Outcomes Associated with a Single Joystick-Operated Ride-on-Toy Navigation Training Incorporated into a Constraint-Induced Movement Therapy Program: A Pilot Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Outcome Measures and Materials
2.2.1. Pretest–Posttest Measures of Motor Function
2.2.2. Training-Specific Measures Assessed during Early and Late Sessions
2.3. Procedures
2.3.1. Camp Structure and Activities
2.3.2. Ride-on-Toy Training Program
2.4. Statistical Analyses
3. Results
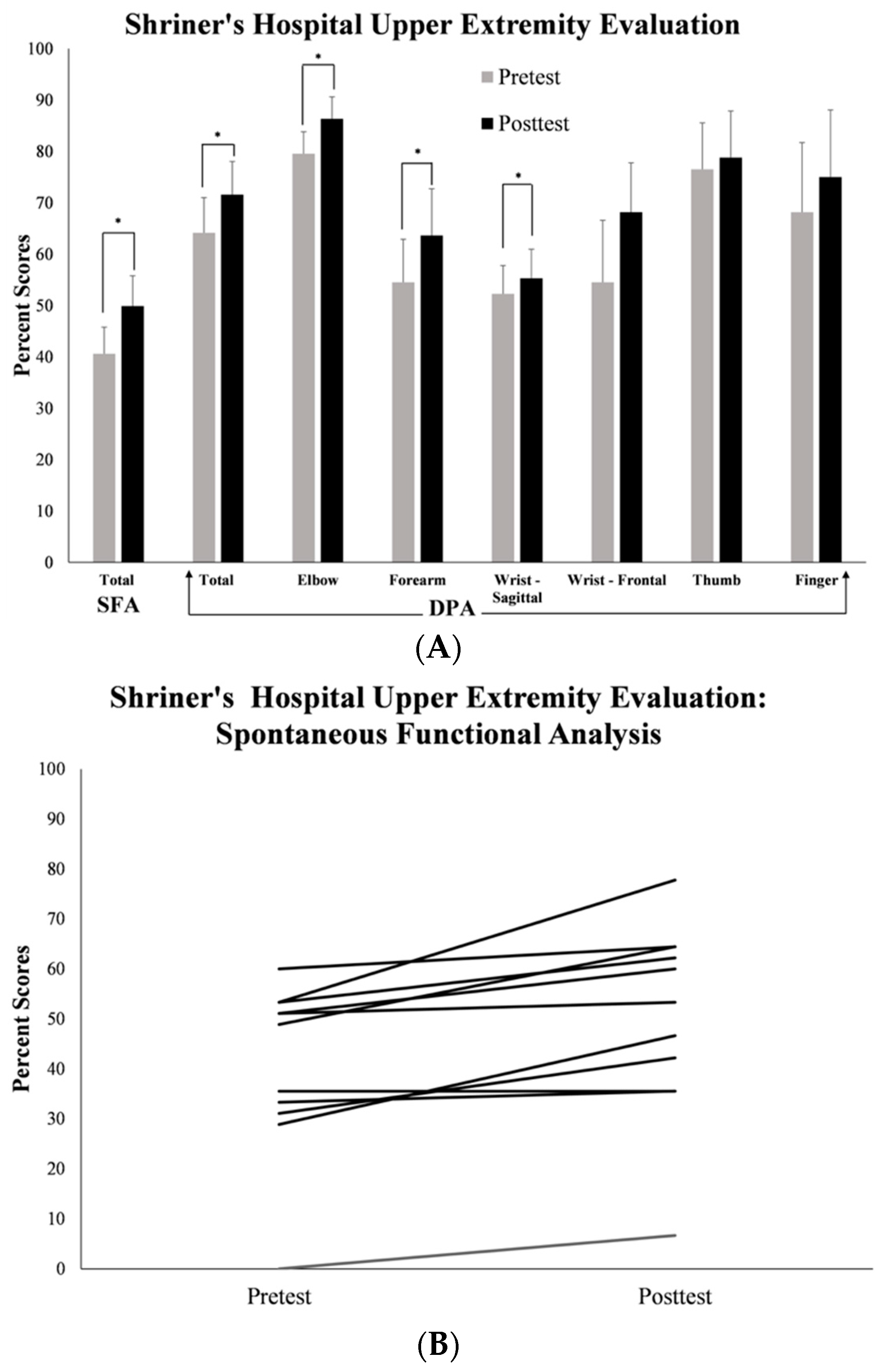
3.1. Pretest–Posttest Measures of Affected UE Motor Function
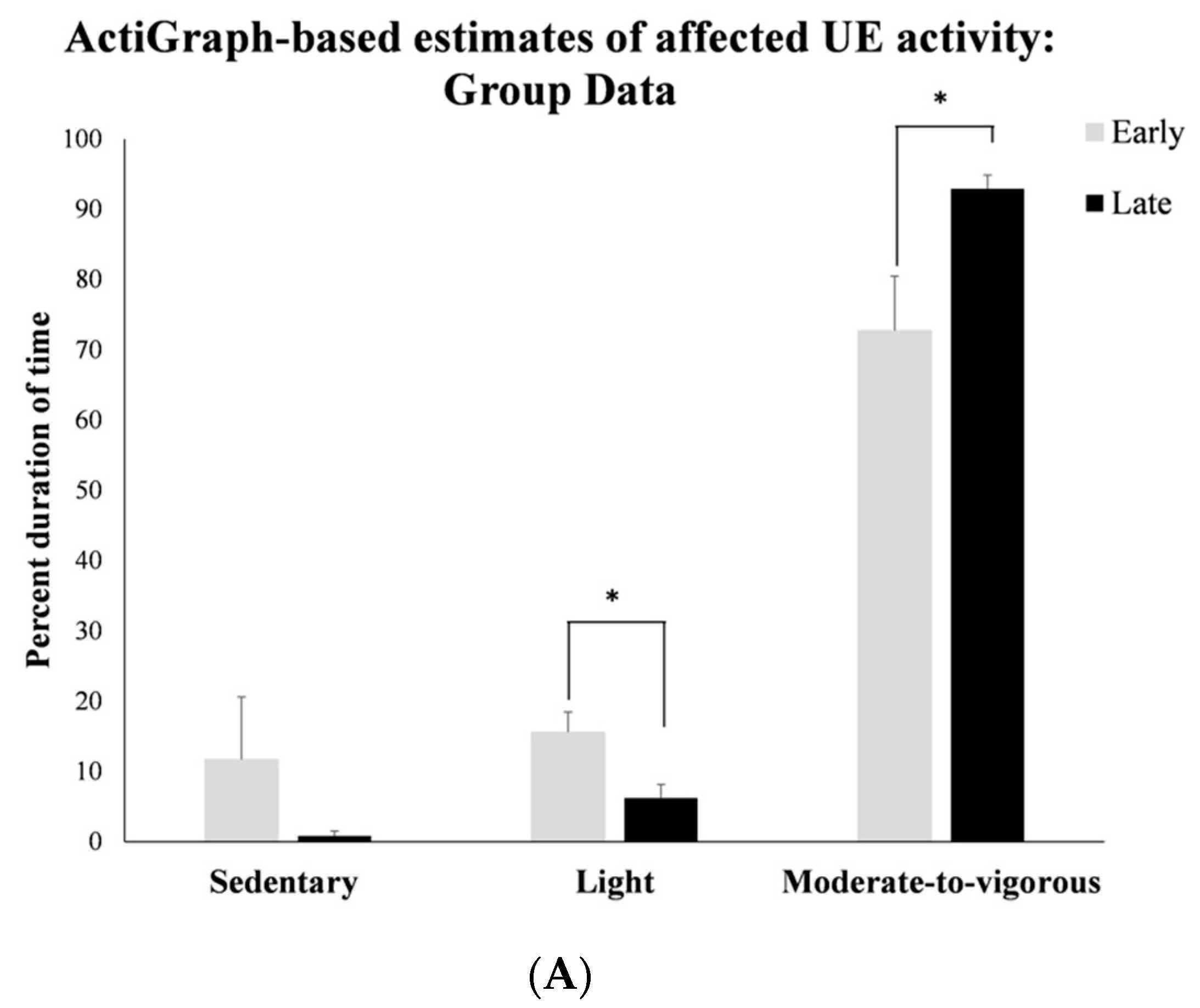
3.2. Objective Accelerometry-Based Measures of Affected UE Activity during Training Sessions
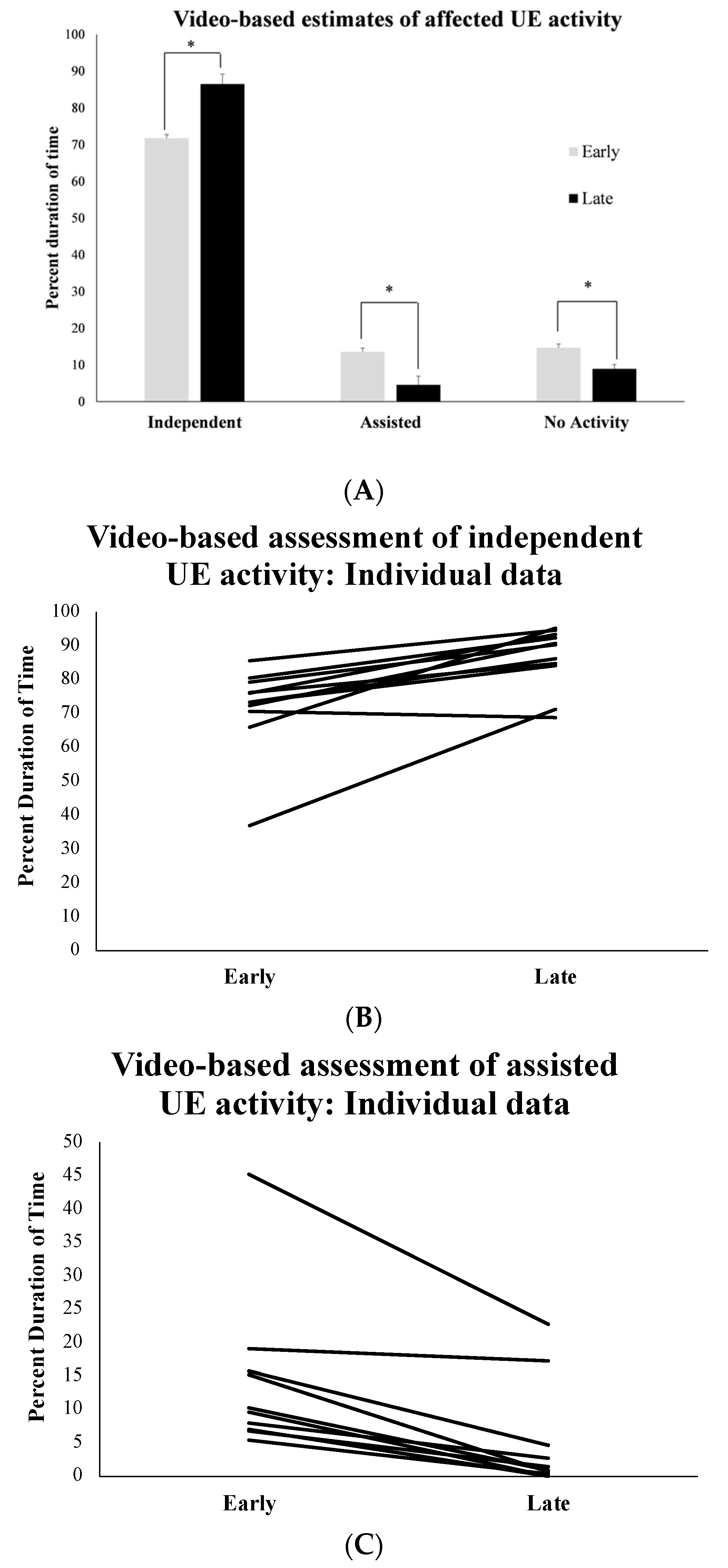
3.3. Observational Video-Based Assessment of Affected UE Activity during Training Sessions
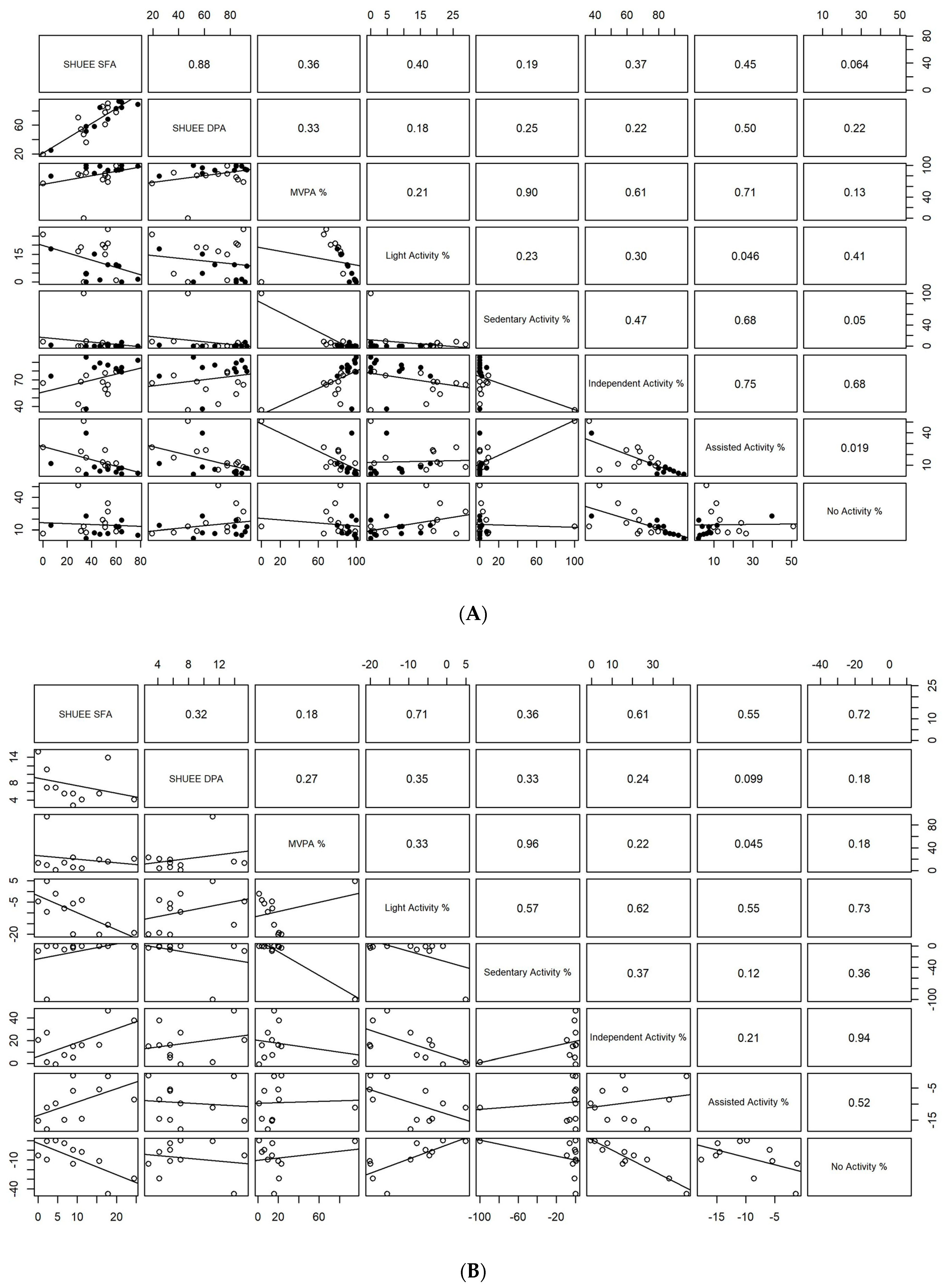
3.4. Exploratory Analyses of Associations between Pretest–Posttest and Training-Specific Measures of Affected UE Activity
4. Discussion
4.1. Summary of Results
4.2. Training-Related Changes in Affected UE Activity and Motor Function with ROT Navigation Training
4.3. Exploratory Associations between Pretest–Posttest and Training-Specific Measures of Affected UE Activity
4.4. Limitations & Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arner, M.; Eliasson, A.C.; Nichlasson, S.; Sommerstein, K.; Hagglund, G. Hand function in cerebral palsy. Report of 367 children in a population-based longitudinal health care program. J. Hand Surg. 2008, 33, 1337–1347. [Google Scholar] [CrossRef]
- Arnould, C.; Penta, M.; Thonnard, J. Hand impairments and their relationship with manual ability in children with cerebral palsy. J. Rehabil. Med. 2008, 39, 708–714. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Mc Namara, M.; Paton, M.C.B.; Popat, H. State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef] [PubMed]
- Taub, D.; Uswatte, G.; Bowman, M.; Mark, V.W.; Delgado, A.; Bryson, C.; Morris, D.; Bishop-McKay, S. Constraint-Induced Therapy Combined with Conventional Neurorehabilitation Techniques in Chronic Stroke Patients with Plegic Hands: A Case Series. Arch. Phys. Med. Rehabil. 2012, 94, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Dong, V.A.; Fong, K.; Chen, Y.F.; Tseng, S.; Wong, L. ‘Remind-to-move’ treatment versus constraint-induced movement therapy for children with hemiplegic cerebral palsy: A randomized controlled trial. Dev. Med. Child Neurol. 2017, 59, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.M.; Charles, J.; Wolf, S.L. Methods of constraint-induced movement therapy for children with hemiplegic cerebral palsy: Development of a child-friendly intervention for improving upper-extremity function. Arch. Phys. Med. Rehabil. 2005, 86, 837–844. [Google Scholar] [CrossRef]
- Eliasson, A.C.; Bonnier, B.; Krumlinde-Sundholm, L. Clinical experience of constraint induced movement therapy in adolescents with hemiplegic cerebral palsy—A day camp model. Dev. Med. Child Neurol. 2003, 45, 357–360. [Google Scholar] [CrossRef]
- Hoare, B.; Imms, C.; Leeane, C.; Jason, W. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: A Cochrane systematic review. Clin. Rehabil. 2007, 21, 675–685. [Google Scholar] [CrossRef]
- Ramey, S.L.; DeLuca, S.C.; Stevenson, R.D.; Conaway, M.; Darragh, A.R.; Lo, W. Constraint-induced movement therapy for cerebral palsy: A randomized trial. Pediatrics 2021, 148, e2020033878. [Google Scholar] [CrossRef]
- Sakzewski, L.; Ziviani, J.; Boyd, R.N. Efficacy of upper limb therapies for unilateral cerebral palsy: A meta-analysis. Pediatrics 2014, 133, e175–e204. [Google Scholar] [CrossRef]
- Sakzewski, L.; Provan, K.; Ziviani, J.; Boyd, R.N. Comparison of dosage of intensive upper limb therapy for children with unilateral cerebral palsy: How big should the therapy pill be? Res. Dev. Disabil. 2015, 37, 9–16. [Google Scholar] [CrossRef]
- Huang, H.; Huang, H.; Chen, Y.; Hsieh, Y.; Shih, M.; Chen, C. Modified ride-on cars and mastery motivation in young children with disabilities: Effects of environmental modifications. Res. Dev. Disabil. 2018, 83, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Tatla, S.K.; Sauve, K.; Jarus, T.; Virji-Babul, N.; Holsti, L. The effects of motivating interventions on rehabilitation outcomes in children and youth with acquired brain injuries: A systematic review. Brain Inj. 2014, 28, 1022–1035. [Google Scholar] [CrossRef] [PubMed]
- El-Shamy, S.M. Efficacy of Armeo® robotic therapy versus conventional therapy on upper limb function in children with hemiplegic cerebral palsy. Am. J. Phys. Med. Rehabil. 2018, 97, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Lin, S.; Yeh, C.; Chen, R.; Tang, H.; Ruan, S.; Wang, T. Development and Feasibility of a Kinect-Based Constraint-Induced Therapy Program in the Home Setting for Children with Unilateral Cerebral Palsy. Front. Bioeng. Biotechnol. 2021, 9, 755506. [Google Scholar] [CrossRef]
- Majnemer, A.; Shevell, M.; Law, M.; Poulin, C.; Rosenbaum, P. Level of motivation in mastering challenging tasks in children with cerebral palsy. Dev. Med. Child Neurol. 2010, 52, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Majnemer, A.; Shikako-Thomas, K.; Lach, L.; Shevell, M.; Law, M.; Schmitz, N. Mastery motivation in adolescents with cerebral palsy. Res. Dev. Disabil. 2013, 34, 3384–3392. [Google Scholar] [CrossRef]
- Bartlett, D.J.; Palisano, R.J. Physical therapists’ perceptions of factors influencing the acquisition of motor abilities of children with cerebral palsy: Implications for clinical reasoning. Phys. Ther. 2002, 82, 237–248. [Google Scholar] [CrossRef]
- James, D.; Pfaff, J.; Jeffries, M. Modified ride-on cars as early mobility for children with mobility limitations: A scoping review. Phys. Occup. Ther. Pediatr. 2019, 39, 525–542. [Google Scholar] [CrossRef]
- Logan, S.W.; Hospodar, C.M.; Feldner, H.A.; Huang, H.; Galloway, J.C. Modified Ride-on Car Use by Children with Complex Medical Needs. Pediatr. Phys. Ther. 2016, 28, 100–107. [Google Scholar] [CrossRef]
- Cheung, W.; Meadan, H.; Yang, H. Effects of powered mobility device interventions on social skills for children with disabilities: A systematic review. J. Dev. Phys. Disabil. 2020, 32, 855–876. [Google Scholar] [CrossRef]
- Hospodar, C.; Feldner, H.; Logan, S. Active mobility, active participation: A systematic review of modified ride-on car use by children with disabilities. Disabil. Rehabil. Assist. Technol. 2021, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Hospodar, C.M.; Sabet, A.; Logan, S.W.; Catena, M.A.; Galloway, J.C. Exploratory analysis of a developmentally progressive modified ride-on car intervention for young children with Down syndrome. Disabil. Rehabil. Assist. Technol. 2021, 16, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Sabet, A.; Feldner, H.; Tucker, J.; Logan, S.W.; Galloway, J.C. ON Time Mobility: Advocating for Mobility Equity. Pediatr. Phys. Ther. 2022, 34, 546–550. [Google Scholar] [CrossRef]
- Amonkar, N.; Kumavor, P.; Morgan, K.; Bubela, D.; Srinivasan, S. Feasibility of Using Joystick-Operated Ride-on-Toys to Promote Upper Extremity Function in Children with Cerebral Palsy: A Pilot Study. Pediatr. Phys. Ther. 2022, 34, 508–517. [Google Scholar] [CrossRef]
- Amonkar, N.; Sullivan, S.; Kumavor, P.; Morgan, K.; Bubela, D.; Srinivasan, S. Joystick-operated ride-on-toys as playful tools to improve upper extremity activity and function in children with hemiplegic cerebral palsy: Results of a pilot feasibility study. In Proceedings of the 76th Annual Meeting of the American Academy for Cerebral Palsy and Developmental Medicine (AACPDM), Las Vegas, NV, USA, 21–24 September 2022. [Google Scholar]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Öhrvall, A.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef]
- Klingels, K.; Jaspers, E.; Van de Winckel, A.; De Cock, P.; Molenaers, G.; Feys, H. A systematic review of arm activity measures for children with hemiplegic cerebral palsy. Clin. Rehabil. 2010, 24, 887–900. [Google Scholar] [CrossRef]
- Davids, J.R.; Peace, L.C.; Wagner, L.V.; Gidewall, M.A.; Blackhurst, D.W.; Roberson, W.M. Validation of the Shriners Hospital for Children Upper Extremity Evaluation (SHUEE) for children with hemiplegic cerebral palsy. Jbjs 2006, 88, 326–333. [Google Scholar] [CrossRef]
- Freedson, P.; Pober, D.; Janz, K.F. Calibration of accelerometer output for children. Med. Sci. Sports Exerc. 2005, 37, S523. [Google Scholar] [CrossRef]
- Chen, H.L.; Lin, K.C.; Hsieh, Y.W.; Wu, C.Y.; Liing, R.J.; Chen, C.L. A study of predictive validity, responsiveness, and minimal clinically important difference of arm accelerometer in real-world activity of patients with chronic stroke. Clin. Rehabil. 2018, 32, 75–83. [Google Scholar] [CrossRef]
- Hedges, L.V. Distribution theory for Glass’s estimator of effect size and related estimators. J. Educ. Stat. 1981, 6, 107–128. [Google Scholar] [CrossRef]
- Cohen, J. The effect size. In Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988; pp. 77–83. [Google Scholar]
- Jackman, M.; Lannin, N.; Galea, C.; Sakzewski, L.; Miller, L.; Novak, I. What is the threshold dose of upper limb training for children with cerebral palsy to improve function? A systematic review. Aust. Occup. Ther. J. 2020, 67, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Polatajko, H.J. Cognitive orientation to daily occupational performance (CO-OP) approach. In Physical & Occupational Therapy in Pediatrics; Hinojosa, J., Kramer, P., Royeen, C.B., Eds.; F.A. Davis Company: Philadelphia, PA, USA, 2017; pp. 183–206. [Google Scholar]
- Morgan, C.; Novak, I.; Dale, R.C.; Guzzetta, A.; Badawi, N. Single blind randomised controlled trial of GAME (Goals Activity Motor Enrichment) in infants at high risk of cerebral palsy. Res. Dev. Disabil. 2016, 55, 256–267. [Google Scholar] [CrossRef]
- Weightman, A.; Preston, N.; Levesley, M.; Bhakta, B.; Holt, R.; Mon-Williams, M. The nature of arm movement in children with cerebral palsy when using computer-generated exercise games. Disabil. Rehabil. Assist. Technol. 2014, 9, 219–225. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Translating Research into Clinical Practice; Wolters Kluwer Health: Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007. [Google Scholar]
- Diamond, A. Close interrelation of motor development and cognitive development and of the cerebellum and prefrontal cortex. Child Dev. 2000, 71, 44–56. [Google Scholar] [CrossRef]
- Gibson, J.J. The Theory of Affordances; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1977; Volume 1, pp. 67–82. [Google Scholar]
- Thelen, E.; Schöner, G.; Scheier, C.; Smith, L.B. The dynamics of embodiment: A field theory of infant perseverative reaching. Behav. Brain Sci. 2001, 24, 1–34. [Google Scholar] [CrossRef]
- Demers, M.; Fung, K.; Subramanian, S.K.; Lemay, M.; Robert, M.T. Integration of motor learning principles into virtual reality interventions for individuals with cerebral palsy: Systematic review. JMIR Serious Games 2021, 9, e23822. [Google Scholar] [CrossRef] [PubMed]
- Levin, M.F.; Weiss, P.; Keshner, E.A. Emergence of virtual reality as a tool for upper limb rehabilitation: Incorporation of motor control and motor learning principles. Phys. Ther. 2015, 95, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Taghizadeh, A.; Webster, K.E.; Bhopti, A.; Carey, L.; Hoare, B. Are they really motor learning therapies? A scoping review of evidence-based, task-focused models of upper limb therapy for children with unilateral cerebral palsy. Disabil. Rehabil. 2022, 9, 1–13. [Google Scholar] [CrossRef]
- Goyal, C.; Vardhan, V.; Naqvi, W.; Arora, S. Effect of virtual reality and haptic feedback on upper extremity function and functional independence in children with hemiplegic cerebral palsy: A research protocol. Pan Afr. Med. J. 2022, 41, 155. [Google Scholar] [CrossRef]
- Acar, G.; Altun, G.P.; Yurdalan, S.; Polat, M.G. Efficacy of neurodevelopmental treatment combined with the Nintendo® Wii in patients with cerebral palsy. J. Phys. Ther. Sci. 2016, 28, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Arps, K.; Darr, N.; Katz, J. Effect of adapted motorized ride-on toy use on developmental skills, quality of life, and driving competency in nonambulatory children age 9–60 months. Assist. Technol. 2021, 35, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Fasoli, S.E.; Fragala-Pinkham, M.; Hughes, R.; Hogan, N.; Stein, J.; Krebs, H.I. Upper limb robot-assisted therapy: A new option for children with hemiplegia. Technol. Disabil. 2010, 22, 193–198. [Google Scholar] [CrossRef]
- Fluet, G.G.; Qiu, Q.; Kelly, D.; Parikh, H.D.; Ramirez, D.; Saleh, S.; Adamovich, S.V. Interfacing a haptic robotic system with complex virtual environments to treat impaired upper extremity motor function in children with cerebral palsy. Dev. Neurorehabilit. 2010, 13, 335–345. [Google Scholar] [CrossRef]
- Spencer, K.; Yuen, H.K.; Jenkins, G.R.; Kirklin, K.; Vogtle, L.K.; Davis, D. The ‘magic’ of magic camp from the perspective of children with hemiparesis. J. Exerc. Rehabil. 2021, 17, 15–20. [Google Scholar] [CrossRef]
- Green, D.; Schertz, M.; Gordon, A.M.; Moore, A.; Schejter Margalit, T.; Farquharson, Y.; Ben Bashat, D.; Weinstein, M.; Lin, J.; Fattal-Valevski, A. A multi-site study of functional outcomes following a themed approach to hand–arm bimanual intensive therapy for children with hemiplegia. Dev. Med. Child Neurol. 2013, 55, 527–533. [Google Scholar] [CrossRef]
- Spencer, K.; Yuen, H.K.; Jenkins, G.R.; Kirklin, K.; Griffin, A.R.; Vogtle, L.K.; Davis, D. Evaluation of a magic camp for children with hemiparesis: A pilot study. Occup. Ther. Health Care 2020, 34, 155–170. [Google Scholar] [CrossRef]
- Hines, A.; Bundy, A.C.; Black, D.; Haertsch, M.; Wallen, M. Upper limb function of children with unilateral cerebral palsy after a magic-themed HABIT: A pre-post-study with 3-and 6-month follow-up. Phys. Occup. Ther. Pediatr. 2019, 39, 404–419. [Google Scholar] [CrossRef]
- Chang, H.J.; Ku, K.H.; Park, Y.S.; Park, J.G.; Cho, E.S.; Seo, J.S.; Kim, C.W. Effects of virtual reality-based rehabilitation on upper extremity function among children with cerebral palsy. Healthcare 2020, 8, 391. [Google Scholar] [CrossRef]
- Menekseoglu, A.K.; Capan, N.; Arman, S.; Aydin, A.R. Effect of a Virtual Reality-Mediated Gamified Rehabilitation Program on Upper Limb Functions in Children with Hemiplegic Cerebral Palsy: A Prospective, Randomized Controlled Study. Am. J. Phys. Med. Rehabil. 2023, 102, 198–205. [Google Scholar] [CrossRef]
- Roberts, H.; Shierk, A.; Clegg, N.J.; Baldwin, D.; Smith, L.; Yeatts, P.; Delgado, M.R. Constraint induced movement therapy camp for children with hemiplegic cerebral palsy augmented by use of an exoskeleton to play games in virtual reality. Phys. Occup. Ther. Pediatr. 2020, 41, 150–165. [Google Scholar] [CrossRef] [PubMed]
- Hines, A.; Bundy, A.C.; Haertsch, M.; Wallen, M. A magic-themed upper limb intervention for children with unilateral cerebral palsy: The perspectives of parents. Dev. Neurorehabilit. 2019, 22, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Waddell, K.J.; Klaesner, J.W.; Bland, M.D. A method for quantifying upper limb performance in daily life using accelerometers. JoVE (J. Vis. Exp.) 2017, 122, e55673. [Google Scholar]
- Coker-Bolt, P.; Downey, R.J.; Connolly, J.; Hoover, R.; Shelton, D.; Seo, N.J. Exploring the feasibility and use of accelerometers before, during, and after a camp-based CIMT program for children with cerebral palsy. J. Pediatr. Rehabil. Med. 2017, 10, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Beani, E.; Maselli, M.; Sicola, E.; Perazza, S.; Cecchi, F.; Dario, P.; Braito, I.; Boyd, R.; Cioni, G.; Sgandurra, G. Actigraph assessment for measuring upper limb activity in unilateral cerebral palsy. J. Neuroeng. Rehabil. 2019, 16, 30. [Google Scholar] [CrossRef]
- Goodwin, B.M.; Sabelhaus, E.K.; Pan, Y.; Bjornson, K.F.; Pham, K.; Walker, W.O.; Steele, K.M. Accelerometer measurements indicate that arm movements of children with cerebral palsy do not increase after constraint-induced movement therapy (CIMT). Am. J. Occup. Ther. 2020, 74, 7405205100p1–7405205100p9. [Google Scholar] [CrossRef]
- Sokal, B.; Uswatte, G.; Vogtle, L.; Byrom, E.; Barman, J. Everyday movement and use of the arms: Relationship in children with hemiparesis differs from adults. J. Pediatr. Rehabil. Med. 2015, 8, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Uswatte, G.; Miltner, W.; Foo, B.; Varma, M.; Moran, S.; Taub, E. Objective measurement of functional upper-extremity movement using accelerometer recordings transformed with a threshold filter. Stroke 2000, 31, 662–667. [Google Scholar] [CrossRef]
- Gordon, A.M.; Schneider, J.A.; Chinnan, A.; Charles, J.R. Efficacy of a hand–arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: A randomized control trial. Dev. Med. Child Neurol. 2007, 49, 830–838. [Google Scholar] [CrossRef]
- Poitras, I.; Clouâtre, J.; Campeau-Lecours, A.; Mercier, C. Accelerometry-Based Metrics to Evaluate the Relative Use of the More Affected Arm during Daily Activities in Adults Living with Cerebral Palsy. Sensors 2022, 22, 1022. [Google Scholar] [CrossRef]
- Hayward, K.S.; Eng, J.J.; Boyd, L.A.; Lakhani, B.; Bernhardt, J.; Lang, C.E. Exploring the role of accelerometers in the measurement of real world upper-limb use after stroke. Brain Impair. 2016, 17, 16–33. [Google Scholar] [CrossRef]
- Wang, T.; Lin, K.; Wu, C.; Chung, C.; Pei, Y.; Teng, Y. Validity, responsiveness, and clinically important difference of the ABILHAND questionnaire in patients with stroke. Arch. Phys. Med. Rehabil. 2011, 92, 1086–1091. [Google Scholar] [CrossRef] [PubMed]



| Child Number | Age at Visit | Gender | Race/Ethnicity | Side of Involvement | MACS Levels |
|---|---|---|---|---|---|
| 1 | 3 years 5 months | F | White, Non-Hispanic | L | 3 |
| 2 | 13 years 10 months | F | Asian | R | 3 |
| 3 | 8 years 11 months | M | White, Non-Hispanic | R | 3 |
| 4 | 4 years 6 months | F | White, Non-Hispanic | L | 2 |
| 5 | 5 years 28 days | M | Multiracial-Korean, Puerto Rican, Irish, and Polish | R | 2 |
| 6 | 8 years 3 months | F | White, Hispanic | R | 2 |
| 7 | 6 years 11 months | F | White, Non-Hispanic | R | 2 |
| 8 | 8 years 7 months | M | White, Hispanic | R | 3 |
| 9 | 4 years 2 months | M | White, Non-Hispanic | L | 4 |
| 10 | 6 years 11 months | M | Multiracial-White, Asian | R | 2 |
| 11 | 7 years 5 months | M | White, Non-Hispanic | R | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Srinivasan, S.; Amonkar, N.; Kumavor, P.; Morgan, K.; Bubela, D. Outcomes Associated with a Single Joystick-Operated Ride-on-Toy Navigation Training Incorporated into a Constraint-Induced Movement Therapy Program: A Pilot Feasibility Study. Behav. Sci. 2023, 13, 413. https://doi.org/10.3390/bs13050413
Srinivasan S, Amonkar N, Kumavor P, Morgan K, Bubela D. Outcomes Associated with a Single Joystick-Operated Ride-on-Toy Navigation Training Incorporated into a Constraint-Induced Movement Therapy Program: A Pilot Feasibility Study. Behavioral Sciences. 2023; 13(5):413. https://doi.org/10.3390/bs13050413
Chicago/Turabian StyleSrinivasan, Sudha, Nidhi Amonkar, Patrick Kumavor, Kristin Morgan, and Deborah Bubela. 2023. "Outcomes Associated with a Single Joystick-Operated Ride-on-Toy Navigation Training Incorporated into a Constraint-Induced Movement Therapy Program: A Pilot Feasibility Study" Behavioral Sciences 13, no. 5: 413. https://doi.org/10.3390/bs13050413
APA StyleSrinivasan, S., Amonkar, N., Kumavor, P., Morgan, K., & Bubela, D. (2023). Outcomes Associated with a Single Joystick-Operated Ride-on-Toy Navigation Training Incorporated into a Constraint-Induced Movement Therapy Program: A Pilot Feasibility Study. Behavioral Sciences, 13(5), 413. https://doi.org/10.3390/bs13050413





