Lifelong Fitness in Ambulatory Children and Adolescents with Cerebral Palsy II: Influencing the Trajectory
Abstract
1. Introduction
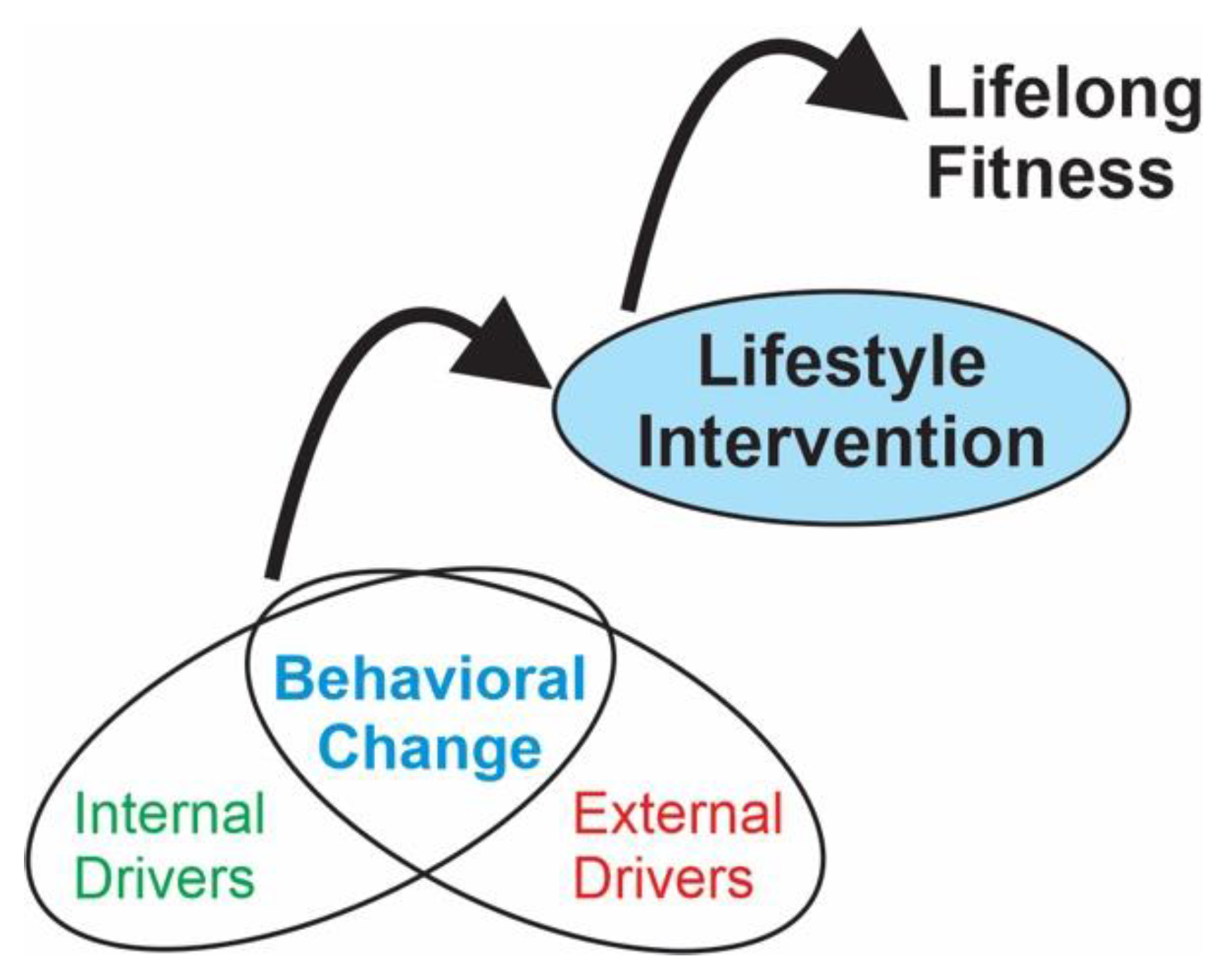
2. Physical Activity and Fitness
3. Altering the Fitness Trajectory of Children with CP
3.1. Internal Drivers of Behavioral Change
3.2. External Drivers of Behavioral Change
3.2.1. Opportunity
3.2.2. Relationships
4. Engaged Consumers
5. Lifestyle Intervention
6. Lifelong Sustainability
Case Example
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Fitness Program Incentive Questions—Program Ideas
- Child name (first):____________________________ Age: _____________
- 1.
- What is your favorite thing to do outside of school?
- 2.
- Do you to do things that make you move around and/or breath hard? (Select One)
- 3.
- What physical activity (sport, dance, martial art, playing outside) do you participate in most outside of school? Why do you like it?
- 4.
- Where do you participate in this activity or exercise? At home, school, or somewhere else?
- 5.
- If you participate outside your home or school, how do you get there?
- 6.
- Was it your idea to start doing this activity or exercise? (Select one)
- Display: Was it your idea to start doing this activity or exercise? (Select one) = Yes or No
- 7.
- If not, who suggested it?
- 8.
- What do you need to get better at this activity or exercise? Select all that apply.
- 9.
- Do you believe working out will help you get better now or in the future? (Select one)
- 10.
- Rank the following physical activities in terms of your interests. Drag to rank each item in order 1 (best)–5 (worst):
- 11.
- How important is it to you to be fit or have an active lifestyle (pick one)?
- 12.
- What would you be most excited about if you were able to do a fitness program?
- 13.
- Does anything about a fitness program worry you?
- 14.
- Do you think having the right type of gear (clothes, water bottles, sneakers, etc.) is important to participate in a fitness program?
- 15.
- Are you willing to do activities that are less fun if they help you get better at sports or activities you like to participate in? (Select one)
- 16.
- Rank order the list of rewards below by what you would prefer, Rank in order of 1 (best)–7 (worst):
- 17.
- What would motivate you to get more fit? Rank in order of 1 (best motivator)–6 (worst):
- 18.
- How often do you think children should exercise to improve their bone and muscle health?
- (Select one)
- 19.
- How many times per week would you be willing or able to go somewhere outside your home to improve your fitness? Consider other things you do, such as homework or music lessons.
- 20.
- Would you be willing to participate in a fitness program for 3 months or more? (Select one)
- 21.
- What would be the biggest challenge for you to participate for 3 months or more?
- 22.
- Other comments:
- End of Block: Part 1: Child
- Start of Block: Part 2: Caretaker
- Caretaker Name (first): ________________________
- 23.
- What physical activities or fitness programs would you like your child to be involved in?
- 24.
- What is your view of your child’s current physical activity or exercise program? How do you support your child’s participation in physical activities?
- 25.
- Does anything about a fitness program that involves or would involve your child concern you? (Select one)
- Display: Does anything about a fitness program that involves or would involve your child concern, you? = Yes or No
- 26.
- If you answered yes to the question above, what would the concern(s) be?
- 27.
- What would motivate your child to get more fit (rank these)? 1 (best)–6 (worst)
- 28.
- Rank order the list of rewards your child may prefer: 1 (best)–7 (worst)
- 29.
- Would you or a caretaker be willing and able to drive your child to a community-based program?
- (Select one)
- 30.
- Would it be more feasible for your child to participate in a community-based program if we provided transportation?
- (Select one)
- 31.
- Do you know what the current recommendation is for your child to exercise to maximize their bone and muscle health?
- Display: Do you know what the current recommendation is for your child to exercise to maximize their bone and muscle health = Yes or No
- 32.
- If you answered yes to the question above, what frequency are you aware of?
- 33.
- How many days per week could your child attend a fitness program, outside your home, considering your schedule, your child’s other activities, rides, etc. Rank 1 (most likely)–4 (least likely)
- 34.
- What would be your preferred frequency if there were few obstacles such as transportation or other obligations? Rank 1 (best)–4 (worst)
- 35.
- How long could your child realistically participate given current constraints (rank order)?
- 36.
- What is the biggest challenge for your child to participate in a regular fitness program?
- 37.
- Other Comments:
- End of Block: Part 2: Caretaker
- Kimbel, J. D.; Duff, S. V.; Friel, K. M.; Grant-Beuttler M.; Sukal Moulton, T.; Moreau, N. Incentives to Participate in Fitness Programming: Insights From Youth and Parents. Qualtrics. 2020.
References
- Joyner, M.J.; Barnes, J.N. I Am 80 Going on 18: Exercise and the Fountain of Youth. J. Appl. Physiol. 2013, 114, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Aerobic, Muscle- and Bone Strengthening: What Counts for School-Aged Children and Adolescents? Available online: https://www.cdc.gov/physicalactivity/basics/children/what_counts.htm (accessed on 21 March 2023).
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; US Dept of Health and Human Services: Washington, DC, USA, 2018.
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Bratteby Tollerz, L.U.; Forslund, A.H.; Olssom, R.M.; Lindström, H.; Holmbäck, U. Children with Cerebral Palsy Do Not Achieve Healthy Activity Levels. Acta Paediatr. 2015, 104, 1125–1129. [Google Scholar] [CrossRef] [PubMed]
- Vella, S.A.; Cliff, D.P.; Magee, C.A.; Okely, A.D. Sports Participation and Parent-Reported Health-Related Quality of Life in Children: Longitudinal Associations. J. Pediatr. 2014, 164, 1469–1474. [Google Scholar] [CrossRef] [PubMed]
- Vella, S.A.; Cliff, D.P.; Magee, C.A.; Okely, A.D. Associations between Sports Participation and Psychological Difficulties during Childhood: A Two-Year Follow-Up. J. Sci. Med. Sport 2015, 18, 304–309. [Google Scholar] [CrossRef]
- Sonu, S.; Post, S.; Feinglass, J. Adverse Childhood Experiences and the Onset of Chronic Disease in Young Adulthood. Prev. Med. 2019, 123, 163–170. [Google Scholar] [CrossRef]
- Peterson, M.D.; Ryan, J.M.; Hurvitz, E.A.; Mahmoudi, E. Chronic Conditions in Adults with Cerebral Palsy. JAMA 2015, 314, 2303–2305. [Google Scholar] [CrossRef]
- Ryan, J.M.; Peterson, M.D.; Ryan, N.; Smith, K.J.; O’Connell, N.E.; Liverani, S.; Anokye, N.; Victor, C.; Allen, E. Mortality Due to Cardiovascular Disease, Respiratory Disease, and Cancer in Adults with Cerebral Palsy. Dev. Med. Child Neurol. 2019, 61, 924–928. [Google Scholar] [CrossRef]
- Smith, K.J.; Peterson, M.D.; O’Connell, N.E.; Victor, C.; Liverani, S.; Anokye, N.; Ryan, J.M. Risk of Depression and Anxiety in Adults with Cerebral Palsy. JAMA Neurol. 2019, 76, 294–300. [Google Scholar] [CrossRef]
- Moreau, N.G.; Friel, K.M.; Fuchs, R.K.; Dayanidhi, S.; Sukal Moulton, T.; Grant-Beuttler, M.; Peterson, M.; Stevenson, R.; Duff, S.V. Lifelong Fitness for Ambulatory Children and Adolescents with Cerebral Palsy I: Key Ingredients for Bone and Muscle Health. Behav. Sci. 2023. accepted. [Google Scholar]
- Bjornson, K.F.; Belza, B.; Kartin, D.; Logsdon, R.; McLaughlin, J.F. Ambulatory Physical Activity Performance in Youth with Cerebral Palsy and Youth Who Are Developing Typically. Phys. Ther. 2007, 87, 248–257. [Google Scholar] [CrossRef]
- Yoon, M.J.; Choi, H.; Kim, J.S.; Lim, S.H.; Yoo, Y.J.; Hong, B.Y. Physical activity, quality of life and parenting stress in children with cerebral palsy. Pediatr. Int. 2022, 64, e15295. [Google Scholar] [CrossRef]
- Cremer, N.; Hurvitz, E.A.; Peterson, M.D. Multimorbidity in Middle-Aged Adults with Cerebral Palsy. Am. J. Med. 2017, 130, 744.e9–744.e15. [Google Scholar] [CrossRef]
- Thorpe, D. The Role of Fitness in Health and Disease: Status of Adults with Cerebral Palsy. Dev. Med. Child. Neurol. 2009, 51 (Suppl. S4), 52–58. [Google Scholar] [CrossRef]
- Strauss, D.; Brooks, J.; Rosenbloom, L.; Shavelle, R. Life Expectancy in Cerebral Palsy: An Update. Dev. Med. Child. Neurol. 2008, 50, 487–493. [Google Scholar] [CrossRef]
- Palisano, R.J.; Chiarello, L.A.; King, G.A.; Novak, I.; Stoner, T.; Fiss, A. Participation-Based Therapy for Children with Physical Disabilities. Disabil. Rehabil. 2012, 34, 1041–1052. [Google Scholar] [CrossRef]
- Reedman, S.; Boyd, R.N.; Sakzewski, L. The Efficacy of Interventions to Increase Physical Activity Participation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. Dev. Med. Child Neurol. 2017, 59, 1011–1018. [Google Scholar] [CrossRef]
- Wulf, G.; Lewthwaite, R. Optimizing Performance Through Intrinsic Motivation and Attention for Learning: The OPTIMAL Theory of Motor Learning. Psychon. Bull. Rev. 2016, 23, 1382–1414. [Google Scholar] [CrossRef]
- González-Hernández, J.; Gómez-López, M.; Pérez-Turpin, J.A.; Muñoz-Villena, A.J.; Andreu-Cabrera, E. Perfectly Active Teenagers. When Does Physical Exercise Help Psychological Well-Being in Adolescents? Int. J. Environ. Res. Public Health 2019, 16, 4525. [Google Scholar] [CrossRef]
- Cleary, S.L.; Taylor, N.F.; Dodd, K.J.; Shields, N. An Aerobic Exercise Program for Young People with Cerebral Palsy in Specialist Schools: A Phase I Randomized Controlled Trial. Dev. Neurorehabil. 2017, 20, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Shields, N.; van den Bos, R.; Buhlert-Smith, K.; Prendergast, L.; Taylor, N.A. Community-based exercise program to increase participation in physical activities among youth with disability: A feasibility study. Disabil. Rehabil. 2019, 41, 1152–1159. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, D.E.; Niles, A.; Richardson, J.; Turner, J.; Tych, M. Enhancing Function, Fitness, and Participation in Adolescents with Cerebral Palsy. Pediatr. Phys. Ther. 2006, 18, 81–82. [Google Scholar] [CrossRef]
- Lakes, K.D.; Sharp, K.; Grant-Beuttler, M.; Neville, R.; Haddad, F.; Sunico, R.; Ho, D.; Schneider, M.; Sawitz, S.; Paulsen, J.; et al. A Six Week Therapeutic Ballet Intervention Improved Gait and Inhibitory Control in Children with Cerebral Palsy—A Pilot Study. Front. Public Health 2019, 7, 137. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.M.; Cassidy, E.E.; Noorduyn, S.G.; O’Connell, N.E. Exercise Interventions for Cerebral Palsy. Cochrane Database Syst. Rev. 2017, 6, CD011660. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Peterson, M.D.; Balemans, A.C.; Hurvitz, E.A. Exercise and Physical Activity Recommendations for People with Cerebral Palsy. Dev. Med. Child Neurol. 2016, 58, 798–808. [Google Scholar] [CrossRef]
- Gaskin, C.J.; Imms, C.R.; Dagley, G.; Msall, M.E.; Reddihough, D. Successfully Negotiating Life Challenges: Learnings from Adults with Cerebral Palsy. Qual. Health Res. 2021, 31, 2176–2193. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Intrinsic and Extrinsic Motivation From a Self-Determination Theory Perspective: Definitions, Theory, Practices, and Future Directions. Contemp. Educ. Psychol. 2020, 61, 101860. [Google Scholar] [CrossRef]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, Physical Activity, and Self-Determination Theory: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 78. [Google Scholar] [CrossRef]
- Flannery, M. Self-Determination Theory: Intrinsic Motivation and Behavioral Change. Oncol. Nurs. Forum. 2017, 44, 155–156. [Google Scholar] [CrossRef]
- Duff, S.V.; Quinn, L. Motor Learning and Skill Acquisition. In Functional Movement Development across the Life Span, 2nd ed.; Cech, D., Martin, S., Eds.; WB. SaundersAspen Pub: Rockville, MD, USA, 2002; pp. 86–117. [Google Scholar]
- Gentile, A.M. A Working Model of Skill Acquisition with Application to Teaching. Quest 1972, 17, 3–23. [Google Scholar] [CrossRef]
- Gentile, A.M. Skill Acquisition: Action, Movement, and Neuromotor Processes. In Movement Science: Foundations for Physical Therapy, 2nd ed.; Carr, J.H., Shepherd, R.D., Eds.; Aspen Pub: Rockville, MD, USA, 2000; pp. 111–187. [Google Scholar]
- Muratori, L.M.; Lamberg, E.M.; Quinn, L.; Duff, S.V. Applying Principles of Motor Learning and Control to Upper Extremity Rehabilitation. J. Hand Ther. 2013, 26, 94–102; quiz 103. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Woollacott, M.; Rachwani, J.; Santamaria, V. Motor Control: Translating Research into Clinical Practice, 6th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2023. [Google Scholar]
- Sidaway, B.; Bates, J.; Occhiogrosso, B.; Schlagenhaufer, J.; Wilkes, D. Interaction of Feedback Frequency and Task Difficulty in Children’s Motor Skill Learning. Phys. Ther. 2012, 92, 948–957. [Google Scholar] [CrossRef]
- Winstein, C.J.; Pohl, P.S.; Lewthwaite, R. Effects of Physical Guidance and Knowledge of Results on Motor Learning: Support for the Guidance Hypothesis. Res. Q. Exerc. Sport 1994, 65, 316–323. [Google Scholar] [CrossRef]
- Berridge, K.C. The Debate Over Dopamine’s Role in Reward: The Case for Incentive Salience. Psychopharmacology (Berl) 2007, 191, 391–431. [Google Scholar] [CrossRef]
- Ewell, L.A.; Leutgeb, S. Replay to Remember: A Boost from Dopamine. Nat. Neurosci. 2014, 17, 1629–1631. [Google Scholar] [CrossRef]
- Ayres, A.J. Sensory Integration and Learning Disorders; Western Psychological Services: Los Angeles, CA, USA, 1972. [Google Scholar]
- Gibson, J.J. The Theory of Affordances. In Perceiving, Acting, and Knowing: Toward an Ecological Psychology; Shaw, R., Bransford, J., Eds.; Erlbaum: Mahwah, NJ, USA, 1977; pp. 67–82. [Google Scholar]
- Lauruschkus, K.; Nordmark, E.; Hallström, I. Parents’ Experiences of Participation in Physical Activities for Children with Cerebral Palsy—Protecting and Pushing towards Independence. Disabil. Rehabil. 2017, 39, 771–778. [Google Scholar] [CrossRef]
- Curran, T.; Wexler, L. School-Based Positive Youth Development: A Systematic Review of the Literature. J. Sch. Health 2017, 87, 71–80. [Google Scholar] [CrossRef]
- Pritchard, L.; Phelan, S.; McKillop, A.; Andersen, J. Child, Parent, and Clinician Experiences with a Child-Driven Goal Setting Approach in Paediatric Rehabilitation. Disabil. Rehabil. 2022, 44, 1042–1049. [Google Scholar] [CrossRef]
- Kimbel, J.D.; Duff, S.V.; Friel, K.M.; Grant-Beuttler, M.; Sukal Moulton, T.; Moreau, N. Incentives to Participate in Fitness Programming: Insights from Youth and Parents. Qualtrics Survey 2020. [Google Scholar]
- Fu, W.; Li, R.; Zhang, Y.; Huang, K. Parenting Stress and Parenting Efficacy of Parents Having Children with Disabilities in China: The Role of Social Support. Int. J. Environ. Res. Public Health 2023, 20, 2133. [Google Scholar] [CrossRef] [PubMed]
- Sakwape, K.; Machailo, R.; Koen, M.P. Exploring role strain and experiences of caregivers of children living with disabilities. Nurs. Open 2023, 10, 2886–2894. [Google Scholar] [CrossRef]
- McIntyre, L.L. Family-Based Practices to Promote Well-Being. Am. J. Intellect. Dev. Disabil. 2020, 125, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Clark, F.; Azen, S.P.; Zemke, R. Occupational Therapy for Independent Living Adults: A Randomized Controlled Trial. JAMA 1997, 278, 1321–1326. [Google Scholar] [CrossRef]
- Hill, V.A.; Vickrey, B.G.; Cheng, E.M.; Valle, N.P.; Ayala-Rivera, M.; Moreno, L.; Munoz, C.; Dombish, H.; Espinosa, A.; Wang, D.; et al. A Pilot Trial of a Lifestyle Intervention for Stroke Survivors: Design of Healthy Eating and Lifestyle after Stroke (HEALS). J. Stroke Cerebrovasc. Dis. 2017, 26, 2806–2813. [Google Scholar] [CrossRef]
- Jackson, J.; Carlson, M.; Mandel, D.; Zemke, R.; Clark, F. Occupation in Lifestyle Redesign®: The Well Elderly Study Occupational Therapy Program. Am. J. Occup. Ther. 1998, 52, 326–336. [Google Scholar] [CrossRef]
- Pyatak, E.A.; Carandang, K.; Rice Collins, C.; Carlson, M. Optimizing Occupations, Habits, and Routines for Health and Well-Being with Lifestyle Redesign®: A Synthesis and Scoping Review. Am. J. Occup. Ther. 2022, 76, 7605205050. [Google Scholar] [CrossRef]
- Slaman, J.; Roebroeck, M.; Dallmijer, A.; Twisk, J.; Stam, H.; Van Den Berg-Emons, R.; Learn 2 Move Research Group. Can a Lifestyle intervention Improve Physical Behavior in Adolescents and Young Adults with Spastic Cerebral Palsy? A Randomized Controlled Trial. Dev. Med. Child Neurol. 2015, 57, 159–166. [Google Scholar] [CrossRef]
- Slaman, J.; Roebroeck, M.; van der Slot, W.; Twisk, J.; Wensink, A.; Stam, H.; van den Berg-Emons, R.; Learn 2 Move Research Group. Can a Lifestyle intervention Improve Physical Fitness in Adolescents and Young Adults with Spastic Cerebral Palsy? A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2014, 95, 1646–1655. [Google Scholar] [CrossRef]
- Law, M.; Baptiste, S.; McColl, M.; Opzoomer, A.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: An Outcome Measure for Occupational Therapy. Can. J. Occup. Ther. 1990, 57, 82–87. [Google Scholar] [CrossRef]
- Law, M.; Anaby, D.; Imms, C.; Teplicky, R.; Turner, L. Improving the Participation of Youth with Physical Disabilities in Community Activities: An Interrupted Time Series Design. Aust. Occup. Ther. J. 2015, 62, 105–115. [Google Scholar] [CrossRef]
- Hay, J.A.; Hawes, R.; Faught, B.E. Evaluation of a Screening Instrument for Developmental Coordination Disorder. J. Adolesc. Health 2004, 34, 308–313. [Google Scholar] [CrossRef]
- Grant-Beuttler, M.; Jennings, J.; McCauley, C.; Dulay, R.; Grossnickle, K.; Kill, K.; Hay, J. Development of an Electronic Version of the Children’s Self-Perceptions of Adequacy in and Predilection for Physical Activity Scale. Pediatr. Exerc. Sci. 2017, 29, 153–160. [Google Scholar] [CrossRef]
- Rollnick, S.; Miller, W.R.; Butler, C.C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. Am. J. Pharm. Educ. 2009, 73, 127. [Google Scholar]
- Rubak, S.; Sandbaek, A.; Lauritzen, T.; Christensen, B. Motivational Interviewing: A Systematic Review and Meta-analysis. Br. J. Gen. Pract. 2005, 55, 305–312. [Google Scholar]
- Schwellnus, H.; King, G.; Baldwin, P.; Keenan, S.; Hartman, L.R. A Solution-Focused Coaching Intervention with Children and Youth with Cerebral Palsy to Achieve Participation-Oriented Goals. Phys. Occup. Ther. Pediatr. 2020, 40, 423–440. [Google Scholar] [CrossRef]
- De Shazer, S.; Berg, I.K.; Lipchik, E.; Nunnally, E.; Molnar, A.; Gingerich, W.; Weiner-Davis, M. Brief Therapy: Focused Solution Development. Fam. Process 1986, 25, 207–221. [Google Scholar] [CrossRef]
- Trepper, T.S.; Dolan, Y.; McCollum, E.E.; Nelson, T. Steve de Shazer and the Future of Solution-Focused Therapy. J. Marital. Fam. Ther. 2006, 32, 133–139. [Google Scholar] [CrossRef]
- Moreau, N.G. Muscle Performance in Children and Youth with Cerebral Palsy: Implications for Resistance Training. In Cerebral Palsy, 2nd ed.; Miller, F., Bachrach, S., Lennon, N., O’Neil, M., Eds.; Springer: Cham, Switzerland, 2020; pp. 1–12. [Google Scholar] [CrossRef]
- Moreau, N.G.; Falvo, M.J.; Damiano, D.L. Rapid Force Generation is Impaired in Cerebral Palsy and is Related to Decreased Muscle Size and Functional Mobility. Gait Posture 2012, 35, 154–158. [Google Scholar] [CrossRef]
- Lewthwaite, R.; Chiviacowsky, S.; Drews, R.; Wulf, G. Choose to Move: The Motivational Impact of Autonomy Support on Motor Learning. Psychon. Bull. Rev. 2015, 22, 1383–1388. [Google Scholar] [CrossRef] [PubMed]
- Darrah, J.; Wessel, J.; Nearingburg, P.; O’Connor, M. Evaluation of a Community Fitness Program for Adolescents with Cerebral Palsy. Pediatr. Phys. Ther. 1999, 11, 18–23. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duff, S.V.; Kimbel, J.D.; Grant-Beuttler, M.; Sukal-Moulton, T.; Moreau, N.G.; Friel, K.M. Lifelong Fitness in Ambulatory Children and Adolescents with Cerebral Palsy II: Influencing the Trajectory. Behav. Sci. 2023, 13, 504. https://doi.org/10.3390/bs13060504
Duff SV, Kimbel JD, Grant-Beuttler M, Sukal-Moulton T, Moreau NG, Friel KM. Lifelong Fitness in Ambulatory Children and Adolescents with Cerebral Palsy II: Influencing the Trajectory. Behavioral Sciences. 2023; 13(6):504. https://doi.org/10.3390/bs13060504
Chicago/Turabian StyleDuff, Susan V., Justine D. Kimbel, Marybeth Grant-Beuttler, Theresa Sukal-Moulton, Noelle G. Moreau, and Kathleen M. Friel. 2023. "Lifelong Fitness in Ambulatory Children and Adolescents with Cerebral Palsy II: Influencing the Trajectory" Behavioral Sciences 13, no. 6: 504. https://doi.org/10.3390/bs13060504
APA StyleDuff, S. V., Kimbel, J. D., Grant-Beuttler, M., Sukal-Moulton, T., Moreau, N. G., & Friel, K. M. (2023). Lifelong Fitness in Ambulatory Children and Adolescents with Cerebral Palsy II: Influencing the Trajectory. Behavioral Sciences, 13(6), 504. https://doi.org/10.3390/bs13060504




