020 | 1 (4.5%) |
| 2021 | 3 (13.6%) |
| 2022 | 6 (27.3%) |
| 2023 | 1 (4.5%) |
| 2024 | 9 (40.9%) |
| 2025 | 2 (9.1%) |
| Country | |
| USA | 9 (40.9%) |
| Australia | 3 (13.6%) |
| Other | 10 (45.5%) |
| Participant characteristics | |
| Age | M = 25.8, SD = 9.5 |
| Child and Adolescents (k = 6, 27.3%) | M = 15.3, SD = 0.8 |
| Adults (k = 16, 72.7%) | M = 28.7, SD = 8.6 |
| Female | 75.3% |
| Study design | |
| RCTs | 22 (95.5%) |
| NRS | 1 (4.5%) |
| Follow-up assessments | 11 (50.0%) |
| 4 weeks | 1 (4.5%) |
| 8 weeks | 1 (4.5%) |
| 12 weeks | 3 (13.6%) |
| 16 weeks | 2 (9.1%) |
| 24 weeks | 2 (9.1%) |
| 1 year | 2 (9.1%) |
| Categories | Subgroup | k | ES | 95% CI | Q | df | p | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Age group | Adolescent | 6 | 0.36 | −0.22 | 0.93 | 0.01 | 1 | 0.92 |
| Adult | 19 | 0.33 | 0.6 | 0.50 | ||||
| Target population | Universal | 6 | 0.46 | 0.04 | 0.88 | 7.20 * | 2 | 0.02 |
| Selected | 10 | 0.36 | −0.01 | 0.74 | ||||
| Indicated | 9 | 0.09 | −0.01 | 0.18 | ||||
| Age group _Target population | Adult_Universal | 4 | 0.64 | 0.06 | 1.23 | 11.19 * | 4 | 0.02 |
| Adult_Selected | 9 | 0.20 | −0.06 | 0.45 | ||||
| Adolescent _Indicated | 3 | 0.19 | −0.18 | 0.55 | ||||
| Adult_Indicated | 6 | 0.07 | −0.05 | 0.20 | ||||
| Adolescent _Universal | 2 | 0.05 | −0.76 | 0.87 | ||||
| Categories | Subgroup | k | ES | 95% CI | Q | df | p | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Theorical framework | CBT | 10 | 0.30 | 0.12 | 0.48 | 0.20 | 3 | 0.98 |
| 3th wave | 4 | 0.33 | 0.19 | 0.47 | ||||
| Other | 4 | 0.32 | −0.44 | 1.08 | ||||
| Not reported | 7 | 0.40 | −0.16 | 0.96 | ||||
| Session frequency | Weekly | 8 | 0.58 | 0.18 | 1.00 | 11.9 ** | 3 | 0.01 |
| Whenever needed | 10 | 0.27 | −0.01 | 0.54 | ||||
| Daily | 6 | 0.07 | −0.04 | 0.18 | ||||
| Treatment Length | 4 weeks | 8 | 0.10 | −0.01 | 0.21 | 27.42 *** | 6 | 0.00 |
| 6 weeks | 4 | 0.12 | −0.11 | 0.35 | ||||
| 8 weeks | 4 | 0.80 | −1.17 | 2.27 | ||||
| 12 weeks | 7 | 0.61 | 0.11 | 1.11 | ||||
| Categories | Subgroup | k | ES | 95% CI | Q | df | p | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Control Condition | Waitinglist | 6 | 0.66 | 0.07 | 1.26 | 4.0 | 3 | 0.26 |
| TAU | 8 | 0.25 | 0.11 | 0.39 | ||||
| Attention placebo | 4 | 0.37 | −0.50 | 1.25 | ||||
| Attention placebo application | 7 | 0.18 | −0.06 | 0.41 | ||||
| Setting | Efficacy | 16 | 0.41 | 0.16 | 0.65 | 6.86 ** | 1 | 0.01 |
| Effectiveness | 9 | 0.09 | −0.01 | 0.18 | ||||
| Categories | Subgroup | k | ES | 95% CI | Q | df | p | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Direct outcome | Suicidality | 16 | 0.18 | 0.05 | 0.32 | 2.28 | 2 | 0.32 |
| Indirect outcome | Depression | 18 | 0.37 | 0.15 | 0.59 | |||
| Anxiety | 12 | 0.22 | 0.02 | 0.41 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sim, K.; Bae, S.-M. Effectiveness of Mobile Applications for Suicide Prevention: A Systematic Review and Meta-Analysis. Behav. Sci. 2025, 15, 1345. https://doi.org/10.3390/bs15101345
Sim K, Bae S-M. Effectiveness of Mobile Applications for Suicide Prevention: A Systematic Review and Meta-Analysis. Behavioral Sciences. 2025; 15(10):1345. https://doi.org/10.3390/bs15101345
Chicago/Turabian StyleSim, Kisun, and Sung-Man Bae. 2025. "Effectiveness of Mobile Applications for Suicide Prevention: A Systematic Review and Meta-Analysis" Behavioral Sciences 15, no. 10: 1345. https://doi.org/10.3390/bs15101345
APA StyleSim, K., & Bae, S.-M. (2025). Effectiveness of Mobile Applications for Suicide Prevention: A Systematic Review and Meta-Analysis. Behavioral Sciences, 15(10), 1345. https://doi.org/10.3390/bs15101345






