Exploration of Psychiatry Residents’ Attitudes toward Patients with Substance Use Disorder, Bipolar Disorder and Schizophrenia in Saudi Arabia
Abstract
1. Introduction
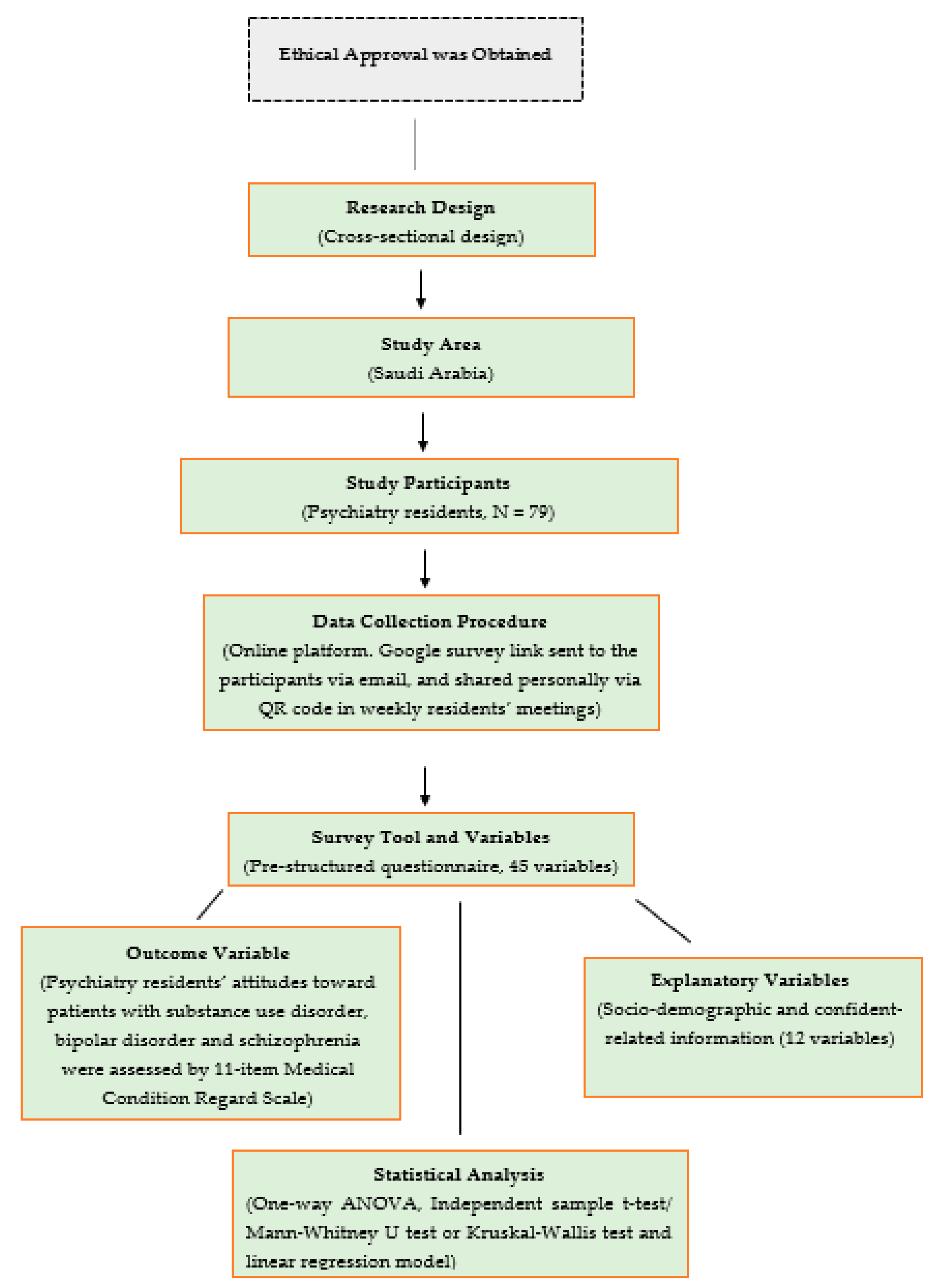
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Participants and Study Procedures
2.3. Study Variables and Measurement
2.3.1. Outcome Measurement
2.3.2. Explanatory Variables
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Attitudes toward Patients with Different Conditions and Their Associated Factors
4. Discussion
Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- APA. Substance-Related and Addictive Disorders. Diagn. Stat. Man. Ment. Disord. 2013, 5, 908–978. [Google Scholar]
- Saquib, N.; Rajab, A.M.; Saquib, J.; AlMazrou, A. Substance Use Disorders in Saudi Arabia: A Scoping Review. Subst. Abuse Treat. Prev. Policy 2020, 15, 41. [Google Scholar] [CrossRef] [PubMed]
- Bassiony, M. Substance Use Disorders in Saudi Arabia. J. Subst. Use 2013, 18, 450–466. [Google Scholar] [CrossRef]
- WHO. Investing in Mental Health; World Health Organization: Geneva, Switzerland, 2003; ISBN 9241562579. [Google Scholar]
- WHO. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2019; ISBN 9241565632. [Google Scholar]
- Van Boekel, L.C.; Brouwers, E.P.M.; Van Weeghel, J.; Garretsen, H.F.L. Stigma among Health Professionals towards Patients with Substance Use Disorders and Its Consequences for Healthcare Delivery: Systematic Review. Drug Alcohol Depend. 2013, 131, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Almutairi, A.F. Mental Illness in Saudi Arabia: An Overview. Psychol. Res. Behav. Manag. 2015, 8, 47–49. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; AlAteeq, D.A.; Bin Hussain, S.I.; Alhenaki, R.S.; Bin Salamah, A.A.; AlModihesh, N.A. Public Awareness, Beliefs, and Attitudes toward Bipolar Disorder in Saudi Arabia. Neuropsychiatr. Dis. Treat. 2019, 15, 2809–2818. [Google Scholar] [CrossRef]
- Roxanne Dryden-Edwards Bipolar Disorder, vs. Schizophrenia. Available online: https://www.medicinenet.com/bipolar_disorder_vs_schizophrenia/article.htm (accessed on 23 March 2023).
- Tyrovolas, S.; El Bcheraoui, C.; Alghnam, S.A.; Alhabib, K.F.; Almadi, M.A.H.; Al-Raddadi, R.M.; Bedi, N.; El Tantawi, M.; Krish, V.S.; Memish, Z.A. The Burden of Disease in Saudi Arabia 1990–2017: Results from the Global Burden of Disease Study 2017. Lancet Planet. Health 2020, 4, e195–e208. [Google Scholar] [CrossRef]
- Alshowkan, A.; Curtis, J.; White, Y. Factors Affecting the Quality of Life for People with Schizophrenia in Saudi Arabia: A Qualitative Study. J. Psychiatry 2015, 18, 1000295. [Google Scholar] [CrossRef]
- Kronfol, Z.; Zakaria Khalil, M.; Kumar, P.; Suhre, K.; Karam, E.; McInnis, M. Bipolar Disorders in the Arab World: A Critical Review. Ann. N. Y. Acad. Sci. 2015, 1345, 59–66. [Google Scholar] [CrossRef]
- Alharbi, R.B. The Prevalence of Stigmatizing Beliefs towards Mental Illness and Mental Health Nursing among Third-Year Undergraduate Nursing Students in Riyadh, Saudi Arabia: A Review. Eur. J. Med. Health Sci. 2023, 5, 41–48. [Google Scholar] [CrossRef]
- Al Hamad, A.M.; Al Sawaf, M.H.; Osman, A.A. Differential Aspects of Consultation-Liaison Psychiatry in a Saudi Hospital. II: Knowledge and Attitudes of Physicians and Patients. EMHJ East. Mediterr. Health J. 2006, 12, 324–330. [Google Scholar]
- Kendler, K.S.; Myers, J. Addiction Resistance: Definition, Validation and Association with Mastery. Drug Alcohol Depend. 2015, 154, 236–242. [Google Scholar] [CrossRef]
- Hoffmeister, J.R.; Cohoon, A.J.; Sorocco, K.H.; Acheson, A.; Lovallo, W.R. Addiction Resistance to Alcohol: What about Heavy Drinkers Who Avoid Alcohol Problems? Drug Alcohol Depend. 2019, 204, 107552. [Google Scholar] [CrossRef] [PubMed]
- Jakubiec, L.; Chirokoff, V.; Abdallah, M.; Sanz-Arigita, E.; Dupuy, M.; Swendsen, J.; Berthoz, S.; Gierski, F.; Guionnet, S.; Misdrahi, D. The Executive Functioning Paradox in Substance Use Disorders. Biomedicines 2022, 10, 2728. [Google Scholar] [CrossRef] [PubMed]
- Tronson, N.C.; Taylor, J.R. Addiction: A Drug-Induced Disorder of Memory Reconsolidation. Curr. Opin. Neurobiol. 2013, 23, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Fountoulakis, K.N.; Yatham, L.N.; Grunze, H.; Vieta, E.; Young, A.H.; Blier, P.; Tohen, M.; Kasper, S.; Moeller, H.J. The CINP Guidelines on the Definition and Evidence-Based Interventions for Treatment-Resistant Bipolar Disorder. Int. J. Neuropsychopharmacol. 2020, 23, 230–256. [Google Scholar]
- Vieta, E.; Goikolea, J.M. Atypical Antipsychotics: Newer Options for Mania and Maintenance Therapy. Bipolar Disord. 2005, 7, 21–33. [Google Scholar] [CrossRef]
- Manning, J.S. Burden of Illness in Bipolar Depression. Prim. Care Companion J. Clin. Psychiatry 2005, 7, 259. [Google Scholar] [CrossRef]
- Keller, M.B.; Lavori, P.W.; Kane, J.M.; Gelenberg, A.J.; Rosenbaum, J.F.; Walzer, E.A.; Baker, L.A. Subsyndromal Symptoms in Bipolar Disorder: A Comparison of Standard and Low Serum Levels of Lithium. Arch. Gen. Psychiatry 1992, 49, 371–376. [Google Scholar] [CrossRef]
- Panov, G. Dissociative Model in Patients with Resistant Schizophrenia. Front. Psychiatry 2022, 13, 845493. [Google Scholar] [CrossRef]
- Gillespie, A.L.; Samanaite, R.; Mill, J.; Egerton, A.; MacCabe, J.H. Is Treatment-Resistant Schizophrenia Categorically Distinct from Treatment-Responsive Schizophrenia? A Systematic Review. BMC Psychiatry 2017, 17, 12. [Google Scholar] [CrossRef] [PubMed]
- Schulze, B. Stigma and Mental Health Professionals: A Review of the Evidence on an Intricate Relationship. Int. Rev. Psychiatry 2007, 19, 137–155. [Google Scholar] [CrossRef] [PubMed]
- Rao, H.; Mahadevappa, H.; Pillay, P.; Sessay, M.; Abraham, A.; Luty, J. A Study of Stigmatized Attitudes towards People with Mental Health Problems among Health Professionals. J. Psychiatr. Ment. Health Nurs. 2009, 16, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Avery, J.; Zerbo, E.; Ross, S. Improving Psychiatrists’ Attitudes towards Individuals with Psychotic Disorders and Co-Occurring Substance Use Disorders. Acad. Psychiatry 2016, 40, 520–522. [Google Scholar] [CrossRef]
- Avery, J.; Zerbo, E. Improving Psychiatry Residents’ Attitudes toward Individuals Diagnosed with Substance Use Disorders. Harv. Rev. Psychiatry 2015, 23, 296–300. [Google Scholar] [CrossRef]
- Gilchrist, G.; Moskalewicz, J.; Slezakova, S.; Okruhlica, L.; Torrens, M.; Vajd, R.; Baldacchino, A. Staff Regard towards Working with Substance Users: A European Multi-centre Study. Addiction 2011, 106, 1114–1125. [Google Scholar] [CrossRef]
- Avery, J.; Han, B.H.; Zerbo, E.; Wu, G.; Mauer, E.; Avery, J.; Ross, S.; Penzner, J.B. Changes in Psychiatry Residents’ Attitudes towards Individuals with Substance Use Disorders over the Course of Residency Training. Am. J. Addict. 2016, 26, 75–79. [Google Scholar] [CrossRef]
- Christison, G.W.; Haviland, M.G.; Riggs, M.L. The Medical Condition Regard Scale: Measuring Reactions to Diagnoses. Acad. Med. 2002, 77, 257–262. [Google Scholar] [CrossRef]
- Avery, J.; Dixon, L.; Adler, D.; Oslin, D.; Hackman, A.; First, M.; Goldman, B.; Koh, S.; Nossel, I.; Siris, S. Psychiatrists’ Attitudes toward Individuals with Substance Use Disorders and Serious Mental Illness. J. Dual Diagn. 2013, 9, 322–326. [Google Scholar] [CrossRef]
- Ducray, K.; Pilch, M. Health Student Regard for Substance-Using Patients as Measured by the Medical Condition Regard Scale: A Systematic Review. Ir. J. Psychol. Med. 2017, 34, 183–196. [Google Scholar] [CrossRef]
- Daoud, J.I. Multicollinearity and Regression Analysis. J. Phys. Conf. Ser. 2017, 949, 12009. [Google Scholar] [CrossRef]
- O’brien, R.M. A Caution Regarding Rules of Thumb for Variance Inflation Factors. Qual. Quant. 2007, 41, 673–690. [Google Scholar] [CrossRef]
- Livingston, J.D.; Milne, T.; Fang, M.L.; Amari, E. The Effectiveness of Interventions for Reducing Stigma Related to Substance Use Disorders: A Systematic Review. Addiction 2012, 107, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Kreek, M.J. Extreme Marginalization: Addiction and Other Mental Health Disorders, Stigma, and Imprisonment. Ann. N. Y. Acad. Sci. 2011, 1231, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Avery, J.; Knoepflmacher, D.; Mauer, E.; Kast, K.A.; Greiner, M.; Avery, J.; Penzner, J.B. Improvement in Residents’ Attitudes toward Individuals with Substance Use Disorders Following an Online Training Module on Stigma. HSS J. 2019, 15, 31–36. [Google Scholar] [CrossRef]
- Lindberg, M.; Vergara, C.; Wild-Wesley, R.; Gruman, C. Physicians-in-Training Attitudes toward Caring for and Working with Patients with Alcohol and Drug Abuse Diagnoses. South. Med. J. 2006, 99, 28–36. [Google Scholar] [CrossRef]
- Tsai, M.-C.; Chou, Y.-Y.; Lin, S.-J. Assessment of Experience and Training Needs in Adolescent Medicine: Perspectives from Pediatricians. Tzu Chi Med. J. 2011, 23, 37–41. [Google Scholar] [CrossRef]
- Hecimovich, M.D.; Volet, S.E. Importance of Building Confidence in Patient Communication and Clinical Skills among Chiropractic Students. J. Chiropr. Educ. 2009, 23, 151–164. [Google Scholar] [CrossRef]
| Variable(s) | Frequency | Percentage (%) |
|---|---|---|
| Background information | ||
| Gender | ||
| Male | 42 | 53.2 |
| Female | 37 | 46.8 |
| Age | ||
| <27 years | 33 | 41.8 |
| ≥27 years | 46 | 58.2 |
| Marital status | ||
| Single | 24 | 30.4 |
| Married | 55 | 69.6 |
| Level of residency | ||
| Junior | 37 | 46.8 |
| Senior | 42 | 53.2 |
| Smoking status | ||
| Yes | 12 | 15.2 |
| No | 67 | 84.4 |
| Completion of addiction rotation | ||
| Yes | 40 | 50.6 |
| No | 39 | 49.4 |
| Managed addiction cases (substance use) | ||
| ≥10 cases | 44 | 55.7 |
| <10 cases | 35 | 44.3 |
| Managed bipolar cases | ||
| ≥10 cases | 53 | 67.1 |
| <10 cases | 22 | 32.9 |
| Managed schizophrenia cases | ||
| ≥10 cases | 56 | 70.9 |
| <10 cases | 23 | 29.1 |
| How confident are you in managing the following cases? | ||
| Confident in managing addiction cases (substance use) | ||
| Not at all confident | 8 | 10.1 |
| Somewhat confident | 42 | 53.2 |
| Very confident | 29 | 36.7 |
| Confident in managing bipolar cases | ||
| Not at all confident | 5 | 6.3 |
| Somewhat confident | 32 | 40.5 |
| Very confident | 42 | 53.2 |
| Confident in managing schizophrenia cases | ||
| Not at all confident | 6 | 7.6 |
| Somewhat confident | 39 | 49.4 |
| Very confident | 34 | 43.0 |
| Variable(s) | Attitude Score toward Three Conditions | |||||
|---|---|---|---|---|---|---|
| Substance Use Disorder † | Bipolar Disorder † | Schizophrenia †† | ||||
| Mean (SD) | p Value | Mean (SD) | p Value | Mean (SD) | p Value | |
| Overall Attitude Score | 41.59 (8.09) | 54.53 (5.90) | 54.20 (6.60) | |||
| Gender | 0.256 | 0.070 | 0.961 | |||
| Male | 41.95 (7.50) | 53.40 (5.93) | 53.95 (7.16) | |||
| Female | 41.19 (8.79) | 55.81 (5.68) | 54.48 (5.99) | |||
| Age | 0.011 | 0.004 | 0.009 | |||
| <27 years | 37.21 (7.02) | 50.30 (6.40) | 49.15 (7.12) | |||
| ≥27 years | 42.12 (9.27) | 55.70 (5.59) | 56.96 (6.17) | |||
| Marital status | 0.462 | 0.297 | 0.564 | |||
| Single | 41.14 (8.08) | 54.09 (6.09) | 53.89 (7.05) | |||
| Married | 42.63 (8.17) | 55.54 (5.41) | 54.92 (5.53) | |||
| Level of residency | 0.015 | 0.005 | 0.021 | |||
| Junior | 39.90 (8.09) | 46.57 (6.25) | 49.88 (7.33) | |||
| Senior | 43.24 (8.17) | 54.49 (5.55) | 54.58 (5.75) | |||
| Smoking status | 0.212 | 0.349 | 0.816 | |||
| Yes | 38.91 (7.67) | 54.50 (4.95) | 55.08 (6.32) | |||
| No | 42.07 (8.12) | 54.54 (6.08) | 54.04 (6.69) | |||
| Completion of addiction rotation | 0.220 | 0.213 | 0.973 | |||
| Yes | 40.76 (8.71) | 54.55 (5.40) | 54.45 (5.99) | |||
| No | 42.44 (7.42) | 54.51 (6.44) | 53.95 (7.25) | |||
| Managed addiction (SUD) cases | 0.059 | 0.299 | 0.327 | |||
| ≥10 cases | 42.43 (7.33) | 55.15 (5.59) | 55.11 (6.28) | |||
| <10 cases | 40.93 (8.67) | 53.74 (6.25) | 53.05 (6.90) | |||
| Managed bipolar cases | 0.315 | 0.046 | 0.638 | |||
| ≥10 cases | 41.39 (8.38) | 56.01 (5.57) | 54.69 (6.20) | |||
| <10 cases | 42.00 (7.61) | 53.54 (6.52) | 53.19 (7.37) | |||
| Managed schizophrenia cases | 0.146 | 0.098 | 0.520 | |||
| ≥10 cases | 41.23 (8.60) | 55.30 (5.47) | 54.82 (5.88) | |||
| <10 cases | 42.48 (6.77) | 52.65 (6.59) | 52.69 (8.05) | |||
| Confident in managing addiction cases | <0.001 | NA | NA | |||
| Not at all confident | 27.37 (5.28) | |||||
| Somewhat confident | 38.93 (4.66) | |||||
| Very confident | 49.38 (3.49) | |||||
| Confident in managing bipolar cases | <0.001 | |||||
| Not at all confident | 46.40 (6.69) | |||||
| Somewhat confident | NA | 53.31 (5.08) | NA | |||
| Very confident | 56.43 (5.42) | |||||
| Confident in managing schizophrenia cases | <0.001 | |||||
| Not at all confident | 42.16 (5.63) | |||||
| Somewhat confident | NA | NA | 52.33 (5.29) | |||
| Very confident | 58.47 (4.09) | |||||
| Variable(s) | Attitude Score toward Three Conditions | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Regression Model 1: Substance Use Disorder | Regression Model 2: Bipolar Disorder | Regression Model 2: Schizophrenia | ||||||||||
| β | 95% CI | p | VIF | β | 95% CI | p | VIF | β | 95% CI | p | VIF | |
| Gender | 1.42 | 1.73 | 1.63 | |||||||||
| Male | Ref. | Ref. | Ref. | |||||||||
| Female | −1.62 | −5.78, 2.53 | 0.438 | 1.98 | −0.93, 4.91 | 0.179 | 0.58 | −2.78, 3.94 | 0.733 | |||
| Age | 1.59 | 1.44 | 1.71 | |||||||||
| <27 years | Ref. | Ref. | Ref. | |||||||||
| ≥27 years | 3.57 | 0.39, 6.75 | 0.018 | 2.74 | 0.78, 3.67 | 0.009 | 1.82 | 0.98, 4.45 | 0.039 | |||
| Marital status | 1.61 | 1.22 | 1.09 | |||||||||
| Single | Ref. | Ref. | Ref. | |||||||||
| Married | 1.69 | −2.78, 6.17 | 0.452 | 1.21 | −1.93, 4.36 | 0.443 | 0.43 | −3.19, 4.05 | 0.814 | |||
| Level of residency | 1.82 | 1.06 | 2.13 | |||||||||
| Junior | Ref. | Ref. | Ref. | |||||||||
| Senior | 1.71 | 0.94, 4.76 | 0.022 | 2.73 | 1.92, 6.20 | 0.008 | 1.64 | 0.90, 5.21 | 0.032 | |||
| Smoking status | 2.11 | 1.24 | 2.05 | |||||||||
| Yes | Ref. | Ref. | Ref. | |||||||||
| No | 2.83 | −2.90, 8.58 | 0.328 | −0.39 | −4.42, 3.64 | 0.847 | −0.39 | −5.03, 4.24 | 0.865 | |||
| Completion of addiction rotation | 2.93 | 3.13 | 3.21 | |||||||||
| Yes | Ref. | Ref. | Ref. | |||||||||
| No | 3.76 | −5.54, 13.06 | 0.422 | 3.19 | −3.33. 9.72 | 0.332 | 4.14 | −3.37, 11.66 | 0.275 | |||
| Managed addiction cases | 1.56 | 2.01 | 2.33 | |||||||||
| ≥10 cases | −0.48 | −6.77, 5.80 | 0.879 | 2.35 | −2.06, 6.76 | 0.291 | 3.38 | −1.69, 8.46 | 0.188 | |||
| <10 cases | Ref. | Ref. | Ref. | |||||||||
| Managed bipolar cases | 2.31 | 1.37 | 1.94 | |||||||||
| ≥10 cases | 1.13 | −6.90, 9.17 | 0.780 | 2.41 | −8.06, 3.22 | 0.195 | 1.13 | −5.64, 5.35 | 0.728 | |||
| <10 cases | Ref. | Ref. | Ref. | |||||||||
| Managed schizophrenia cases | 2.04 | 2.27 | 2.95 | |||||||||
| ≥10 cases | −0.49 | −9.31, 8.32 | 0.911 | 4.88 | −1.30, 9.06 | 0.120 | 2.39 | −4.73, 9.51 | 0.506 | |||
| <10 cases | Ref. | Ref. | Ref. | |||||||||
| Confident in managing addiction cases | 1.88 | NI | NI | |||||||||
| Not at all confident | Ref. | |||||||||||
| Somewhat confident | 3. 77 | 1.71, 7.11 | <0.001 | |||||||||
| Very confident | 4.90 | 2.11, 9.12 | <0.001 | |||||||||
| Confident in managing bipolar cases | 2.64 | |||||||||||
| Not at all confident | Ref. | |||||||||||
| Somewhat confident | NI | 5.00 | 1.11, 9.90 | 0.013 | NI | |||||||
| Very confident | 6.11 | 2.90, 11.7 | <0.001 | |||||||||
| Confident in managing schizophrenia cases | 2.46 | |||||||||||
| Not at all confident | Ref. | |||||||||||
| Somewhat confident | NI | NI | 4.62 | 1.23, 9.22 | <0.001 | |||||||
| Very confident | 5.10 | 3.77, 11.11 | <0.001 | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alarifi, A.M.; Alshahrani, N.Z.; Albali, N.H.; Aljalajel, K.M.; Alotaibi, N.M.; Fallatah, A.A.; Zeitounie, M.R.; Alghamdi, K.A.; Alsaaid, M.A.; Alshehri, A. Exploration of Psychiatry Residents’ Attitudes toward Patients with Substance Use Disorder, Bipolar Disorder and Schizophrenia in Saudi Arabia. Behav. Sci. 2023, 13, 642. https://doi.org/10.3390/bs13080642
Alarifi AM, Alshahrani NZ, Albali NH, Aljalajel KM, Alotaibi NM, Fallatah AA, Zeitounie MR, Alghamdi KA, Alsaaid MA, Alshehri A. Exploration of Psychiatry Residents’ Attitudes toward Patients with Substance Use Disorder, Bipolar Disorder and Schizophrenia in Saudi Arabia. Behavioral Sciences. 2023; 13(8):642. https://doi.org/10.3390/bs13080642
Chicago/Turabian StyleAlarifi, Abdullah M., Najim Z. Alshahrani, Nawaf H. Albali, Khalid M. Aljalajel, Nourh M. Alotaibi, Anan A. Fallatah, Majd Rachid Zeitounie, Khalid A. Alghamdi, Maan A. Alsaaid, and Ahmed Alshehri. 2023. "Exploration of Psychiatry Residents’ Attitudes toward Patients with Substance Use Disorder, Bipolar Disorder and Schizophrenia in Saudi Arabia" Behavioral Sciences 13, no. 8: 642. https://doi.org/10.3390/bs13080642
APA StyleAlarifi, A. M., Alshahrani, N. Z., Albali, N. H., Aljalajel, K. M., Alotaibi, N. M., Fallatah, A. A., Zeitounie, M. R., Alghamdi, K. A., Alsaaid, M. A., & Alshehri, A. (2023). Exploration of Psychiatry Residents’ Attitudes toward Patients with Substance Use Disorder, Bipolar Disorder and Schizophrenia in Saudi Arabia. Behavioral Sciences, 13(8), 642. https://doi.org/10.3390/bs13080642






