Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach
Abstract
1. Introduction
1.1. The Pandemic Burden for Informal Caregivers
1.2. Caregivers’ Resources: Coping Strategies, Emotional Regulation, Resilience
1.3. Literature Gap and the Present Study’s Aim
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Participants
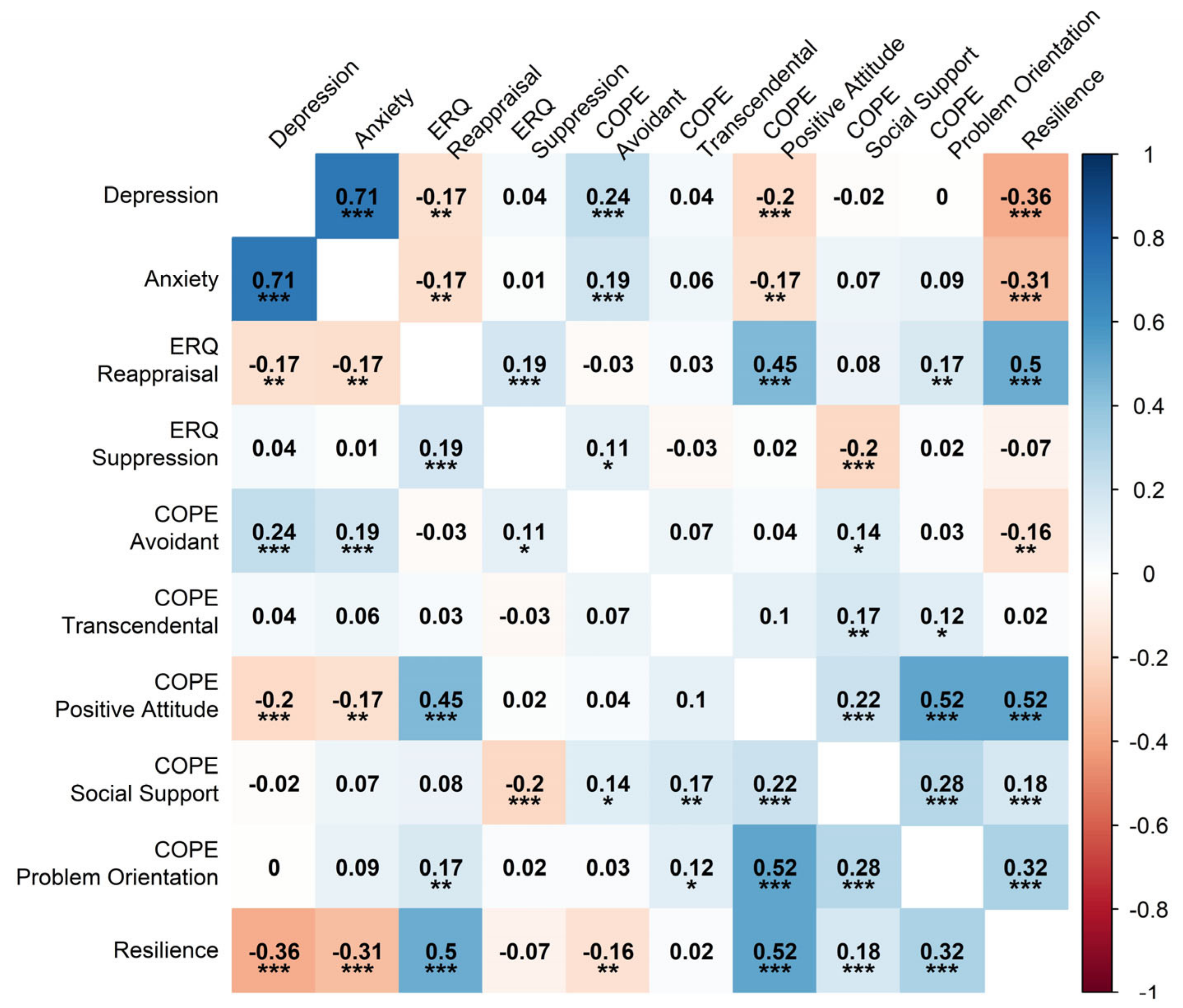
3.2. Preliminary Analysis
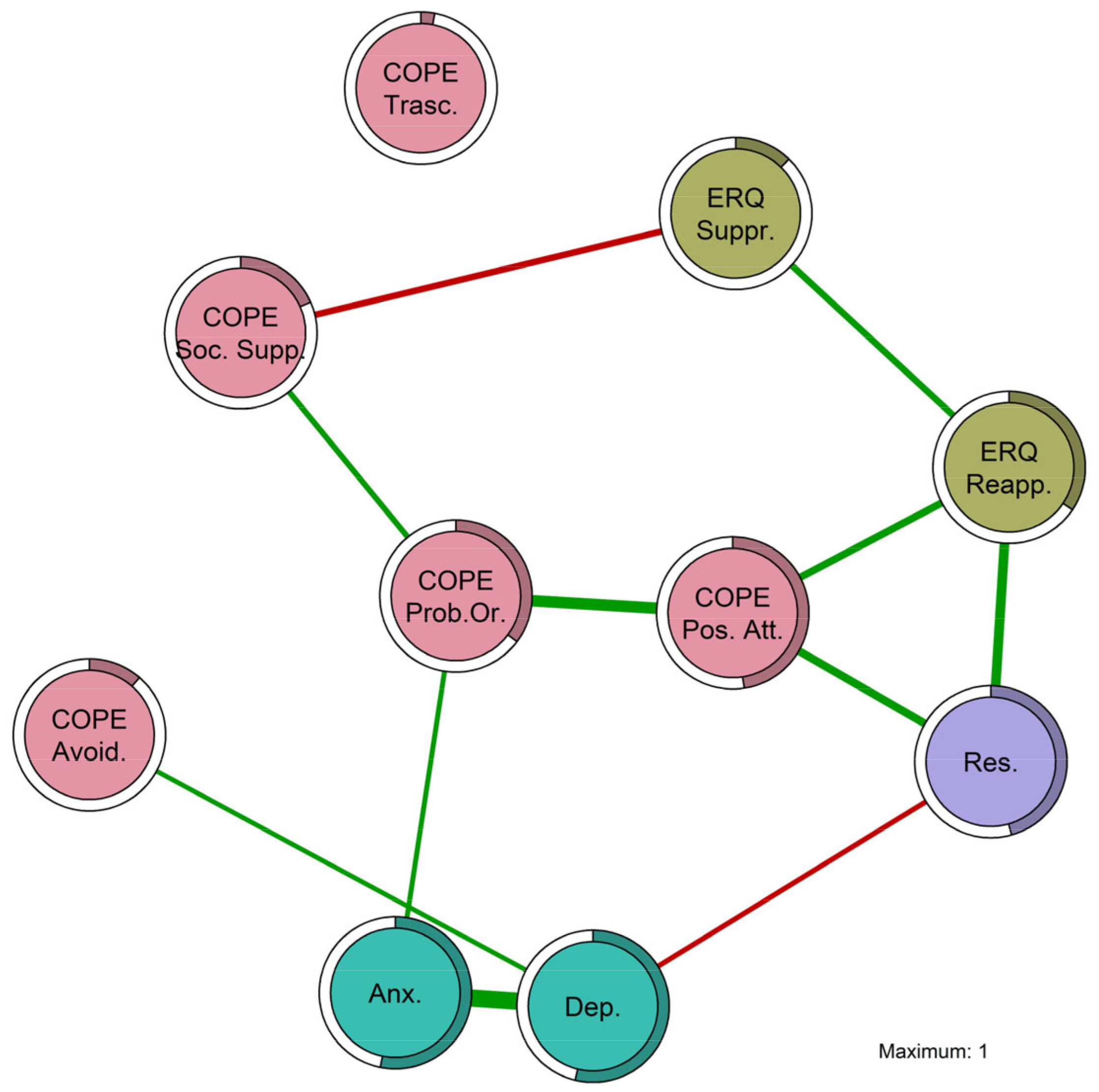
3.3. Psychometric Network Analysis
3.3.1. Network Stability
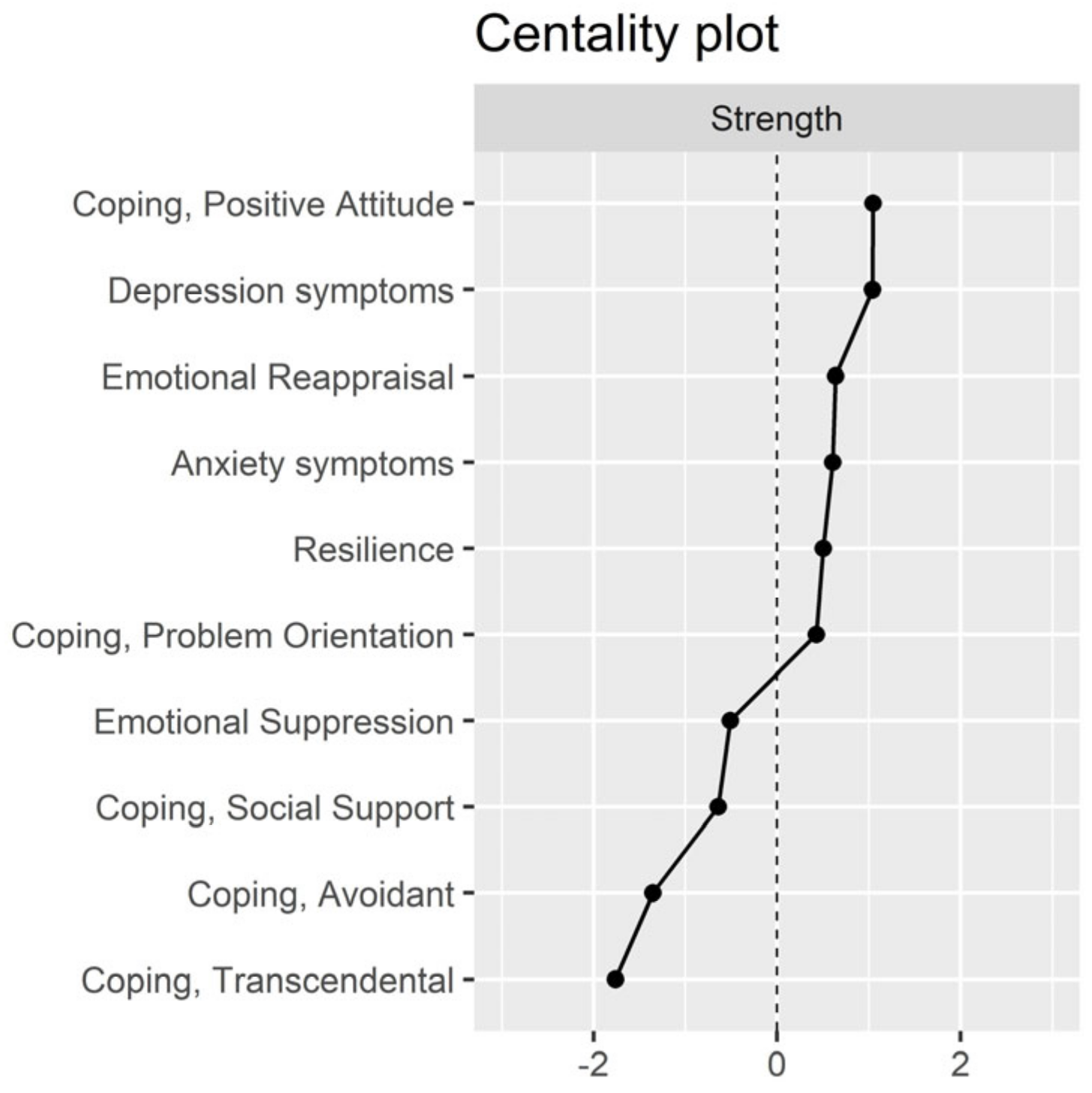
3.3.2. Centrality Indices
4. Discussion
4.1. Interpretation of Research Findings
4.2. Implications for Clinical and Research Fields
4.3. Limitations, Strengths, and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brandt, A.M.; Gardner, M. The Golden Age of Medicine? In Medicine in the Twentieth Century; Taylor & Francis: Abingdon, UK, 2000; ISBN 978-1-00-307845-6. [Google Scholar]
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.-P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.E.G.; Mahanani, W.R.; et al. The World Report on Ageing and Health: A Policy Framework for Healthy Ageing. Lancet Lond. Engl. 2016, 387, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Blum, K.; Sherman, D.W. Understanding the Experience of Caregivers: A Focus on Transitions. Semin. Oncol. Nurs. 2010, 26, 243–258. [Google Scholar] [CrossRef] [PubMed]
- Haley, W.E.; Elayoubi, J. Family Caregiving as a Global and Lifespan Public Health Issue. Lancet Public Health 2024, 9, e2–e3. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 DALYs and HALE Collaborators. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 359 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)32335-3/fulltext (accessed on 28 July 2024). [CrossRef] [PubMed]
- Revenson, T.A.; Griva, K.; Luszczynska, A.; Morrison, V.; Panagopoulou, E.; Vilchinsky, N.; Hagedoorn, M. The Emotional Experience of Caregiving. In Caregiving in the Illness Context; Palgrave Macmillan: London, UK, 2016; pp. 38–47. [Google Scholar]
- Bauer, J.M.; Sousa-Poza, A. Impacts of Informal Caregiving on Caregiver Employment, Health, and Family. J. Popul. Aging 2015, 8, 113–145. [Google Scholar] [CrossRef]
- Gemmill, R.; Cooke, L.; Williams, A.C.; Grant, M. Informal Caregivers of Hematopoietic Cell Transplant Patients: A Review and Recommendations for Interventions and Research. Cancer Nurs. 2011, 34, E13–E21. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sörensen, S. Differences between Caregivers and Noncaregivers in Psychological Health and Physical Health: A Meta-Analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef] [PubMed]
- Schulz, R.; Sherwood, P.R. Physical and Mental Health Effects of Family Caregiving. Am. J. Nurs. 2008, 108, 23–27, quiz 27. [Google Scholar] [CrossRef]
- Adelman, R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver Burden: A Clinical Review. JAMA 2014, 311, 1052. [Google Scholar] [CrossRef] [PubMed]
- Sambasivam, R.; Liu, J.; Vaingankar, J.A.; Ong, H.L.; Tan, M.-E.; Fauziana, R.; Picco, L.; Chong, S.A.; Subramaniam, M. The Hidden Patient: Chronic Physical Morbidity, Psychological Distress, and Quality of Life in Caregivers of Older Adults. Psychogeriatrics 2019, 19, 65–72. [Google Scholar] [CrossRef]
- Bailey, C.; Guo, P.; MacArtney, J.; Finucane, A.; Swan, S.; Meade, R.; Wagstaff, E. The Experiences of Informal Carers during the COVID-19 Pandemic: A Qualitative Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13455. [Google Scholar] [CrossRef]
- Hughes, M.C.; Liu, Y.; Baumbach, A. Impact of COVID-19 on the Health and Well-Being of Informal Caregivers of People with Dementia: A Rapid Systematic Review. Gerontol. Geriatr. Med. 2021, 7, 23337214211020164. [Google Scholar] [CrossRef]
- Serafini, A.; Peralta, G.; Martucci, P.; Tagliaferro, A.; Hutchinson, A.; Barbetta, C. COVID-19 Pandemic: Brief Overview of the Consequences on Family Informal Caregiving. COVID 2023, 3, 381–391. [Google Scholar] [CrossRef]
- Rossi, A.A.; Panzeri, A.; Taccini, F.; Parola, A.; Mannarini, S. The Rising of the Shield Hero. Development of the Post-Traumatic Symptom Questionnaire (PTSQ) and Assessment of the Protective Effect of Self-Esteem from Trauma-Related Anxiety and Depression. J. Child Adolesc. Trauma 2024, 17, 1–19. [Google Scholar] [CrossRef]
- Panzeri, A.; Rossi Ferrario, S. Supporting Rehabilitation Patients with COVID-19 during the Pandemic: Experiences from a Technology-Based Psychological Approach. In Proceedings of the CEUR Workshop Proceedings: Second Symposium on Psychology-Based Technologies—Psychobit, Naples, Italy, 28–29 September 2020; Volume 2730. [Google Scholar]
- Bottesi, G.; Marino, C.; Vieno, A.; Ghisi, M.; Spada, M.M. Psychological Distress in the Context of the COVID-19 Pandemic: The Joint Contribution of Intolerance of Uncertainty and Cyberchondria. Psychol. Health 2022, 37, 1396–1413. [Google Scholar] [CrossRef]
- Board on Health Care Services. Retooling for an Aging America: Building the Health Care Workforce; The National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- Panzeri, A.; Bettinardi, O.; Bottesi, G.; Bertolotti, G.; Brambatti, L.; Monfredo, M.; Mignemi, G.; Bruno, G.; Vidotto, G.; Spoto, A.; et al. Assessment of Perceived Support in the Context of Emergency: Development and Validation of the Psycho-Social Support Scale. Curr. Psychol. 2022, 42, 22514–22525. [Google Scholar] [CrossRef] [PubMed]
- Ratti, M.M.; Rossi, A.; Delli Zotti, G.B.; Sarno, L.; Spotti, D. Social Support, Psychological Distress and Depression in Hemodialysis Patients. Psicol. Della Salute 2017, 1, 112–122. [Google Scholar] [CrossRef]
- Perez, S.G.; Nuccio, A.G.; Stripling, A.M. A Rapid Review of the Detrimental Impact of Loneliness and Social Isolation in Caregivers of Older Adults. Am. J. Geriatr. Psychiatry 2021, 29, S122–S123. [Google Scholar] [CrossRef]
- Starr, L.R.; Davila, J. Responding to Anxiety with Rumination and Hopelessness: Mechanism of Anxiety-Depression Symptom Co-Occurrence? Cogn. Ther. Res. 2012, 36, 321–337. [Google Scholar] [CrossRef]
- Rossi, A.A.; Marconi, M.; Taccini, F.; Verusio, C.; Mannarini, S. From Fear to Hopelessness: The Buffering Effect of Patient-Centered Communication in a Sample of Oncological Patients during COVID-19. Behav. Sci. 2021, 11, 87. [Google Scholar] [CrossRef]
- Balzarotti, S.; John, O.P.; Gross, J.J. An Italian Adaptation of the Emotion Regulation Questionnaire. Eur. J. Psychol. Assess. 2010, 26, 61–67. [Google Scholar] [CrossRef]
- Gross, J.J.; John, O.P. Individual Differences in Two Emotion Regulation Processes: Implications for Affect, Relationships, and Well-Being. J. Pers. Soc. Psychol. 2003, 85, 348–362. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984; ISBN 0-8261-4192-7. [Google Scholar]
- Hamidou, Z.; Auquier, P.; Leroy, T.; Barlesi, F.; Salas, S.; Chinot, O.; Baumstarck, K. Dyadic Effects of Coping Strategies, Time Perspectives, and Personality on the Quality of Life of Cancer Patients and Their Caregivers. Psychooncology 2018, 27, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Iavarone, A.; Ziello, A.; Pastore, F.; Fasanaro, A.M.; Poderico, C. Caregiver Burden and Coping Strategies in Caregivers of Patients with Alzheimer’s Disease. Neuropsychiatr. Dis. Treat. 2014, 10, 1407–1413. [Google Scholar] [CrossRef]
- Wu, C.; Liu, Y.; Ma, S.; Jing, G.; Zhou, W.; Qu, L.; Wang, Z.; Cheng, M.; Wu, Y. The Mediating Roles of Coping Styles and Resilience in the Relationship between Perceived Social Support and Posttraumatic Growth among Primary Caregivers of Schizophrenic Patients: A Cross-Sectional Study. BMC Psychiatry 2021, 21, 58. [Google Scholar] [CrossRef] [PubMed]
- Foà, C.; Tonarelli, A.; Caricati, L.; Fruggeri, L. COPE-NVI-25: Validazione Italiana Della Versione Ridotta Della Coping Orientation to the Problems Experienced (COPE-NVI). Psicol. Della Salute 2015, 2, 123–140. [Google Scholar] [CrossRef]
- Sica, C.; Magni, C.; Ghisi, M.; Altoè, G.; Sighinolfi, C.; Chiri, L.R.; Franceschini, S. Coping Orientation to Problems Experienced-Nuova Versione Italiana (COPE-NVI): Uno Strumento per La Misura Degli Stili Di Coping. Psicoter. Cogn. Comport. 2008, 14, 27–53. [Google Scholar]
- Luthar, S.S.; Cicchetti, D.; Becker, B. The Construct of Resilience: A Critical Evaluation and Guidelines for Future Work. Child Dev. 2000, 71, 543–562. [Google Scholar] [CrossRef]
- Bonanno, G.A. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive after Extremely Aversive Events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef]
- Wilks, S.E.; Croom, B. Perceived Stress and Resilience in Alzheimer’s Disease Caregivers: Testing Moderation and Mediation Models of Social Support. Aging Ment. Health 2008, 12, 357–365. [Google Scholar] [CrossRef]
- Gallagher, S.; Wetherell, M.A. Risk of Depression in Family Caregivers: Unintended Consequence of COVID-19. BJPsych Open 2020, 6, e119. [Google Scholar] [CrossRef]
- Muldrew, D.H.L.; Fee, A.; Coates, V. Impact of the COVID-19 Pandemic on Family Carers in the Community: A Scoping Review. Health Soc. Care Community 2022, 30, 1275–1285. [Google Scholar] [CrossRef] [PubMed]
- Van den Bergh, N.; Marchetti, I.; Koster, E.H.W. Bridges over Troubled Waters: Mapping the Interplay Between Anxiety, Depression and Stress Through Network Analysis of the DASS-21. Cogn. Ther. Res. 2021, 45, 46–60. [Google Scholar] [CrossRef]
- Mannarini, S.; Taccini, F.; Rossi, A.A. Stigma toward Internalizing and Externalizing Disorders: How Do Adolescents Perceive Their Peers? A Network Analysis Approach. J. Res. Adolesc. Off. J. Soc. Res. Adolesc. 2023, 33, 803–815. [Google Scholar] [CrossRef]
- Costantini, G.; Perugini, M. Network Analysis. In The Wiley Handbook of Personality Assessment; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2016; pp. 74–89. ISBN 978-1-119-17348-9. [Google Scholar]
- Bottesi, G.; Marchetti, I.; Sica, C.; Ghisi, M. What Is the Internal Structure of Intolerance of Uncertainty? A Network Analysis Approach. J. Anxiety Disord. 2020, 75, 102293. [Google Scholar] [CrossRef]
- Callegari, C.; Bertù, L.; Lucano, M.; Ielmini, M.; Braggio, E.; Vender, S. Reliability and Validity of the Italian Version of the 14-Item Resilience Scale. Psychol. Res. Behav. Manag. 2016, 9, 277–284. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Shevlin, M.; Butter, S.; McBride, O.; Murphy, J.; Gibson-Miller, J.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; et al. Measurement Invariance of the Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder Scale (GAD-7) across Four European Countries during the COVID-19 Pandemic. BMC Psychiatry 2022, 22, 154. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2023. [Google Scholar]
- R Core Team. RStudio Team RStudio: Integrated Development for R; R Core Team: Vienna, Austria, 2023. [Google Scholar]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating Psychological Networks and Their Accuracy: A Tutorial Paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. Qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Jones, P.J. Networktools: Tools for Identifying Important Nodes in Networks; R Core Team: Vienna, Austria, 2018. [Google Scholar]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016; ISBN 978-3-319-24277-4. [Google Scholar]
- Revelle, W. Package “Psych”—Procedures for Psychological, Psychometric and Personality Research; R Core Team: Vienna, Austria, 2015; pp. 1–358. [Google Scholar]
- Mullarkey, M.C.; Marchetti, I.; Beevers, C.G. Using Network Analysis to Identify Central Symptoms of Adolescent Depression. J. Clin. Child. Adolesc. Psychol. 2019, 48, 656–668. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, I. Hopelessness: A Network Analysis. Cogn. Ther. Res. 2019, 43, 611–619. [Google Scholar] [CrossRef]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O.J. State of the aRt Personality Research: A Tutorial on Network Analysis of Personality Data in R. J. Res. Personal. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Epskamp, S.; Maris, G.; Waldorp, L.J.; Borsboom, D. Network Psychometrics. In The Wiley Handbook of Psychometric Testing: A Multidisciplinary Reference on Survey, Scale and Test Development; University of Amsterdam: Amsterdam, The Netherlands, 2017; Volume 2, pp. 953–986. ISBN 978-1-118-48977-2. [Google Scholar]
- Lauritzen, S.L. Graphical Models; Oxford Statistical Science Series; Oxford University Press: Oxford, UK; New York, NY, USA,, 1996; ISBN 978-0-19-852219-5. [Google Scholar]
- Murphy, K.P. Machine Learning; MIT Press: Cambridge, MA, USA, 2012. [Google Scholar]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse Inverse Covariance Estimation with the Graphical Lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef]
- Golino, H.F.; Epskamp, S. Exploratory Graph Analysis: A New Approach for Estimating the Number of Dimensions in Psychological Research. PLoS ONE 2017, 12, e0174035. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, Z. Extended Bayesian Information Criteria for Model Selection with Large Model Spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef]
- Barber, R.F.; Drton, M. High-Dimensional Ising Model Selection with Bayesian Information Criteria. Electron. J. Stat. 2015, 9, 567–607. [Google Scholar] [CrossRef]
- Van Borkulo, C.D.; Borsboom, D.; Epskamp, S.; Blanken, T.F.; Boschloo, L.; Schoevers, R.A.; Waldorp, L.J. A New Method for Constructing Networks from Binary Data. Sci. Rep. 2014, 4, 5918. [Google Scholar] [CrossRef]
- Fried, E.I.; Eidhof, M.B.; Palic, S.; Costantini, G.; Huisman-van Dijk, H.M.; Bockting, C.L.H.; Engelhard, I.; Armour, C.; Nielsen, A.B.S.; Karstoft, K.-I. Replicability and Generalizability of Posttraumatic Stress Disorder (PTSD) Networks: A Cross-Cultural Multisite Study of PTSD Symptoms in Four Trauma Patient Samples. Clin. Psychol. Sci. 2018, 6, 335–351. [Google Scholar] [CrossRef]
- Dalege, J.; Borsboom, D.; Van Harreveld, F.; Van Der Maas, H.L.J. Network Analysis on Attitudes: A Brief Tutorial. Soc. Psychol. Personal. Sci. 2017, 8, 528–537. [Google Scholar] [CrossRef]
- Haslbeck, J.M.B.; Waldorp, L.J. How Well Do Network Models Predict Observations? On the Importance of Predictability in Network Models. Behav. Res. Methods 2018, 50, 853–861. [Google Scholar] [CrossRef]
- McNally, R.J.; Heeren, A.; Robinaugh, D.J. A Bayesian Network Analysis of Posttraumatic Stress Disorder Symptoms in Adults Reporting Childhood Sexual Abuse. Eur. J. Psychotraumatol. 2017, 8, 1341276. [Google Scholar] [CrossRef]
- Gardner, P.J.; Moallef, P. Psychological Impact on SARS Survivors: Critical Review of the English Language Literature. Can. Psychol. 2015, 56, 123–135. [Google Scholar] [CrossRef]
- Garrido-Hernansaiz, H.; Rodríguez-Rey, R.; Alonso-Tapia, J. Coping and Resilience Are Differently Related Depending on the Population: A Comparison between Three Clinical Samples and the General Population. Int. J. Stress Manag. 2020, 27, 304–309. [Google Scholar] [CrossRef]
- McEvoy, P.M.; Mahoney, A.E.J.; Moulds, M.L. Are Worry, Rumination, and Post-Event Processing One and the Same?: Development of the Repetitive Thinking Questionnaire. J. Anxiety Disord. 2010, 24, 509–519. [Google Scholar] [CrossRef]
- Beck, A.T. Cognitive Therapy of Depression; Guilford Press: New York, NY, USA, 1979. [Google Scholar]
- Morris, D.W. Adaptive Affect: The Nature of Anxiety and Depression. Neuropsychiatr. Dis. Treat. 2019, 15, 3323–3326. [Google Scholar] [CrossRef]
- Pauw, L.S.; Medland, H.; Paling, S.J.; Moeck, E.K.; Greenaway, K.H.; Kalokerinos, E.K.; Hinton, J.D.X.; Hollenstein, T.; Koval, P. Social Support Predicts Differential Use, but Not Differential Effectiveness, of Expressive Suppression and Social Sharing in Daily Life. Affect. Sci. 2022, 3, 641–652. [Google Scholar] [CrossRef]
- Srivastava, S.; Tamir, M.; McGonigal, K.M.; John, O.P.; Gross, J.J. The Social Costs of Emotional Suppression: A Prospective Study of the Transition to College. J. Pers. Soc. Psychol. 2009, 96, 883–897. [Google Scholar] [CrossRef]
- Finch, B.; Ong, E. Exploring Coping Resiliency and Depression among University Students in a Post-Pandemic Context. Adv. Ment. Health 2024, 1–17. [Google Scholar] [CrossRef]
- Panzeri, A.; Rossi Ferrario, S.; Cerutti, P. Psychological Differences Among Healthcare Workers of a Rehabilitation Institute During the COVID-19 Pandemic: A Two-Step Study. Front. Psychol. 2021, 12, 636129. [Google Scholar] [CrossRef]
- Munroe, M.; Al-Refae, M.; Chan, H.W.; Ferrari, M. Using Self-Compassion to Grow in the Face of Trauma: The Role of Positive Reframing and Problem-Focused Coping Strategies. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, S157–S164. [Google Scholar] [CrossRef]
- Training for Resilience. In Resilience and Mental Health: Challenges across the Lifespan; Litz, B.T., Charney, D., Friedman, M.J., Southwick, S.M., Eds.; Cambridge University Press: Cambridge, UK, 2011; ISBN 978-0-521-89839-3. [Google Scholar]
- Mayordomo, T.; Viguer, P.; Sales, A.; Satorres, E.; Meléndez, J.C. Resilience and Coping as Predictors of Well-Being in Adults. In Mental Health and Psychopathology; Routledge: Abingdon, UK, 2021; ISBN 978-1-00-324360-1. [Google Scholar]
- Windle, G.; Bennett, K.M. The Social Ecology of Resilience. In The Social Ecology of Resilience; Springer: New York, NY, USA, 2012; pp. 219–231. [Google Scholar]
- Bennett, K.M.; Panzeri, A.; Derrer-Merk, E.; Butter, S.; Hartman, T.K.; Mason, L.; McBride, O.; Murphy, J.; Shevlin, M.; Gibson-Miller, J.; et al. Predicting Resilience during the COVID-19 Pandemic in the United Kingdom: Cross-Sectional and Longitudinal Results. PLoS ONE 2023, 18, e0283254. [Google Scholar] [CrossRef]
- McKenna, O.; Fakolade, A.; Cardwell, K.; Langlois, N.; Jiang, K.; Pilutti, L.A. Towards Conceptual Convergence: A Systematic Review of Psychological Resilience in Family Caregivers of Persons Living with Chronic Neurological Conditions. Health Expect. 2022, 25, 4–37. [Google Scholar] [CrossRef]
- Palacio, G.C.; Krikorian, A.; Gómez-Romero, M.J.; Limonero, J.T. Resilience in Caregivers: A Systematic Review. Am. J. Hosp. Palliat. Med. 2020, 37, 648–658. [Google Scholar] [CrossRef]
- Contreras, A.; Butter, S.; Granziol, U.; Panzeri, A.; Peinado, V.; Trucharte, A.; Zavlis, O.; Valiente, C.; Vázquez, C.; Murphy, J.; et al. The Network Structure of Psychopathological and Resilient Responses to the Pandemic: A Multicountry General Population Study of Depression and Anxiety. J. Trauma. Stress 2024, 37, 126–140. [Google Scholar] [CrossRef]
- Panzeri, A.; DeVita, M.; Di Rosa, E.; Bottesi, G.; Brundisini, V.; Guarrera, C.; Ravelli, A.; Ponza, I.; Cattelan, A.; Volpe, B.; et al. Trauma Shaping the Psychopathological Correlates of Patients with Long-COVID: A 6-Months Longitudinal Study with Repeated Measures Mixed Models. Psychiatry Res. 2023, 330, 115609. [Google Scholar] [CrossRef]
- Epskamp, S.; Waldorp, L.J.; Mõttus, R.; Borsboom, D. The Gaussian Graphical Model in Cross-Sectional and Time-Series Data. Multivar. Behav. Res. 2018, 53, 453–480. [Google Scholar] [CrossRef]
- Rossi Ferrario, S.; Panzeri, A.; Pistono, M. Psychological Difficulties of LVAD Patients and Caregivers: A Follow up over 1 Year from Discharge. Artif. Organs 2021, 46, 479–490. [Google Scholar] [CrossRef]
- Tamres, L.K.; Janicki, D.; Helgeson, V.S. Sex Differences in Coping Behavior: A Meta-Analytic Review and an Examination of Relative Coping. Personal. Soc. Psychol. Rev. 2002, 6, 2–30. [Google Scholar] [CrossRef]
- O’Rourke, T.; Vogel, C.; John, D.; Pryss, R.; Schobel, J.; Haug, F.; Haug, J.; Pieh, C.; Nater, U.M.; Feneberg, A.C.; et al. The Impact of Coping Styles and Gender on Situational Coping: An Ecological Momentary Assessment Study With the mHealth Application TrackYourStress. Front. Psychol. 2022, 13, 913125. [Google Scholar] [CrossRef] [PubMed]
- Flake, J.K.; Fried, E.I. Measurement Schmeasurement: Questionable Measurement Practices and How to Avoid Them. Adv. Methods Pract. Psychol. Sci. 2020, 3, 456–465. [Google Scholar] [CrossRef]
- Freeston, M.; Tiplady, A.; Mawn, L.; Bottesi, G.; Thwaites, S. Towards a Model of Uncertainty Distress in the Context of Coronavirus (COVID-19). Cogn. Behav. Ther. 2020, 13, e31. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, T.; Cheung, D.S.T.; Chau, P.H.; Ho, M.-H.; Han, Y.; Lin, C.C. Dyadic Advance Care Planning: Systematic Review of Patient–Caregiver Interventions and Effects. BMJ Support. Palliat. Care 2023. advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Marconi, M.; Taccini, F.; Verusio, C.; Mannarini, S. Screening for Distress in Oncological Patients: The Revised Version of the Psychological Distress Inventory (PDI-R). Front. Psychol. 2022, 13, 859478. [Google Scholar] [CrossRef] [PubMed]
- Talley, R.C.; Crews, J.E. Framing the Public Health of Caregiving. Am. J. Public Health 2007, 97, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Zhai, S.; Chu, F.; Tan, M.; Chi, N.-C.; Ward, T.; Yuwen, W. Digital Health Interventions to Support Family Caregivers: An Updated Systematic Review. Digit. Health 2023, 9, 205520762311719. [Google Scholar] [CrossRef]
- Malhotra, C.; Huynh, V.A.; Shafiq, M.; Batcagan-Abueg, A.P.M. Advance Care Planning and Caregiver Outcomes: Intervention Efficacy—Systematic Review. BMJ Support. Palliat. Care 2023, 13, e537–e546. [Google Scholar] [CrossRef]
| Females (N = 330) | Males (N = 21) | Total (N = 351) | |
|---|---|---|---|
| Age, mean (SD) | 49.221 (11.182) | 50.952 (9.882) | 49.325 (11.104) |
| Range | 18–85 | 38–68 | 18–85 |
| Relationship status | |||
| Single | 44 (13.3%) | 4 (19.0%) | 48 (13.7%) |
| Engaged | 28 (8.5%) | 1 (4.8%) | 29 (8.3%) |
| Cohabiting | 36 (10.9%) | 3 (14.3%) | 39 (11.1%) |
| Married | 197 (59.7%) | 13 (61.9%) | 210 (59.8%) |
| Separated | 10 (3.0%) | 0 (0.0%) | 10 (2.8%) |
| Divorced | 9 (2.7%) | 0 (0.0%) | 9 (2.6%) |
| Widow | 6 (1.8%) | 0 (0.0%) | 6 (1.7%) |
| Education | |||
| Primary school | 4 (1.2%) | 0 (0.0%) | 4 (1.1%) |
| Middle school | 42 (12.7%) | 4 (19.0%) | 46 (13.1%) |
| High school | 175 (53.0%) | 11 (52.4%) | 186 (53.0%) |
| Bachelor’s degree | 31 (9.4%) | 1 (4.8%) | 32 (9.1%) |
| Master’s degree | 48 (14.5%) | 4 (19.0%) | 52 (14.8%) |
| Post-graduate | 29 (8.8%) | 1 (4.8%) | 30 (8.5%) |
| None | 1 (0.3%) | 0 (0.0%) | 1 (0.3%) |
| Occupational status | |||
| Student | 7 (2.1%) | 0 (0.0%) | 7 (2.0%) |
| Working student | 8 (2.4%) | 0 (0.0%) | 8 (2.3%) |
| Employed | 183 (55.5%) | 14 (66.7%) | 197 (56.1%) |
| Unemployed | 64 (19.4%) | 3 (14.3%) | 67 (19.1%) |
| Retired | 43 (13.0%) | 1 (4.8%) | 44 (12.5%) |
| Other | 25 (7.6%) | 3 (14.3%) | 28 (8.0%) |
| Mean | Sd | Median | Min | Max | Skewness | Kurtosis | Se | ω | |
|---|---|---|---|---|---|---|---|---|---|
| PHQ-9 | 13.031 | 6.012 | 12 | 0 | 27 | 0.401 | −0.484 | 0.321 | 0.89 |
| GAD-7 | 12.422 | 4.924 | 12 | 0 | 21 | 0.109 | −0.941 | 0.263 | 0.92 |
| ERQ Reappraisal | 26.04 | 8.101 | 26 | 6 | 42 | −0.2 | −0.285 | 0.432 | 0.93 |
| ERQ Suppression | 15.148 | 5.709 | 15 | 4 | 28 | −0.082 | −0.676 | 0.305 | 0.77 |
| COPE Avoidance | 9.513 | 3.653 | 9 | 5 | 29 | 1.282 | 2.133 | 0.195 | 0.72 |
| COPE Transcendental | 9.538 | 6.483 | 8 | 4 | 24 | 1.089 | −0.181 | 0.346 | 0.98 |
| COPE Positive Attitude | 21.897 | 7.65 | 21 | 6 | 36 | 0.142 | −0.723 | 0.408 | 0.92 |
| COPE Social Support | 14.513 | 6.423 | 13 | 5 | 30 | 0.67 | −0.309 | 0.343 | 0.90 |
| COPE Problem orientation | 19.402 | 5.729 | 19 | 5 | 30 | 0.144 | −0.799 | 0.306 | 0.86 |
| Resilience | 60.943 | 16.02 | 62 | 20 | 98 | −0.029 | −0.645 | 0.855 | 0.93 |
| Depression Symptoms | Anxiety Symptoms | ERQ Reappraisal | ERQ Suppression | COPE Avoidant | COPE Transcendental | COPE Positive Attitude | COPE Social Support | COPE Problem Orientation | Resilience | Predictability | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression symptoms | - | 0.647 | 0 | 0 | 0.135 | 0 | 0 | 0 | 0 | −0.146 | 0.538 | |
| Anxiety symptoms | 0.647 | - | 0 | 0 | 0 | 0 | 0 | 0 | 0.138 | 0 | 0.532 | |
| ERQ Reappraisal | 0 | 0 | - | 0.211 | 0 | 0 | 0.244 | 0 | 0 | 0.34 | 0.344 | |
| ERQ Suppression | 0 | 0 | 0.211 | - | 0 | 0 | 0 | −0.204 | 0 | 0 | 0.123 | |
| COPE Avoidant | 0.135 | 0 | 0 | 0 | - | 0 | 0 | 0 | 0 | 0 | 0.114 | |
| COPE Transcendental | 0 | 0 | 0 | 0 | 0 | - | 0 | 0 | 0 | 0 | 0.029 | |
| COPE Positive Attitude | 0 | 0 | 0.244 | 0 | 0 | 0 | - | 0 | 0.421 | 0.265 | 0.476 | |
| COPE Social Support | 0 | 0 | 0 | −0.204 | 0 | 0 | 0 | - | 0.167 | 0 | 0.184 | |
| COPE Problem Orientation | 0 | 0.138 | 0 | 0 | 0 | 0 | 0.421 | 0.167 | - | 0 | 0.352 | |
| Resilience | −0.146 | 0 | 0.34 | 0 | 0 | 0 | 0.265 | 0 | 0 | - | 0.456 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panzeri, A.; Bottesi, G.; Ghisi, M.; Scalavicci, C.; Spoto, A.; Vidotto, G. Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach. Behav. Sci. 2024, 14, 709. https://doi.org/10.3390/bs14080709
Panzeri A, Bottesi G, Ghisi M, Scalavicci C, Spoto A, Vidotto G. Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach. Behavioral Sciences. 2024; 14(8):709. https://doi.org/10.3390/bs14080709
Chicago/Turabian StylePanzeri, Anna, Gioia Bottesi, Marta Ghisi, Cecilia Scalavicci, Andrea Spoto, and Giulio Vidotto. 2024. "Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach" Behavioral Sciences 14, no. 8: 709. https://doi.org/10.3390/bs14080709
APA StylePanzeri, A., Bottesi, G., Ghisi, M., Scalavicci, C., Spoto, A., & Vidotto, G. (2024). Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach. Behavioral Sciences, 14(8), 709. https://doi.org/10.3390/bs14080709







