Leveraging Artificial Intelligence to Predict Health Belief Model and COVID-19 Vaccine Uptake Using Survey Text from US Nurses
Abstract
1. Introduction
1.1. Gaining Insight from Open-Field Comments
1.2. Health Belief Model Constructs
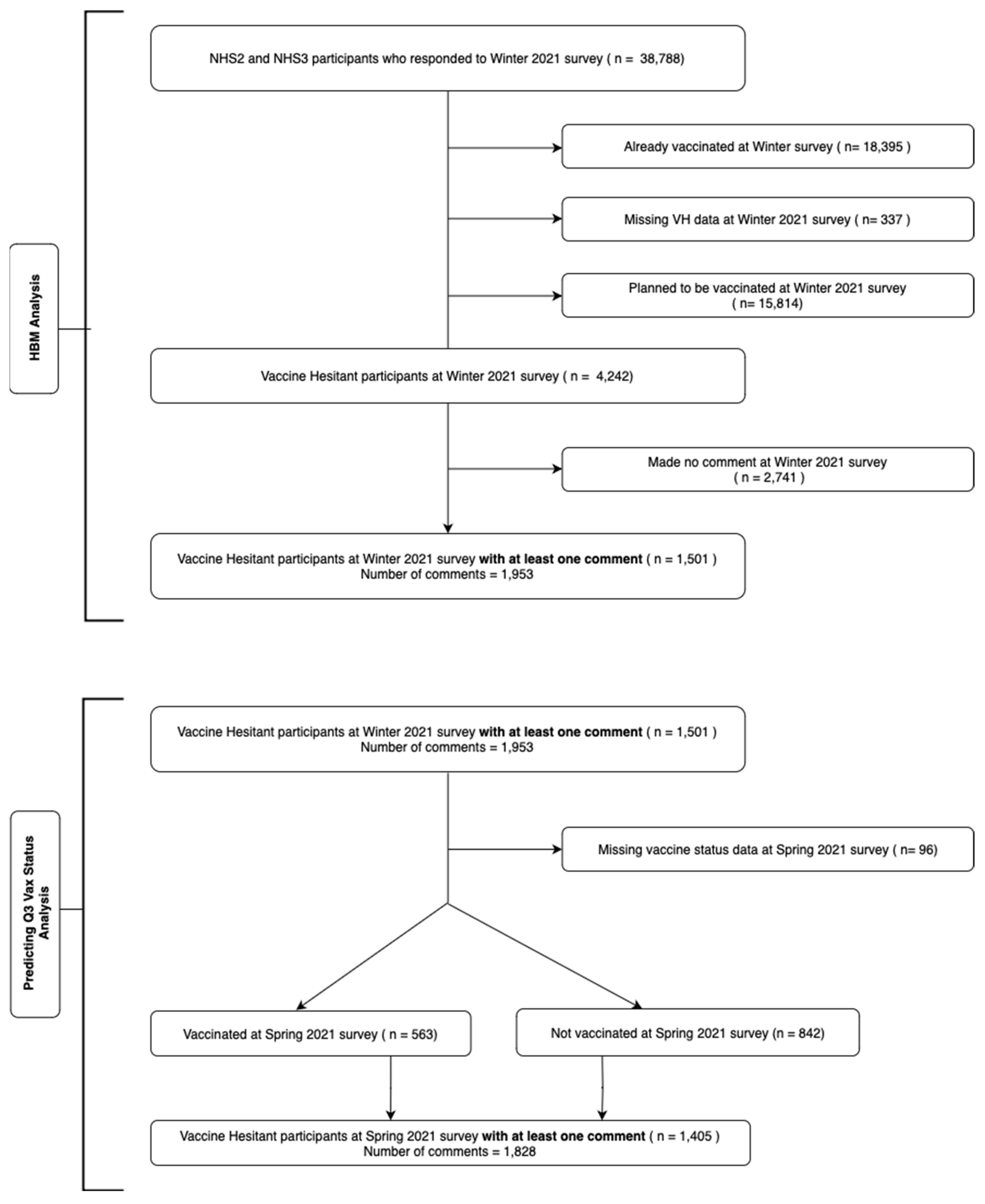
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Machine Learning Models
3. Results
3.1. HBM Prediction
3.2. Results for Vaccine Status Prediction
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
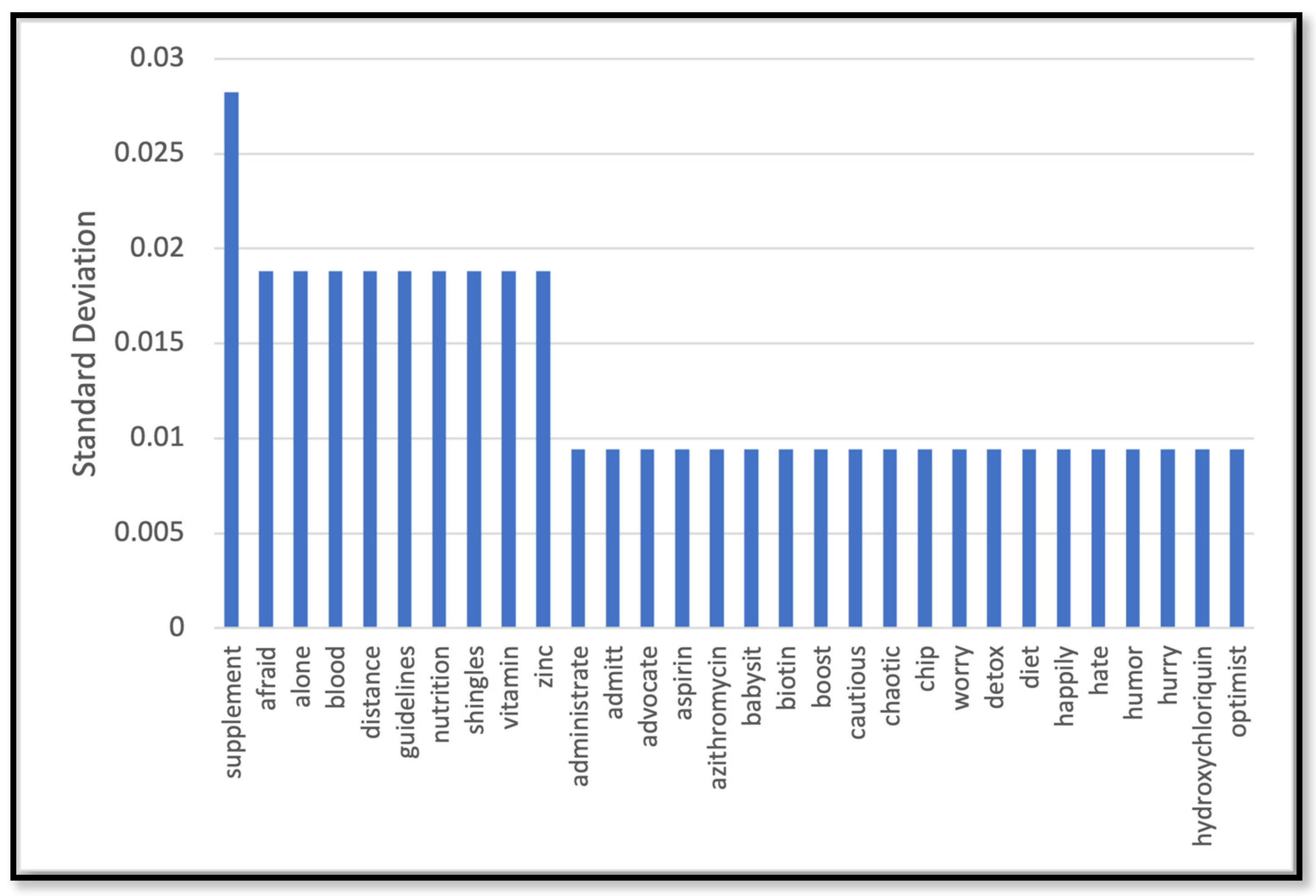
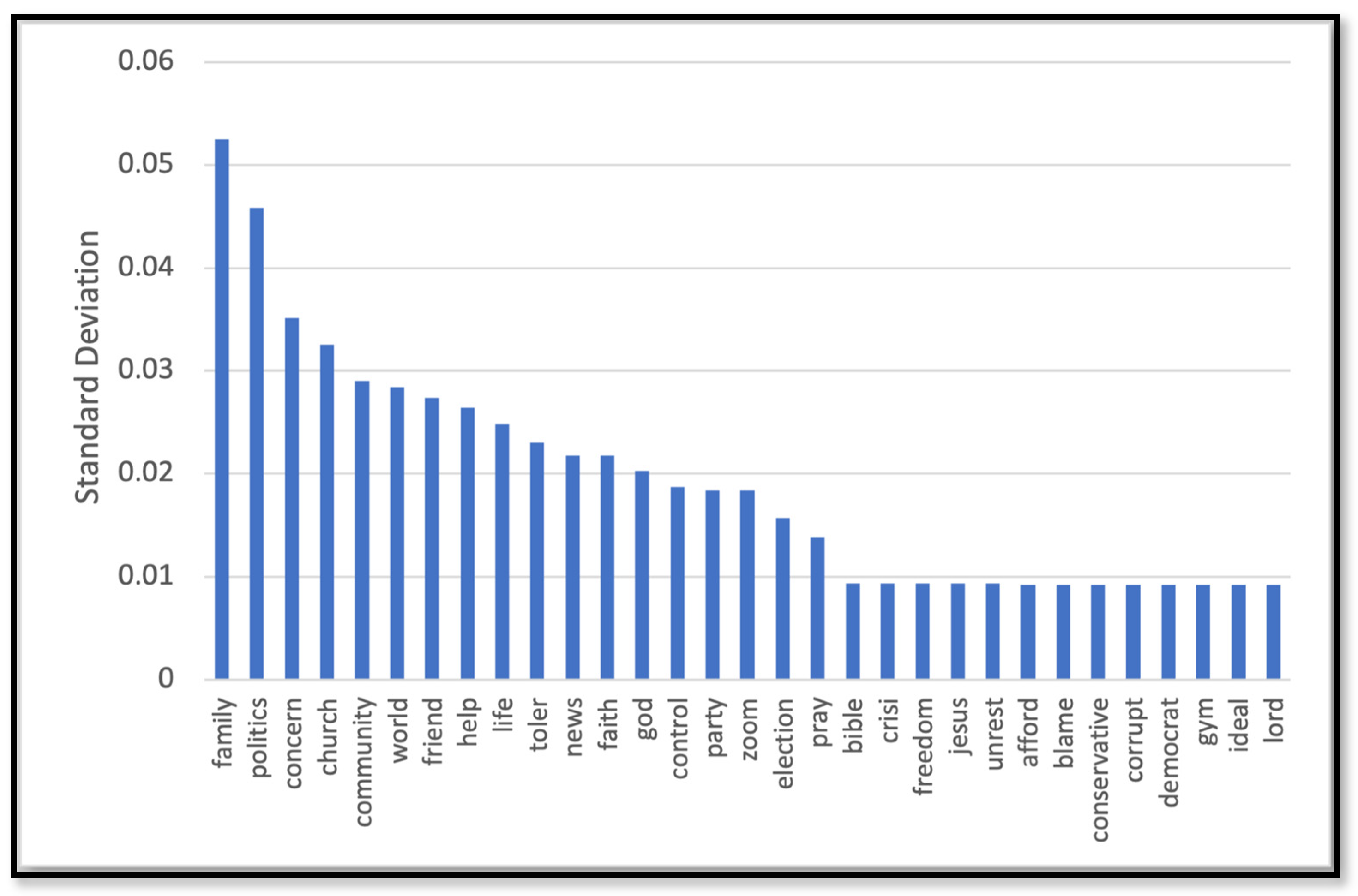
Appendix A. Data Preprocessing and Feature Selection
References
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef] [PubMed]
- Rich-Edwards, J.W.; Ding, M.; Rocheleau, C.M.; Boiano, J.M.; Kang, J.H.; Becene, I.; Nguyen, L.H.; Chan, A.T.; Hart, J.E.; Chavarro, J.E.; et al. American Frontline Healthcare Personnel’s Access to and Use of Personal Protective Equipment Early in the COVID-19 Pandemic. J. Occup. Environ. Med. 2021, 63, 913–920. [Google Scholar] [CrossRef] [PubMed]
- US Food and Drug Administration. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines (accessed on 29 April 2023).
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Toth-Manikowski, S.M.; Swirsky, E.S.; Gandhi, R.; Piscitello, G. COVID-19 Vaccination Hesitancy among Health Care Workers, Communication, and Policy-Making. Am. J. Infect. Control 2022, 50, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Billings, J.; Ching, B.C.F.; Gkofa, V.; Greene, T.; Bloomfield, M. Experiences of Frontline Healthcare Workers and Their Views about Support during COVID-19 and Previous Pandemics: A Systematic Review and Qualitative Meta-Synthesis. BMC Health Serv. Res. 2021, 21, 923. [Google Scholar] [CrossRef] [PubMed]
- Gharpure, R.; Guo, A.; Bishnoi, C.K.; Patel, U.; Gifford, D.; Tippins, A.; Jaffe, A.; Shulman, E.; Stone, N.; Mungai, E.; et al. Early COVID-19 First-Dose Vaccination Coverage Among Residents and Staff Members of Skilled Nursing Facilities Participating in the Pharmacy Partnership for Long-Term Care Program—United States, December 2020–January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Heyerdahl, L.W.; Dielen, S.; Nguyen, T.; Van Riet, C.; Kattumana, T.; Simas, C.; Vandaele, N.; Vandamme, A.-M.; Vandermeulen, C.; Giles-Vernick, T.; et al. Doubt at the Core: Unspoken Vaccine Hesitancy among Healthcare Workers. Lancet Reg. Health Eur. 2022, 12, 100289. [Google Scholar] [CrossRef] [PubMed]
- The Nurses’ Health Study and Nurses’ Health Study II Are among the Largest Investigations into the Risk Factors for Major Chronic Diseases in Women. Available online: https://nurseshealthstudy.org (accessed on 8 April 2023).
- Riiskjaer, E.; Ammentorp, J.; Kofoed, P.-E. The Value of Open-Ended Questions in Surveys on Patient Experience: Number of Comments and Perceived Usefulness from a Hospital Perspective. Int. J. Qual. Health Care 2012, 24, 509–516. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Pathak, V.; Jena, B.; Kalra, S. Qualitative Research. Perspect Clin. Res. 2013, 4, 192. [Google Scholar] [CrossRef]
- Charmaz, K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2006. [Google Scholar]
- Nguyen, K.T.N.H.; Stuart, J.J.; Shah, A.H.; Becene, I.A.; West, M.G.; Berrill, J.; Gelaye, B.; Borba, C.P.C.; Rich-Edwards, J.W. Novel Methods for Leveraging Large Cohort Studies for Qualitative and Mixed-Methods Research. Am. J. Epidemiol. 2023, 192, 821–829. [Google Scholar] [CrossRef]
- Marsland, S. Machine Learning: An Algorithmic Perspective, 2nd ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2014. [Google Scholar] [CrossRef]
- Muhammad, I.; Yan, Z. Supervised machine learning approaches: A survey. IJSC 2015, 5, 946–952. [Google Scholar] [CrossRef]
- Lu, J.; Luo, M.; Yee, A.Z.H.; Sheldenkar, A.; Lau, J.; Lwin, M.O. Do Superstitious Beliefs Affect Influenza Vaccine Uptake through Shaping Health Beliefs? Vaccine 2019, 37, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Walkowiak, M.P.; Domaradzki, J.; Walkowiak, D. Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines 2022, 10, 528. [Google Scholar] [CrossRef] [PubMed]
- Walkowiak, M.P.; Walkowiak, J.B.; Walkowiak, D. More Time, Carrot-and-Stick, or Piling Coffins? Estimating the Role of Factors Overcoming COVID-19 Vaccine Hesitancy in Poland and Lithuania in the Years 2021–2022. Vaccines 2022, 10, 1523. [Google Scholar] [CrossRef] [PubMed]
- Consoli, D.; Mina, A. An evolutionary perspective on health innovation systems. J. Evol. Econ. 2009, 19, 297–319. [Google Scholar] [CrossRef]
- Goldberg, Y.; Mandel, M.; Woodbridge, Y.; Fluss, R.; Novikov, I.; Yaari, R.; Ziv, A.; Freedman, L.; Huppert, A. Protection of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: A three-month nationwide experience from Israel. Am. J. Epidemiol. 2021. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Ruder, S. An overview of gradient descent optimization algorithms. arXiv 2016, arXiv:1609.04747. [Google Scholar]
- Neural Network Models. Available online: https://scikit-learn.org/stable/modules/neural_networks_supervised.html (accessed on 8 April 2023).
- Goldstein, S.; MacDonald, N.; Guirguis, S. Health communication and vaccine hesitancy. Vaccine 2015, 33, 4212–4214. [Google Scholar] [CrossRef]
- Shmueli, L. Predicting Intention to Receive COVID-19 Vaccine among the General Population Using the Health Belief Model and the Theory of Planned Behavior Model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 Vaccine Demand and Hesitancy: A Nationwide Online Survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Mercadante, A.R.; Law, A.V. Will They, or Won’t They? Examining Patients’ Vaccine Intention for Flu and COVID-19 Using the Health Belief Model. Res. Soc. Adm. Pharm. 2021, 17, 1596–1605. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, S.A.; Kelley, C.F.; Horton, J.P.; Jamieson, D.J. Coronavirus Disease 2019 (COVID-19) Vaccines and Pregnancy: What Obstetricians Need to Know. Obs. Gynecol. 2021, 137, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R. Measuring trust in vaccination: A systematic review. Lancet 2018, 392, 1783–1794. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Bergen, I.; Böger, S.; Beaudart, C.; Hiligsmann, M.; Cheung, K. Beliefs regarding COVID-19 vaccinations of young adults in the United Kingdom: An interview study applying the Integrated Change Model. PLoS ONE 2022, 17, e0277109. [Google Scholar] [CrossRef]
- Limbu, Y.B.; Gautam, R.K.; Pham, L. The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 973. [Google Scholar] [CrossRef]
- Xiao, X.; Wong, R. Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine 2020, 38, 5131–5138. [Google Scholar] [CrossRef]
- Yan, J.; Zhang, B.; Liu, N.; Yan, S.; Cheng, Q.; Fan, W.; Yang, Q.; Xi, W.; Chen, Z. Effective and Efficient Dimensionality Reduction for Large-Scale and Streaming Data Preprocessing. IEEE Trans. Knowl. Data Eng. 2006, 18, 320–333. [Google Scholar] [CrossRef]
- Xu, X.; Liang, T.; Zhu, J.; Zheng, D.; Sun, T. Review of Classical Dimensionality Reduction and Sample Selection Methods for Large-Scale Data Processing. Neurocomputing 2019, 328, 5–15. [Google Scholar] [CrossRef]




| HBM Construct | Definition | Example Comment |
|---|---|---|
| Perceived Barriers | Belief about the tangible and psychological costs of the advised action. | “Not fully tested or approved and is unnecessary for someone low risk like me. Also has not been studied for its effects on fertility and future pregnancies. I also know someone person that died 2 days after receiving the vaccine who had no medical conditions other than being overweight”. |
| Perceived Severity | Feelings about the seriousness of contracting an illness or of leaving it untreated include evaluations of both medical and clinical consequences (for example, death, disability, and pain) and possible social consequences (such as the effects of the conditions on work, family life, and social relations). | “There is a 99.7% survival rate for someone my age anyway”. |
| Perceived Susceptibility | Belief about the chances of getting a condition or disease. | “I honestly don’t know what to believe anymore. I consider myself healthy for my age; no co-morbidities; and it take vitamins and supplements that have been proven to boost the immune system. So I see no reason to take a rushed vaccine. I have never gotten a flu shot and have never gotten the flu either” |
| Non-HBM | Comments that do not fall into any of the above categories. | “I needed to travel in mid January as my dad had major surgery and needed someone to be with him”. |
| Machine Learning Algorithm | Recall (Sensitivity) | Precision | F1-Score | Accuracy | AUC-ROC |
|---|---|---|---|---|---|
| Random Forest | 0.60 | 0.61 | 0.59 | 0.60 | 0.84 |
| Multinomial NB | 0.60 | 0.57 | 0.56 | 0.72 | 0.86 |
| Logistic Regression | 0.58 | 0.54 | 0.55 | 0.68 | 0.86 |
| SGD | 0.61 | 0.63 | 0.61 | 0.67 | 0.87 |
| Neural network | 0.82 | 0.85 | 0.79 | 0.82 | 0.91 |
| Machine Learning Algorithm | Recall (Sensitivity) | Precision | F1-Score | Accuracy | AUC-ROC |
|---|---|---|---|---|---|
| Random Forest | 0.71 | 0.76 | 0.72 | 0.78 | 0.83 |
| Multinomial NB | 0.84 | 0.89 | 0.86 | 0.88 | 0.86 |
| Logistic Regression | 0.69 | 0.86 | 0.71 | 0.79 | 0.85 |
| SGD | 0.78 | 0.81 | 0.79 | 0.82 | 0.83 |
| Neural network | 0.89 | 0.90 | 0.89 | 0.89 | 0.88 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omranian, S.; Khoddam, A.; Campos-Castillo, C.; Fouladvand, S.; McRoy, S.; Rich-Edwards, J. Leveraging Artificial Intelligence to Predict Health Belief Model and COVID-19 Vaccine Uptake Using Survey Text from US Nurses. Behav. Sci. 2024, 14, 217. https://doi.org/10.3390/bs14030217
Omranian S, Khoddam A, Campos-Castillo C, Fouladvand S, McRoy S, Rich-Edwards J. Leveraging Artificial Intelligence to Predict Health Belief Model and COVID-19 Vaccine Uptake Using Survey Text from US Nurses. Behavioral Sciences. 2024; 14(3):217. https://doi.org/10.3390/bs14030217
Chicago/Turabian StyleOmranian, Samaneh, Alireza Khoddam, Celeste Campos-Castillo, Sajjad Fouladvand, Susan McRoy, and Janet Rich-Edwards. 2024. "Leveraging Artificial Intelligence to Predict Health Belief Model and COVID-19 Vaccine Uptake Using Survey Text from US Nurses" Behavioral Sciences 14, no. 3: 217. https://doi.org/10.3390/bs14030217
APA StyleOmranian, S., Khoddam, A., Campos-Castillo, C., Fouladvand, S., McRoy, S., & Rich-Edwards, J. (2024). Leveraging Artificial Intelligence to Predict Health Belief Model and COVID-19 Vaccine Uptake Using Survey Text from US Nurses. Behavioral Sciences, 14(3), 217. https://doi.org/10.3390/bs14030217







