Use of Goal Attainment Scaling to Measure Educational and Rehabilitation Improvements in Children with Multiple Disabilities
Abstract
1. Introduction
2. Methods
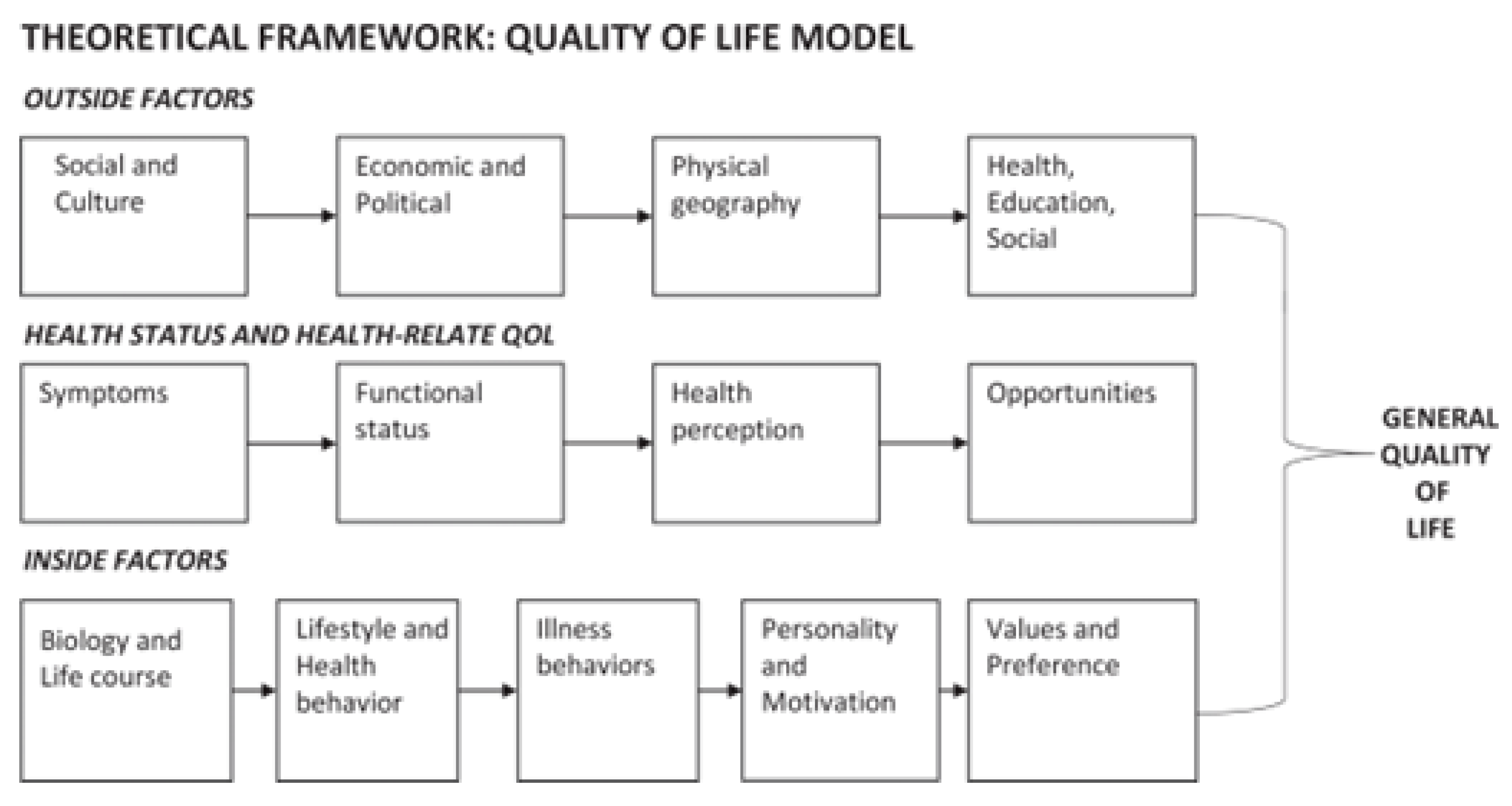
2.1. Protections for Human Participants
2.2. Project Site and Participants
3. Outcomes
4. Procedures
4.1. Step 1: Evidence-Based Assessment
4.1.1. Required Assessments: These Assessments Were Administered for All Enrolled Students
Developmental Assessment for Individuals with Severe Disabilities
Caregiver Priorities and Child Health Index of Life with Disabilities
Faces Pain Scale—Revised
Pediatric Evaluation of Disability Inventory
4.1.2. Commentary Assessments: These Assessments Were Completed When Appropriate for Individual Children
Cortical Visual Impairment Range Assessment
Matching Assistive Technology to Child-Augmentative Communication Evaluations Simplified Assessment
4.2. Step 2: Family Interview
4.3. Step 3: ICF and GAS Development
4.4. Step 4: Goal Measurement across the Year
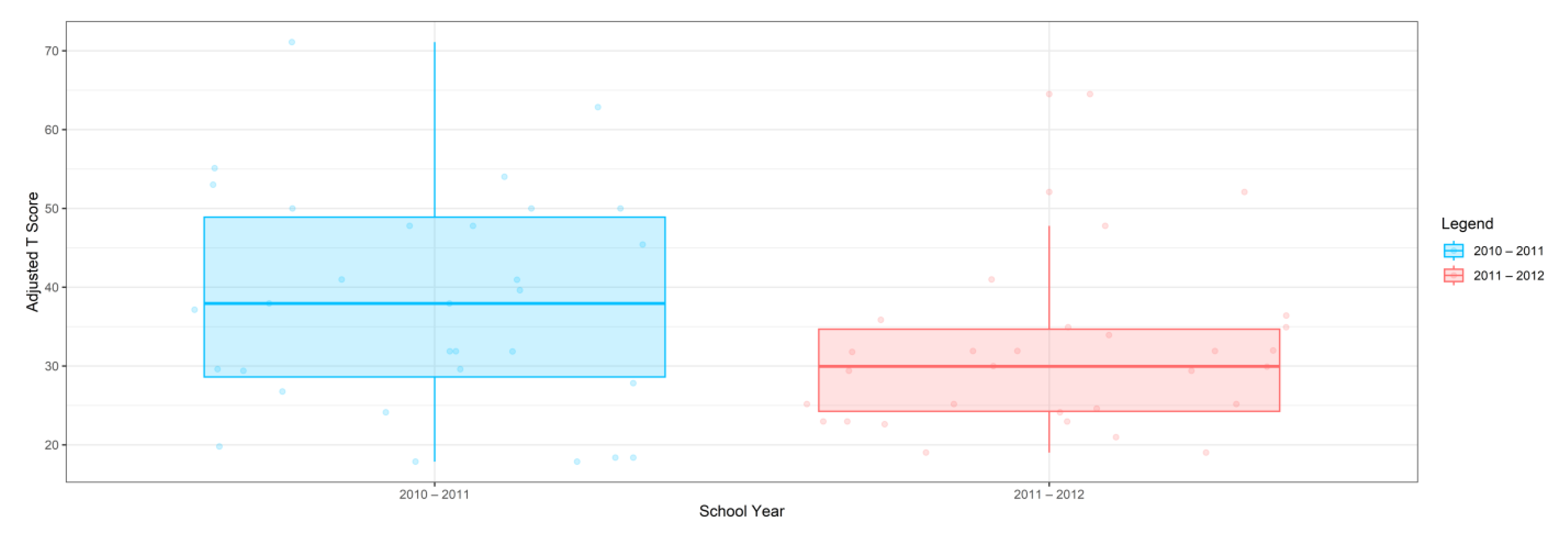
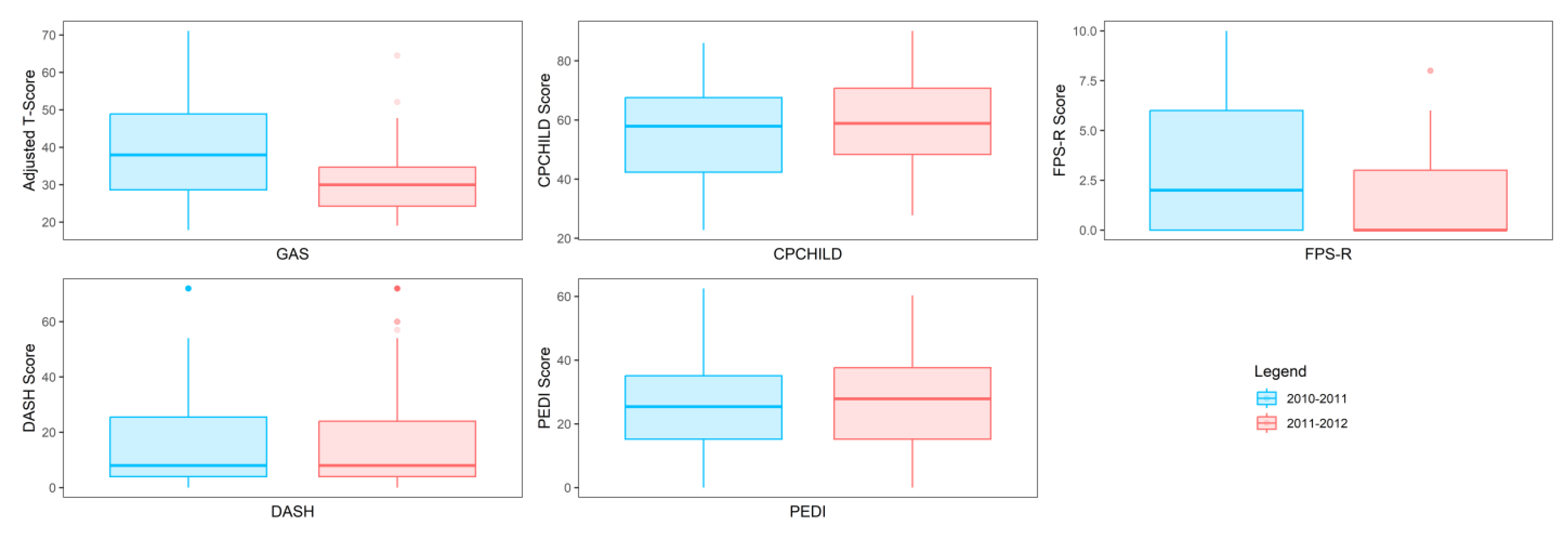
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. PACE Quality of Life Questionnaire
Appendix A.1.1. Internal Questions
- What is your child’s diagnosis(es) or disease?
- Do you know how your child’s diagnosis or disease affects your child’s future?
- Do you need information on your child’s diagnosis(es) or disease and its progression?
- What can your child do?
- Do you have any concerns about your child’s overall health?
- Generally, what does your child do each weekday? Weekend?
- How would you describe your child’s personality?
- What makes your child happy? Sad? Mad? Sick?
- What does your child enjoy?
- Does your child have any bad behaviors? If so, what?
- What good behaviors does your child have?
Appendix A.1.2. Health Status and Health-Related Quality of Life Questions
- How does your child sleep at night?
- What position does your child sleep in?
- Does your child experience pain? If so, how often? Can you explain what causes your child’s pain?
- Are your child’s arms and legs tight or loose?
- Is your child’s head and trunk tight or loose?
- Does your child have seizures? If so, how do you control them? How often do they occur?
- Is your child’s weight good?
- Does your child move freely and well?
- Does your child like to move?
- Does your child see well?
- Does your child hear well?
- Does your child like to be touched?
- Does your child like to touch things?
- Does your child like to sit?
- Does your child like to stand?
- What calms your child?
- Does your child cough a lot?
- Does your child vomit a lot?
- What activities does your child participate in daily? Weekly?
- Does your child participate in any community activities? (e.g., little league, miracle league, horseback riding, adaptive swimming)
- How does your child bathe? How often does your child bathe?
- Who fixes your child’s hair?
- Does your child use diapers? Toilet?
- How does your child get dressed each day?
- How does your child eat? Do they enjoy eating? Do you think they get enough calories?
- Can your child change position in the bed?
- How does your child get to school?
- How does your child move about in your home?
- How does your child move about at the grocery store, doctor’s office, or other community locations?
- How is your child’s overall health?
- How would you rate your child’s quality of life?
- What do you dream of your child doing now?
- What do you dream of your child doing in the future?
- What activities would you like to have your child experience or participate in?
Appendix A.1.3. External Questions
- Do you want us to know anything about you and your child’s culture? Religion? Income? Politics?
- Is there anything in the environment that bothers you or your child? (e.g., Heat? Pools? Horses? Animals?)
- Is there anything we can do to help with your job? Income? Education?
- What medications does your child take?
- What doctors does your child see?
- What therapies does your child have?
- Do you like your child’s school? What are the pluses of your child’s school? What are the minuses of your child’s school?
- What do you and your family like to do? What else would you like to do?
- How do you transport your child to appointments?
- Would any changes to your home make it easier to care for them?
- Do you need any equipment to improve your ability to care for your family and child?
- How is the health of your family members?
- How would you rate your family member’s quality of life?
Appendix A.1.4. Reference
Appendix B
International Classification of Functioning, Disability, and Health
- Name: VH
- Age: 15 years
- Body weight: 118 pounds
- Height: 144 inches
- Head circumference: 22.44 inches
- Primary Nutritional Method: Gastronomy tube
- Blood pressure: 118/82
- Heart rate: 108
- Respiratory rate: 25 breaths per minute
- Temperature: 98.6 degrees
- Seizure History and Frequency: Yes, and with medication, occurrence of one time annually.
- Developmental History: VH was born full-term to married parents, but care was transferred to paternal grandmother by age of 12 months, who was a licensed practical nurse. VH demonstrated hypotonia at birth and was later diagnosed with mitochondrial myopathy. Seizures were also present within the first year of life.
- General development level: 3–4 months
- Surgeries: Gastronomy tube placement, right femoral head osteotomy, spinal fusion for neuromuscular scoliosis (2009), two femoral fractures without surgical intervention, semi-annual botox to right hamstring and bilateral wrist flexors.
- Strengths
- Excellent temperament
- Supportive paternal grandmother support with assistance from father
- Successful access in right hand with button switch
- Improving visual skills, such as seeing more color, greater visual distance
- Loves music and interactions with family and friends
- Receptive greater than expressive language
- Sense of humor
- Healthy body growth
- Tolerates frequent positional changes necessary for skeletal alignment, pain management, nutritional needs, pressure relief, and skin integrity
- Body structure and function impairments:
- Nervous system
- Cognition
- Cortical visual impairment
- Marked hypotonia (head and trunk)
- Hypertonia (upper extremities’ (UEs) and lower extremities’ (LEs) flexors)
- Clonus with quick stretch of bilateral plantar flexors
- Selective neuromotor control
- Motor planning and learning
- Pain
- Musculoskeletal system
- Marked weakness of oral, head, trunk, UEs’, and LEs’ musculature
- Initiating and sustaining movement of mouth, head, trunk, UEs, and LEs
- Alignment of UEs, head and trunk, and LEs with postures of flexion of head, shoulder retraction and external rotation, elbow flexion, wrist and finger flexion, hip flexion, abduction, external rotation, knee flexion, and plantar flexion
- Hypermobility of head and trunk
- Hypomobility of UEs and LEs
- Coordination of oral, head, trunk, UEs’, and LEs’ musculature
- Osteopenia
- Circulatory system
- Cardiovascular endurance
- Distal circulatory perfusion with cool distal extremities
- Pulmonary system
- Abdominal breathing
- Flared posture of rib cage
- Weakened cough strength
- Sleep apnea
- Gastrointestinal system
- Aspiration risk
- Swallowing dysfunction
- Sialorrhea/Drooling
- Integumentary
- Potential for skin breakdown
- Spinal and hip scars
- Sensory systems
- Vision—cortical visual impairment; latency; see red, yellow, and green primarily; can attend with low levels of background noise; light, reflective qualities, and movements assist with vision; dark background beneficial
- Auditory—intact
- Tactile and proprioception—limited experiences, tolerates input
- Vestibular—limited experiences, tolerates input
- Activity Limitations
- Typical learning methods
- Receptive language/communication
- Expressive language/communication
- Swallowing
- Seeing and interpreting complex visual information
- Eating with mouth to meet nutritional needs
- Dependent for bed mobility or positional changes
- Unsupported sitting
- Unsupported standing
- Dependent for mobility
- Dependent for transitions/transfers
- Dependent for dressing
- Dependent for bathing
- Incontinent
- Reaching
- Grasping
- Normal sleeping durations and habits
- Physical activity
- Participation Restrictions
- Successful learning of academic and life skills material in a regular education classroom
- Fitness and extracurricular programming in typical school and community environments
- Participation desires of parents/caregivers
- Aquatic Therapy
- Attend church
- Go on vacation to Atlanta to visit family
- Family picnic
- Participation barriers
- Managing caregiver demands
- Managing health care appointments
- Public transportation for wheelchair
- Wheelchair accessibility in community environments
- Knowledgeable human assistance and assistive technology required to accommodate for impairments, activity limitations, and promotion for active participation
- Life expectations and opportunities set too low by others
- Liability concerns of community organizations
- Funding
- Environmental Enhancers
- Grandmother is a licensed practical nurse so the level of care at home is excellent
- BiPAP at night
- Ankle foot orthoses
- Hospital bed in home
- Hoyer lift in home
- Ramp into home
- Roll-in shower
- Certified nursing assistant in home to assist grandmother with activities of daily living
- Stander at school
- Power mobility at school for brief and safe environmental exploration
- Switch assistive technology (simple and brief episodes of communication at school)
- Environmental Barriers
- No family-owned wheelchair transportation so dependent on Medicaid transportation
- Lower socioeconomics
Appendix C
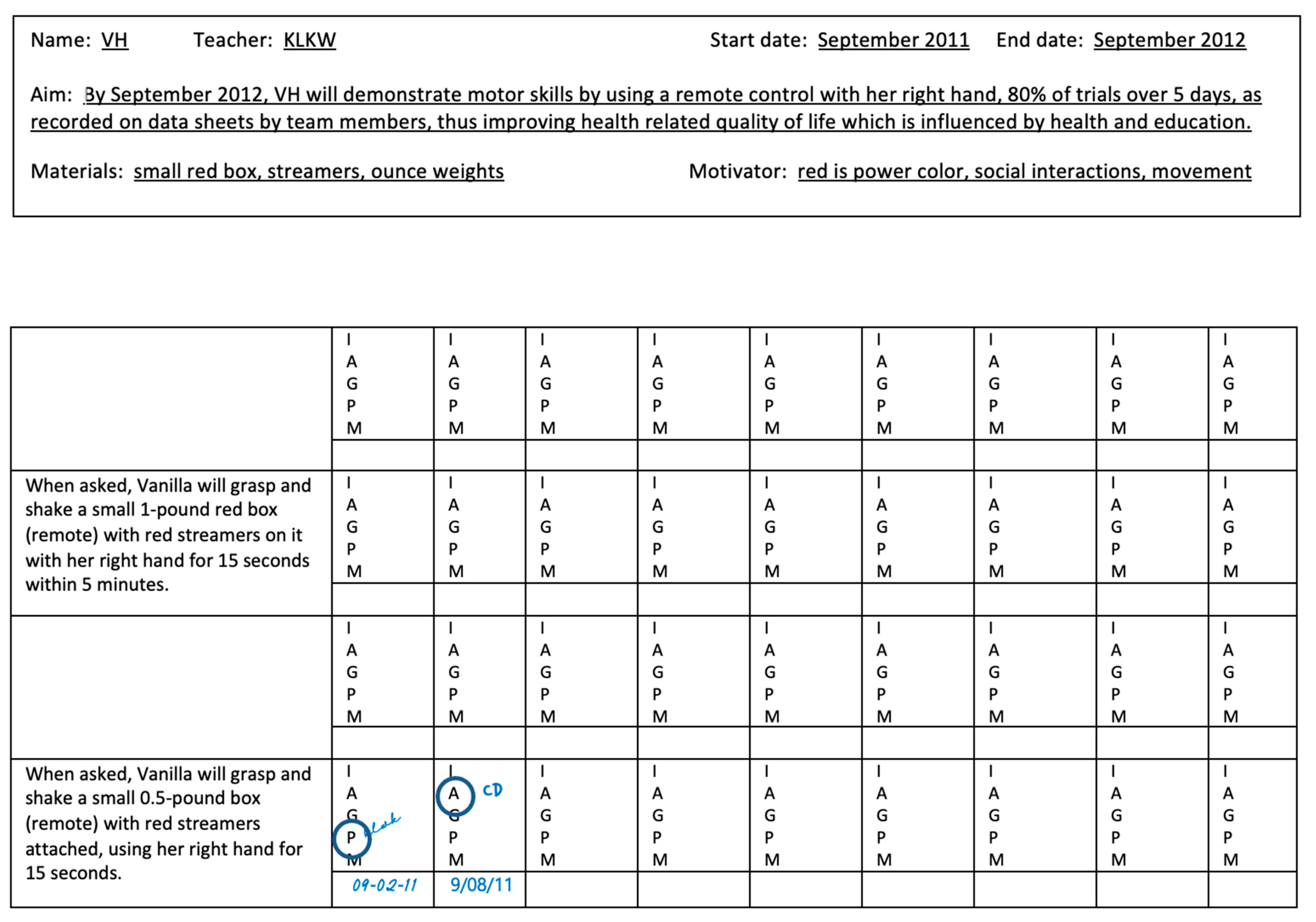
Goal Attainment Scaling Examples for a Child with Multiple Disabilities
| Scale 1—Gross Motor | Scale 2—Feeding | Scale 3—Self-Care | Scale 4—Language with Assistive Technology | |
|---|---|---|---|---|
| Level of Attainment | By September 2012, V will increase her gross motor skills by standing in a vibrating supine stander with bilateral AFOs and immobilizers, 80% of trials over 5 days, as recorded on data sheets by faculty and staff, thus improving health related quality of life which is influenced by health and education. | By September 2012, V will demonstrate oral motor skills by tasting different foods with no facial grimacing, 80% of trials as recorded on data sheets by faculty and staff, thus improving health related quality of life which is influenced by health and education. | By September 2012, V will demonstrate daily living skills by wiping her mouth with a red washcloth, 80% of trials over 5 days, as recorded on data sheets by faculty and staff, thus improving health related quality of life which is influenced by health and education. | By September 2012, V will use a button switch in her right hand (with hands splints on) to socialize with others, 80% of trials over 5 days as recorded on data sheets by faculty and staff, thus improving health related quality of life which is influenced by health and education. |
| V will stand in a vibrating supine stander angled at 70 degrees with bilateral AFOs and immobilizers for 20 min while participating in classroom instruction and interacting with classmates. | During school breakfast and/or lunch time and to enhance oral motor experiences, V will taste 1 different food with no facial grimacing. | When asked and with red washcloth placed in her hand, V will wipe saliva from her mouth within 5 min to promote oral hygiene and social acceptance. | V will use her spec switch in her right hand (with hands splints on) to socialize with others one time throughout the school day. | |
| Much Less | ||||
| −2 | ||||
| than expected | ||||
| V will stand in a vibrating supine stander angled at 70 degrees with bilateral AFOs and immobilizers for 30 min while participating in classroom instruction and interacting with classmates. | During school breakfast and/or lunch time and to enhance oral motor experiences, V will taste 2 different foods with no facial grimacing. | When asked and with red washcloth placed in her hand, V will wipe saliva from her mouth within 4 min to promote oral hygiene and social acceptance. | V will use her spec switch in her right hand (with hands splints on) to socialize with others two times throughout the school day. | |
| Somewhat less | ||||
| −1 | ||||
| than expected | ||||
| V will stand in a vibrating supine stander angled at 70 degrees with bilateral AFOs and immobilizers for 40 min while participating in classroom instruction and interacting with classmates. | During school breakfast and/or lunch time and to enhance oral motor experiences, V will taste 3 different foods with no facial grimacing. | When asked and with red washcloth placed in her hand, V will wipe saliva from her mouth within 3 min to promote oral hygiene and social acceptance. | V will use her spec switch in her right hand (with hands splints on) to socialize with others three times throughout the school day. | |
| Expected level | ||||
| 0 | ||||
| of outcome | ||||
| V will stand in a vibrating supine stander angled at 70 degrees with bilateral AFOs and immobilizers for 50 min while participating in classroom instruction and interacting with classmates. | During school breakfast and/or lunch time and to enhance oral motor experiences, V will taste 4 different foods with no facial grimacing. | When asked and with red washcloth placed in her hand, V will wipe saliva from her mouth within 2 min to promote oral hygiene and social acceptance. | V will use her spec switch in her right hand (with hands splints on) to socialize with others four times throughout the school day. | |
| Somewhat more | ||||
| +1 | ||||
| than expected | ||||
| V will stand in a vibrating supine stander angled at 70 degrees with bilateral AFOs and immobilizers for 60 min while participating in classroom instruction and interacting with classmates. | During school breakfast and/or lunch time and to enhance oral motor experiences, V will taste 5 different foods with no facial grimacing. | When asked and with red washcloth placed in her hand, V will wipe saliva from her mouth within 1 min to promote oral hygiene and social acceptance. | V will use her spec switch in her right hand (with hands splints on) to socialize with others five times throughout the school day. | |
| Much more | ||||
| +2 | ||||
| than expected | ||||
Appendix D
Goal Attainment Scaling Data Collection Sheet modified from Murdoch Center Data Sheet
References
- United Nations Children’s Fund. Promoting the Rights of Children with Disabilities; United Nations Children’s Fund: Florence, Italy, 2007. [Google Scholar]
- National Center for Education Statistics. Students with Disabilities. 2022. Available online: https://nces.ed.gov/programs/coe/indicator/cgg (accessed on 21 February 2023).
- US Department of Education. Individuals with Disabilities Education Act; US Department of Education: Washington, DC, USA, 2018.
- Cohen, E.; Kuo, D.Z.; Agrawal, R.; Berry, J.G.; Bhagat, S.K.; Simon, T.D.; Srivastava, R. Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics 2011, 127, 529–538. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Classification of Functioning, Disability and Health. 2001. Available online: http://www.who.int/classifications/icf/en/ (accessed on 12 March 2002).
- Glader, L.; Plews-Ogan, J.; Agrawal, R. Children with medical complexity: Creating a framework for care based on the International Classification of Functioning, Disability and Health. Dev. Med. Child Neurol. 2016, 58, 1116–1123. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C.; van Dijk, J.; McDonnell, A.P.; Thompson, K. The framework for understanding young children with severe disabilities: The van Dijk Approach to Assessment. Res. Pract. Pers. Sev. Disabil. 2002, 27, 97–111. [Google Scholar] [CrossRef]
- Wolf-Schein, E.G. Considerations in Assessment of Children with Severe Disabilities including Deaf-Blindness and Autism. Int. J. Disabil. Dev. Educ. 1998, 45, 35–55. [Google Scholar] [CrossRef]
- Berry, J.G.; Hall, M.; Cohen, E.; O’Neill, M.; Feudtner, C. Ways to Identify Children with Medical Complexity and the Importance of Why. J. Pediatr. 2015, 167, 229–237. [Google Scholar] [CrossRef]
- Sarathy, K.; Doshi, C.; Aroojis, A. Clinical Examination of Children with Cerebral Palsy. Indian J. Orthop. 2019, 53, 35–44. [Google Scholar] [CrossRef]
- Kiresuk, T.J.; Smith, A.; Cardillo, J.E. Goal Attainment Scaling: Applications, Theory, and Measurement; Lawrence Erlbaum Associates: New York, NY, USA, 1994. [Google Scholar]
- Mailloux, Z.; May-Benson, T.A.; Summers, C.A.; Miller, L.J.; Brett-Green, B.; Burke, J.P.; Cohn, E.S.; Koomar, J.A.; Parham, L.D.; Roley, S.S.; et al. Goal attainment scaling as a measure of meaningful outcomes for children with sensory integration disorders. Am. J. Occup. Ther. 2007, 61, 254–259. [Google Scholar] [CrossRef]
- Chiarello, L.A.; Effgen, S.K.; Jeffries, L.; McCoy, S.W.; Bush, H. Student Outcomes of School-Based Physical Therapy as Measured by Goal Attainment Scaling. Pediatr. Phys. Ther. 2016, 28, 277–284. [Google Scholar] [CrossRef]
- Steenbeek, D.; Gorter, J.W.; Ketelaar, M.; Galama, K.; Lindeman, E. Responsiveness of Goal Attainment Scaling in comparison to two standardized measures in outcome evaluation of children with cerebral palsy. Clin. Rehabil. 2011, 25, 1128–1139. [Google Scholar] [CrossRef]
- Haladay, D.; Swisher, L.; Hardwick, D. Goal attainment scaling for patients with low back pain in rehabilitation: A systematic review. Health Sci. Rep. 2021, 4, e378. [Google Scholar] [CrossRef]
- Hoorntje, A.; Waterval-Witjes, S.; Koenraadt, K.L.; Kuijer, P.P.F.; Blankevoort, L.; Kerkhoffs, G.M.; van Geenen, R.C. Goal Attainment Scaling Rehabilitation Improves Satisfaction with Work Activities for Younger Working Patients After Knee Arthroplasty: Results from the Randomized Controlled ACTION Trial. J. Bone Jt. Surg. Am. Vol. 2020, 102, 1445–1453. [Google Scholar] [CrossRef] [PubMed]
- Harpster, K.; Sheehan, A.; Foster, E.A.; Leffler, E.; Schwab, S.M.; Angeli, J.M. The methodological application of goal attainment scaling in pediatric rehabilitation research: A systematic review. Disabil. Rehabil. 2019, 41, 2855–2864. [Google Scholar] [CrossRef] [PubMed]
- Dodds, C.B.; Bjornson, K.F.; Sweeney, J.K.; Narayanan, U. The effects of supported physical activity on parental-reported health-related quality of life in children with medical complexity. J. Pediatr. Rehabil. Med. 2015, 8, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Doran, G.T. There’s a SMART way to write management’s goals and objectives. Manag. Rev. 1981, 70, 35–36. [Google Scholar]
- Krasny-Pacini, A.; Pauly, F.; Hiebel, J.; Godon, S.; Isner-Horobeti, M.E.; Chevignard, M. Feasibility of a shorter Goal Attainment Scaling method for a pediatric spasticity clinic—The 3-milestones GAS. Ann. Phys. Rehabil. Med. 2017, 60, 249–257. [Google Scholar] [CrossRef] [PubMed]
- King, G.A.; McDougall, J.; Palisano, R.J.; Gritzan, J.; Tucker, M.A. Goal attainment scaling: Its use in evaluating pediatric therapy programs. Phys. Occup. Ther. Pediatr. 1999, 19, 31–52. [Google Scholar] [CrossRef]
- Gaffney, E.; Gaffney, K.; Bartleson, L.; Dodds, C. Goal Attainment Scaling Made Easy With an App: GOALed. Pediatr. Phys. Ther. 2019, 31, 225–230. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research Applications to Practice, 2nd ed.; Prentice Hall Heallth, Inc.: Upper Saddle River, NJ, USA, 2000. [Google Scholar]
- Dykes, M.K.; Erin, J.N. Developmental Assessment for Individuals with Severe Disabilities; Pro-Ed: Austin, TX, USA, 1999. [Google Scholar]
- Narayanan, U.G.; Fehlings, D.; Weir, S.; Knights, S.; Kiran, S.; Campbell, K. Initial development and validation of the Caregiver Priorities and Child Health Index of Life with Disabilities (CPCHILD). Dev. Med. Child Neurol. 2006, 48, 804–812. [Google Scholar] [CrossRef]
- Dodds, C.B.; Bjornson, K.F.; Sweeney, J.K.; Narayanan, U.G. The effect of supported physical activity on parental-reported sleep qualities and pain severity in children with medical complexity. J. Pediatr. Rehabil. Med. 2016, 9, 195–206. [Google Scholar] [CrossRef]
- Daly, C.; Moore, C.L.; Johannes, S.; Middleton, J.; Kenyon, L.K. Pilot Evaluation of a School-Based Programme Focused on Activity, Fitness, and Function among Children with Cerebral Palsy at GMFCS Level IV: Single-Subject Research Design. Physiother. Can. 2020, 72, 195–204. [Google Scholar] [CrossRef]
- Bieri, D.; Reeve, R.A.; Champion, G.D.; Addicoat, L.; Ziegler, J.B. The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: Development, initial validation, and preliminary investigation for ratio scale properties. Pain 1990, 41, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.; Belew, J.L. Qualitative evaluation of a pain intensity screen for children with severe neurodevelopmental disabilities. Pain Manag. Nurs. 2013, 14, e115–e123. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, D.; von Baeyer, C.L.; Stinson, J.N.; Sung, L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics 2010, 126, e1168–e1198. [Google Scholar] [CrossRef] [PubMed]
- Haley, S.; Coster, W.J.; Ludow, L.; LHaltiwanger, J. Pediatric Evaluation of Disability Inventory; Boston University: Boston, MA, USA, 1992. [Google Scholar]
- Berg, M.; Jahnsen, R.; Froslie, K.F.; Hussain, A. Reliability of the Pediatric Evaluation of Disability Inventory (PEDI). Phys. Occup. Ther. Pediatr. 2004, 24, 61–77. [Google Scholar] [CrossRef]
- Shore, B.J.; Allar, B.G.; Miller, P.E.; Matheney, T.H.; Snyder, B.D.; Fragala-Pinkham, M. Measuring the Reliability and Construct Validity of the Pediatric Evaluation of Disability Inventory-Computer Adaptive Test (PEDI-CAT) in Children with Cerebral Palsy. Arch. Phys. Med. Rehabil. 2019, 100, 45–51. [Google Scholar] [CrossRef]
- Roman-Lantzy, C. Cortical Visual Impairment; American Foundation for the Blind Press: New York, NY, USA, 2007. [Google Scholar]
- McConnell, E.L.; Saunders, K.J.; Little, J.A. What assessments are currently used to investigate and diagnose cerebral visual impairment (CVI) in children? A systematic review. Ophthalmic Physiol. Opt. 2021, 41, 224–244. [Google Scholar] [CrossRef]
- Roman-Lantzy, C. Cortical Visual Impairment: An Approach to Assessment and Intervention, 2nd ed.; American Foundation for the Blind Press: New York, NY, USA, 2018. [Google Scholar]
- Zapf, S.A.; Scherer, M.J.; Baxter, M.F.; D, H.R. Validating a measure to assess factors that affect assistive technology use by students with disabilities in elementary and secondary education. Disabil. Rehabil. Assist. Technol. 2016, 11, 38–49. [Google Scholar]
- Patrick, D.L.; Chiang, Y.P. Measurement of health outcomes in treatment effectiveness evaluations: Conceptual and methodological challenges. Med. Care 2000, 38 (Suppl. S9), II14–II25. [Google Scholar] [CrossRef]
- Dodds, C.; Rempel, G. A quality of life model promotes enablement for children with medical complexity. J. Pediatr. Rehabil. Med. 2016, 9, 253–255. [Google Scholar] [CrossRef]
- Autism Classroom Resources. The Murdoch Program Library A Library of Task Analyses Data Sheet. Available online: https://autismclassroomresources.com/murdoch-program-library-a-tool-for-teaching-life-skills/ (accessed on 17 January 2022).
- Harty, M.; Griesel, M.; van der Merwe, A. The ICF as a common language for rehabilitation goal-setting: Comparing client and professional priorities. Health Qual Life Outcomes 2011, 9, 87. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Namara, M.M.; Paton, M.C.B.; Popat, H.; et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [PubMed]
- Pritchard-Wiart, L.; Thompson-Hodgetts, S.; McKillop, A.B.; Rosychuk, R.; Mrklas, K.; Zwaigenbaum, L.; Zwicker, J.; Andersen, J.; King, G.; Firouzeh, P. A multi-center, pragmatic, effectiveness-implementation (hybrid I) cluster randomized controlled trial to evaluate a child-oriented goal-setting approach in paediatric rehabilitation (the ENGAGE approach): A study protocol. BMC Pediatr. 2022, 22, 375. [Google Scholar] [CrossRef]
- Christensen, R.; MacIntosh, A.; Switzer, L.; Fehlings, D. Change in pain status in children with cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 374–379. [Google Scholar] [CrossRef] [PubMed]
| Demographic and Characteristics | # of Children 1 |
|---|---|
| DIAGNOSIS | |
| Cerebral palsy | 17 |
| Genetic health conditions | 11 |
| Traumatic brain injury | 3 |
| CO-OCCURRING CONDITIONS | |
| Seizures | 19 |
| Cortical visual impairment | 15 |
| Tracheostomy | 1 |
| GENDER | |
| Male | 15 |
| Female | 16 |
| RACE and ETHNICITY | |
| Black/African American | 13 |
| White | 17 |
| Other | 1 |
| Not Hispanic/Latino | 31 |
| MOBILITY FUNCTION | |
| Wheelchair users propelled by caregiver | 29 |
| Wheelchair user self-propel | 2 |
| FEEDING FUNCTION | |
| Gastronomy or Jejunostomy tube | 13 |
| Gastronomy Tube/Oral | 4 |
| Oral | 14 |
| SELFCARE FUNCTION | |
| Maximum assistance | 30 |
| Moderate assistance | 1 |
| EXPRESSIVE and RECEPTIVE FUNCTION | |
| Maximum assistance | 29 |
| Moderate assistance | 2 |
| 2010–2011 Number of Goals | Scaled Score | T–Score | Classroom T–Score | School T–Score | 2011–2012 Number of Goals | Scaled Score | T–Score | Classroom T–Score | School T–Score | Bell Curve of Adjusted Scores Based on Number of Goals | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 35.74 | 29.45 | ||||||||||
| CLASSROOM 1 | 50.396 | 32.65 | |||||||||
| 1 | 6 | 0.83 | 62.91 | 5 | −1.2 | 31.91 | 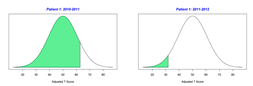 | ||||
| 2 | 6 | 0.33 | 44.84 | 5 | −1.2 | 31.91 | 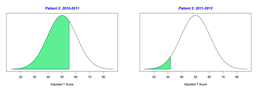 | ||||
| 3 | 5 | 0.2 | 53.02 | 7 | −0.86 | 36.45 | 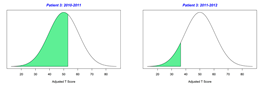 | ||||
| 4 | 7 | −2 | 18.28 | 5 | −1.2 | 31.91 | 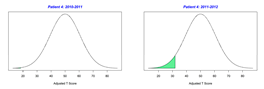 | ||||
| 5 | 0 | 50 | 7 | −1.14 | 31.93 |  | |||||
| 6 | 7 | −0.14 | 47.74 | 7 | −0.14 | 47.74 | 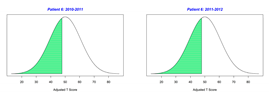 | ||||
| 7 | 0 | 50 | 8 | −0.88 | 35.94 |  | |||||
| CLASSROOM 2 | 27.356 | 22.95 | |||||||||
| 8 | 7 | −1.29 | 29.67 | 8 | −0.88 | 35.94 | 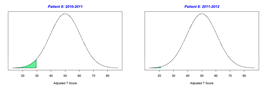 | ||||
| 9 | 6 | −0.67 | 39.67 | 7 | −1.71 | 22.89 | 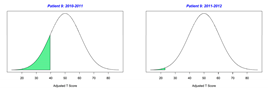 | ||||
| 10 | 8 | −2 | 17.87 | 5 | −1 | 34.92 | 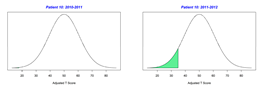 | ||||
| 11 | 6 | −1.17 | 31.93 | 7 | −1.71 | 22.89 | 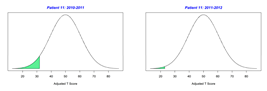 | ||||
| 12 | 8 | −1.38 | 30.12 | 7 | −1.57 | 25.15 | 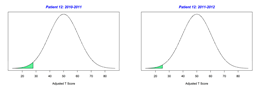 | ||||
| 13 | 7 | −1.29 | 29.67 | 8 | −1.25 | 29.92 |  | ||||
| CLASSROOM 3 | 30.413 | 20.15 | |||||||||
| 14 | 5 | −0.8 | 37.94 | 6 | −2 | 19.02 | 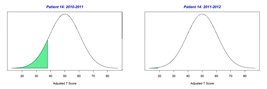 | ||||
| 15 | 6 | −1.67 | 24.18 | 7 | −1.57 | 25.15 | 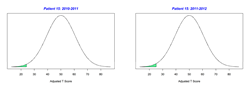 | ||||
| 16 | 5 | −0.6 | 40.95 | 6 | −1.67 | 24.18 | 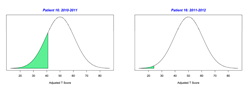 | ||||
| 17 | 7 | −2 | 18.38 | 6 | −2 | 19.02 |  | ||||
| 18 | 7 | −0.29 | 45.48 | 6 | −1.33 | 29.34 | 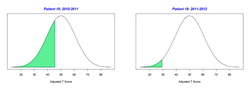 | ||||
| 19 | 8 | −1.13 | 31.93 | 7 | −1.57 | 25.15 | 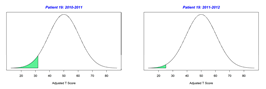 | ||||
| CLASSROOM 4 | 45.058 | 33.12 | |||||||||
| 20 | 7 | −0.57 | 40.96 | 7 | −1.71 | 22.89 | 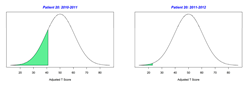 | ||||
| 21 | 6 | −1.33 | 29.34 | 6 | −1.33 | 29.34 |  | ||||
| 22 | 8 | 0.25 | 54.02 | 5 | −1 | 34.92 | 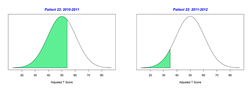 | ||||
| 23 | 5 | 1.4 | 71.11 | 4 | 1 | 64.51 |  | ||||
| 24 | 0 | 50 | −2 | 30 |  | ||||||
| 25 | 8 | −0.75 | 37.95 | 8 | 0.13 | 52.01 | 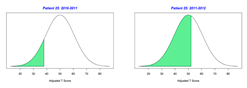 | ||||
| CLASSROOM 5 | 27.513 | 40.14 | |||||||||
| 26 | 6 | −1.5 | 26.76 | 3 | −1.33 | 31.74 | 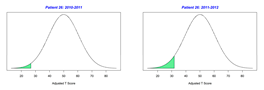 | ||||
| 27 | 8 | −2 | 17.87 | 8 | −1 | 33.94 | 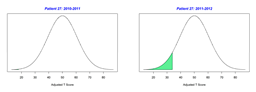 | ||||
| 28 | 6 | −1.17 | 31.93 | 7 | −0.57 | 40.96 | 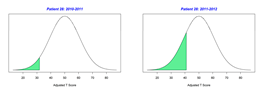 | ||||
| 29 | 7 | −0.14 | 47.74 | 3 | −2 | 22.62 | 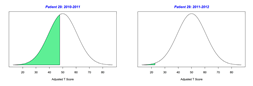 | ||||
| 30 | 8 | −1.88 | 19.88 | 4 | −1.75 | 24.61 | 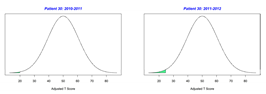 | ||||
| 31 | 6 | −0.83 | 37.09 | 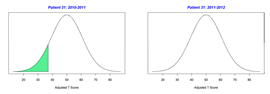 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kascak, K.; Keller, E.; Dodds, C. Use of Goal Attainment Scaling to Measure Educational and Rehabilitation Improvements in Children with Multiple Disabilities. Behav. Sci. 2023, 13, 625. https://doi.org/10.3390/bs13080625
Kascak K, Keller E, Dodds C. Use of Goal Attainment Scaling to Measure Educational and Rehabilitation Improvements in Children with Multiple Disabilities. Behavioral Sciences. 2023; 13(8):625. https://doi.org/10.3390/bs13080625
Chicago/Turabian StyleKascak, Kimberly, Everette Keller, and Cindy Dodds. 2023. "Use of Goal Attainment Scaling to Measure Educational and Rehabilitation Improvements in Children with Multiple Disabilities" Behavioral Sciences 13, no. 8: 625. https://doi.org/10.3390/bs13080625
APA StyleKascak, K., Keller, E., & Dodds, C. (2023). Use of Goal Attainment Scaling to Measure Educational and Rehabilitation Improvements in Children with Multiple Disabilities. Behavioral Sciences, 13(8), 625. https://doi.org/10.3390/bs13080625





