Effectiveness of Cognitive Behavioral Therapy (CBT) on Psychological Distress among Mothers of Children with Autism Spectrum Disorder: The Role of Problem-Solving Appraisal
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Question
2.2. Research Hypothesis
2.3. Design
2.4. Settings
2.5. Eligibility Criteria
2.5.1. Inclusion Criteria
- Mothers aged 20–50 years.
- Mothers must be the primary caregiver and resident of a child diagnosed with autism spectrum disorder (ASD) for 2 years.
- The child’s diagnosis of ASD must be made by a psychiatrist.
- Mothers can have only one child diagnosed with ASD.
- No prior participation of mother or child in rehabilitation or intervention programs.
2.5.2. Exclusion Criteria for Mothers
- Current or past psychiatric diagnosis.
- Attendance of <5 CBT sessions.
- Severe levels of psychological distress (scores in severe ranges on DASS-21 subscales).
2.5.3. Exclusion Criteria for Children
- Estimated intellectual disability (IQ < 70).
- Severe symptom deterioration or regression.
- Ongoing treatment with psychiatric medications.
- Comorbid diagnoses of multiple developmental disorders.
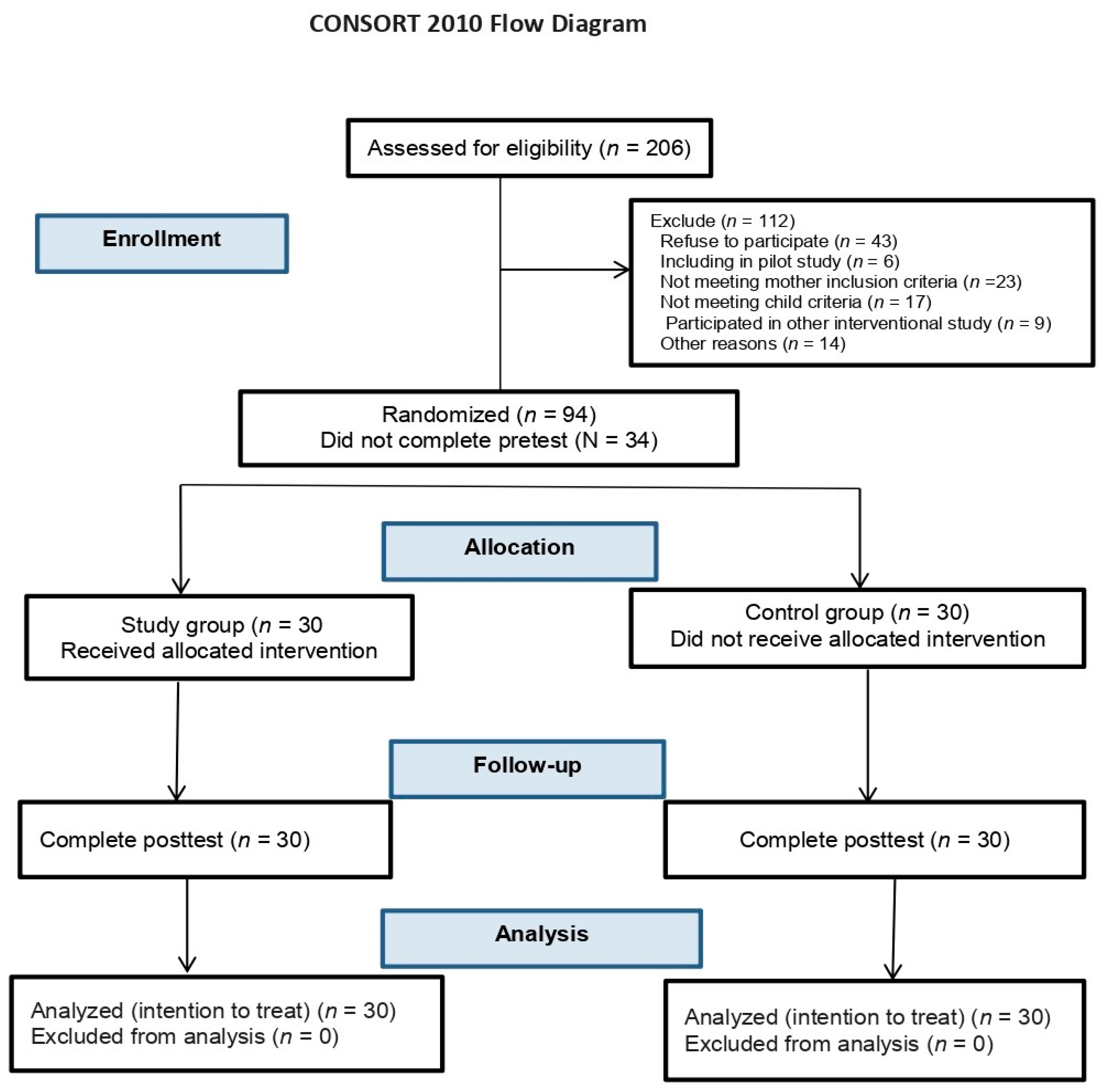
2.6. Participants and Sample Size Determination
2.7. Data Collection Tools
- Sociodemographic Questionnaire: Collected information on the age of mothers; level of education; marital status; occupation; the adequacy of family income; and the age, sex, and severity of autism of the child.
- Depression anxiety stress scale (DASS-21): A 21-item scale assessing symptoms of depression, anxiety, and stress over the past week [57]. The Arabic DASS-21 translated by [58] was used. It has robust reliability and validity in Arab populations [58]. In this study, internal consistency was high (Cronbach’s alpha = 0.903).
- Problem-Solving Inventory (PSI): A 32-item scale measuring perceived problem-solving abilities across three subscales: problem-solving confidence, approach-avoidance style, and personal control [59]. The PSI has strong psychometric properties and utilizes a 6-point Likert scale [60]. Lower scores indicate better perceived problem-solving [61]. In this study, PSI had high internal consistency (Cronbach’s alpha = 0.938).
2.8. Ethical Approval
2.9. Procedure
2.9.1. Study Randomization
2.9.2. Cognitive Behavioral Therapy Intervention
2.9.3. Objectives and Teaching Methods
2.9.4. Phases of the CBT Program
- -
- Assessment Phase (two sessions): Initiated with pre-testing procedures (T1), participants received comprehensive information about the study’s objectives and implementation strategies, both verbally and in writing. The study group received the program sessions across three hospitals simultaneously, always convening in the same room in outpatient clinics.
- -
- Implementation Phase (Eight Sessions): Each session combined theoretical and practical elements of CBT. The final segment of each session allowed for open discussion and inquiries. Session themes ranged from educating about ASD and its impact on family dynamics to teaching cognitive restructuring techniques and problem-solving skills.
- -
- Sessions of the CBT program
- -
- Session (1): During this session, participants received education about their child’s disease, including information about signs and symptoms, specific needs, principles of behavioral management skills, and the impact on their family. As part of their homework for this session, participants were instructed to document any symptoms exhibited by their child that contribute to challenges or difficulties.
- -
- Session (2): During this session, the researchers aimed to elucidate the connection between thoughts, emotions, and behaviors. They specifically addressed how biased thoughts can influence one’s emotions and actions. Participants engaged in discussions regarding the awareness of negative automatic thoughts (ATs) and the accompanying feelings that arise in stressful life situations. As part of their homework for this session, participants were assigned the task of reflecting on their understanding of emotions and examining their own emotional experiences.
- -
- Session (3): participants were encouraged by the researchers to take note of negative irrational thoughts, and discussions were held on how to effectively recognize these thoughts. Subsequently, participants were taught methods to transform and substitute negative thoughts with positive and logical ones, and they were also guided on how to reframe negative thinking patterns. Moreover, the session involved a detailed exploration of techniques such as guided imagery, meditation, and visualization.
- -
- Session (4): The researchers discussed the principles and techniques of cognitive restructuring, which involve replacing negative automatic thoughts (ATs) with more positive ones. In addition, the session addressed problem-based coping skills, the importance of developing positive friendships for effective problem-solving, and the use of modeling to manage stress. The researchers also assisted participants in practicing progressive relaxation techniques, including both active and passive approaches.
- -
- Session (5): During this session, participants were introduced to problem-solving appraisal techniques, which aimed to assist them in effectively dealing with various stressful situations. Additionally, the researchers highlighted the importance of self-instruction and self-talk as strategies to control negative thoughts. Participants were encouraged to explore and apply these techniques to manage their own cognitive processes and enhance their ability to cope with stress.
- -
- Session (6): In this session, participants were instructed in the step-by-step process of problem-solving using the solved technique. They were encouraged to visually illustrate their problems and select potential solutions. Through group discussions, participants had the opportunity to share their experiences and engage in open dialogue. Moreover, participants were prompted to express their inner feelings towards their problems, focusing on both positive and negative aspects.
- -
- Session (7): Participants were actively encouraged to follow the steps of problem-solving. The researchers emphasized the importance of systematically approaching problem-solving tasks and provided guidance to participants on each step of the process. By following these steps, participants were equipped with a structured approach to effectively tackle their problems.
- -
- Session (8): The researchers consolidated the key learnings from the previous sessions. Participants were given opportunities to practice the skills they had been taught, with a specific focus on their application in real-life situations. Emphasis was placed on utilizing these skills in various aspects of their lives. This phase aimed to reinforce the application of acquired skills and prepare participants for the challenges they may face beyond the therapy sessions.
- -
- Evaluation Phase (two sessions): Participants’ responses and homework assignments were used as indicators of session efficacy. Post-intervention assessments were conducted using the same instruments immediately after the program’s conclusion to evaluate the impact of problem-solving techniques in the CBT program.
2.9.5. Program Validity
2.10. Statistical Analysis
3. Results
4. Discussion
4.1. Implications
4.2. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Genovese, A.; Butler, M.G. The Autism Spectrum: Behavioral, Psychiatric and Genetic Associations. Genes 2023, 14, 677. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, B.; Wu, C.; Wang, J.; Sun, M. Autism Spectrum Disorder: Neurodevelopmental Risk Factors, Biological Mechanism, and Precision Therapy. Int. J. Mol. Sci. 2023, 24, 1819. [Google Scholar] [CrossRef] [PubMed]
- Mojarad, B.A.; Qaiser, F.; Yuen, R.K.C. Genetics and Epigenetics of ASD. In Neurodevelopmental Pediatrics: Genetic and Environmental Influences; Springer: Cham, Switzerland, 2023; pp. 293–307. [Google Scholar] [CrossRef]
- Eisenstat, D.D.; Goldowitz, D.; Oberländer, T.F.; Yager, J.Y. Neurodevelopmental Pediatrics: Genetic and Environmental Influences; Springer: Cham, Switzerland, 2023; pp. 1–832. [Google Scholar] [CrossRef]
- Li, Y.A.; Chen, Z.J.; Li, X.D.; Gu, M.H.; Xia, N.; Gong, C.; Zhou, Z.W.; Yasin, G.; Xie, H.Y.; Wei, X.P.; et al. Epidemiology of Autism Spectrum Disorders: Global Burden of Disease 2019 and Bibliometric Analysis of Risk Factors. Front. Pediatr. 2022, 10, 972809. [Google Scholar] [CrossRef] [PubMed]
- Lyu, J.C.; Luli, G.K. Understanding the Public Discussion about the Centers for Disease Control and Prevention during the COVID-19 Pandemic Using Twitter Data: Text Mining Analysis Study. J. Med. Internet Res. 2021, 23, e25108. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, N.; Li, C.; Zhang, Z.; Teng, H.; Wang, Y.; Zhao, T.; Shi, L.; Zhang, K.; Xia, K.; et al. Genetic Evidence of Gender Difference in Autism Spectrum Disorder Supports the Female-Protective Effect. Transl. Psychiatry 2020, 10, 4. [Google Scholar] [CrossRef]
- Odo, V.O.; Ukeme, W.V.; Nwanosike, L.C.; Karatu, B.A.; Urama, S.I.; Nzenwaku, J.U. Moderating Role of Motivational Preference in the Relationship between Attachment Quality and Emotional Empathy among Autistic Caregivers. Psychol. Health Med. 2023, 28, 867–875. [Google Scholar] [CrossRef] [PubMed]
- Gemegah, E.; Hartas, D.; Totsika, V. Public Attitudes to People with ASD: Contact, Knowledge and Ethnicity. Adv. Autism 2020, 7, 225–240. [Google Scholar] [CrossRef]
- Patel, A.D.; Arya, A.; Agarwal, V.; Gupta, P.K.; Agarwal, M. Burden of Care and Quality of Life in Caregivers of Children and Adolescents with Autism Spectrum Disorder. Asian J. Psychiatr. 2022, 70, 103030. [Google Scholar] [CrossRef]
- Tathgur, M.K.; Kang, H.K. Challenges of the Caregivers in Managing a Child with Autism Spectrum Disorder—A Qualitative Analysis. Indian J. Psychol. Med. 2021, 43, 416–421. [Google Scholar] [CrossRef]
- Tang, J.; Zhang, T. Causes of the Male-Female Ratio of Depression Based on the Psychosocial Factors. Front. Psychol. 2022, 13, 1052702. [Google Scholar] [CrossRef]
- Stangl, A.L.; Earnshaw, V.A.; Logie, C.H.; Van Brakel, W.; Simbayi, L.C.; Barré, I.; Dovidio, J.F. The Health Stigma and Discrimination Framework: A Global, Crosscutting Framework to Inform Research, Intervention Development, and Policy on Health-Related Stigmas. BMC Med. 2019, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Terrell, K.R.; Stanton, B.R.; Hamadi, H.Y.; Merten, J.W.; Quinn, N. Exploring Life Stressors, Depression, and Coping Strategies in College Students. J. Am. Coll. Health 2022, 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Dagani, J.; Buizza, C.; Ferrari, C.; Ghilardi, A. The Role of Psychological Distress, Stigma and Coping Strategies on Help-Seeking Intentions in a Sample of Italian College Students. BMC Psychol. 2023, 11, 177. [Google Scholar] [CrossRef]
- Al-Shammary, A.A.; Hassan, S.N.; Alshammari, F.S.; Alshammari, M.R.R. A Mixed-Method Analysis to Identify the Current Focus, Trends, and Gaps in Health Science Research in Saudi Arabia. Front. Public Health 2023, 10, 1028361. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, K.; Alahmadi, S.; Sayedahmad, A.; Mosleh, H. Psychological Well-Being of Mothers of Children with Autism in Saudi Arabia. Cureus 2022, 14, e23284. [Google Scholar] [CrossRef]
- Alruwaili, M.; Elsayed Ramadan, O.M.; Shaban, M.; Alruwaili, A.; Alsadaan, N.; Ali, S.; Al Thobaity, A.; Salihu, D. An Assessment of Pediatric Nurses Awareness and Perceived Knowledge of Autism Spectrum Disorders: A Gulf State Survey. Perspect. Psychiatr. Care 2023, 2023, 4815914. [Google Scholar] [CrossRef]
- Moran, M.J.; Murray, S.A.; LaPorte, E.; Lucas-Thompson, R.G. Associations Between Children’s Emotion Regulation, Mindful Parenting, Parent Stress, and Parent Coping during the COVID-19 Pandemic. Fam. J. 2023, 31, 426–431. [Google Scholar] [CrossRef]
- Al-Oran, H.M.; Khuan, L. Predictors of Parenting Stress in Parents of Children Diagnosed with Autism Spectrum Disorder: A Scoping Review. Egypt J. Neurol. Psychiatr. Neurosurg. 2021, 57, 103. [Google Scholar] [CrossRef]
- Lievore, R.; Lanfranchi, S.; Mammarella, I.C. Parenting Stress in Autism: Do Children’s Characteristics Still Count More than Stressors Related to the COVID-19 Pandemic? Curr. Psychol. 2023, 1–11. [Google Scholar] [CrossRef]
- Fields, A.; Harmon, C.; Lee, Z.; Louie, J.Y.; Tottenham, N. Parent’s Anxiety Links Household Stress and Young Children’s Behavioral Dysregulation. Dev. Psychobiol. 2021, 63, 16. [Google Scholar] [CrossRef]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and Health: Psychological, Behavioral, and Biological Determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607. [Google Scholar] [CrossRef]
- Baloh, R.W. Stress, Anxiety and Depression. In Exercise and the Brain: Why Physical Exercise is Essential to Peak Cognitive Health; Springer International Publishing: Cham, Switzerland, 2022; pp. 129–146. [Google Scholar] [CrossRef]
- Mulder, E.J.H.; Robles De Medina, P.G.; Huizink, A.C.; Van Den Bergh, B.R.H.; Buitelaar, J.K.; Visser, G.H.A. Prenatal Maternal Stress: Effects on Pregnancy and the (Unborn) Child. Early Hum. Dev. 2002, 70, 3–14. [Google Scholar] [CrossRef]
- Jeličić, L.; Veselinović, A.; Ćirović, M.; Jakovljević, V.; Raičević, S.; Subotić, M. Maternal Distress during Pregnancy and the Postpartum Period: Underlying Mechanisms and Child’s Developmental Outcomes—A Narrative Review. Int. J. Mol. Sci. 2022, 23, 13932. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.A.; Cooper, N.J.; Sutton, A.J.; Abrams, K.R.; Hubbard, S.J. A Review of the Quantitative Effectiveness Evidence Synthesis Methods Used in Public Health Intervention Guidelines. BMC Public Health 2021, 21, 278. [Google Scholar] [CrossRef]
- Søvold, L.E.; Naslund, J.A.; Kousoulis, A.A.; Saxena, S.; Qoronfleh, M.W.; Grobler, C.; Münter, L. Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front. Public Health 2021, 9, 679397. [Google Scholar] [CrossRef] [PubMed]
- Uy, J.P.; Tan, A.P.; Broeckman, B.B.F.P.; Gluckman, P.D.; Chong, Y.S.; Chen, H.; Fortier, M.V.; Meaney, M.J.; Callaghan, B.L. Effects of Maternal Childhood Trauma on Child Emotional Health: Maternal Mental Health and Frontoamygdala Pathways. J. Child Psychol. Psychiatry 2023, 64, 426–436. [Google Scholar] [CrossRef] [PubMed]
- Colizzi, M.; Lasalvia, A.; Ruggeri, M. Prevention and Early Intervention in Youth Mental Health: Is It Time for a Multidisciplinary and Trans-Diagnostic Model for Care? Int. J. Ment. Health Syst. 2020, 14, 23. [Google Scholar] [CrossRef]
- Singh, V.; Kumar, A.; Gupta, S. Mental Health Prevention and Promotion—A Narrative Review. Front. Psychiatry 2022, 13, 898009. [Google Scholar] [CrossRef]
- Chand, S.P.; Kuckel, D.P.; Huecker, M.R. Cognitive Behavior Therapy. In Reaching Out: The Psychology of Assertive Outreach; Routledge: London, UK, 2023; pp. 186–206. [Google Scholar]
- Alkhateeb, J.M.; Hadidi, M.S.; Mounzer, W. The Impact of Autism Spectrum Disorder on Parents in Arab Countries: A Systematic Literature Review. Front. Psychol. 2022, 13, 955442. [Google Scholar] [CrossRef]
- Solish, A.; Klemencic, N.; Ritzema, A.; Nolan, V.; Pilkington, M.; Anagnostou, E.; Brian, J. Effectiveness of a Modified Group Cognitive Behavioral Therapy Program for Anxiety in Children with ASD Delivered in a Community Context. Mol. Autism 2020, 11, 34. [Google Scholar] [CrossRef]
- Kilburn, T.R.; Sørensen, M.J.; Thastum, M.; Rapee, R.M.; Rask, C.U.; Arendt, K.B.; Carlsen, A.H.; Thomsen, P.H. Group Based Cognitive Behavioural Therapy for Anxiety in Children with Autism Spectrum Disorder: A Randomised Controlled Trial in a General Child Psychiatric Hospital Setting. J. Autism Dev. Disord. 2023, 53, 525–538. [Google Scholar] [CrossRef]
- Kalvin, C.B.; Jordan, R.P.; Rowley, S.N.; Weis, A.; Wood, K.S.; Wood, J.J.; Ibrahim, K.; Sukhodolsky, D.G. Conducting CBT for Anxiety in Children with Autism Spectrum Disorder during COVID-19 Pandemic. J. Autism Dev. Disord. 2021, 51, 4239–4247. [Google Scholar] [CrossRef] [PubMed]
- Fenn, M.K.; Byrne, D.M. The Key Principles of Cognitive Behavioural Therapy. InnovAiT 2013, 6, 579–585. [Google Scholar] [CrossRef]
- Alallawi, B.; Hastings, R.P.; Gray, G. A Systematic Scoping Review of Social, Educational, and Psychological Research on Individuals with Autism Spectrum Disorder and Their Family Members in Arab Countries and Cultures. Rev. J. Autism Dev. Disord. 2020, 7, 364–382. [Google Scholar] [CrossRef]
- Fordham, B.; Sugavanam, T.; Hopewell, S.; Hemming, K.; Howick, J.; Kirtley, S.; Das Nair, R.; Hamer-Hunt, J.; Lamb, S.E. Effectiveness of Cognitive–Behavioural Therapy: A Protocol for an Overview of Systematic Reviews and Meta-Analyses. BMJ Open 2018, 8, e025761. [Google Scholar] [CrossRef] [PubMed]
- Naeem, F. Cultural Adaptations of CBT: A Summary and Discussion of the Special Issue on Cultural Adaptation of CBT. Cogn. Behav. Ther. 2019, 12, e40. [Google Scholar] [CrossRef]
- Bhugra, D.; Watson, C.; Wijesuriya, R. Culture and Mental Illnesses. Int. Rev. Psychiatry 2021, 33, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Pourmand, V.; Lawley, K.A.; Lehman, B.J. Cultural Differences in Stress and Affection Following Social Support Receipt. PLoS ONE 2021, 16, e0256859. [Google Scholar] [CrossRef] [PubMed]
- Fincham, G.W.; Strauss, C.; Montero-Marin, J.; Cavanagh, K. Effect of Breathwork on Stress and Mental Health: A Meta-Analysis of Randomised-Controlled Trials. Sci. Rep. 2023, 13, 432. [Google Scholar] [CrossRef]
- Kendall, P.C.; Ney, J.S.; Maxwell, C.A.; Lehrbach, K.R.; Jakubovic, R.J.; McKnight, D.S.; Friedman, A.L. Adapting CBT for Youth Anxiety: Flexibility, within Fidelity, in Different Settings. Front. Psychiatry 2023, 14, 1067047. [Google Scholar] [CrossRef]
- Matthys, W.; Schutter, D.J.L.G. Moral Thinking and Empathy in Cognitive Behavioral Therapy for Children and Adolescents with Conduct Problems: A Narrative Review. Clin. Child Fam. Psychol. Rev. 2023, 26, 401–415. [Google Scholar] [CrossRef]
- Matson, J.L. Handbook of Clinical Child Psychology: Integrating Theory and Research into Practice; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Riise, E.N.; Haugland, B.S.M.; Wergeland, G.J.H. Cognitive Behavioral Therapy (CBT) with Children and Adolescents. In Handbook of Clinical Child Psychology; Springer: Cham, Switzerland, 2023; pp. 407–424. [Google Scholar] [CrossRef]
- Sadler, S.; Sadler, P.P.; Sadler, P. Self-Efficacy Theory. In Encyclopedia of Personality and Individual Differences; Springer: Cham, Switzerland, 2020; pp. 4722–4727. [Google Scholar] [CrossRef]
- Linge, A.D.; Bjørkly, S.K.; Jensen, C.; Hasle, B. Bandura’s Self-Efficacy Model Used to Explore Participants’ Experiences of Health, Lifestyle, and Work after Attending a Vocational Rehabilitation Program with Lifestyle Intervention—A Focus Group Study. J. Multidiscip. Healthc. 2021, 14, 3533. [Google Scholar] [CrossRef] [PubMed]
- Ghanouni, P.; Hood, G. Stress, Coping, and Resiliency among Families of Individuals with Autism: A Systematic Review. Rev. J. Autism Dev. Disord. 2021, 8, 389–402. [Google Scholar] [CrossRef]
- Kubo, N.; Kitagawa, M.; Iwamoto, S.; Kishimoto, T. Effects of an Attachment-Based Parent Intervention on Mothers of Children with Autism Spectrum Disorder: Preliminary Findings from a Non-Randomized Controlled Trial. Child Adolesc. Psychiatry Ment. Health 2021, 15, 37. [Google Scholar] [CrossRef] [PubMed]
- Samadi, H.; Samadi, S.A. Understanding Different Aspects of Caregiving for Individuals with Autism Spectrum Disorders (ASDs) a Narrative Review of the Literature. Brain Sci. 2020, 10, 557. [Google Scholar] [CrossRef]
- Schwichtenberg, A.J.; Kellerman, A.M.; Young, G.S.; Miller, M.; Ozonoff, S. Mothers of Children with Autism Spectrum Disorders: Play Behaviors with Infant Siblings and Social Responsiveness. Autism 2019, 23, 821–833. [Google Scholar] [CrossRef] [PubMed]
- Lamba, N.; Van Tonder, A.; Shrivastava, A.; Raghavan, A. Exploring Challenges and Support Structures of Mothers with Children with Autism Spectrum Disorder in the United Arab Emirates. Res. Dev. Disabil. 2022, 120, 104138. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Xu, M.; Wu, D.; Tang, Y.; Zhang, L.; Liu, X.; Zhou, L.; Li, F.; Jiang, L. From Child Social Impairment to Parenting Stress in Mothers of Children with ASD: The Role of Parental Self-Efficacy and Social Support. Front. Psychiatry 2022, 13, 1005748. [Google Scholar] [CrossRef]
- McIntyre, L.L.; Brown, M. Examining the Utilisation and Usefulness of Social Support for Mothers with Young Children with Autism Spectrum Disorder. J. Intellect. Dev. Disabil. 2018, 43, 93. [Google Scholar] [CrossRef]
- Lee, J.; Lee, E.H.; Moon, S.H. Systematic Review of the Measurement Properties of the Depression Anxiety Stress Scales–21 by Applying Updated COSMIN Methodology. Qual. Life Res. 2019, 28, 2325–2339. [Google Scholar] [CrossRef]
- Ali, A.M.; Green, J. Factor Structure of the Depression Anxiety Stress Scale-21 (DASS-21): Unidimensionality of the Arabic Version among Egyptian Drug Users. Subst. Abuse Treat. Prev. Policy 2019, 14, 40. [Google Scholar] [CrossRef]
- Sahin, N.; Sahin, N.H.; Heppner, P.P. Psychometric properties of the problem-solving inventory in a group of Turkish University-students. Cognit. Ther. Res. 1993, 17, 379–396. [Google Scholar] [CrossRef]
- Antony, M.M.; Cox, B.J.; Enns, M.W.; Bieling, P.J.; Swinson, R.P. Psychometric Properties of the 42-Item and 21-Item Versions of the Depression Anxiety Stress Scales in Clinical Groups and a Community Sample. Psychol. Assess 1998, 10, 176–181. [Google Scholar] [CrossRef]
- Heppner, P.P.; Petersen, C.H. The Development and Implications of a Personal Problem-Solving Inventory. J. Couns. Psychol. 1982, 29, 66–75. [Google Scholar] [CrossRef]
- Kazantzis, N.; Luong, H.K.; Usatoff, A.S.; Impala, T.; Yew, R.Y.; Hofmann, S.G. The Processes of Cognitive Behavioral Therapy: A Review of Meta-Analyses. Cognit. Ther. Res. 2018, 42, 349–357. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: Toward a Unifying Theory of Behavioral Change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Strunk, D.R.; Adler, A.D.; Hollars, S.N. Cognitive Therapy Skills Predict Cognitive Reactivity to Sad Mood Following Cognitive Therapy for Depression. Cognit. Ther. Res. 2013, 37, 1214–1219. [Google Scholar] [CrossRef] [PubMed]
- McGuire, A.; Steele, R.G.; Singh, M.N. Systematic Review on the Application of Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) for Preschool-Aged Children. Clin. Child Fam. Psychol. Rev. 2021, 24, 20–37. [Google Scholar] [CrossRef] [PubMed]
- Stikkelbroek, Y.; Vink, G.; Nauta, M.H.; Bottelier, M.A.; Vet, L.J.J.; Lont, C.M.; van Baar, A.L.; Bodden, D.H.M. Effectiveness and Moderators of Individual Cognitive Behavioral Therapy versus Treatment as Usual in Clinically Depressed Adolescents: A Randomized Controlled Trial. Sci. Rep. 2020, 10, 14815. [Google Scholar] [CrossRef] [PubMed]
- Nakao, M.; Shirotsuki, K.; Sugaya, N. Cognitive–Behavioral Therapy for Management of Mental Health and Stress-Related Disorders: Recent Advances in Techniques and Technologies. Biopsychosoc. Med. 2021, 15, 16. [Google Scholar] [CrossRef]
- Ozonoff, S.; Goodlin-Jones, B.L.; Solomon, M. Evidence-Based Assessment of Autism Spectrum Disorders in Children and Adolescents. J. Clin. Child Adolesc. Psychol. 2005, 34, 523–540. [Google Scholar] [CrossRef]
- Ulrich, B.; Barden, C.; Cassidy, L.; Varn-Davis, N. Critical Care Nurse Work Environments 2018: Findings and Implications. Crit. Care Nurse 2019, 39, 67–84. [Google Scholar] [CrossRef] [PubMed]
- Scarpinato, N.; Bradley, J.; Kurbjun, K.; Bateman, X.; Holtzer, B.; Ely, B. Caring for the Child with an Autism Spectrum Disorder in the Acute Care Setting. J. Spec. Pediatr. Nurs. 2010, 15, 244–254. [Google Scholar] [CrossRef]
- Kavanagh, M.; Brouwer, K.; Lawrence, P. Comparing the Effectiveness of an 8-Week and 12-Week Cognitive Behavioural Therapy Group for Bipolar Affective Disorder. J. Affect. Disord. Rep. 2021, 6, 100244. [Google Scholar] [CrossRef]
- Van Lieshout, R.J.; Layton, H.; Savoy, C.D.; Haber, E.; Feller, A.; Biscaro, A.; Bieling, P.J.; Ferro, M.A. Public Health Nurse-Delivered Group Cognitive Behavioural Therapy for Postpartum Depression: A Randomized Controlled Trial. Can. J. Psychiatry 2022, 67, 432–440. [Google Scholar] [CrossRef]
- Hargitai, L.D.; Livingston, L.A.; Waldren, L.H.; Robinson, R.; Jarrold, C.; Shah, P. Attention-Deficit Hyperactivity Disorder Traits Are a More Important Predictor of Internalising Problems than Autistic Traits. Sci. Rep. 2023, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Fredrick, S.S.; Nickerson, A.B.; Sun, L.; Rodgers, J.D.; Thomeer, M.L.; Lopata, C.; Todd, F. ASD Symptoms, Social Skills, and Comorbidity: Predictors of Bullying Perpetration. J. Autism Dev. Disord. 2023, 53, 3092–3102. [Google Scholar] [CrossRef] [PubMed]
- Dellapiazza, F.; Michelon, C.; Picot, M.C.; Baghdadli, A. Early Risk Factors for Anxiety Disorders in Children with Autism Spectrum Disorders: Results from the ELENA Cohort. Sci. Rep. 2022, 12, 10914. [Google Scholar] [CrossRef]
- Lindor, E.; Sivaratnam, C.; May, T.; Stefanac, N.; Howells, K.; Rinehart, N. Problem Behavior in Autism Spectrum Disorder: Considering Core Symptom Severity and Accompanying Sleep Disturbance. Front. Psychiatry 2019, 10, 487. [Google Scholar] [CrossRef]
- Brown, C.E.; Quetsch, L.B.; Aloia, L.S.; Kanne, S.M. Predictors of Aggression, Disruptive Behavior, and Anger Dysregulation in Youths with Autism Spectrum Disorder. J. Autism Dev. Disord. 2023, 1–17. [Google Scholar] [CrossRef]
- Mansour, R.; Ward, A.R.; Lane, D.M.; Loveland, K.A.; Aman, M.G.; Jerger, S.; Schachar, R.J.; Pearson, D.A. ADHD Severity as a Predictor of Cognitive Task Performance in Children with Autism Spectrum Disorder (ASD). Res. Dev. Disabil. 2021, 111, 103882. [Google Scholar] [CrossRef] [PubMed]
| Participants’ Characteristics | All Participants (n = 60) | Study Group (n = 30) | Control Group (n = 30) | χ2 | p | |||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||
| Age (years) | ||||||||
| 20–30 | 25 | 41.7 | 11 | 36.7 | 14 | 46.7 | 0.789 | 0.674 |
| 30–40 | 14 | 23.3 | 7 | 23.3 | 7 | 23.3 | ||
| 40–50 | 21 | 35.0 | 12 | 40.0 | 9 | 30.0 | ||
| Mean ± SD | 34.80 ± 10.25 | 35.53 ± 10.81 | 34.07 ± 9.78 | 0.551 | 0.584 | |||
| Education | ||||||||
| Elementary education | 32 | 53.3 | 11 | 36.7 | 21 | 70.0 | 7.081 * | 0.029 * |
| Secondary education | 18 | 30.0 | 13 | 43.3 | 5 | 16.7 | ||
| University | 10 | 16.7 | 6 | 20.0 | 4 | 13.3 | ||
| Mother occupation | ||||||||
| Working | 28 | 46.7 | 15 | 50.0 | 13 | 43.3 | 0.268 | 0.605 |
| Housewife | 32 | 53.3 | 15 | 50.0 | 17 | 56.7 | ||
| Adequacy of monthly income | ||||||||
| Adequacy | 26 | 43.3 | 11 | 36.7 | 15 | 50.0 | 1.086 | 0.297 |
| Inadequate | 34 | 56.7 | 19 | 63.3 | 15 | 50.0 | ||
| Marital status | ||||||||
| Married | 32 | 53.3 | 21 | 70.0 | 11 | 36.7 | 6.696 * | 0.010 * |
| Other | 28 | 46.7 | 9 | 30.0 | 19 | 63.3 | ||
| Child’s age | ||||||||
| 4–8 | 32 | 53.3 | 18 | 60.0 | 14 | 46.7 | 1.071 | 0.301 |
| 8–12 | 28 | 46.7 | 12 | 40.0 | 16 | 53.3 | ||
| Child’s sex | ||||||||
| Male | 41 | 68.4 | 25 | 61 | 16 | 39 | 0.601 | 0.438 |
| Female | 19 | 31.6 | 9 | 47.3 | 10 | 52.7 | ||
| Severity of autism | ||||||||
| Mild | 23 | 38.3 | 12 | 40.0 | 11 | 36.7 | 0.287 | 0.866 |
| Moderate | 24 | 40.0 | 11 | 36.7 | 13 | 43.3 | ||
| Severe | 13 | 21.7 | 7 | 23.3 | 6 | 20.0 | ||
| Depression Anxiety Stress Scale (DASS-21) | All Participants (n = 60) | Study Group (n = 30) | Control Group (n = 30) | Test of Sig. (p1) | Test of Sig. (p2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | |||||||||
| No | % | No | % | No | % | No | % | No | % | No | % | |||
| Depression | ||||||||||||||
| Normal | 2 | 3.3 | 11 | 18.3 | 2 | 6.7 | 9 | 30.0 | 0 | 0.0 | 2 | 6.7 | χ2 = 2.263 (MCp = 0.386) | χ2 = 8.909 * (0.012 *) |
| Mild | 36 | 60.0 | 38 | 63.3 | 16 | 53.3 | 19 | 63.3 | 20 | 66.7 | 19 | 63.3 | ||
| Moderate | 22 | 36.7 | 11 | 18.3 | 12 | 40.0 | 2 | 6.7 | 10 | 33.3 | 9 | 30.0 | ||
| Total score | 13.70 ± 3.10 | 12.23 ± 2.90 | 13.60 ± 3.50 | 11.07 ± 2.27 | 13.80 ± 2.70 | 13.40 ± 3.02 | t1 = 0.248 (0.805) | t1 = 3.378 * (0.001 *) | ||||||
| % score | 32.62 ± 7.38 | 29.13 ± 6.91 | 32.38 ± 8.33 | 26.35 ± 5.41 | 32.86 ± 6.42 | 31.90 ± 7.20 | ||||||||
| t2 (p0) | 3.496 * (0.001 *) | 4.080 * (<0.001 *) | 0.797 (0.432) | |||||||||||
| % reduction | 7.70 ± 24.80 | 13.68 ± 29.11 | 1.73 ± 18.16 | U = 270.0 * (0.004 *) | ||||||||||
| Anxiety | ||||||||||||||
| Normal | 3 | 5.0 | 9 | 15.0 | 2 | 6.7 | 7 | 23.3 | 1 | 3.3 | 2 | 6.7 | χ2 = 0.927 (MCp = 1.000) | χ2 = 20.076 * (MCp < 0.001 *) |
| Mild | 11 | 18.3 | 15 | 25 | 5 | 16.6 | 13 | 43.3 | 6 | 20 | 2 | 6.6 | ||
| Moderate | 23 | 38.3 | 26 | 43.3 | 12 | 40.0 | 8 | 26.7 | 11 | 36.7 | 18 | 60.0 | ||
| Severe | 23 | 38.3 | 10 | 16.7 | 11 | 36.7 | 2 | 6.7 | 12 | 40.0 | 8 | 26.7 | ||
| Total score | 14.40 ± 4.40 | 11.13 ± 5.11 | 14.13 ± 4.55 | 9.13 ± 5.22 | 14.67 ±4.31 | 13.13 ± 4.19 | t1 = 0.466 (0.643) | t1 = 3.274 * (0.002 *) | ||||||
| % score | 34.29 ± 10.48 | 26.51 ± 12.16 | 33.65 ± 10.83 | 21.75 ± 12.42 | 34.92 ± 10.26 | 31.27 ± 9.98 | ||||||||
| t2 (p0) | 5.195 * (<0.001 *) | 5.732 * (<0.001 *) | 1.916 (0.065) | |||||||||||
| % reduction | 21.03 ± 34.61 | 33.94 ± 28.79 | 8.55 ± 35.61 | U = 237.000 * (0.003 *) | ||||||||||
| Stress | ||||||||||||||
| Normal | 22 | 36.7 | 29 | 48.3 | 13 | 43.3 | 22 | 73.3 | 9 | 30.0 | 7 | 23.3 | χ2 = 1.304 (MCp = 0.788) | χ2 = 19.377 * (MCp < 0.001 *) |
| Mild | 13 | 21.7 | 14 | 23.3 | 6 | 20.0 | 6 | 20.0 | 7 | 23.3 | 8 | 26.7 | ||
| Moderate | 20 | 33.3 | 9 | 15.0 | 9 | 30.0 | 2 | 6.7 | 11 | 36.7 | 7 | 23.3 | ||
| Severe | 5 | 8.3 | 8 | 13.3 | 2 | 6.7 | 0 | 0.0 | 3 | 10.0 | 8 | 26.7 | ||
| Total score | 17.83 ± 5.0 | 15.63 ± 6.77 | 16.80 ± 5.29 | 12.87 ± 4.75 | 18.87 ± 4.54 | 18.40 ± 7.42 | t1 = 1.623 (0.110) | t1 = 3.423 * (0.001 *) | ||||||
| % score | 42.46 ± 11.90 | 37.28 ± 16.07 | 40.0 ± 12.61 | 30.74 ± 11.20 | 44.92 ± 10.81 | 43.81 ± 17.66 | ||||||||
| t2 (p0) | 2.676 * (0.010 *) | 5.894 * (<0.001 *) | 0.325 (0.747) | |||||||||||
| % reduction | 10.19 ± 39.71 | 22.17 ± 20.95 | 1.79 ± 49.73 | U = 315.500 * (0.046 *) | ||||||||||
| Overall DASS-21 | ||||||||||||||
| Total score | 45.93 ± 9.03 | 39.0 ± 11.32 | 44.53 ± 9.91 | 33.07 ± 8.59 | 47.33 ± 7.97 | 44.93 ± 10.67 | t1 = 1.206 (0.233) | t1 = 4.744 * (<0.001 *) | ||||||
| % score | 36.46 ± 7.16 | 30.95 ± 8.98 | 35.34 ± 7.86 | 26.24 ± 6.82 | 37.57 ± 6.33 | 35.66 ± 8.47 | ||||||||
| t2 (p0) | 5.456 * (<0.001 *) | 10.656 * (<0.001 *) | 1.201 (0.240) | |||||||||||
| % reduction | 14.31 ± 22.72 | 24.75 ± 14.07 | 3.86 ± 25.04 | U = 188.000 * (<0.001 *) | ||||||||||
| Problem-Solving Skills Scale | All Participants (n = 60) | Study Group (n = 30) | Control Group (n = 30) | Test of Sig. (p1) | Test of Sig. (p2) | |||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | |||
| Problem-Solving Confidence (PSC) | ||||||||
| Total score | 40.23 ± 5.24 | 38.23 ± 5.35 | 40.73 ± 5.01 | 36.83 ± 5.11 | 39.73 ± 5.50 | 39.63 ± 5.30 | t1 = 0.737 (0.464) | t1 = 2.084 * (0.042 *) |
| % score | 53.15 ± 9.52 | 49.52 ± 9.73 | 54.06 ± 9.11 | 46.97 ± 9.28 | 52.24 ± 9.99 | 52.06 ± 9.64 | ||
| t2 (p0) | 2.204 * (0.031 *) | 3.158 * (0.004 *) | 0.080 (0.937) | |||||
| % reduction | 3.38 ± 18.22 | 8.21 ± 17.34 | 1.45 ± 18.06 | t = 2.113 * (0.039 *) | ||||
| Approach–Avoidance Style (AAS)1 | ||||||||
| Total score | 57.00 ± 5.49 | 52.35 ± 6.54 | 56.80 ± 5.83 | 48.90 ± 4.82 | 57.20 ± 5.22 | 55.80 ± 6.25 | t1 = 0.280 (0.780) | t1 = 4.944 * (<0.001 *) |
| % score | 51.25 ± 6.86 | 45.50 ± 8.10 | 51.00 ± 7.28 | 41.13 ± 6.03 | 51.50 ± 6.53 | 49.87 ± 7.58 | ||
| t2 (p0) | 5.357 * (<0.001 *) | 6.816 * (<0.001 *) | 1.368 (0.182) | |||||
| % reduction | 7.76 ± 11.11 | 13.28 ± 10.21 | −2.24 ± 9.14 | t = 4.409 * (<0.001 *) | ||||
| Personal Control (PC) | ||||||||
| Total score | 19.32 ± 3.41 | 18.17 ± 3.89 | 19.03 ± 2.55 | 16.87 ± 4.61 | 19.60 ± 4.12 | 19.47 ± 2.47 | t1 = 0.640 (0.525) | t1 = 2.723 * (0.009 *) |
| % score | 57.27 ± 13.65 | 52.67 ± 15.57 | 56.13 ± 10.21 | 47.47 ± 18.43 | 58.40 ± 16.50 | 57.87 ± 9.90 | ||
| t2 (p0) | 5.220 * (<0.001 *) | 2.078 * (0.047 *) | 0.188 (0.852) | |||||
| % reduction | 2.02 ± 31.16 | 9.06 ± 28.95 | 5.01 ± 32.16 | t = 1.781 (0.080) | ||||
| Overall problem-solving skills scale | ||||||||
| Total score | 116.55 ± 8.58 | 108.77 ± 9.48 | 116.57 ± 7.46 | 102.60 ± 6.75 | 116.53 ± 9.70 | 114.93 ± 7.65 | t1 = 0.015 (0.988) | t1 = 6.623 * (<0.001 *) |
| % score | 52.84 ± 5.36 | 47.98 ± 5.92 | 52.85 ± 4.66 | 44.13 ± 4.22 | 52.83 ± 6.06 | 51.83 ± 4.78 | ||
| t2 (p0) | 5.290 * (<0.001 *) | 7.691 * (<0.001 *) | 0.944(0.353) | |||||
| % reduction | 6.29 ± 9.38 | 11.65 ± 7.75 | 0.93 ± 7.71 | t = 5.370 * (<0.001 *) | ||||
| Overall DASS-21 | Overall PSI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Beta | t | p | 95% CI | B | Beta | t | p | 95% CI | |||
| LL | UL | LL | UL | |||||||||
| Age of mother | −0.023 | −0.036 | 0.284 | 0.779 | −0.189 | 0.144 | 0.188 | 0.482 | 3.908 * | 0.001 * | 0.088 | 0.287 |
| Education | −1.337 | −0.146 | 1.060 | 0.300 | −3.945 | 1.272 | 0.871 | 0.154 | 1.156 | 0.260 | −0.687 | 2.429 |
| Adequacy of financial | 3.402 | 0.244 | 1.793 | 0.086 | −0.522 | 7.325 | 4.938 | 0.574 | 4.359 * | <0.001 * | 2.595 | 7.281 |
| Marital status | −1.163 | −0.079 | 0.588 | 0.562 | −5.255 | 2.930 | −0.208 | −0.023 | 0.176 | 0.862 | −2.652 | 2.236 |
| Child age | 6.273 | 0.458 | 3.128 * | 0.005 * | 2.125 | 10.420 | −0.229 | −0.027 | 0.191 | 0.850 | −2.706 | 2.248 |
| Severity of autism | 2.268 | 0.263 | 2.144 * | 0.043 * | 0.080 | 4.456 | 0.702 | 0.132 | 1.111 | 0.278 | −0.605 | 2.008 |
| R2 = 0.741, F = 10.944 *, p < 0.001 * | R2 = 0.758, F = 12.016 *, p < 0.001 * | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdelaziz, E.M.; Alsadaan, N.; Alqahtani, M.; Elsharkawy, N.B.; Ouda, M.M.A.; Ramadan, O.M.E.; Shaban, M.; Shokre, E.S. Effectiveness of Cognitive Behavioral Therapy (CBT) on Psychological Distress among Mothers of Children with Autism Spectrum Disorder: The Role of Problem-Solving Appraisal. Behav. Sci. 2024, 14, 46. https://doi.org/10.3390/bs14010046
Abdelaziz EM, Alsadaan N, Alqahtani M, Elsharkawy NB, Ouda MMA, Ramadan OME, Shaban M, Shokre ES. Effectiveness of Cognitive Behavioral Therapy (CBT) on Psychological Distress among Mothers of Children with Autism Spectrum Disorder: The Role of Problem-Solving Appraisal. Behavioral Sciences. 2024; 14(1):46. https://doi.org/10.3390/bs14010046
Chicago/Turabian StyleAbdelaziz, Enas Mahrous, Nourah Alsadaan, Mohammed Alqahtani, Nadia Bassuoni Elsharkawy, Marwa Mohamed Ahmed Ouda, Osama Mohamed Elsayed Ramadan, Mostafa Shaban, and Evon S. Shokre. 2024. "Effectiveness of Cognitive Behavioral Therapy (CBT) on Psychological Distress among Mothers of Children with Autism Spectrum Disorder: The Role of Problem-Solving Appraisal" Behavioral Sciences 14, no. 1: 46. https://doi.org/10.3390/bs14010046
APA StyleAbdelaziz, E. M., Alsadaan, N., Alqahtani, M., Elsharkawy, N. B., Ouda, M. M. A., Ramadan, O. M. E., Shaban, M., & Shokre, E. S. (2024). Effectiveness of Cognitive Behavioral Therapy (CBT) on Psychological Distress among Mothers of Children with Autism Spectrum Disorder: The Role of Problem-Solving Appraisal. Behavioral Sciences, 14(1), 46. https://doi.org/10.3390/bs14010046









