Abstract
Fibromyalgia Syndrome (FMS) is a chronic condition of widespread pain accompanied by several symptoms such as stiffness, fatigue, sleep problems, depression, anxiety, and cognitive deficits. To date, there is no specific treatment for FMS. The European League Against Rheumatism, and the majority of the international recommendations for managing FMS, has claimed psychoeducational intervention as the first step in FMS treatment for adequate symptoms management. However, scientific studies in this regard are scarce, diverse, and with contradictory findings. Results integration from analogous studies could provide a clear presentation of the real clinical value of psychoeducation in FMS. Therefore, the current systematic review aims at exploring the effect of psychoeducation on emotional, clinical, and functional symptoms of FMS patients and encourages researchers towards psychoeducation’s procedure optimization and systematization. The systematic review was conducted according to the guidelines of the Cochrane Collaboration and PRISMA statements. The selected articles were evaluated using the Cochrane risk of bias (ROB) assessment tool. The selected articles were extracted from PubMed, Scopus, and Web of Science databases. The literature search identified 11 studies eligible for the systematic review. The ROB evaluation revealed that 2 of the 11 studies showed a low quality, the other 2 had a moderate quality, and the remaining 7 studies exhibited a high quality. Results showed that psychoeducation is generally included as an important first therapeutic step in multicomponent treatments for FMS. Moreover, psychoeducation generally seems to be quite beneficial in reducing emotional (i.e., number of days feeling emotionally well, general anxiety, depression levels, etc.) and clinical symptoms (levels of fatigue, morning stiffness, pain intensity, etc.), as well as increasing functional status (i.e., general physical function, morning fatigue, stiffness, etc.). Despite that psychoeducation´s clinical benefits are highlighted, there is scarce amount of research on psychoeducation beyond its usefulness as part of multicomponent treatments.
1. Introduction
Fibromyalgia Syndrome (FMS) is conceptualized as a chronic condition of widespread pain accompanied by fatigue, sleep problems, depression, and anxiety [1,2,3]. In addition, there is also evidence of cognitive problems in FMS (also called “fibro fog” [4,5]), comprising deficits in attention, perception, concentration, memory, and higher cognitive functions [4,6,7,8,9]. Its prevalence is estimated in 2–4% of the general population, being more frequent in women than in men [2]. In this detail, recent research showed a possible gender bias that seems to lead professionals to underestimate FMS prevalence in men and overestimate it in women [8,9]. FMS negatively impacts the health-related quality of life, especially in activities of daily life, work, career, parenting, interpersonal relationships, and mental health [10,11,12,13].
Related to the negative impact of FMS on the patients’ lives, psychosocial factors (e.g., stress level, social support, personality traits, etc.) seem to play a relevant mediating role between the disease symptoms and their influence on general health and daily activities [14,15]. Moreover, some studies have revealed FMS patients are characterized to a greater extent by personality traits such as alexithymia [16,17], neuroticism [18,19,20], psychoticism [19], avoidant personality [21,22], and type D personality [23]. The last is defined by a high negative affect and social inhibition [24]. FMS patients also tend to exhibit lower self-esteem [6,25,26], difficulties in pain-related self-efficacy [27,28], a negative self-image [29,30], higher levels of pain catastrophizing [19,31], and altered emotional processing [32,33,34,35,36].
The etiology of FMS is still unknown, being a biopsychosocial and multifactorial disorder, in which numerous factors such as genetic predisposition, endocrine factors, stressful life events, physical trauma, sleep problems, and emotional and cognitive disturbances among others, interactively intervene [15]. Unfortunately, given the multitude of factors implicated, no objective clinical test to confirm its diagnosis is currently available [37,38,39,40].
There exist different hypotheses related to FMS etiology. The most empirically supported is the presence of a Central Sensitization to pain phenomenon and deficiencies in endogenous pain and inhibitory mechanisms [41,42,43,44]. These deficiencies are corroborated by greater activation of the “pain neuromatrix” under experimental evocation of pain [45] and abnormally low levels of the neurotransmitters involved in descending pain inhibition (e.g., serotonin or norepinephrine) in FMS [46]. Likewise, inadequate functioning of the inhibitory pathways mediated by the activity of endogenous opioids [47] and an increase in neurotransmitters involved in nociceptive facilitation such as Substance P [48] have been confirmed in FMS. In addition, Central Sensitization to pain in FMS is assumed to prevent the inhibition normally exerted by Aβ fibers responsible for conducting sensory information [49] on the Aδ and C nociceptive pathways [50].
In brief, Central Sensitization to pain in FMS implies hyperexcitability and excessive synaptic efficacy in Central Nervous System (CNS) neurons involved in sensory and nociceptive processing [51,52]. This derives in hyperexcitability of afferent (ascending) nociceptive pathways [53] and inhibition of the efferent (descending) anti-nociceptive pathways [47,54]; which ends up altering the adequate and protective pain signal inhibition [55].
On the behavioral level, the Central Sensitization to pain in FMS is further supported by lower pain thresholds and tolerance as well as the presence of hyperalgesia and allodynia [7,41].
Other hypotheses have discussed the genetic and neurological influence on FMS. Apropos of the first, the HLA class I and II antigen (e.g., DR4) and polymorphisms related to the reuptake of 5-hydroxytryptamine (or serotonin, 5-HTT) such as 5-HTTLPR, or those associated with the catecholaminergic and serotonergic systems such as catechol-O-methyltransferase [56,57] have been contemplated. In reference to the second, less density or peripheral neuropathy in small fibers in FMS patients has been most recently discovered [58,59].
Given the etiological mechanisms of FMS are not totally well-known, there is currently no consensus about its appropriate therapy, and sometimes, treatment effects have been claimed to be unsatisfactory [60]. Several interventions, especially the combination of pharmacological and non-pharmacological treatments, however, seem to be useful in lessening FMS symptoms and their impact on the general quality of life [61,62,63,64]. Positive effects of interventions such as cognitive-behavioral therapy (CBT) [65,66,67], mindfulness training [68,69,70], acceptance and commitment therapy (ACC) [71,72], and moderate exercise [65] have been also stated.
Among the mentioned therapies, CBT has been proven to be the most effective therapy for FMS [66,73,74,75]. CBT is composed by psychoeducation, attitudes´ acquisition, training on pain-healthy beliefs, strategies for the maintenance of adequate lifestyles and the prevention of relapses, physiological deactivation techniques (abdominal breathing and relaxation), and cognitive intervention on maladaptive/negative disease beliefs, expectations, and behaviors [74,75,76]. For cognitive intervention, cognitive restructuring, problem-solving, and attention management techniques are used [66,67,75,76]. Though less effective, mindfulness therapy is intended to bolster FMS patients’ ability to be focused on the present moment through meditation, conscious breathing, body scan, and mindful movements [68,69,70]. ACC therapy attempts to increase psychological flexibility, pain acceptance, and treatment process commitment in FMS [77]. Psychological flexibility allows FMS patients to accept and manage a variety of unavoidable events associated with pain, instead of investing energy in fighting with them. ACC reduces avoidance behaviors, facilitates acceptance and contact with the present, and promotes a state of mental calm [71,72,78].
On the subject of moderate exercise interventions, FMS patients are advised to avoid a sedentary lifestyle and keep active at the physical and social levels [62]. The Body Mass Index (BMI), social isolation, general functioning, and well-being are demonstrated to be improved and controlled by exercise and physical activity interventions [60,70,79,80]. Obesity seems to be a common problem in FMS patients which is associated with greater pain sensitivity, poorer sleep quality, reduced physical strength and flexibility [81,82], and marked reduction of cognitive performance [82].
Most therapy approaches directed to FMS patients include psychoeducation as the first phase of the treatment due to its relevance in patients’ adherence and prognosis [66,67]. Indeed, according to the European League Against Rheumatism (EULAR) recommendations for managing FMS, psychoeducational intervention has to be the first mandatory step in FMS patients’ treatment [83]. In line with the above, Multidisciplinary Pain Education Programs (MPEP) have been observed to be significantly beneficial in Central Pain Sensitization (CPS) conditions [84,85]. FMS is well-known to be the prototypical CPS condition [86].
Broadly, the main purposes of educative interventions are: (1) to give patients and caregivers the necessary information about the pathologies´ characteristics and treatment options; and (2) to provide details on potential positive effects on family functioning and patient behavior [87]. Patient´s education may be defined as any set of educative activities planned by qualified professionals and aimed at providing information and/or restructuring the patients´ disease perception and, therefore, improving patients’ health-related behaviors and/or status [88].
FMS´s psychoeducation generally involves information about the distinction between acute and chronic pain, FMS nature, disease contributing factors, treatments that are most safe and effective, and the symptoms´ characteristics; and coping strategies, among others [83,89,90,91]. Moreover, educative programs may contribute to increase therapeutic adherence as previously reported, self-confidence, self-esteem, and pain self-efficacy in FMS patients [92]. An efficient psychoeducation in FMS patients might positively impact the disease’s treatment and prognosis [92].
As a whole, patient education, as a part of a wider multidisciplinary program, might be not only useful but crucial for FMS patients’ symptom management [67,89]. Psychoeducation in FMS patients may increase the knowledge and understanding of the disease, being a therapeutic strategy itself that positively impacts the rest of the treatment [62,93,94]. To the extent that patients understand what FMS is and deconstruct the myths surrounding this disease: (1) a better active and healthy facing of the disease will be achieved [95]; (2) FMS patients will be more likely to draw upon support networks and socio-health resources [95]; and (3) to develop a more favorable attitude towards the disease, which will also have a potential impact on the disease treatment and prognosis [93,94,95].
Nonetheless, further research is needed to determine a framework from which to develop non-pharmacological interventions (i.e., psychological therapies) guidelines in FMS [15], including the optimization and systematization of psychoeducational programs. Scientific studies in this regard are scarce, methodologically diverse (i.e., different combinations of therapies, several protocols of psychoeducation, variability related to the number of sessions of psychoeducation, etc.), and with findings in different directions [83,86]. Results integration from analogous studies could provide a clear presentation of the real clinical value of psychoeducation in FMS.
Based on the previous aforementioned literature, the current systematic review intended to: (1) explore the effect of psychoeducation on emotional (e.g., depression and anxiety), clinical (e.g., pain), and functional (e.g., fatigue, health-related quality of life and impact´s disease) FMS related-outcomes; and (2) encourage further research on clinical settings psychoeducation methodization.
2. Materials and Methods
2.1. Search Strategy
This systematic review was performed according to the guidelines of the Cochrane Collaboration and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [96]. The search terms were as follows: “fibromyalgia” and “psychoeducation”. The terms were extracted from the Medical Subject Headings (MeSH). The PICO question was: what is the effect of psychoeducation on emotional, clinical, and functional related outcomes in FMS?
The selected articles were extracted from PubMed, Scopus, and Web of Science databases. All articles were screened; those that fulfilled the inclusion criteria for full-text analysis were selected. Among these, the titles and abstracts were revised to remove those not relevant for the review. Afterward, the resulting articles were screened in depth for eligibility. To attain a final set of articles to be reviewed, the full texts of relevant articles were retrieved and screened based on the inclusion and exclusion criteria. The PRISMA flowchart (Figure 1) shows the screening and selection process for the inclusion of studies. The last search was conducted on 1 February 2023.
2.2. Eligibility Criteria
Inclusion criteria were as follows: (1) peer-reviewed original studies of FMS and psychoeducation (i.e., longitudinal studies, pilot studies, pilot randomized controlled trials, randomized controlled clinical, quasi-experimental replicated single-case/small group designs, and uncontrolled and controlled pre-post-test studies); (2) studies comprising adult patients (≥18 years old) with an official diagnosis of FMS; and (3) studies written in English. The exclusion criteria were: (1) review article or meta-analysis; (2) comment, editorial, case report, letter, or meeting/congress abstract; and (3) non-English publication.
2.3. Data Extraction and Quality Assessment
The study characteristics, methodologies, and results were extracted independently by C.M.G.-S. and C.I.M. in the following sequence: first author, study name, country, year of publication, study design, sample size and the number of participants in each study group, participant age and sex, and the diagnostic criteria of FMS. The study characteristics are presented in Table 1.
With the objective of assessing the quality of the selected articles, the risk of bias (ROB) in each study was evaluated by C.M.G.-S. and C.I.M. according to the Cochrane ROB assessment tool. This tool comprises seven items evaluating ROB: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. For each item, the ROB was graded as high, medium, or low. Moreover, the global quality of each article was also assessed.
2.4. Data Synthesis
In view of the aim of the current systematic review, the authors checked each study´s main objectives, the methodology, and if there were or were not control groups included. In addition, the characteristics and purposes of FMS psychoeducational programs (i.e., the effect on emotional, clinical, and/or functional symptoms, the content of sessions, the number of interventions, etc.) were analyzed together with the pre-post and follow-up results. The clinical relevance of the main findings and the principal limitations of each research were also determined (see Table 1 for more detail). In addition, the specific subject-matter of the FMS psychoeducational programs are detailed in Table 2. Finally, the biases of each study were analyzed and reported in the Section 3.4 and Table 3 The latter analyses were performed to determine the effect of psychoeducation in FMS with the commitment to improve FMS clinical intervention and guide future research lines in this field.
3. Results
3.1. Literature Search and Study Characteristics
From among a total of 62 articles identified by database searches, 21 were finally selected for screening after removing duplicates. A general PRISMA flow chart was devised detailing the number of studies excluded at each stage of the screening (Figure 1). An analysis of 11 full-text articles was conducted in order to determine their eligibility for the present review. Only 11 articles fulfilled the inclusion criteria; therefore, they were subjected to the data extraction (Table 1) and quality assessment (Table 3) processes. The selected studies were published between 2002 and 2022. Of the 11 studies, 1 was a Delphi technique [97], 2 were pilot studies [98,99], and 8 were randomized controlled trials [100,101,102,103,104,105,106,107]. Four studies were conducted in Spain [98,100,101,102], 2 in Sweden [99,107], 2 in Canada [104,105], 1 in The United States of America [106], 1 in Ireland, the United Kingdom, North America, and other non-specified countries [103], and 1 in Brazil [97]. The 11 selected studies included a total of 1659 participants (age range: 27–60 years old), of which 1073 were FMS patients.
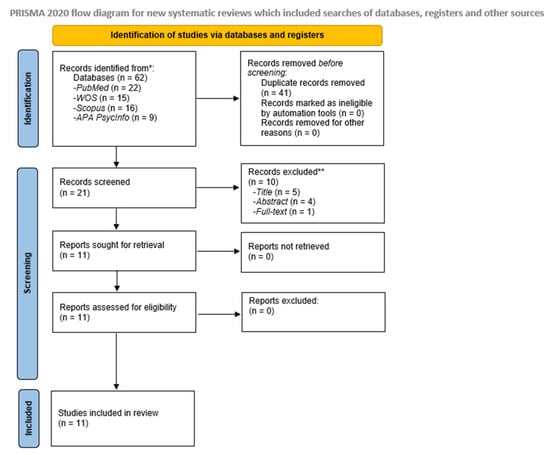
Figure 1.
Flow diagram for relevant eligible studies related to psychoeducation effects on emotional, clinical, and functional Fibromyalgia Syndrome related-outcomes.
Figure 1.
Flow diagram for relevant eligible studies related to psychoeducation effects on emotional, clinical, and functional Fibromyalgia Syndrome related-outcomes.
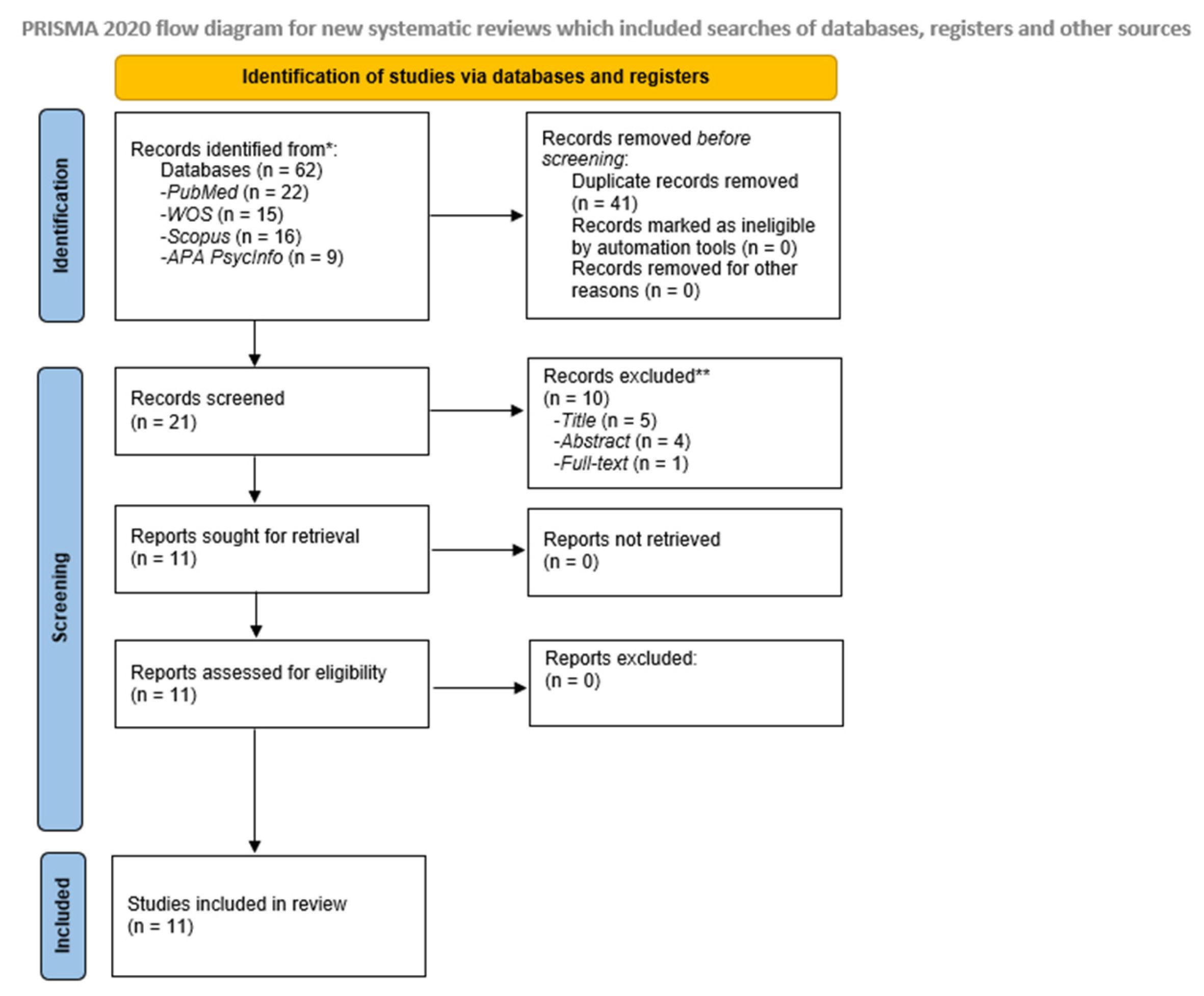

Table 1.
Characteristics of relevant eligible studies related to psychoeducation effects on emotional, clinical, and functional Fibromyalgia Syndrome´ related-outcomes.
Table 1.
Characteristics of relevant eligible studies related to psychoeducation effects on emotional, clinical, and functional Fibromyalgia Syndrome´ related-outcomes.
| First Author (Publication Year), Study Name, Country | Objectives | Study Design/Procedure | Sample Size [Mean ± Age (SD)] | FMS Diagnostic Criteria | Instruments and Variables | Results |
|---|---|---|---|---|---|---|
| Antunes et al. (2022). Amigos de Fibro (Fibro Friends): Validation of an Educational Program to Promote Health in Fibromyalgia. Brazil. [97]. | To validate a multidisciplinary educational health promotion program for individuals with FMS. | Delphi technique. Procedure: Phases: (1) Development of Amigos de Fibro; (2) Content validation of Amigos de Fibro; (3) Adjusting the Amigos de Fibro; (4) Final assessment of Amigos de Fibro; and (5) Final version of Amigos de Fibro. | N = 23 health professionals (expert judges). 10 males (43.5%) and 13 females (56.5%). Aged between 31 and 40 years old (39.2%). N = 45 individuals with FMS (target audience). 4 males (9%) and 41 females (91%). Aged between 31 and 40 years old (38%). | 2016 ACR, revised version. | Groups of professionals and individuals with FMS listed their demands through the focus group. Evaluation of Amigos de Fibro, built with the information and results obtained from the first round, regarding the objectives, proposed themes and initiatives, relevance, writing style, and structure of the program (with specialists and individuals with FMS). Final evaluation of the material after the corrections are made, based on the judges’ suggestions. | Content validity index (CVI) ≤ 0.78 and coefficient kappa ≤ 0.61. All 25 items evaluated in both groups presented considerable minimum CVI by CVI and the kappa coefficient. Global CVI of Amigos de Fibro, by the specialist judges, was 0.90; and 0.95 by the target audience judges. The kappa coefficient of the expert judges was 0.90 and that of the target audience judges was 0.85. Amigos de Fibro was considered with adequate content validity and internal consistency. |
| Pérez-Aranda et al. (2021). Do humor styles predict clinical response to the MINDSET (MINDfulneSs & EducaTion) program? A pilot study in patients with fibromyalgia. Spain. [98]. | To explore the role of humor styles in predicting clinical changes after the multicomponent intervention (MINDSET) that combines mindfulness and psychoeducation for FMS patients. | Pilot Study. * Procedure: MINDSET intervention: 4 psychoeducation sessions about FMS, based on a previously validated program, and 4 sessions of mindfulness training, based on the Mindfulness-Based Stress Reduction curriculum. Psychoeducation Sessions: 2 h, twice per week, run by health psychologists in a group setting of 8–10 patients. Intervention added on to the patient’s usual care (i.e., medication). No additional active treatments. | N = 35 FMS patients. N = 34 (97.1%) FMS female patients [54.97 ± 8.65]. | 1990 ACR. | FFMQ-15. FIQR. HSQ. PGIC. | FMS patients: affiliative humor and positive/negative ratio humor styles had a unique predictive effect on self-reported clinical changes. Association between humor styles with functional impact and mindfulness facets. Some humor styles may imply a better disposition in patients to learn and implement the concepts and resources that the intervention offered. |
| Melin et al. (2018). Psychoeducation against depression, anxiety, alexithymia, and fibromyalgia: a pilot study in primary care for patients on sick leave. Sweden. [99]. | (1) To try the feasibility of ASSA in a Swedish primary care setting; (2) to explore associations between symptoms of depression, anxiety, alexithymia, and MUPS. | Pilot Study. * ¤ Procedure: ASSA began with 8 group sessions—‘the Affect School’, which were followed directly by 10 individual sessions—‘the Script Analysis’. All 27 respondents one-week post-intervention terminated ASSA within 20 weeks from the start. Script Analysis sessions were performed with one instructor, either the physiotherapist, the GP, or one social counselor. Affect School comprised 8 weekly, 2-h sessions, of a 5–7 participant group, led by the same instructors (one psychotherapist, one physiotherapist, and one GP) during all sessions. Psychoeducation Sessions: 8 weekly 2-h sessions with a 5–7 participant group led by two instructors followed by 10 individual hour-long sessions. Follow-up: 18 months. | N = 36 patients. 29 female patients (81%). Median age 39, range 27–60 years. (N FMS patients: 2 [6%]). | Not specified. | TAS-20. SASB. SCI-93. EuroQol ‘health barometer’ (100 mm—VAS). | Patients: one-week post-intervention median test score changes were significantly favorable for 9 of 11 measures (depression, anxiety, alexithymia, MUPS, general health, self-affirmation, self-love, self-blame, and self-hate); at 18 months post-intervention the results remained significantly favorable for 15 respondents for 7 of 11 measures (depression, alexithymia, MUPS, general health, self-affirmation, self-love, and self-hate). |
| Feliu-Soler et al. (2016). Cost-utility and biological underpinnings of Mindfulness-Based Stress Reduction (MBSR) versus a psychoeducational program (FibroQoL) for fibromyalgia: a 12-month randomized controlled trial (EUDAIMON study). Spain [102]. | (1) To examine the effectiveness and cost-utility for FMS patients of MBSR as an add-on to treatment as usual (TAU) versus TAU + the psychoeducational program FibroQoL, and versus TAU only; (2) to examine pre-post differences in brain structure and function, as well as levels of specific inflammatory markers in the three study arms; and (3) to analyze the role of some psychological variables as mediators of 12-month clinical outcomes. | 12-month randomized controlled trial. * ¤ Procedure: Protocol in progress. Psychoeducation Sessions (FibroQoL): 8, 2-h sessions. Three treatment arms: (1) TAU + MBSR; (2) TAU + FibroQoL; (3) TAU. Control Group: TAU (pharmacologic treatment + counselling about aerobic exercise adjusted to patients’ physical limitations). Active control group: TAU + FibroQoL. FibroQoL: a psycho-educational program for FMS patients based on a consensus document drawn up by the Health Department of Catalonia. Planned follow-up: 12 months. | N = 180 FMS female patients. N = 60 FMS female patients per group. | 1990 ACR. | Sociodemographic-clinical questionnaire. Structured Clinical Interview for DSM Axis I Disorders (SCID-I). Screening measures: MMSE. Primary Outcome: FIQR. Secondary Outcomes: CSRI. EQ-5D-5L. FFMQ. FSDC. HADS. MISCI. PCS. PIPS. PSS. SCS. Other measures: CEQ. PGIC. PSIC. Log of out-session for MBSR and psychotherapeutic practices. Adverse events of the interventions. Neuroimaging MRI. Brain structure: VBM. Inflammatory markers: Blood samples. | Protocol in progress. |
| Bourgault et al. (2015). Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: a mixed-methods randomized controlled trial. Canada [104]. | To evaluate, quantitatively and qualitatively, the efficacy of the PASSAGE Program—a multicomponent interdisciplinary group intervention for the self-management of FMS. | A mixed-methods randomized controlled trial. * ¤ Intervention (INT) vs. waitlist (WL). Qualitative group interviews with a subset of patients were also conducted. Procedure: Intervention: PASSAGE Program (a structured multicomponent interdisciplinary group intervention aimed at reducing FMS symptoms and maintaining optimal function through the use of self-management strategies and patient education). 9 group sessions with 8 participants lasting 2.5 h each. Each session involved 3 major components: (1) psycho-educational tools; (2) CBT-related techniques; and (3) patient-tailored exercise activities. Follow-up: 3 months. | N = 28 INT Group. 26 females (92.9%). [49.98 ± 9.23]. N = 28 WL Group. 26 females (92.9%). [46.74 ± 11.42]. | 1990 ACR. | Primary outcomes: Change in pain intensity (0–10). Secondary outcomes: Fibromyalgia severity. Pain interference. Sleep quality. Pain coping strategies. Depression. Health-related quality of life. PGIC. Perceived pain relief. | FMS patients: the intervention had a statistically significant impact on the three PGIC measures. At the end of the PASSAGE Program, the percentages of patients who reported pain relief and perceived overall improvement on their pain levels, functioning, and quality of life were significantly higher in the INT Group than in the WL Group. The same differences were observed 3 months post-intervention. The results of the qualitative analysis were in line with the quantitative findings regarding the efficacy of the intervention. The improvement, however, was not reflected in the primary and secondary outcomes. |
| Dowd et al. (2015). Comparison of an Online Mindfulness-based Cognitive Therapy Intervention With Online Pain Management Psychoeducation: A Randomized Controlled Study. Ireland, the UK, North America, and other countries [103]. | To test the effectiveness of a computerized mindfulness-based cognitive therapy intervention (MIA) compared to computerized pain management psychoeducation (PE) in a randomized study. | A randomized controlled study. * ¤ Procedure: Participants in each condition received 12 sessions of treatment, twice per week for 6 weeks. MIA intervention was based on established mindfulness meditation and emotional regulation programs shown to be effective for chronic pain. Psychoeducation Sessions: based on many of the common elements found within pain management programs. The PE program was presented in a series of twice-weekly emails containing written information about chronic pain self-management. Follow-up: 6 months. | N = 124 chronic pain patients. 112 females (90.3%) and 12 males). [44.53 ± 12.25]. N MIA group = 62 participants (N FMS patients: 15). N PE group = 62 participants. (N FMS patients: 18). | Not specified. | Primary Outcomes: Pain interference (BPI). Psychological Distress (HADS). Secondary Outcomes: Pain Intensity: 2 NRS from BPI. PCS. SWL. Average Pain Pain Right Now. CPAQ. MAAS. PGIC. | FMS patients: both groups showed improvements in pain interference, pain acceptance, and catastrophizing from pre-treatment to post-treatment and at follow-up. Reduced average pain intensity from baseline to post-treatment for both groups, but not at follow-up. Increases in subjective well-being, were more pronounced in the MIA than in the PE group. MIA group: greater reduction in pain ‘right now’, and increases in their ability to manage emotions, manage stress and enjoy pleasant events on completion of the intervention. |
| Luciano et al. (2013). Cost-Utility of a Psychoeducational Intervention in Fibromyalgia Patients Compared With Usual Care. An Economic Evaluation Alongside a 12-Month Randomized Controlled Trial. Spain. [101]. | (1) To determine the effectiveness of adding psychoeducational treatment implemented in general practice to usual care for patients with fibromyalgia; (2) to analyze the cost-utility of the intervention from health care and societal perspectives. | 12-month randomized controlled trial. * ¤ Procedure: See Luciano et al., 2011. | See Luciano et al., 2011. | 1990 ACR. | See Luciano et al., 2011. | FMS patients who received psychoeducation: greater improvement on global functional status, physical functioning, pain, morning fatigue, stiffness, and depression. It was confirmed the long-term clinical effectiveness of a psychoeducational treatment program for FMS implemented at the primary care level and the cost-utility from a healthcare and societal perspective. |
| Luciano et al. (2011). Effectiveness of a Psychoeducational Treatment Program Implemented in General Practice for Fibromyalgia Patients. A Randomized Controlled Trial. Spain. [100]. | To examine whether a psychoeducational intervention implemented in primary care is more effective than usual care for improving the functional status of patients with FMS. | Randomized Controlled Trial. * ¤ Procedure: The treatment program is based on a consensus document developed by an expert panel in 2005 and published in 2006 by the Catalan Health Department. Psychoeducation Sessions: 9, 2-h sessions (5 sessions of education and 4 sessions of autogenic relaxation), delivered over a 2-month period (1-afternoon session per week), run by GP and rheumatologist, with a maximum of 18 patients per group. Six separate intervention groups were performed. Intervention group: Usual care from their GP + psychoeducational program. Control group: Usual care from their GP. Usual care from their GP: pharmacologic treatment + counselling about aerobic exercise adjusted to patients’ physical limitations. Follow-up: 12 months. | N = 211 participants. N = 105 intervention group. FMS female patients (97.2%) [55.17 ± 8.58]. N = 106 control group. FMS female patients (98.1%) [55.42 ± 8.63]. | 1990 ACR. | Sociodemographic Questionnaire. Chronic Medical Conditions Checklist. Marlowe-Crowne Social Desirability Scale. FIQ. STAI. | FMS patients who received psychoeducation: a 2-month psychoeducational intervention improves the functional status to a greater extent than usual care, at least in the short-term. The social desirability bias did not explain the reported outcomes. Trait anxiety was associated with response to treatment. |
| Mannerkorpi et al. (2009). Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analyses. Sweden [107]. | To evaluate the effects of pool exercise in patients with fibromyalgia and chronic widespread pain and to determine characteristics influencing the effects of treatment. | Randomized controlled trial. * ¤ Procedure: 20-session exercise programme combined with a standardized 6-session education programme based on self-efficacy principles with an active control group, which undertook the same education programme. Psychoeducation Sessions: The education programme, which was designed to introduce strategies to cope with FMS symptoms, consisted of 6 1-h sessions, conducted once a week for 6 weeks. The programme was led by a physiotherapist. The pedagogical approach was based on the active participation of the patients through discussions and practical exercises. The control group received the same education programme. Exercise programme: comprised 20 sessions of 45-min pool exercise once a week for 20 weeks in temperate (33 °C) water, supervised by a physiotherapist. The exercise was planned to permit individual progress, aiming to improve overall function and to motivate regular physical activity. Follow-up: 11–12 months after the baseline. | N = 166: 134 FMS female patients + 32 chronic widespread pain (CWP) female patients. N = 81 Exercise—Education Group. [44.60 ± 9.26]. Intervention group. N = 85 Education Group. [46.50 ± 8.30]. Control Group. | 1990 ACR. | Primary outcomes: FIQ total score. Body functions (6MWT). Secondary outcomes: Pain (the FIQ Pain). Fatigue (the FIQ Fatigue). Depression (HADS-D). Health-related quality of life (SF36). Amount of leisure time physical activity (LTPAI). Exploratory outcomes: Clinical manifestations of stress (SCI). Multiple dimensions of fatigue (MFI-20). Experience in physical activity (ITT and PP). Note: PP is defined as attendance at least 60% of the sessions. | FMS patients: The exercise-education programme showed significant, but small, improvement on health status in patients with fibromyalgia and chronic widespread pain, compared with education only. Patients with milder symptoms improved most with this treatment. |
| Rook et al. (2007). Group Exercise, Education, and Combination Self-management in Women With Fibromyalgia. United States [106]. | To evaluate and directly compare the effects of 4 common self-management interventions on well-established measures of functional status, symptom severity, and self-efficacy in women with fibromyalgia. | Randomized Controlled Trial. * ¤ Procedure: Both exercise programs involved approximately 60 min of activity per session. Each session began with a brief warm-up of walking on a treadmill at a comfortable pace and then progressed to a self-determined level of moderate effort for a predetermined amount of time. All participants, regardless of fitness level, began with 5 min of walking and increased a maximum of 2 to 4 min weekly following a predetermined progression. The AE group progressed to a total of 45 min of walking. The ST group reached a maximum of 20 min of treadmill walking followed by 25 min of strength training movements. Psychoeducation Sessions: The Fibromyalgia Self-Help Course (FSHC) is a 7-session program that teaches individuals with fibromyalgia about the condition and self-management skills. Sessions were 120 min long every 2 weeks. All FSHC instructors were certified by the Arthritis Foundation. Follow-up: 6 months. | N = 207 enrolled and randomized FMS female patients. N = 138 FMS female patients who completed the intervention. N = 35 Aerobic and flexibility exercise (AE) Group [48.00 ± 11.00]. N = 35 strength training, aerobic, and flexibility exercise (ST) Group. [50.00 ± 11.00]. N = 27 the Arthritis Foundation’s Fibromyalgia Self-Help Course (FSHC) Group. [51.00 ± 12.00]. N = 38 a combination of ST and FSHC (ST-FSHC) Group. [50.00 ± 11.00]. | 1990 ACR. | Primary outcomes: Change in physical function from baseline to completion of the intervention (FIQ and SF-36). Secondary outcomes: Social and emotional function, symptoms (FIQ, the bodily pain and vitality subscales of the SF-36, and BDI). Self-efficacy (adapted Arthritis Self-Efficacy Scale). | FMS patients: progressive walking, simple strength training movements, and stretching activities improve functional status, key symptoms, and self-efficacy in women with fibromyalgia actively being treated with medication. The benefits of exercise are enhanced when combined with targeted self-management education. Appropriate exercise and patient education be included in the treatment of fibromyalgia. |
| King et al. (2002). The effects of exercise and education, individually or combined, in women with fibromyalgia. Canada [105]. | To examine the effectiveness of a supervised aerobic exercise program, a self-management education program, and the combination of exercise and education for women with fibromyalgia (FMS). | Randomized controlled trial with repeated measures design. * ¤ Procedure: The intervention programs were based upon principles of self-management (Bandura’s social cognitive theory). Treatment programs ran simultaneously for 12 weeks. Due to the large number of subjects required, the programs were offered on 5 different occasions over a 2 year period (winter–spring once, fall–winter, and spring–summer twice each). Education Group: met once a week for one and a half to 2 h per session. Exercise and education group: combined exercise and education programs. The educational component was the same as for the education-only group. The exercise-only group met twice per week and on the third day met for education and then exercise. Control group: On the day of the initial assessment, they were given a page of instructions for basic stretches and 5 items related to general coping strategies. They were contacted once or twice throughout the 12-week period to ensure they were filling out their logbook and to answer any questions. Subjects from the control group were offered one of the intervention programs at the end of the follow-up period. Follow-up: 3 months. | N = 170 FMS female patients. N = 46 Exercise Group. [45.2 ± 9.4]. N = 48 Education Group. [44.9 ± 10.0]. N = 37 Exercise & Education Group. [47.4 ± 9.0]. N = 39 Control Group. [47.3 ± 7.3]. | 1990 ACR. | SE. SE Pain. SE Function. SE Coping with symptoms. FIQ. 6MW. Tender Point Count. Total Survey Site Score. | FMS patients: subjects receiving the combination of exercise and education and who complied with the treatment protocol improved their perceived ability to cope with other symptoms. A supervised exercise program increased walking distance at post-test, an increase that was maintained at follow-up in the exercise-only group. Results demonstrate the challenges with conducting exercise and education studies in persons with FMS. |
Note: * Pre and Post Evaluation. ¤ Follow-up assessment. Abbreviations: 6MW: Six Minute Walk; 6MWT: 6-min walk test; ACR: American College of Rheumatology’s Criteria; ASSA: Affect School and Script Analyses; BPI: Brief Pain Inventory; CBT: Cognitive-Behavioral Therapy; CEQ: Adapted version of the Credibility/Expectancy questionnaire; CPAQ: Chronic Pain Acceptance Questionnaire; CSRI: Client Service Receipt Inventory; CVI: Content Validity Index; EQ-5D-5L: EuroQoL-5D questionnaire; FFMQ: Five Facet Mindfulness Questionnaire; FFMQ-15: Five-Facets Mindfulness Questionnaire; FIQ: Fibromyalgia Impact Questionnaire; FIQR: Revised Fibromyalgia Impact Questionnaire; FMS: Fibromyalgia Syndrome; FSDC: Fibromyalgia Survey Diagnostic Criteria; FSHC: Fibromyalgia Self-Help Course; GP: General Practitioners; HADS: Hospital Anxiety and Depression Scale; HSQ: Humor Styles Questionnaire; INT: Intervention; ITT: Intention-to-treat; LTPAI: The Leisure Time Physical Activity Instrument; MAAS: Mindful Attention Awareness Scale; MBSR: Mindfulness-Based Stress Reduction; MFI-20: The Multidimensional Fatigue Inventory; MIA: Mindfulness-based Cognitive Therapy Intervention; MIR: Magnetic Resonance Imaging; MISCI: Multidimensional Inventory of Subjective Cognitive Impairment; MMSE: Mini-Mental State Examination; MUPS: Medically Unexplained Physical Symptoms; NRS: numerical rating scales; PCS: Pain Catastrophizing Scale; PE: Pain Management Psychoeducation; PGIC: Patient Global Impression of Change; PIPS: Psychological inflexibility in pain scale; PP: per-protocol; PSIC: Pain Specific Impression of Change; PSS: Perceived Stress Scale; SASB: Structural Analysis of Social Behavior assessment tool; SCI: The Stress and Crisis Inventory; SCI-93: Stress and Crisis Inventory-93; SCS-12: Self-Compassion Scale-short form; SE: Chronic Pain Self-Efficacy Scale; STAI: State Trait Anxiety Inventory; SWL: Satisfaction with Life Scale; TAS-20: Toronto Alexithymia Scale-20 items; TAU: Treatment as Usual; UK: United Kingdom; VAS: Visual Analogue Scale; VBM: Voxel-Based Morphometry; WL: Waiting List.
3.2. Psychoeducation and Emotional, Clinical, and Functional Related-Outcomes in Fibromyalgia Syndrome
Psychoeducation has generally been included as part of the multi-component treatments for FMS patients and the success of these treatments has in fact been attributed to the characteristic combination of therapeutic strategies [98,102,103,104,105,106,107].
The first group of researchers proposed a multi-component program, namely the MINDSET (MINDfulneSs & EducaTion) program [98], which combined mindfulness and psychoeducation. In the reference study, Pérez-Aranda et al. [98] found that affiliative humor and positive/negative ratio humor styles had a unique predictive effect on self-reported clinical changes [98]. Additionally, significant correlations between humor styles and functional impact and mindfulness facets were also reported [98]. The authors concluded that some humor styles may imply a better disposition in patients to learn and implement the concepts and resources offered by mindfulness and psychoeducation sessions [98]. Participants showed a notable degree of adherence (74% of attendance to the sessions) and considered the intervention satisfactory (9/10), useful (8.9/10), recommendable (8.7/10), and non-aversive (0.5/10), in a post-treatment ad-hoc opinion survey [98].
Other researchers also combined psychoeducation with mindfulness-based therapies. For instance, Feliu-Soler et al. [102] created a protocol to evaluate the cost-utility and biological underpinnings of a Mindfulness-Based Stress Reduction (MBSR) intervention versus a psychoeducational program (FibroQoL) for FMS. The protocol proposed a 12-month randomized controlled trial (EUDAIMON study) with the purpose of: (1) analyzing the aforementioned cost-utility; (2) examining pre-post differences in brain structure and function; (3) determining the level of specific inflammatory markers in the three study arms or branches; and (4) exploring the mediational role of psychological variables on the 12-month clinical outcomes [102]. Unfortunately, the protocol remains to be tested.
Similarly, Dowd et al. [103] compared an Online Mindfulness-based Cognitive Therapy Intervention (MIA) with an Online Pain Management Psychoeducation (PE), in a randomized controlled study. Dowd et al. [103] reported that both groups (i.e., PE and MIA groups) showed improvements on pain interference, pain acceptance, and catastrophizing from pre-treatment to post-treatment and follow-up. Average pain intensity was also reduced from baseline to post-treatment, but not at follow-up, for both groups [103]. Increases in subjective well-being were more pronounced in the MIA than in the PE group [103]. Upon completion of the intervention, MIA group showed a greater reduction in pain ‘right now’, and an increase in the ability to manage both emotions and stress and enjoy pleasant events [103].
By contrast, Luciano et al. [100] conducted a randomized control trial for testing a multi-component treatment combining usual care and psychoeducation. The psychoeducational intervention consisted in a 2-month program that was proved to improve at short-term the functional status to a greater extent than the usual care [100]. Social desirability bias—also evaluated in Luciano et al. [100]—did not explain the reported outcomes, and trait anxiety was associated with response to treatment [100]. The 12-month follow-up showed a greater improvement on the global functional status, physical functioning, pain, morning fatigue, stiffness, and depression in FMS patients who did receive psychoeducation [101]. The sensitivity analysis suggested that the intervention was cost-effective even after imputing all missing data [101]. As the authors advised, its implementation at primary care will benefit 3 FMS patients rather than 1, as befall with the standard treatment [101].
Multi-component programs combining psychoeducation and physical exercises were also found in three of the reviewed articles [104,105,106,107]. In the study of Bourgault et al. [104] the beneficial effects of a multicomponent interdisciplinary group intervention for the self-management of FMS, named the PASSAGE program, were explored. The PASSAGE program was aimed at reducing FMS symptoms and maintaining optimal function through the use of self-management strategies and patient education. This program included 3 key intervention components: (1) psycho-educational tools; (2) CBT-related techniques; and (3) patient-tailored physical exercise activities. The percentages of patients reporting pain relief and perceiving an overall improvement on pain levels, functioning, and quality of life were significantly higher in the INT Group (Intervention Group) than in the WL Group (Waiting list Group) [104].
King et al. [105] studied the effects of physical exercise (walking exercises) and education, individually or combined, in FMS patients. The authors observed that FMS patients receiving the combination of physical exercise and education, and complied with the treatment protocol, significantly improved their perceived ability to cope with other symptoms.
Likewise, Mannerkorpi et al. [107] implemented an intervention of pool exercise and education for patients with FMS and chronic widespread pain and compared it with single education. Authors observed that the pool exercise-education program showed significant—but lesser—improvement on health status in FMS and chronic widespread pain patients, compared with single education.
Rook et al. [106] combined physical exercise, education, and self-management in an intervention program addressed to FMS patients. Results pointed out that progressive walking, simple strength training movements, and stretching activities enhanced functional status, the characteristics symptoms of the disorder, and self-efficacy in FMS patients [106]. Moreover, the physical exercise´s benefits were further intensified when was united with targeted self-management education [106].
Despite the aforementioned results, the reviewed studies showed scarce research on psychoeducation benefits beyond its usefulness as part of multicomponent treatments. Moreover, the differences in the protocol and the variability between interventions were also prevalent. Solely Melin et al. [99] conducted a pilot study to test the effectiveness of a psychoeducation program for depression, anxiety, and alexithymia in FMS and chronic pain patients. Nine of the 11 factors evaluated were significative favorable one-week post-intervention. This was the case of depression, anxiety, alexithymia, Medically Unexplained Physical Symptoms (MUPS), general health, self-affirmation, self-love, self-blame, and self-hate. Eighteen months post-intervention, changes remained significantly favorable for 7 of the 11 factors (i.e., depression, alexithymia, MUPS, general health, self-affirmation, self-love, and self-hate) but this result was restricted to 15 patients. Unfortunately, only 6% of the sample included in the study of Melin et al. [99] were FMS patients. Findings must therefore be considered with caution.
3.3. Structure of the Fibromyalgia Syndrome Psychoeducation Programs
The specific subject-matter of the FMS psychoeducational programs are detailed in Table 2. As a whole, the programs included information related to the diagnosis, typical symptoms (i.e., pain, fatigue, and sleep problems), and manners to cope with them, usual disease progress, comorbid medical conditions, potential etiology, information about: (1) the influence of psychosocial factors on symptoms; (2) treatments (pharmacological and non-pharmacological); (3) FMS typical myths; (4) the benefits of regular physic exercise; (5) the typical barriers to behavior change; and (6) chronic pain´ resources (i.e., personal, derived from the relatives, the social network, communities, and/or social organizations such as patients associations, etc.) and care services, among others [97,98,99,100,101,102,103,104,105,106,107]. The authors agreed on emphasizing the need to provide enough time to solve possible doubts in patients and ended up the program with a summary session [97,98,99,100,101,102,103,104,105,106,107].
It should be not overlooked, the lack of systematization between the different psychoeducation programs analyzed. Reliability and validity analyses of the programs’ structure were also predominantly missed. Only Antunes et al. [97] validated the “Amigos de Fibro (Fibro Friends)” program; an educational program to promote health in FMS. On purpose, Antunes et al. [97] informed of an adequate content validity and internal consistency for the program.

Table 2.
Structure of the Fibromyalgia Syndrome psychoeducation programs.
Table 2.
Structure of the Fibromyalgia Syndrome psychoeducation programs.
| Study (Author and Year) | Psychoeducation Program Content |
|---|---|
| Antunes et al. (2022) [97]. |
|
| Pérez-Aranda et al. (2021) [98]. |
|
| Melin et al. (2018). Affect School [99]. |
(1) Joy; (2) Fear; (3) Interest and surprise; (4) Shame; (5) Anger; (6) Distaste and dissmell; (7) Distress; (8) Pain.
(2) How we act in different situations and how we interpret experiences are depending on our scripts; (3) Scripts are formed by family rules and common cultural rules for how affects should be handled; (4) Intensity and expressions of emotion are controlled by scripts; (5) Affects can be completely suppressed and thereby unconscious.
(2) How do you know that you feel…? (3) Do you feel … in a particular place in your body? (4) Does it happen often that you feel…? (5) How do you know that someone else is…? (6) Can you understand and accept another person’s…? |
| Feliu-Soler et al. (2016). FibroQoL. [102]. |
|
| Bourgault et al. (2015) [104]. |
|
| Dowd et al. (2015) [103]. |
|
| Luciano et al. (2011) [100]. Luciano et al. (2013) [101]. |
|
| Mannerkorpi et al. (2009) [107]. |
|
| Rook et al. (2007) [106]. | The Fibromyalgia Self-Help Course (FSHC):
|
| King et al. (2002) [105]. |
|
Abbreviations: FMS: Fibromyalgia Syndrome.
3.4. Risk of Bias
The ROB evaluation (see Table 3) revealed that 2 of the 11 studies showed a low quality [98,99], the other 2 demonstrated a moderate quality [97,103], and the 7 remaining exhibited a high quality [100,101,102,103,104,105,106,107]. The most frequent biases were performance bias (blinding of participants and personnel) and detection bias (blinding of outcome assessment).
The recognized limitations by authors included: (1) the small number of FMS patients taking part in the studies [98,99]; (2) the lack of a control group [98,99] or an active control group [101]; (3) the absence of other clinical, coping-related, and mindfulness measures [98]; (4) the use of insufficient assessment instruments [101]; (5) difficulties in the control and assessment of the home practice [103]; (6) the non-analysis of common comorbid psychiatric disorders (i.e., major depression, personality disorders, etc.) [100], and other relevant variables such as the pharmacological intake [99]; and (7) the non-report of the follow-up assessments [100]. The last did not let prove whether intervention led to neither permanent improvement on FMS patients’ functional status or determine the direct and indirect costs derived from interventions—an aspect especially relevant when policymakers are involved.
Other limitations were also found by the present review, such as: (1) the non-specifications of the number of male and female patients [98,99,103]; (2) the non-sample match in sex, with a high predominance of female [97,98,99,100,101,102,103,104,105,106,107]; (3) the absence of male FMS patients [102]; (4) the non-specification of the primary and secondary outcomes [98,99,100,101,105]; (5) the non-perform of the follow-up assessments [98]; (6) the lack of information about participants´ nationality [103]; (7) the absence of a pilot study testing the program utility and effectivity [97]; (8) the non-specification of the FMS diagnostic criteria used [99,103]; (9) the general low sample size [99]; (10) the non-use of any measure for patients experiences and opinions (i.e., the Patient Global Impression of Change [PGIC]) [98,99,100,101]; (11) the lack of details on the sample characteristics related to the diagnosis [99]; and (12) the non-clarification of how the sample size was calculated [98,99,107]. By contrast, 7 studies a priori determined the sample size [100,101,102,103,104,105,106].
The aforementioned biases and limitations need to be overcome in future studies to better understand the effect of psychoeducation on FMS patients and improve the FMS interventions.

Table 3.
Risk of Bias Assessment of relevant eligible studies.
Table 3.
Risk of Bias Assessment of relevant eligible studies.
| Study (Author and Year) | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Blinding of Participants and Personnel (Performance Bias) | Blinding of Outcome Assessment (Detection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) | Other Bias | General Assessment (Low, Medium, High) |
|---|---|---|---|---|---|---|---|---|
| Antunes et al. (2022) [97]. | H | L | H | L | L | L | Yes | Medium |
| Pérez-Aranda et al. (2021) [98]. | H | H | H | H | L | L | Yes | Low |
| Melin et al. (2018) [99]. | H | H | H | H | L | L | Yes | Low |
| Feliu-Soler et al. (2016) [102]. | L | L | L | L | L | L | Yes | High |
| Bourgault et al. (2015) [104]. | L | L | L | L | L | L | Yes | High |
| Dowd et al. (2015) [103]. | L | L | H | H | L | L | Yes | Medium |
| Luciano et al. (2013) [101]. | L | L | L | L | L | L | Yes | High |
| Luciano et al. (2011) [100]. | L | L | L | L | L | L | Yes | High |
| Mannerkorpi et al. (2009) [107]. | L | L | L | L | L | L | Yes | High |
| Rook et al. (2007) [106]. | L | L | L | L | L | L | Yes | High |
| King et al. (2002) [105]. | L | L | L | L | L | L | Yes | High |
Note: L: Low, M: Medium, H: High.
4. Discussion
The present systematic review aimed at exploring the effect of psychoeducation in emotional, clinical, and functional related-outcomes in FMS patients and encouraging further research on clinical settings psychoeducation optimization.
The review confirmed psychoeducation is generally included as a part of other multi-component treatments [98,102,103,104,105,106,107]. Indeed, among the studies reviewed, only Melin et al. [99] evaluated a single psychoeducational program confirming its feasibility for patients on sick leave due to depression and/or anxiety. Psychoeducation was mostly evaluated in interaction with mindfulness [98,102,103], TAU (Treatment as Usual) [100,101] or physical exercise [104,105,106,107]. On behalf of the first, the MINDSET (MINDfulneSs & EducaTion) program [98] demonstrated that some humor styles might lead to higher readiness to learn and use the concepts and resources offered by mindfulness and psychoeducation intervention in FMS patients [98]. Nonetheless, though authors considered MINDSET clinically relevant for the emotions and emotions´ regulation in the treatment of FMS, the specific effect of psychoeducation sessions was not studied at all.
The EUDAIMON study proposed by Feliu-Soler et al. [102] consisted in a protocol of a 12-month randomized controlled trial, to examine the cost-utility and biological underpinnings of Mindfulness-Based Stress Reduction (MBSR) in comparison with a psychoeducational program (FibroQoL) in FMS. However, as in the above study, no firm conclusion about psychoeducation was drawn. The proposed protocol lacked of a real implementation.
Fortunately, the Online combined program MIA-PE by Dowd et al. [103] did evidence equivalent changes across several evaluated outcomes for participants in both conditions (psychoeducation and mindfulness) over time (e.g., improvements on pain interference, pain acceptance, and catastrophizing and reduced average pain intensity). Even so, the MIA intervention showed a number of unique benefits (e.g., greater reduction in pain ‘right now’, increases in the ability to manage both emotions and stress and enjoy pleasant events). Note that the level of participant attrition in the study highlighted the relevance of fostering to a greater extent participant engagement in future online chronic pain programs [103]. In this regard, after the situation provoked by the COVID-19 the online therapies have been postulated as essential. COVID-19 consequences have been especially negative for chronic pain patients in general [108], and FMS patients in particular [108]. The wide accessibility and low-cost of online intervention methods establish their offer as rather fundamental and worthy in FMS patients [109,110,111,112].
With respect to TAU and psychoeducation, Luciano et al. [100] showed a greater increase in patients’ functional status compared to usual care by itself [100]. Specific improvements were reported in physical function, the total number of days of feeling well, levels of pain, general fatigue, morning fatigue, stiffness, anxiety (less trait anxiety), and depression [100]. In the follow-up of the Luciano et al. [101] study, the long-term clinical effectiveness of the psychoeducational treatment was confirmed in FMS patients [101].
Regarding the multi-component programs incorporating psychoeducation and physical exercises [104,105,106,107], particularly, the PASSAGE [104] program aimed at reducing FMS symptoms and maintaining optimal function through the use of self-management strategies and patient education through sessions involved 3 major components: (1) psycho-educational tools; (2) CBT-related techniques; and (3) patient-tailored exercise activities. Authors informed of significantly greater levels of pain relief and perceived overall improvement on functioning, and quality of life in the INT Group compared to the WL Group [104]. King et al. [105] also reported an enriched in the perceived ability to cope with other symptoms in FMS patients who received the combination of exercise and education and follow entirely the treatment protocol. Mannerkorpi et al. [107] pointed out that the implementation of an education and pool exercise combination in FMS and chronic widespread pain patients led to a slight augmentation in the health status of both patients´ groups compared with the single education. Consistently, Rook et al. [106] using a program based on Group Exercise (progressive walking, simple strength training movements, and stretching activities), Education, and Self-management in FMS patients observed that progressive walking, simple strength training movements, and stretching activities improved functional status, key symptoms of the disorder, and self-efficacy in FMS patients [106]. Interestingly, the benefits of physical exercise (i.e., progressive walking, simple strength training movements, and stretching activities) increased when combined with targeted self-management education [106].
The evaluated studies confirm a positive value of education in chronic pain, specifically in FMS [98,102,103,104,105,106,107]; and its benefits on the patient’s functional status [100,101,107], physical function, pain [100,101,104], fatigue, stiffness, depression [100,101], anxiety [99,100,101], and quality of life [104]. Findings are also in line with the scientific evidence suggesting that multicomponent therapies in FMS may reduce pain, fatigue, depressed mood, and health-related quality of life disabilities, as well as, improve self-efficacy, pain coping, and physical fitness, compared to the single education, WL, or TAU [104,105,106,107,113,114,115,116,117].
Hence, the present systematic review confirms psychoeducation as clinically relevant for FMS, but especially when used in combination with other treatments. This entails support for the majority of evidence-based guidelines for the management of FMS that highly recommend multicomponent treatment [83,91,118]. For instance, the Multi-Component Cognitive Behavioral Therapy (MCCBT) for FMS is recommended by Division 12: Society of Clinical Psychology of the American Psychological Association (APA) [73]. The MCCBT for FMS often includes the following components and techniques: (1) education about the syndrome, including its nature and the patient´s role in its care; (2) symptom self-management skills targeting pain, fatigue, sleep, cognition, mood, and functional status (e.g., deep relaxation and breathing, graded activation, pleasant activity scheduling, and sleep hygiene); and (3) lifestyle change promoting skills targeting barriers to change, unhelpful thinking styles, and long term maintenance of change (e.g., stress management, goal setting, structured problem solving, reframing, and communication skills) [73].
Despite the reported benefits, it is important to highlight the scarce studies on psychoeducation beyond its usefulness as part of multicomponent treatments and, e.g., the limited small FMS sample size [99]. Indeed, Melin et al. [99] was the only study evaluating a single psychoeducation program, but unfortunately did not account for a satisfying FMS sample size. Further research lines, especially for FMS patients, on psychoeducation effectiveness have been revealed to be required. Research on FMS male patients, and FMS patients from other countries (apart from Europe)—note sociocultural factors influencing psychoeducation interventions—related to the effectiveness of psychoeducation and the etiology of the disease, and/or validation of psychoeducation are encouraged to enhance evidence-based clinical practice in FMS treatment and create and optimize a unique and common protocol between researchers and clinicians. The latter could allow addressing the cost-effectiveness or cost-utility of nonpharmacological treatments in FMS patients.
5. Conclusions
To conclude, to date, psychoeducation has been generally included in other FMS multicomponent treatments. These multicomponent therapies seem to be useful for FMS treatment, with psychoeducation an undoubtedly essential component. However, the reviewed evidence does not certainly support the total utility of psychoeducation as a single treatment. Its beneficial effects are mostly enhanced in a multi-component treatment or in relation to other interventions. In addition, a lack of a psychoeducational systematic and homogeneous protocol between studies is discerned. Though further research is required, the present findings value the importance of ensuring that patients benefit from the enhancer-positive effects of psychoeducation.
Author Contributions
Conceptualization, C.M.G.-S. and C.I.M.; methodology, C.M.G.-S. and C.I.M.; formal analysis, C.M.G.-S. and C.I.M.; investigation, C.M.G.-S. and C.I.M.; resources, C.M.G.-S. and C.I.M.; data curation, C.M.G.-S. and C.I.M.; writing—original draft preparation, C.M.G.-S. and C.I.M.; writing—review and editing, C.M.G.-S. and C.I.M.; C.M.G.-S. and C.I.M.; supervision, C.M.G.-S. and C.I.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant from the Consejería de Universidad, Investigación e Innovación en materia de I+D+i de la Junta de Andalucía (ProyExcel_00374).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990, 33, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B.; Yunus, M.B. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Thieme, K.; Turk, D.C.; Flor, H. Comorbid depression and anxiety in fibromyalgia syndrome: Relationship to somatic and psychosocial variables. Psychosom. Med. 2004, 66, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.L.; Huang, C.J.; Fang, S.C.; Ko, L.H.; Tsai, P.S. Cognitive Impairment in Fibromyalgia: A Meta-Analysis of Case-Control Studies. Psychosom. Med. 2018, 80, 432–438. [Google Scholar] [CrossRef]
- Teodoro, T.; Edwards, M.J.; Isaacs, J.D. A unifying theory for cognitive abnormalities in functional neurological disorders, fibromyalgia and chronic fatigue syndrome: Systematic review. J. Neurol. Neurosurg. Psychiatry 2018, 89, 1308–1319. [Google Scholar] [CrossRef]
- Galvez-Sanchez, C.M.; Reyes del Paso, G.A.; Duschek, S. Cognitive impairments in fibromyalgia syndrome: Associations with positive and negative affect, alexithymia, pain catastrophizing and self-esteem. Front. Psychol. 2018, 9, 377. [Google Scholar] [CrossRef]
- Reyes del Paso, G.A.; Pulgar, A.; Duschek, S.; Garrido, S. Cognitive impairment in fibromyalgia syndrome: The impact of pain, emotional disorders, medication, and cardiovascular regulation. Eur. J. Pain 2012, 16, 421–429. [Google Scholar] [CrossRef]
- Srinivasan, S.; Maloney, E.; Wright, B.; Kennedy, M.; Kallail, K.J.; Rasker, J.J.; Häuser, W.; Wolfe, F. The Problematic Nature of Fibromyalgia Diagnosis in the Community. ACR Open Rheumatol. 2019, 1, 43–51. [Google Scholar] [CrossRef]
- Wolfe, F.; Walitt, B.; Perrot, S.; Rasker, J.J.; Häuser, W. Fibromyalgia diagnosis and biased assessment: Sex, prevalence and bias. PLoS ONE 2018, 13, e0203755. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C.M.; Montoro, C.I.; Duschek, S.; Del Paso, G.A.R. Pain catastrophizing mediates the negative influence of pain and trait-anxiety on health-related quality of life in fibromyalgia. Qual. Life Res. 2020, 29, 1871–1881. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C.M.; Montoro, C.I.; Duschek, S.; Reyes del Paso, A. Depression and trait-anxiety mediate the influence of clinical pain on health-related quality of life in fibromyalgia. J. Affect. Disord. 2020, 265, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Perrot, S.; Vicaut, E.; Servant, D.; Ravaud, P. Prevalence of fibromyalgia in France: A multi-step study research combining national screening and clinical confirmation: The DEFI study (Determination of Epidemiology of FIbromyalgia). BMC Musculoskelet. Disord. 2011, 12, 224. [Google Scholar] [CrossRef]
- Lee, J.W.; Lee, K.E.; Park, D.J.; Kim, S.H.; Nah, S.S.; Lee, J.H.; Kim, S.K.; Lee, Y.A.; Hong, S.J.; Kim, H.S.; et al. Determinants of quality of life in patients with fibromyalgia: A structural equation modeling approach. PLoS ONE 2017, 12, e0171186. [Google Scholar] [CrossRef] [PubMed]
- Montoro, C.I.; Galvez-Sánchez, C.M. The Mediating Role of Depression and Pain Catastrophizing in the Relationship between Functional Capacity and Pain Intensity in Patients with Fibromyalgia. Behav. Neurol. 2022, 2022, 9770047. [Google Scholar] [CrossRef] [PubMed]
- Galvez-Sánchez, C.M.; Duschek, S.; Reyes Del Paso, G.A. Psychological impact of fibromyalgia: Current perspectives. Psychol. Res. Behav. Manag. 2019, 12, 117–127. [Google Scholar] [CrossRef]
- Montoro, C.I.; Reyes del Paso, G.A.; Duschek, S. Alexithymia in fibromyalgia syndrome. Pers. Individ. Differ. 2016, 102, 170–179. [Google Scholar] [CrossRef]
- Castelli, L.; Tesio, V.; Colonna, F.; Molinaro, S.; Leombruni, P.; Bruzzone, M.; Fusaro, E.; Sarzi-Puttini, P.; Torta, R. Alexithymia and psychological distress in fibromyalgia: Prevalence and relation with quality of life. Clin. Exp. Rheumatol. 2012, 30 (Suppl. 74), 70–77. [Google Scholar]
- Vural, M.; Berkol, T.D.; Erdogdu, Z.; Kucukserat, B.; Aksoy, C. Evaluation of personality profile in patients with fibromyalgia syndrome and healthy controls. Mod. Rheumatol. 2014, 24, 823–828. [Google Scholar] [CrossRef]
- Montoro, C.I.; Duschek, S.; Muñoz Ladrón de Guevara, C.; Fernández-Serrano, M.J.; Reyes del Paso, G.A. Aberrant cerebral blood flow responses during cognition: Implications for the understanding of cognitive deficits in fibromyalgia. Neuropsychology 2015, 29, 173–182. [Google Scholar] [CrossRef]
- Malin, K.; Littlejohn, G.O. Personality and fibromyalgia syndrome. Open Rheumatol. J. 2012, 6, 273–285. [Google Scholar] [CrossRef]
- Uguz, F.; Ciçek, E.; Salli, A.; Karahan, A.Y.; Albayrak, I.; Kaya, N.; Uğurlu, H. Axis I and Axis II psychiatric disorders in patients with fibromyalgia. Gen. Hosp. Psychiatry 2010, 32, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Gumà-Uriel, L.; Peñarrubia-María, M.T.; Cerdà-Lafont, M.; Cunillera-Puertolas, O.; Almeda-Ortega, J.; Fernández-Vergel, R.; García-Campayo, J.; Luciano, J.V. Impact of IPDE-SQ personality disorders on the healthcare and societal costs of fibromyalgia patients: A cross-sectional study. BMC Fam. Pract. 2016, 17, 61. [Google Scholar] [CrossRef] [PubMed]
- van Middendorp, H.; Lumley, M.A.; Jacobs, J.W.; van Doornen, L.J.; Bijlsma, J.W.; Geenen, R. Emotions and emotional approach and avoidance strategies in fibromyalgia. J. Psychosom. Res. 2008, 64, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Denollet, J. DS14: Standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom. Med. 2005, 67, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Garaigordobil, M. Fibromialgia: Discapacidad funcional, autoestima y perfil de personalidad. Inf. Psicol. 2013, 106, 4–16. [Google Scholar] [CrossRef]
- Michielsen, H.J.; Van Houdenhove, B.; Leirs, I.; Vandenbroeck, A.; Onghena, P. Depression, attribution style and self-esteem in chronic fatigue syndrome and fibromyalgia patients: Is there a link? Clin. Rheumatol. 2006, 25, 183–188. [Google Scholar] [CrossRef]
- Vong, S.K.; Cheing, G.L.; Chan, C.C.; Chan, F.; Leung, A.S. Measurement structure of the Pain Self-Efficacy Questionnaire in a sample of Chinese patients with chronic pain. Clin. Rehabil. 2009, 23, 1034–1043. [Google Scholar] [CrossRef]
- Mannerkorpi, K.; Svantesson, U.; Broberg, C. Relationships between performance-based tests and patients’ ratings of activity limitations, self-efficacy, and pain in fibromyalgia. Arch. Phys. Med. Rehabil. 2006, 87, 259–264. [Google Scholar] [CrossRef]
- Baptista, A.S.; Villela, A.L.; Jones, A.; Natour, J. Effectiveness of dance in patients with fibromyalgia: A randomized, single-blind, controlled study. Clin. Exp. Rheumatol. 2012, 30 (Suppl. 74), 18–23. [Google Scholar]
- Van Overmeire, R.; Vesentini, L.; Vanclooster, S.; Muysewinkel, E.; Bilsen, J. Body Image, Medication Use, and Mental Health among Women with Fibromyalgia in Flanders, Belgium. Int. J. Environ. Res. Public Health 2022, 19, 1418. [Google Scholar] [CrossRef]
- Varallo, G.; Suso-Ribera, C.; Ghiggia, A.; Veneruso, M.; Cattivelli, R.; Guerrini Usubini, A.; Franceschini, C.; Musetti, A.; Plazzi, G.; Fontana, J.M.; et al. Catastrophizing, Kinesiophobia, and Acceptance as Mediators of the Relationship between Perceived Pain Severity, Self-Reported and Performance-Based Physical Function in Women with Fibromyalgia and Obesity. J. Pain Res. 2022, 15, 3017–3029. [Google Scholar] [CrossRef] [PubMed]
- Scarpina, F.; Ghiggia, A.; Vaioli, G.; Varallo, G.; Capodaglio, P.; Arreghini, M.; Castelli, L. Altered recognition of fearful and angry facial expressions in women with fibromyalgia syndrome: An experimental case-control study. Sci. Rep. 2022, 12, 21498. [Google Scholar] [CrossRef] [PubMed]
- Fischer-Jbali, L.R.; Montoro, C.I.; Montoya, P.; Halder, W.; Duschek, S. Central nervous activity during implicit processing of emotional face expressions in fibromyalgia syndrome. Brain Res. 2021, 1758, 147333. [Google Scholar] [CrossRef]
- Fischer-Jbali, L.R.; Montoro, C.I.; Montoya, P.; Halder, W.; Duschek, S. Central nervous activity during a dot probe task with facial expressions in fibromyalgia. Biol. Psychol. 2022, 172, 108361. [Google Scholar] [CrossRef] [PubMed]
- Amaro-Díaz, L.; Montoro, C.I.; Fischer-Jbali, L.R.; Galvez-Sánchez, C.M. Chronic Pain and Emotional Stroop: A Systematic Review. J. Clin. Med. 2022, 11, 3259. [Google Scholar] [CrossRef] [PubMed]
- Fischer-Jbali, L.R.; Montoro, C.I.; Montoya, P.; Halder, W.; Duschek, S. Central nervous activity during an emotional Stroop task in fibromyalgia syndrome. Int. J. Psychophysiol. 2022, 177, 133–144. [Google Scholar] [CrossRef]
- Choy, E.; Perrot, S.; Leon, T.; Kaplan, J.; Petersel, D.; Ginovker, A.; Kramer, E. A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Serv. Res. 2010, 10, 102. [Google Scholar] [CrossRef]
- Hooten, W.M.; Timming, R.; Belgrade, M.; Gaul, J.; Goertz, M.; Haake, B.; Walker, N. Assessment and Management of Chronic Pain; Institute for Clinical Systems Improvement (ICSI): Bloomington, MN, USA, 2013. [Google Scholar]
- Moyano, S.; Kilstein, J.G.; de Miguel, C.A. Nuevos criterios diagnósticos de fibromialgia: ¿vinieron para quedarse? Reumatol. Clin. 2014, 3, 716–721. [Google Scholar] [CrossRef]
- Okifuji, A.; Turk, D.C.; Sinclair, J.D.; Starz, T.W.; Marcus, D.A. A standardized manual tender point survey. I. Development and determination of a threshold point for the identification of positive tender points in fibromyalgia syndrome. J. Rheumatol. 1997, 24, 377–383. [Google Scholar]
- Montoro, C.I.; Duschek, S.; de Guevara, C.M.; Reyes Del Paso, G.A. Patterns of Cerebral Blood Flow Modulation During Painful Stimulation in Fibromyalgia: A Transcranial Doppler Sonography Study. Pain Med. 2016, 17, 2256–2267. [Google Scholar] [CrossRef]
- de la Coba, P.; Montoro, C.I.; Reyes Del Paso, G.A.; Galvez-Sánchez, C.M. Algometry for the assessment of central sensitisation to pain in fibromyalgia patients: A systematic review. Ann. Med. 2022, 54, 1403–1422. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C.M.; Muñoz Ladrón de Guevara, C.; Montoro, C.I.; Fernández-Serrano, M.J.; Duschek, S.; Reyes Del Paso, G.A. Cognitive deficits in fibromyalgia syndrome are associated with pain responses to low intensity pressure stimulation. PLoS ONE 2018, 13, e0201488. [Google Scholar] [CrossRef] [PubMed]
- de la Coba, P.; Bruehl, S.; Galvez-Sánchez, C.M.; Reyes Del Paso, G.A. Slowly Repeated Evoked Pain as a Marker of Central Sensitization in Fibromyalgia: Diagnostic Accuracy and Reliability in Comparison with Temporal Summation of Pain. Psychosom. Med. 2018, 80, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Gracely, R.H.; Geisser, M.E.; Giesecke, T.; Grant, M.A.; Petzke, F.; Williams, D.A.; Clauw, D.J. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 2004, 127 Pt 4, 835–843. [Google Scholar] [CrossRef] [PubMed]
- Millan, M.J. Descending control of pain. Prog. Neurobiol. 2002, 66, 355–474. [Google Scholar] [CrossRef]
- Julien, N.; Goffaux, P.; Arsenault, P.; Marchand, S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain 2005, 114, 295–302. [Google Scholar] [CrossRef]
- Russell, I.J.; Orr, M.D.; Littman, B.; Vipraio, G.A.; Alboukrek, D.; Michalek, J.E.; Lopez, Y.; MacKillip, F. Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome. Arthritis Rheum. 1994, 37, 1593–1601. [Google Scholar] [CrossRef]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152 (Suppl. 3), S2–S15. [Google Scholar] [CrossRef]
- Scholz, J.; Woolf, C.J. Can we conquer pain? Nat. Neurosci. 2002, 5, 1062–1067. [Google Scholar] [CrossRef]
- Clauw, D.J. Diagnosing and treating chronic musculoskeletal pain based on the underlying mechanism(s). Best Pract. Res. Clin. Rheumatol. 2015, 29, 6–19. [Google Scholar] [CrossRef]
- Woolf, C.J.; Salter, M.W. Neuronal plasticity: Increasing the gain in pain. Science 2000, 288, 1765–1768. [Google Scholar] [CrossRef] [PubMed]
- Staud, R.; Koo, E.; Robinson, M.E.; Price, D.D. Spatial summation of mechanically evoked muscle pain and painful aftersensations in normal subjects and fibromyalgia patients. Pain 2007, 130, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Gebhart, G.F. Descending modulation of pain. Neurosci. Biobehav. Rev. 2004, 27, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Price, D.D.; Staud, R. Neurobiology of fibromyalgia syndrome. J. Rheumatol. 2005, 75, 22–28. [Google Scholar]
- Arnold, L.M.; Hudson, J.I.; Hess, E.V.; Ware, A.E.; Fritz, D.A.; Auchenbach, M.B.; Starck, L.O.; Keck, P.E., Jr. Family study of fibromyalgia. Arthritis Rheum. 2004, 50, 944–952. [Google Scholar] [CrossRef]
- Buskila, D.; Sarzi-Puttini, P. Biology and therapy of fibromyalgia. Genetic aspects of fibromyalgia syndrome. Arthritis Res. Ther. 2006, 8, 218. [Google Scholar] [CrossRef] [PubMed]
- Farhad, K.; Oaklander, A.L. Fibromyalgia and small-fiber polyneuropathy: What’s in a name? Muscle Nerve 2018, 58, 611–613. [Google Scholar] [CrossRef]
- Martínez-Lavín, M. Fibromyalgia and small fiber neuropathy: The plot thickens! Clin. Rheumatol. 2018, 37, 3167–3171. [Google Scholar] [CrossRef]
- Álvarez-Gallardo, I.C.; Bidonde, J.; Busch, A.; Westby, M.; Kenny, G.P.; Delgado-Fernández, M.; Carbonell-Baeza, A.; Rahman, P.; De Angelis, G.; Brosseau, L. Therapeutic validity of exercise interventions in the management of fibromyalgia. J. Sports Med. Phys. Fitness 2019, 59, 828–838. [Google Scholar] [CrossRef]
- Arnold, L.M.; Gebke, K.B.; Choy, E.H. Fibromyalgia: Management strategies for primary care providers. Int. J. Clin. Pract. 2016, 70, 99–112. [Google Scholar] [CrossRef]
- González, E.; Elorza, J.; Failde, I. Comorbilidad psiquiátrica y Fibromialgia. Su efecto sobre la calidad de vida de los pacientes [Psychiatric comorbidity and Fibromyalgia and Its effect on the quality of life of patients]. Actas Esp. Psiquiatr. 2010, 38, 295–300. [Google Scholar] [PubMed]
- Samami, E.; Shahhosseini, Z.; Elyasi, F. The Effect of Psychological Interventions on the Quality of Life in Women with Fibromyalgia: A Systematic Review. J. Clin. Psychol. Med. Settings 2021, 28, 503–517. [Google Scholar] [CrossRef] [PubMed]
- Sumpton, J.E.; Moulin, D.E. Fibromyalgia: Presentation and management with a focus on pharmacological treatment. Pain Res. Manag. 2008, 13, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Winkelmann, A.; Bork, H.; Brückle, W.; Dexl, C.; Heldmann, P.; Henningsen, P.; Krumbein, L.; Pullwitt, V.; Schiltenwolf, M.; Häuser, W. Physiotherapie, Ergotherapie und physikalische Verfahren beim Fibromyalgiesyndrom: Aktualisierte Leitlinie 2017 und Übersicht von systematischen Übersichtsarbeiten [Physiotherapy, occupational therapy and physical therapy in fibromyalgia syndrome: Updated guidelines 2017 and overview of systematic review articles]. Schmerz 2017, 31, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Pardos-Gascón, E.M.; Narambuena, L.; Leal-Costa, C.; van-der Hofstadt-Román, C.J. Differential efficacy between cognitive-behavioral therapy and mindfulness-based therapies for chronic pain: Systematic review. Int. J. Clin. Health Psychol. 2021, 21, 100197. [Google Scholar] [CrossRef]
- Hassett, A.L.; Gevirtz, R.N. Nonpharmacologic treatment for fibromyalgia: Patient education, cognitive-behavioral therapy, relaxation techniques, and complementary and alternative medicine. Rheum. Dis. Clin. N. Am. 2009, 35, 393–407. [Google Scholar] [CrossRef] [PubMed]
- Haugmark, T.; Hagen, K.B.; Smedslund, G.; Zangi, H.A. Mindfulness- and acceptance-based interventions for patients with fibromyalgia—A systematic review and meta-analyses. PLoS ONE 2019, 14, e0221897. [Google Scholar] [CrossRef]
- Adler-Neal, A.L.; Zeidan, F. Mindfulness Meditation for Fibromyalgia: Mechanistic and Clinical Considerations. Curr. Rheumatol. Rep. 2017, 19, 59. [Google Scholar] [CrossRef]
- Bravo, C.; Skjaerven, L.H.; Guitard Sein-Echaluce, L.; Catalan-Matamoros, D. Effectiveness of movement and body awareness therapies in patients with fibromyalgia: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2019, 55, 646–657. [Google Scholar] [CrossRef]
- Simister, H.D.; Tkachuk, G.A.; Shay, B.L.; Vincent, N.; Pear, J.J.; Skrabek, R.Q. Randomized Controlled Trial of Online Acceptance and Commitment Therapy for Fibromyalgia. J. Pain 2018, 19, 741–753. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C.M.; Montoro, C.I.; Moreno-Padilla, M.; Reyes Del Paso, G.A.; de la Coba, P. Effectiveness of Acceptance and Commitment Therapy in Central Pain Sensitization Syndromes: A Systematic Review. J. Clin. Med. 2021, 10, 2706. [Google Scholar] [CrossRef] [PubMed]
- American Psychological Association APA—División 12. Treatment Target: Fibromyalgia. 2023. APA. Available online: https://div12.org/diagnosis/fibromyalgia/ (accessed on 1 February 2023).
- Lumley, M.A.; Schubiner, H.; Lockhart, N.A.; Kidwell, K.M.; Harte, S.E.; Clauw, D.J.; Williams, D.A. Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: A cluster-randomized controlled trial. Pain 2017, 158, 2354–2363. [Google Scholar] [CrossRef] [PubMed]
- Thieme, K.; Turk, D.C. Cognitive-behavioral and operant-behavioral therapy for people with fibromyalgia. Reumatismo 2012, 64, 275–285. [Google Scholar] [CrossRef]
- García-Torres, F.; Alós, F.J.; Pérez-Dueñas, C.; Morina, J.A. Guía de Tratamientos Psicológicos Eficaces en Psiconcología. Alteraciones Psicológicas y Físicas; Pirámide Editorial: Madrid, Spain, 2016. [Google Scholar]
- Veehof, M.M.; Oskam, M.J.; Schreurs, K.M.G.; Bohlmeijer, E.T. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain 2011, 152, 533–542. [Google Scholar] [CrossRef]
- Ducasse, D.; Fond, G. Acceptance and commitment therapy. Encephale 2015, 41, 1–9. [Google Scholar] [CrossRef]
- Araújo, F.M.; DeSantana, J.M. Physical therapy modalities for treating fibromyalgia. F1000Res 2019, 8, 17176. [Google Scholar] [CrossRef]
- Assumpção, A.; Pagano, T.; Matsutani, L.A.; Ferreira, E.A.; Pereira, C.A.; Marques, A.P. Quality of life and discriminating power of two questionnaires in fibromyalgia patients: Fibromyalgia impact Questionnaire and medical outcomes study 36-Item short-form health survey. Rev. Bras. Fisioter. 2010, 14, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Okifuji, A.; Donaldson, G.W.; Barck, L.; Fine, P.G. Relationship between fibromyalgia and obesity in pain, function, mood, and sleep. J. Pain 2010, 11, 1329–1337. [Google Scholar] [CrossRef] [PubMed]
- Muñoz Ladrón de Guevara, C.; Reyes Del Paso, G.A.; Fernández Serrano, M.J.; Montoro, C.I. Fibromyalgia Syndrome and Cognitive Decline: The Role of Body Mass Index and Clinical Symptoms. J. Clin. Med. 2022, 11, 3404. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluß, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef]
- Morlion, B.; Kempke, S.; Luyten, P.; Coppens, E.; Van Wambeke, P. Multidisciplinary pain education program (MPEP) for chronic pain patients: Preliminary evidence for effectiveness and mechanisms of change. Curr. Med. Res. Opin. 2011, 27, 1595–1601. [Google Scholar] [CrossRef] [PubMed]
- Van Dyke, B.P.; Newman, A.K.; Moraís, C.A.; Burns, J.W.; Eyer, J.C.; Thorn, B.E. Heterogeneity of Treatment Effects in a Randomized Trial of Literacy-Adapted Group Cognitive-Behavioral Therapy, Pain Psychoeducation, and Usual Medical Care for Multiply Disadvantaged Patients with Chronic Pain. J. Pain 2019, 20, 1236–1248. [Google Scholar] [CrossRef] [PubMed]
- Conversano, C.; Poli, A.; Ciacchini, R.; Hitchcott, P.; Bazzichi, L.; Gemignani, A. A psychoeducational intervention is a treatment for fibromyalgia syndrome. Clin. Exp. Rheumatol. 2019, 37 (Suppl. 116), 98–104. [Google Scholar] [PubMed]
- Daviet, J.C.; Bonan, I.; Caire, J.M.; Colle, F.; Damamme, L.; Froger, J.; Leblond, C.; Leger, A.; Muller, F.; Simon, O.; et al. Therapeutic patient education for stroke survivors: Non-pharmacological management. A literature review. Ann. Phys. Rehabil. Med. 2012, 55, 641–656. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K. Patient Education: A Practical Approach; Sage: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- García-Ríos, M.C.; Navarro-Ledesma, S.; Tapia-Haro, R.M.; Toledano-Moreno, S.; Casas-Barragán, A.; Correa-Rodríguez, M.; Aguilar-Ferrándiz, M.E. Effectiveness of health education in patients with fibromyalgia: A systematic review. Eur. J. Phys. Rehabil. Med. 2019, 55, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Häuser, W.; Ablin, J.; Perrot, S.; Fitzcharles, M.A. Management of fibromyalgia: Practical guides from recent evidence-based guidelines. Pol. Arch. Intern. Med. 2017, 127, 47–56. [Google Scholar] [CrossRef]
- Häuser, W.; Thieme, K.; Turk, D.C. Guidelines on the management of fibromyalgia syndrome—A systematic review. Eur. J. Pain 2010, 14, 5–10. [Google Scholar] [CrossRef]
- Carville, S.F.; Arendt-Nielsen, L.; Bliddal, H.; Blotman, F.; Branco, J.C.; Buskila, D.; Da Silva, J.A.; Danneskiold-Samsøe, B.; Dincer, F.; Henriksson, C.; et al. EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann. Rheum. Dis. 2008, 67, 536–541. [Google Scholar] [CrossRef]
- Sarzi-Puttini, P.; Giorgi, V.; Atzeni, F.; Gorla, R.; Kosek, E.; Choy, E.H.; Bazzichi, L.; Häuser, W.; Ablin, J.N.; Aloush, V.; et al. Diagnostic and therapeutic care pathway for fibromyalgia. Clin. Exp. Rheumatol. 2021, 39 (Suppl. 130), 120–127. [Google Scholar] [CrossRef]
- Sarzi-Puttini, P.; Giorgi, V.; Atzeni, F.; Gorla, R.; Kosek, E.; Choy, E.H.; Bazzichi, L.; Häuser, W.; Ablin, J.N.; Aloush, V.; et al. Fibromyalgia position paper. Clin. Exp. Rheumatol. 2021, 39 (Suppl. 130), 186–193. [Google Scholar] [CrossRef]
- Berard, A.A.; Smith, A.P. Post Your Journey: Instagram as a Support Community for People with Fibromyalgia. Qual. Health Res. 2019, 29, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Antunes, M.D.; Schmitt, A.C.B.; Marques, A.P. Amigos de Fibro (Fibro Friends): Validation of an Educational Program to Promote Health in Fibromyalgia. Int. J. Environ. Res. Public Health 2022, 19, 5297. [Google Scholar] [CrossRef]
- Pérez-Aranda, A.; Angarita-Osorio, N.; Feliu-Soler, A.; Andrés-Rodríguez, L.; Borràs, X.; Luciano, J.V. Do humor styles predict clinical response to the MINDSET (MINDfulneSs & EducaTion) program? A pilot study in patients with fibromyalgia. Reumatol. Clin. (Engl. Ed.) 2021, 17, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Melin, E.O.; Svensson, R.; Thulesius, H.O. Psychoeducation against depression, anxiety, alexithymia and fibromyalgia: A pilot study in primary care for patients on sick leave. Scand. J. Prim. Health Care 2008, 36, 123–133. [Google Scholar] [CrossRef]
- Luciano, J.V.; Martínez, N.; Peñarrubia-María, M.T.; Fernández-Vergel, R.; García-Campayo, J.; Verduras, C.; Blanco, M.E.; Jiménez, M.; Ruiz, J.M.; López del Hoyo, Y.; et al. Effectiveness of a psychoeducational treatment program implemented in general practice for fibromyalgia patients: A randomized controlled trial. Clin. J. Pain 2011, 27, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Luciano, J.V.; Sabes-Figuera, R.; Cardeñosa, E.T.; Peñarrubia-María, M.; Fernández-Vergel, R.; García-Campayo, J.; Knapp, M.; Serrano-Blanco, A. Cost-utility of a psychoeducational intervention in fibromyalgia patients compared with usual care: An economic evaluation alongside a 12-month randomized controlled trial. Clin. J. Pain 2013, 29, 702–711. [Google Scholar] [CrossRef] [PubMed]
- Feliu-Soler, A.; Borràs, X.; Peñarrubia-María, M.T.; Rozadilla-Sacanell, A.; D’Amico, F.; Moss-Morris, R.; Howard, M.A.; Fayed, N.; Soriano-Mas, C.; Puebla-Guedea, M.; et al. Cost-utility and biological underpinnings of Mindfulness-Based Stress Reduction (MBSR) versus a psychoeducational programme (FibroQoL) for fibromyalgia: A 12-month randomized controlled trial (EUDAIMON study). BMC Complement. Altern. Med. 2016, 16, 81. [Google Scholar] [CrossRef]
- Dowd, H.; Hogan, M.J.; McGuire, B.E.; Davis, M.C.; Sarma, K.M.; Fish, R.A.; Zautra, A.J. Comparison of an Online Mindfulness-based Cognitive Therapy Intervention with Online Pain Management Psychoeducation: A Randomized Controlled Study. Clin. J. Pain 2015, 31, 517–527. [Google Scholar] [CrossRef]
- Bourgault, P.; Lacasse, A.; Marchand, S.; Courtemanche-Harel, R.; Charest, J.; Gaumond, I.; Barcellos de Souza, J.; Choinière, M. Multicomponent interdisciplinary group intervention for self-management of fibromyalgia: A mixed-methods randomized controlled trial. PLoS ONE 2015, 10, e0126324. [Google Scholar] [CrossRef]
- King, S.J.; Wessel, J.; Bhambhani, Y.; Sholter, D.; Maksymowych, W. The effects of exercise and education, individually or combined, in women with fibromyalgia. J. Rheumatol. 2002, 29, 2620–2627. [Google Scholar] [PubMed]
- Rooks, D.S.; Gautam, S.; Romeling, M.; Cross, M.L.; Stratigakis, D.; Evans, B.; Goldenberg, D.L.; Iversen, M.D.; Katz, J.N. Group exercise, education, and combination self-management in women with fibromyalgia: A randomized trial. Arch. Intern. Med. 2007, 167, 2192–2200. [Google Scholar] [CrossRef] [PubMed]
- Mannerkorpi, K.; Nordeman, L.; Ericsson, A.; Arndorw, M.; GAU Study Group. Pool exercise for patients with fibromyalgia or chronic widespread pain: A randomized controlled trial and subgroup analyses. J. Rehabil. Med. 2009, 41, 751–760. [Google Scholar] [CrossRef]
- Iannuccelli, C.; Lucchino, B.; Gioia, C.; Dolcini, G.; Favretti, M.; Franculli, D.; Di Franco, M. Mental health and well-being during the COVID-19 pandemic: Stress vulnerability, resilience and mood disturbances in fibromyalgia and rheumatoid arthritis. Clin. Exp. Rheumatol. 2021, 39 (Suppl. 130), 153–160. [Google Scholar] [CrossRef] [PubMed]
- Aloush, V.; Gurfinkel, A.; Shachar, N.; Ablin, J.N.; Elkana, O. Physical and mental impact of COVID-19 outbreak on fibromyalgia patients. Clin. Exp. Rheumatol. 2021, 39 (Suppl. 130), 108–114. [Google Scholar] [CrossRef]
- Davis, M.C.; Zautra, A.J. An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: Results of a randomized controlled trial. Ann. Behav. Med. 2013, 46, 273–284. [Google Scholar] [CrossRef]
- Ljótsson, B.; Atterlöf, E.; Lagerlöf, M.; Andersson, E.; Jernelöv, S.; Hedman, E.; Kemani, M.; Wicksell, R.K. Internet-delivered acceptance and values-based exposure treatment for fibromyalgia: A pilot study. Cogn. Behav. Ther. 2014, 43, 93–104. [Google Scholar] [CrossRef]
- Lai, L.; Liu, Y.; McCracken, L.M.; Li, Y.; Ren, Z. The efficacy of acceptance and commitment therapy for chronic pain: A three-level meta-analysis and a trial sequential analysis of randomized controlled trials. Behav. Res. Ther. 2023, 165, 104308. [Google Scholar] [CrossRef]
- Gowans, S.E.; DeHueck, A.; Voss, S. A randomized, controlled trial of exercise and education for individuals with fibromyalgia. Arthritis Care Res. 1999, 12, 120–128. [Google Scholar] [CrossRef]
- Hammond, A.; Freeman, K. Community patient education and exercise for people with fibromyalgia: A parallel group randomized controlled trial. Clin. Rehabil. 2006, 20, 835–846. [Google Scholar] [CrossRef]
- Arfuch, V.M.; Caballol Angelats, R.; Aguilar Martín, C.; Carrasco-Querol, N.; Sancho Sol, M.C.; González Serra, G.; Fusté Anguera, I.; Gonçalves, A.Q.; Berenguera, A. Assessing the benefits on quality of life of a multicomponent intervention for fibromyalgia syndrome in primary care: Patients’ and health professionals’ appraisals: A qualitative study protocol. BMJ Open 2020, 10, e039873. [Google Scholar] [CrossRef]
- Serrat, M.; Sanabria-Mazo, J.P.; García-Troiteiro, E.; Fontcuberta, A.; Mateo-Canedo, C.; Almirall, M.; Feliu-Soler, A.; Méndez-Ulrich, J.L.; Sanz, A.; Luciano, J.V. Efficacy of a Multicomponent Intervention for Fibromyalgia Based on Pain Neuroscience Education, Exercise Therapy, Psychological Support, and Nature Exposure (NAT-FM): Study Protocol of a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 7, 634. [Google Scholar] [CrossRef] [PubMed]
- Bruce, B.K.; Allman, M.E.; Rivera, F.A.; Wang, B.; Berianu, F.; Butendieck, R.R.; Calamia, K.T.; Hines, S.L.; Rummans, T.A.; Niazi, S.K.; et al. Intensive Multicomponent Fibromyalgia Treatment: A Translational Study to Evaluate Effectiveness in Routine Care Delivery. J. Clin. Rheumatol. 2021, 27, e496–e500. [Google Scholar] [CrossRef] [PubMed]
- Arnold, B.; Häuser, W.; Arnold, M.; Bernateck, M.; Bernardy, K.; Brückle, W.; Friedel, E.; Hesselschwerdt, H.J.; Jäckel, W.; Köllner, V.; et al. Multimodale Therapie des Fibromyalgiesyndroms. Systematische Übersicht, Metaanalyse und Leitlinie [Multicomponent therapy of fibromyalgia syndrome. Systematic review, meta-analysis and guideline. Schmerz 2012, 26, 287–290. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
